What is relapsing polychondritis
Relapsing polychondritis is a rare autoimmune condition which presents as recurrent episodes of inflammation in cartilage bearing tissues like the ear, nose, larynx and trachea 1. The inflammatory episodes are recurrent and unpredictable. A concomitant autoimmune disease also occurs in more than 30% of patients. Jaksh-Wartenhorst described the first case in 1923. A 32-year-old patient presented with fever, pain, and swelling of the ears and later developed stenosis of external auditory canal and saddle nose deformity. A biopsy of the nasal cartilage showed the absence of cartilage. The term relapsing polychondritis was coined by Pearson and his coworkers in 1960. They recognized it as an inflammatory condition of the and noncartilaginous structures 2.
Relapsing polychondritis is a rare disease, being more common in Caucasians with the prevalence of 4.5 cases/million in a military population in the United States 3. The annual incidence was estimated at 3.5 per million person-years in Rochester, MN, USA 4. However, a population-based cohort study conducted in the United Kingdom found a lower annual incidence, estimated at 0.71 per million person-years. The same study estimated the prevalence of relapsing polychondritis and estimated it at 9.0 cases per million population 5. The peak age at onset is between 40 years to 50 years, though it can occur at any age. Relapsing polychondritis occurs with equal frequency in both sexes and all racial groups. Over 30% of cases are associated with existing autoimmune condition or hematologic condition 6.
Clinical spectrum of relapsing polychondritis is variable and varies with duration of the disease and disease severity. Ear cartilage involvement is present in 90% of the cases, and inflammation is restricted to the cartilaginous portion of the ear with sparing of the ear lobes. Patients most frequently present with discoloration of the ear and pain. Articular involvement is the second most common manifestation present in 50% to 75% of patients. Wrist, metacarpophalangeal, proximal interphalangeal joints are commonly involved. Eye manifestation occurs in 20% to 60% of relapsing polychondritis patients and involves episcleritis, scleritis, keratitis, and uveitis. Nose chondritis occurs in about 25% of cases. Inflammation of the cartilaginous rings around trachea and bronchi results in the collapse of these airways (tracheobronchomalacia). Patient presents with a cough, hoarseness of voice, wheezing. Respiratory compromise is the most frequent cause of death in these patients.
The diagnosis of relapsing polychondritis is not always easy because there are no specific tests. Even when diagnosed, the treatment is not standardized. The drug treatment is tailored to each patient and the cornerstone of therapy is the use of glucocorticoids. For patients with severe relapsing polychondritis, other immunosuppressive are used including methotrexate and cyclophosphamide 7. Recently newer biological agents have also been used to manage relapsing polychondritis patients with varying results. However, prior to initiating treatment with these novel agents, the patient needs a thorough work up to ensure that he or she is fit to receive the therapy. Any patient with worsening of symptoms should be referred to the specialist 8. People who develop severe heart or respiratory complications may require surgery.
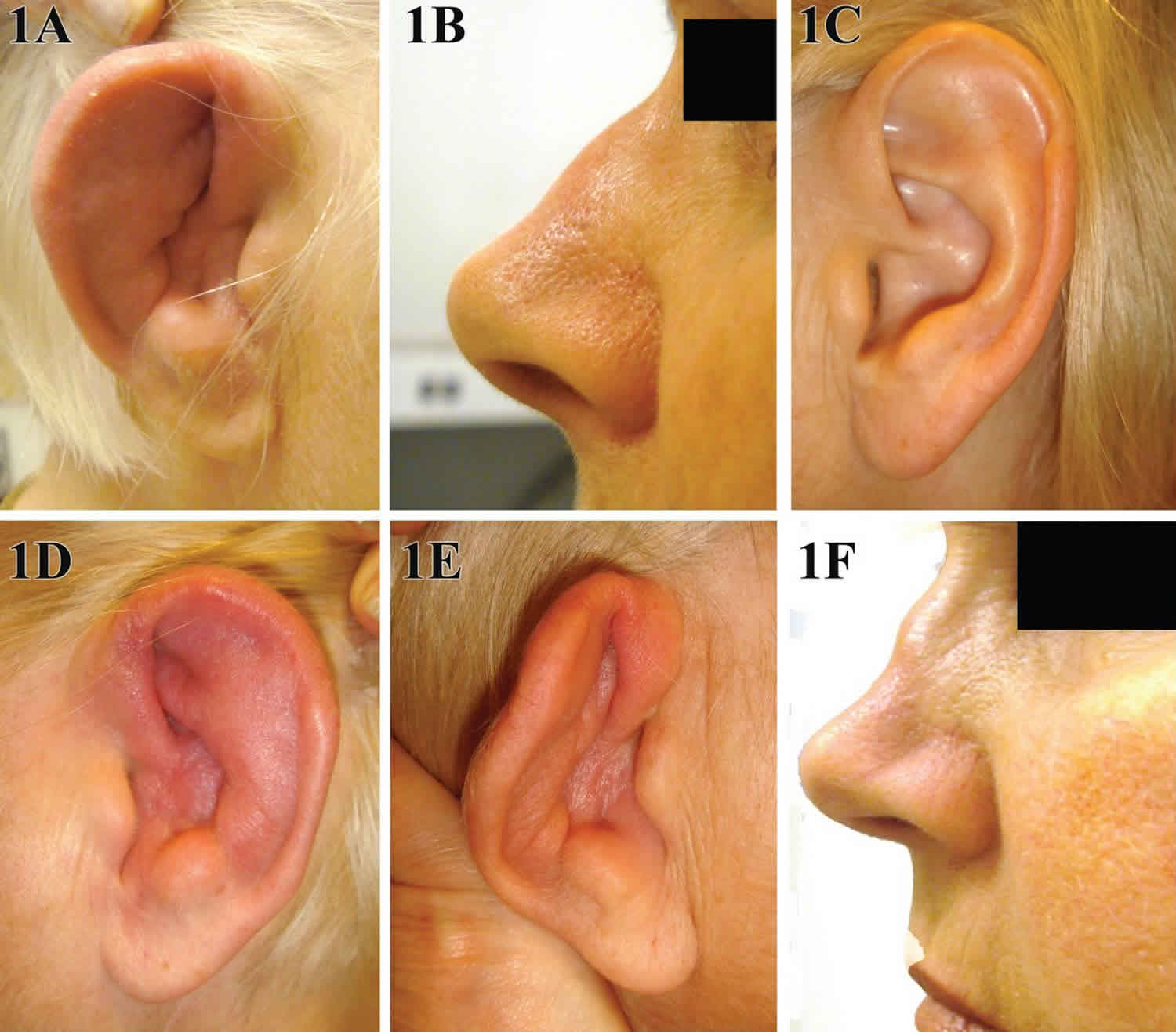
Figure 1. Relapsing polychondritis
Footnote: A 31-year-old man presented to the emergency department with a 2-week history of swelling of the left ear and a 6-month history of weight loss, fatigue, and generalized aches. During the 2 years before presentation, he had been treated multiple times with antibiotics for recurrent episodes of pain in both ears. The physical examination revealed a tender, erythematous, and edematous left pinna, with sparing of the lobule (Panel A). The patient also had a prominent saddle-nose deformity that had developed over the previous year (Panel B). The costochondral joints were tender on palpation, and the left knee was swollen and tender. Laboratory studies showed an erythrocyte sedimentation rate of more than 120 mm per hour (reference range, 0 to 15). He received a diagnosis of relapsing polychondritis, a systemic autoimmune condition that affects cartilaginous structures, particularly of the ears, nose, joints, larynx, and large airways. Prednisone was prescribed at a dose of 40 mg daily, and the patient had some alleviation of the pain and swelling within 2 weeks. After 1 month, therapy with methotrexate was started, and the prednisone was slowly tapered over a period of 6 months.
[Source 9]Relapsing polychondritis causes
The cause of relapsing polychondritis is not known 1. Scientists suspect that relapsing polychondritis is an autoimmune condition 10. It is suggested to result in a genetically predisposed individual on exposure to a triggering factor. The triggering factor may be an infectious agent, chemical, toxic exposure, or direct trauma. Relapsing polychondritis cases have been reported after trauma to the ear. A possible explanation includes cryptogenic antigenic release after trauma and recognition antigen by the immune system. Genetic studies have shown an association between HLA-DR4 antigen and relapsing polychondritis 11.
Relapsing polychondritis primarily involves cartilaginous structures, suggesting immune mechanism are acting against proteoglycan the main constituent of cartilage. Circulating and tissue-specific antibodies against collagen type II, IX and XI are shown in patients with relapsing polychondritis. In addition to humoral immunity, cellular immunity helps in maintaining cartilage inflammation. CD4+ cell secretes cytokines like interelukin-8, macrophage inflammatory protein 1β, monocyte chemoattractant protein one which leads to recruitment of monocyte and macrophages. Macrophage release proteolytic enzymes, metalloproteinase (MMP-3), cathepsin L and K which leads to the destruction of cartilage. In early stages of the disease there is polymorphic inflammatory cell infiltration, later there is chondrocyte apoptosis, focal calcification, and fibrosis of the cartilage 12.
Relapsing polychondritis symptoms
Relapsing polychondritis is characterized by recurrent inflammation of cartilage (the tough but flexible tissue that covers the ends of bones at a joint) and other tissues throughout the body.
Signs and symptoms of relapsing polychondritis include the following:
- Auricular chondritis
- Nonerosive seronegative inflammatory polyarthritis
- Nasal chondritis
- Ocular inflammation
- Respiratory tract chondritis
- Audiovestibular damage
- Cardiovascular disease
- Skin disease
- Central nervous system (CNS) manifestations
- Renal manifestations
- A variety of other conditions
The features of relapsing polychondritis and the severity of symptoms vary significantly from person to person, but may include:
- Ear: The ears are the most commonly affected body part. Symptoms include a sudden onset of pain, swelling, and tenderness of the cartilage of one or both ears. The pinna usually loses firmness and becomes floppy; hearing impairment may also occur. Inflammation of the inner ear may also cause nausea, vomiting, dizziness, and/or ataxia.
- Joint: The second most common finding is joint pain with or without arthritis.
- Eye: Affected people may experience episcleritis, uveitis and/or scleritis. Scleritis may lead to a bluish or dark discoloration of the sclera (white of the eye) and may even be associated with vision loss in severe cases. Proptosis (bulging out of one or both eye balls) may also be a symptom of relapsing polychondritis.
- Nose: Nasal cartilage inflammation may lead to stuffiness, crusting, rhinorrhea, epistaxis (nose bleeds), compromised sense of smell and/or saddle nose deformity (a condition where the nose is weakened and thus “saddled” in the middle).
- Airways: Inflammation may affect the larynx, trachea (windpipe), and bronchi (tubes that branch off the trachea and carry air to the lungs). Airway involvement may lead to a cough, wheezing, hoarseness and recurrent infections. It can become life-threatening if not properly diagnosed and managed.
Less commonly, relapsing polychondritis may affect the heart, kidneys, nervous system, gastrointestinal tract, and/or vascular (veins) system. Nonspecific symptoms such as fever, weight loss, malaise, and fatigue may also be present.
In approximately one third of affected people, relapsing polychondritis is associated with other medical problems. Conditions reportedly associated with relapsing polychondritis include hematological disease (including Hodgkin’s lymphoma and myelodysplastic syndromes); gastrointestinal disorders (including Crohn’s disease and ulcerative colitis); endocrine diseases (including diabetes mellitus type 1 and thyroid disorders) and others.
Episodes of relapsing polychondritis may last a few days or weeks and typically resolve with or without treatment. However, it is generally progressive, and many people have persistent symptoms in between flares.
Table 1. Systemic vasculitis and connective tissue disorders associated with relapsing polychondritis (not exhaustive)
| Systemic vasculitis | Behçet’s disease (MAGIC syndrome), granulomatosis with polyangiitis, polyarthritis nodosa, Churg and Strauss’s syndrome |
| Connective tissue diseases | Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, mixed connective tissue diseases, systemic sclerosis |
| Spondyloarthritis | Ankylosing spondylitis, psoriatic arthritis, reactive arthritis, inflammatory bowels diseases |
| Other autoimmune diseases | Autoimmune thyroiditis, type 1 diabetes, familial Mediterranean fever, myasthenia gravis, primary biliary cirrhosis |
| Malignancies | Myelodysplastic syndromes, lymphomas, myeloproliferative neoplasms, thymoma |
| Dermatosis | Sweet’s syndrome, neutrophilic dermatosis, pyoderma gangrenosum, leukocytoclastic vasculitis, psoriasis |
Abbreviation: MAGIC, mouth and genital ulcers with inflamed cartilage
[Source 13 ]Relapsing polychondritis complications
Complications of relapsing polychondritis include the following:
- Vertigo
- Tinnitus
- Voice hoarseness
- Joint deformity
- Epiglottitis
- Scleritis
- Conjunctivitis
- Iritis
- Need for permanent tracheotomy (severe cases)
- Severe pulmonary infection
- Blindness
- Frail chest wall
- Respiratory failure
- Aortic regurgitation
- Mitral regurgitation
- Aortic dissection
- Glomerulonephritis-associated renal failure
Relapsing polychondritis diagnosis
Diagnosis of relapsing polychondritis is primarily based on a combination of clinical features, radiology, and biopsy of a cartilaginous site. It is guided by a set of clinical criteria suggested by McAdams et al. 14, three of out of six criteria are required to make the diagnosis. These include:
- Recurrent chondritis of both auricles
- Nonerosive inflammatory arthritis
- Chondritis of nasal cartilages
- Inflammation of ocular structures: conjunctivitis/keratitis/scleritis/uveitis
- Chondritis of respiratory tract: Laryngeal, tracheal cartilage
- Cochlear or vestibular damage: Neurosensory hearing loss/tinnitus/vertigo
Any patient suspecting of having relapsing polychondritis should have a dynamic exploratory CT scan to evaluate for airway involvement. CT scans show functional airway abnormalities such as air trapping and collapse. It can also show thickening of the airway wall and luminal narrowing. Pulmonary function testing is done to evaluate for airway trapping. Pulmonary function test should be done to evaluate for lung volumes. PET-CT is a new diagnostic modality which helps in early disease recognition and provides a site for targeted biopsy.
Biopsy of auricular cartilage is performed to confirm the diagnosis of polychondritis. When relapsing polychondritis is associated with other Rheumatic diseases, positive serologic tests for rheumatoid factor, the anti-nuclear antibody may be seen. Complement levels are usually normal in patients with relapsing polychondritis. A non-erosive process of juxta-articular osteopenia and uniform, joint space narrowing characterizes arthropathy of relapsing polychondritis. Anti-type II collagen antibody tests are not routinely available, and hen these tests are done, these antibodies are not present in all the cases. There are no lab markers to assess for ongoing cartilage damage.
Relapsing polychondritis treatment
Due to the rarity of relapsing polychondritis, there are no there is no standardized treatment approach, and the treatment is guided by the clinical presentation and the severity of the disease 15.
Relapsing polychondritis is a complex condition that requires a team approach for patient care, as follows:
- Dermatologists or specialists in infectious diseases are often involved early in the course of the disease to evaluate the patient for infectious causes of cellulitis or perichondritis.
- Rheumatologists usually become the primary care provider and should be involved early in patient care.
- Ophthalmologists should also be involved early to diagnose, monitor, and treat the potentially devastating ocular complications.
- Cardiologists, neurologists, nephrologists, and otolaryngologists may be asked to manage other aspects of relapsing polychondritis.
- Plastic surgeons can aid in nasal reconstruction if saddle-nose deformity is present.
For patients presenting with ear, nasal or joint involvement but no systemic involvement, anti-inflammatory medications, colchicine or dapsone is recommended. Low-dose glucocorticoid therapy is often required.
For patients with large airway involvement (laryngeal or tracheobronchial chondritis), abrupt onset of sensorineural hearing loss, ocular involvement IV methylprednisolone 1 gram for three days followed by oral prednisone 1 mg/kg along with immunosuppressive therapy is indicated 1. Most commonly used immunosuppressive agents include cyclophosphamide, methotrexate, azathioprine and cyclosporine. Cyclophosphamide is commonly used as the initial medication (1 mg/kg to 2 mg/kg) after remission is achieved it is switched to other less toxic immunosuppressive agents like azathioprine or methotrexate.
Biologics have been used in the treatment of relapsing polychondritis, most commonly used biologic is TNF inhibitor-Infliximab. Other biologics which have been tried with variable results include Adalimumab, etanercept, abatacept, tocilizumab. Data on Rituximab did not show success, and this agent is not recommended as the first line biologic agent.
Surgical intervention such as stenting, airway dilation, tracheostomy and laryngotracheal reconstruction are needed in case of airway collapse.
Surgical treatment
Surgeries encountered in the care of patients with relapsing polychondritis may include the following:
- Tracheostomy
- Permanent tracheotomy placement
- Tracheal stent placement
- Aortic aneurysm repair
- Cardiac valve replacement
- Saddle-nose deformity repair
Subglottic stenosis can be treated with submucosal corticosteroid injection followed by serial dilation. Wierzbicka et al reported good airway patency for more than 24 months in eight of 12 patients with relapsing polychondritis or other autoimmune disorders treated with this approach. [58]
The benefits of any proposed surgery must be weighed adequately against the patient’s risk for infection, especially in the event of acute relapse, since patients are at an increased risk of infection whether or not they are using corticosteroids.
Additionally, patients with relapsing polychondritis and tracheal disease may be at particular risk regarding complications resulting from tracheal intubation and extubation.
Relapsing polychondritis prognosis
The prognosis or long-term outlook for people with relapsing polychondritis varies from person to person. In general, relapsing polychondritis is a chronic and progressive (worsening overtime) condition. Some form of disability is common in the later stages of relapsing polychondritis; these may include visual impairment, hearing loss, vestibular dysfunction, and/or cardiopulmonary (heart and lung) disease 16.
Complications of relapsing polychondritis such as saddle-nose deformity, systemic vasculitis, laryngotracheobronchial stricture, arthritis, and anemia in patients younger than 51 years portend a poorer prognosis than in age-matched patients with relapsing polychondritis without complications. In patients older than 51 years, only anemia is associated with a poorer prognosis. Renal involvement is a poor prognostic factor at all ages.
Severe cases of relapsing polychondritis can be life-threatening. Respiratory complications (windpipe collapse and infections) are the most common cause of death followed by cardiovascular (heart and blood vessel) involvement 17.
In recent years, improvements have been made in the outcomes of patients with relapsing polychondritis. Survival rates have increased from 70% after 5 years, to 94% after 8 years and even 91% after 10 years in a recent study 18.
Relapsing polychondritis life expectancy
Patients with relapsing polychondritis have frequent relapses and the quality of life is poor. The mortality rate of relapsing polychondritis patients is twice that of the general population. The outcome of patients with relapsing polychondritis has improved in the recent years; survival has increased from 70% at five years to 91% at ten years 1. However, those data may represent relapsing polychondritis in patients with less severe disease than patients studied in earlier reports. Another study reported a 5-year survival rate associated with relapsing polychondritis has been reported to be 66-74% (45% if relapsing polychondritis occurs with systemic vasculitis), with a 10-year survival rate of 55% 19.
The more common clinical presentation is a relatively benign disease with respiratory failure due to airway collapse being the most common cause of death.
The most frequent causes of death associated with relapsing polychondritis include infection secondary to corticosteroid treatment or respiratory compromise (10%-50% of deaths result from airway complications), systemic vasculitis, and malignancy unrelated to relapsing polychondritis.
Although the life expectancy in all patients with relapsing polychondritis is decreased compared with age- and sex-matched healthy individuals, patients with renal involvement have a significantly lower age-adjusted life expectancy. In those with renal disease, uremia is the third most frequent cause of death.
Until randomized controlled studies are available, the treatment of relapsing polychondritis will remain empirical and based on personal experience. For healthcare workers who have never treated such a patient, referral to a tertiary care center is recommended 20.
References- Chauhan K, Hanna A. Relapsing Polychondritis. [Updated 2019 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436007
- Borgia F, Giuffrida R, Guarneri F, Cannavò SP. Relapsing Polychondritis: An Updated Review. Biomedicines. 2018 Aug 02;6, 3.
- Relapsing polychondritis in the Department of Defense population and review of the literature. Mathew SD, Battafarano DF, Morris MJ. Semin Arthritis Rheum. 2012 Aug; 42(1):70-83.
- Relapsing polychondritis. Kent PD, Michet CJ Jr, Luthra HS. Curr Opin Rheumatol. 2004 Jan; 16(1):56-61.
- Incidence and mortality of relapsing polychondritis in the UK: a population-based cohort study. Hazra N, Dregan A, Charlton J, Gulliford MC, D’Cruz DP. Rheumatology (Oxford). 2015 Dec; 54(12):2181-7.
- Leung KK, Edani S. Red-eared zebra diagnosis: Case of relapsing polychondritis. Can Fam Physician. 2018 May;64(5):363-367.
- Meshkov AD, Novikov PI, Zhilyaev EV, Ilevsky IDJ, Moiseev SV. Tofacitinib in steroid-dependent relapsing polychondritis. Ann. Rheum. Dis. 2018 May 03
- Moulis G, Pugnet G, Costedoat-Chalumeau N, Mathian A, Leroux G, Boutémy J, Espitia O, Bouillet L, Berthier S, Gaultier JB, Jeandel PY, Konaté A, Mékinian A, Solau-Gervais E, Terrier B, Wendling D, Andry F, Garnier C, Cathébras P, Arnaud L, Palmaro A, Cacoub P, Amoura Z, Piette JC, Arlet P, Lapeyre-Mestre M, Sailler L. Efficacy and safety of biologics in relapsing polychondritis: a French national multicentre study. Ann. Rheum. Dis. 2018 Aug;77(8):1172-1178
- Relapsing Polychondritis. N Engl J Med 2018; 378:1715 DOI: 10.1056/NEJMicm1713302 https://www.nejm.org/doi/full/10.1056/NEJMicm1713302
- Relapsing Polychondritis. https://rarediseases.org/rare-diseases/relapsing-polychondritis/
- Paravar T. Less common rheumatologic disorders: Current concepts of skin and systemic manifestations. Clin. Dermatol. 2018 Jul – Aug;36(4):525-532
- Zampeli E, Moutsopoulos HM. Relapsing polychondritis: a diagnosis not to be missed. Rheumatology (Oxford). 2018 Oct 01;57(10):1768.
- Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol. 2018;10:1-11. Published 2018 Jan 9. doi:10.2147/OARRR.S142892 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768290/
- Rose T, Schneider U, Bertolo M, Klotsche J, Casteleyn V, Biesen R, Burmester GR, Hiepe F. Observational study and brief analysis of diagnostic criteria in relapsing polychondritis. Rheumatol. Int. 2018 Nov;38(11):2095-2101
- Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol. 2018;10:1-11
- Relapsing Polychondritis. https://emedicine.medscape.com/article/331475-overview
- Relapsing polychondritis. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=728
- Puéchal X, Terrier B, Mouthon L, Costedoat-Chalumeau N, Guillevin L, Le Jeunne C. Relapsing polychondritis. Joint Bone Spine. March 2014; 81(2):118-124
- Michet CJ Jr, McKenna CH, Luthra HS, O’Fallon WM. Relapsing polychondritis. Survival and predictive role of early disease manifestations. Ann Intern Med. 1986 Jan. 104(1):74-8.
- Sharma A, Law AD, Bambery P, Sagar V, Wanchu A, Dhir V, Vijayvergiya R, Sharma K, Gupta A, Panda NK, Singh S. Relapsing polychondritis: clinical presentations, disease activity and outcomes. Orphanet J Rare Dis. 2014 Dec 20;9:198.