Renal vein thrombosis
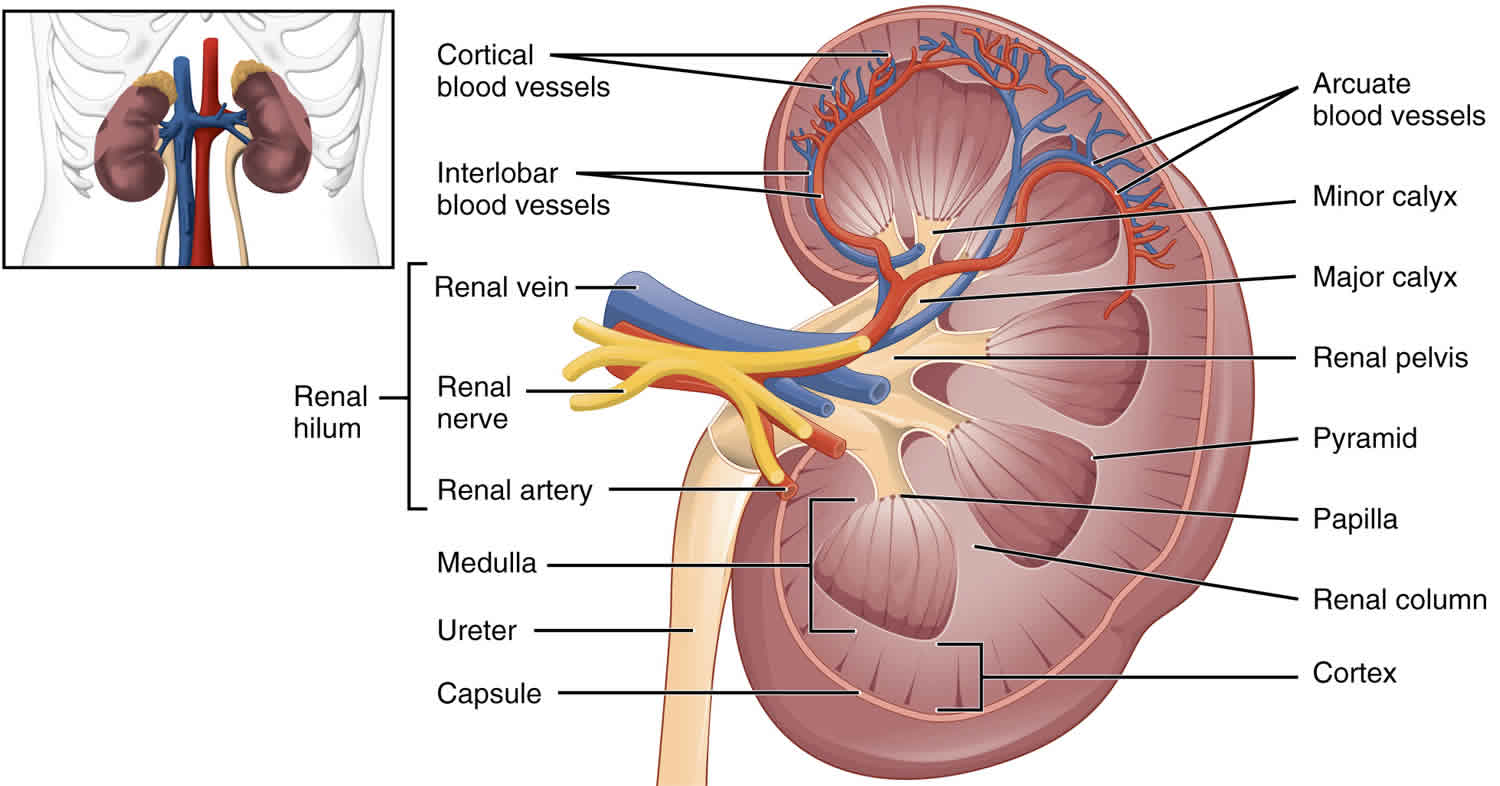
Renal vein thrombosis is the presence of thrombus in the major renal veins or its tributaries and it is a rare clinical entity. Renal vein thrombosis can present acutely or go unnoticed and can result in acute kidney injury or chronic kidney disease 1. Renal vein thrombosis is commonly associated with nephrotic syndrome (i.e., >3 g/day protein loss in the urine, hypoalbuminemia, hypercholesterolemia, edema), primary hypercoagulability disorders, renal cell cancer, extrinsic compression, infections, trauma, Behçet syndrome, antiphospholipid antibody syndrome or as a post-renal transplant complication 2. Almost two-thirds of patients have bilateral renal vein involvement. The left renal vein is more commonly involved due to its extensive venous network compared to the right. Thrombosis may extend from the vena cava into the peripheral venules or may originate in the peripheral veins and propagate to the main renal vein 3. The severe passive congestion that develops causes the kidney to swell and become engorged, leading to degeneration of nephrons and causing symptoms of flank pain, hematuria and decreased urine output.
In the intrauterine life, renal vein thrombosis can occur mostly in the presence of factor V Leiden 4. In the neonates, renal vein thrombosis is one of the most frequent causes of venous thrombosis and usually follows severe dehydration or prolonged periods of hypotension 5.
There is scarce data on the exact US prevalence of renal vein thrombosis in adults as it is often asymptomatic with spontaneous resolution. There is also a high degree of variability as the reported number of cases of renal vein thrombosis in patients with nephrotic syndrome, and membranous nephropathy is 5% to 60% 6.
No specific numbers are available for the frequencies of renal vein thrombosis by gender. However, since renal vein thrombosis is commonly associated with membranous nephropathy, a male predominance is reported. This is because membranous nephropathy has a 2:1 male to female ratio. Similarly, age is a factor in renal vein thrombosis only to the extent as any age-related risk of glomerular disease, for example, membranous nephropathy peaks in the fourth through the sixth decade, making renal vein thrombosis likely in this specific age group). Lastly, there is no racial predilection.
Renal vein thrombosis causes
The most common cause of renal vein thrombosis is nephrotic syndrome (i.e., >3 g/day protein loss in the urine, hypoalbuminemia, hypercholesterolemia, edema), as it results in a hypercoagulable state 1. Nephrotic syndrome is responsible for a hypercoagulable state. The excessive urinary protein loss is associated with decreased antithrombin III, a relative excess of fibrinogen, and changes in other clotting factors; all lead to a propensity to clot 7. Numerous studies have demonstrated a direct relation between nephrotic syndrome and both arterial and venous thromboses. Why the renal vein is susceptible to thrombosis is unclear 8.
In patients who are nephrotic, the most common underlying nephropathy associated with renal vein thrombosis is membranous nephropathy, followed by minimal change disease, and membranoproliferative glomerulonephritis 9. Other common systemic and local causes of renal vein thrombosis are as follows:
Systemic causes of renal vein thrombosis
- Primary hypercoagulability disorders (e.g., antithrombin III deficiency, protein C or S deficiency, factor V Leiden mutation, prothrombin G20210A mutation)
- Antiphospholipid syndrome
- Postrenal transplant/allograft rejection
- Renal vasculitis
- Sickle cell nephropathy 10
- Systemic lupus erythematosus (SLE)
- Amyloidosis
- Diabetic nephropathy
- Pregnancy or estrogen therapy
- Behcet syndrome
- Severe dehydration or prolonged hypotension (especially in neonates)
Local causes of renal vein thrombosis
- The malignant renal tumors, typically renal cell carcinoma that extends into the renal veins, are associated with thrombus in 4% to 25% of cases 11.
- Extrinsic compression of the renal vein or inferior vena cava due to a tumor, lymph nodes, retroperitoneal disease or an aortic aneurysm
- Blunt abdominal trauma or trauma during venography
In children, renal vein thrombosis is the most common vascular condition in the neonatal kidney 12:
- Dehydration and sepsis are common underlying factors for renal vein thrombosis
- Sickle cell disease 13
- Polycythemia
- Maternal diabetes
- Indwelling umbilical venous catheters
The pathogenesis of renal vein thrombosis is based on the Virchow’s triad which is due to one or more of the following:
- Vascular endothelial damage due to an injury of the vessel wall or in cases of homocystinuria where high levels of homocysteine cause spontaneous microtrauma to the endothelium
- Stasis of blood flow, for example, in severe dehydration/volume depletion in infants
- A hypercoagulable state such as in patients with nephrotic syndrome where excessive urinary protein loss, decreased antithrombin III levels, a relative excess of fibrinogen, and changes in other clotting factors; all leads to the propensity of a clot
Renal vein thrombosis symptoms
Most often, renal vein thrombosis has an insidious onset, producing minimal to no symptoms and is usually diagnosed incidentally during imaging for some other reason.
Clinical presentation of renal vein thrombosis varies by the rapidity of venous occlusion and development of venous collaterals. Chronic renal vein thrombosis has an insidious onset and is usually asymptomatic. Rarely, it may present as peripheral edema.
Acute renal vein thrombosis usually presents with symptoms of renal infarction, including flank pain, flank tenderness, rapid deterioration of renal function and worsening proteinuria, micro or macroscopic hematuria. Nausea, vomiting or fever may be present.
In a renal transplant, renal vein thrombosis usually presents within 48 hours of surgery manifesting as sudden anuria and tenderness over the transplanted kidney.
In neonates and infants, acute renal vein thrombosis may present with gross hematuria, flank mass, signs and symptoms of dehydration or shock, and oligo-anuria.
Left-sided renal vein thrombosis can lead to gonadal vein thrombosis manifested as pelvic congestion syndrome in females and whereas in males with painful swelling of the left testis and varicocele.
Renal vein thrombosis complications
Renal vein thrombosis complications include a decline in renal function, leading to chronic kidney disease with a potential to lead to end-stage renal disease. Renal atrophy, hypertension or extension of thrombus/embolism may occur. Left-sided renal vein thrombosis may cause pelvic congestion syndrome in females and swelling of left testis or varicocele in males. Renal vein thrombosis after renal transplant usually occurs early after the surgery and has a reported prevalence of 0.1% to 4.2% and ultimately leads to loss of graft in almost all cases 14.
Renal vein thrombosis diagnosis
Renal venography is the gold standard diagnostic test for renal vein thrombosis and has the additional advantage of a therapeutic procedure. However, it is rarely used in current practice due to the availability of lesser invasive tests. Renal ultrasonography is a safe, non-invasive test, though it is usually not sensitive enough to make a diagnosis of renal vein thrombosis. Renal ultrasonography shows an enlarged kidney and hyper-echogenic kidney in approximately 90% of the patients in the early phase of acute renal vein thrombosis 15. Color Doppler or contrast-enhanced ultrasonography may yield better results. Computed tomography (CT) angiography is the test of choice for diagnosing renal vein thrombosis which can demonstrate thrombus in the renal vein and, at times, in the vena cava. The sensitivity and specificity of CT angiography is almost 100% 16. Contrast-enhanced, 3D magnetic resonance venography is as sensitive as CT and has the major benefit of avoidance of radiation and intravenous (IV) contrast. Both CT and 3D magnetic resonance venography can help detect renal vein thrombosis as well as the presence of renal cell cancer.
No specific laboratory studies are indicated for renal vein thrombosis (renal vein thrombosis), except those specific for the underlying etiology (e.g., for nephrotic syndrome or coexisting hypercoagulable state).
Renal vein thrombosis treatment
Generally, renal vein thrombosis is considered as a result of an underlying kidney disease rather than its cause. Therapy is therefore directed at treatment of the underlying disorder most commonly nephrotic syndrome and supporting renal function.
Although no randomized trials exist to evaluate the role of anticoagulation therapy in asymptomatic renal vein thrombosis, anticoagulation therapy should be provided to prevent the risk of progression of thrombus or occurrence of an embolic event. Patients with symptomatic renal vein thrombosis (such as acute renal vein thrombosis) should be treated similarly to patients who have pulmonary embolism (PE) or deep venous thrombosis (DVT). Typically, initial treatment includes starting unfractionated or low-molecular-weight heparin and then bridged to warfarin, for a goal INR of 2 or 3. Direct thrombin inhibitors and factor Xa inhibitors have not been studied in nephrotic patients with renal vein thrombosis and are not recommended for anticoagulation. Patients with documented renal vein thrombosis and pulmonary embolism who have contraindications for anticoagulation can be effectively treated with suprarenal inferior vena cava filters. Anticoagulation is generally given for 6 to 12 months, though most recommendations are to continue as long as a patient remains nephrotic.
Systemic fibrinolysis carries a risk of significant life-threatening bleeding and is usually not recommended. Local thrombolytic therapy with or without catheter-directed thrombectomy in patients with acute renal vein thrombosis is associated with acute renal failure. Surgical thrombectomy can be rarely considered in the setting of acute bilateral renal vein thrombosis and acute renal failure especially if percutaneous thrombectomy and/or thrombolysis cannot be performed.
Renal vein thrombosis prognosis
Renal vein thrombosis prognosis is favorable with treatment. However, morbidity and mortality of renal vein thrombosis depend on its underlying cause. For example, in cases of renal vein thrombosis secondary to cancer, complications can arise from the malignancy itself or result in a thromboembolism at other sites such as DVT (deep venous thrombosis) or pulmonary embolism. Prognosis of renal vein thrombosis due to nephrotic syndrome as per a retrospective cohort study showed a 40% mortality at 6 months in 27 patients with renal vein thrombosis 17. Survivors appeared to have stable renal function and resolution of nephrotic syndrome. renal vein thrombosis that develops after a renal transplant has a poor prognosis and usually results in graft failure, particularly in the first month post-transplant 18.
References- Mazhar HR, Aeddula NR. Renal Vein Thrombosis. [Updated 2018 Dec 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536971
- Singhal R, Brimble KS. Thromboembolic complications in the nephrotic syndrome: pathophysiology and clinical management. Thromb. Res. 2006;118(3):397-407.
- Kuhlmann U, Steurer J, Bollinger A, Pouliadis G, Briner J, Siegenthaler W. [Incidence and clinical significance of thromboses and thrombo-embolic complications in nephrotic syndrome patients]. Schweiz Med Wochenschr. 1981 Jul 07;111(27-28):1034-40.
- Zigman A, Yazbeck S, Emil S, Nguyen L. Renal vein thrombosis: a 10-year review. J. Pediatr. Surg. 2000 Nov;35(11):1540-2.
- Winyard PJ, Bharucha T, De Bruyn R, Dillon MJ, van’t Hoff W, Trompeter RS, Liesner R, Wade A, Rees L. Perinatal renal venous thrombosis: presenting renal length predicts outcome. Arch. Dis. Child. Fetal Neonatal Ed. 2006 Jul;91(4):F273-8.
- Llach F. Thromboembolic complications in nephrotic syndrome. Coagulation abnormalities, renal vein thrombosis, and other conditions. Postgrad Med. 1984 Nov 01;76(6):111-4, 116-8, 121-3.
- Renal vein thrombosis. https://emedicine.medscape.com/article/460752-overview
- Harris SL, Smith MP, Laurie A, Darlow BA. Neonatal renal vein thrombosis and prothrombotic risk. Acta Paediatr. 2010 Jul. 99 (7):1104-7.
- Ross O, Pourmoussa A, Batech M, Sim JJ. Characteristics of patients diagnosed with renal vein thrombosis and glomerulopathy: a case series. Int Urol Nephrol. 2017 Feb;49(2):285-293.
- Aeddula NR, Baradhi KM. Sickle Cell Nephropathy. [Updated 2019 Jun 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526017
- Ljungberg B, Stenling R, Osterdahl B, Farrelly E, Aberg T, Roos G. Vein invasion in renal cell carcinoma: impact on metastatic behavior and survival. J. Urol. 1995 Nov;154(5):1681-4.
- The ultrasound appearances of neonatal renal vein thrombosis. J Hibbert, D C Howlett, K L Greenwood, L M MacDonald, and A J Saunders. The British Journal of Radiology 1997 70:839, 1191-1194
- CT Evaluation of Renovascular Disease. Akira Kawashima, Carl M. Sandler, Randy D. Ernst, Eric P. Tamm, Stanford M. Goldman, and Elliot K. Fishman. RadioGraphics 2000 20:5, 1321-1340
- El Zorkany K, Bridson JM, Sharma A, Halawa A. Transplant Renal Vein Thrombosis. Exp Clin Transplant. 2017 Apr;15(2):123-129.
- Ricci MA, Lloyd DA. Renal venous thrombosis in infants and children. Arch Surg. 1990 Sep;125(9):1195-9.
- Alvarez-Castells A, Sebastiá Cerqueda C, Quiroga Gómez S. [Computerized tomography angiography of the renal vessels]. Arch. Esp. Urol. 2001 Jul-Aug;54(6):603-15.
- Gauthier M, Canoui-Poitrine F, Guéry E, Desvaux D, Hue S, Canaud G, Stehle T, Lang P, Kofman T, Grimbert P, Matignon M. Anticardiolipin antibodies and 12-month graft function in kidney transplant recipients: a prognosis cohort survey. Nephrol. Dial. Transplant. 2018 Apr 01;33(4):709-716.
- Dimitroulis D, Bokos J, Zavos G, Nikiteas N, Karidis NP, Katsaronis P, Kostakis A. Vascular complications in renal transplantation: a single-center experience in 1367 renal transplantations and review of the literature. Transplant. Proc. 2009 Jun;41(5):1609-14.