What is retinal vein occlusion
Retinal vein occlusion is a blockage of the small veins that carry blood away from the retina. The retina is the layer of tissue at the back of the inner eye that converts light images to nerve signals and sends them to the brain. A retinal vein occlusion is one of the most common types of retinal vascular disease, second only to diabetic retinopathy 1. Retinal vein occlusions are classified based on location of the obstruction. For example, a branch retinal vein occlusion (BRVO) affects one of the branches of the central retinal vein, whereas a hemispheric retinal vein occlusion (HRVO) affects a trunk of the central retinal vein draining the superior or inferior retinal hemisphere. A central retinal vein occlusion (CRVO) occludes the central retinal vein proper.
Can retinal vein occlusion be cured?
Retinal vein occlusion cannot be cured. There is no way to reverse or open the blockage. Many people will regain vision, even without treatment. However, vision rarely returns to normal.
You may need treatment to prevent another blockage from forming in the same or the other eye.
- It’s important to manage diabetes, high blood pressure, and high cholesterol levels.
- Some people may need to take aspirin or other blood thinners.
Retinal vein occlusion causes
Retinal vein occlusion is most often caused by hardening of the arteries (atherosclerosis) and the formation of a blood clot.
Blockage of smaller veins (branch retinal vein occlusion or BRVO) in the retina often occurs in places where retinal arteries that have been thickened or hardened by atherosclerosis cross over and place pressure on a retinal vein.
Risk factors for retinal vein occlusion include:
- Atherosclerosis
- Diabetes
- High blood pressure (hypertension)
- Other eye conditions, such as glaucoma, macular edema, or vitreous hemorrhage
The risk of these disorders increases with age, therefore retinal vein occlusion most often affects older people.
Blockage of retinal veins may cause other eye problems, including:
- Glaucoma (high pressure in the eye), caused by new, abnormal blood vessels growing in the front part of the eye
- Macular edema, caused by the leakage of fluid in the retina
Retinal vein occlusion prevention
Retinal vein occlusion is a sign of a general blood vessel (vascular) disease. Measures used to prevent other blood vessel diseases may decrease the risk of retinal vein occlusion.
These measures include:
- Eating a low-fat diet
- Getting regular exercise
- Maintaining an ideal weight
- Not smoking
Aspirin or other blood thinners may help prevent blockages in the other eye.
Controlling diabetes may help prevent retinal vein occlusion.
Retinal vein occlusion symptoms
Retinal vein occlusion symptoms include sudden blurring or vision loss in all or part of one eye.
Retinal vein occlusion possible complications
Retinal vein occlusion complications may include:
- Glaucoma
- Partial or complete vision loss in the affected eye
Retinal vein occlusion diagnosis
Tests to evaluate for retinal vein occlusion include:
- Examination of the retina after dilating the pupil
- Fluorescein angiography
- Intraocular pressure
- Pupil reflex response
- Refraction eye exam
- Retinal photography
- Slit lamp examination
- Testing of side vision (visual field examination)
- Visual acuity test to determine the smallest letters you can read on a chart
Other tests may include:
- Blood tests for diabetes, high cholesterol, and triglyceride levels
- Blood tests to look for a clotting or blood thickening (hyperviscosity) problem (in people under age 40 years)
Your doctor will closely monitor any blockage for several months. It may take 3 or more months for harmful effects such as glaucoma to develop after the occlusion.
Retinal vein occlusion treatment
Many people will regain vision, even without treatment. However, vision rarely returns to normal. There is no way to reverse or open the blockage.
You may need treatment to prevent another blockage from forming in the same or the other eye.
- It’s important to manage diabetes, high blood pressure, and high cholesterol levels.
- Some people may need to take aspirin or other blood thinners.
Treatment for the complications of retinal vein occlusion may include:
- Focal laser treatment, if macular edema is present.
- Injections of anti-vascular endothelial growth factor (anti-VEGF) drugs into the eye. These drugs may block the growth of new blood vessels that can cause glaucoma. This treatment is still being studied.
- Laser treatment to prevent the growth of new, abnormal blood vessels that leads to glaucoma.
Medical therapy
Medical therapy can limit complications from retinal vein occlusions. Anti-VEGF intraocular injections can cause regression of iris neovascularization 2 and macular edema 3. In addition, the SCORE study demonstrated the benefit of triamcinolone acetonide for macular edema secondary to central retinal vein occlusions (vs. sham) 4, but did not demonstrate benefit for branch retinal vein occlusions (vs. focal laser) 5.
The mainstay of therapy is now anti-VEGF therapy for macular edema with either central retinal vein occlusion or branch retinal vein occlusion. Both ranibizumab (BRAVO and CRUISE) 6 and aflibercept (GALILEO/COPERNICUS; VIBRANT) 7 have been shown to be efficacious in the treatment of macular edema. Significant gains in visual acuity results and the retinal edema subsides with therapy. Both drugs are recommended to be used monthly for the 6 treatments and then as needed. Bevacizumab is also used off-label to treat macular edema.
Steroid implants, such as the dexamethasone (OZURDEX plant) implant 8 can also treat the macular edema and are best reserved as a second therapy or for eyes with chronic edema.
The SCORE2 Study compared aflibercept with bevacizumab for macular edema due to central retinal vein occlusion using a non-inferiority trial design. The primary endpoint was a 6 months. Bevacizumab was non-inferior to aflibercept with respect to visual acuity and optical coherence tomography (OCT) thickness 9. After 6 months, good responders were divided into monthly and treat and extend regimens using the original assigned drugs. No significant difference was seen between monthly and treat and extend for each drug. There were fewer treatments given for the treat and extend arms as compared to monthly 10. Poor responders at 6 months were assigned a different treatment: aflibercept eyes were assigned to dexamethasone implant and bevacizumab eyes were assigned to aflibercept. These results are not yet available.
Medical follow up
Ischemic retinal vein occlusions can cause iris or retinal neovascularization in addition to macular edema and should be observed with an undilated iris and angle examination followed by a dilated fundus examination on a period basis. central retinal vein occlusion eyes should be examined monthly for 6 months. The risk is highest for development of rubeosis within the first 90 days and decreases through 6 months. In general, fluorescein angiography should be delayed until retinal hemorrhages clear to allow for good visualization of the choriocapillaris.
Surgery
The Central Retinal Vein Occlusion Study supported panretinal photocoagulation for iris neovascularization after it occurs 11. It did not support grid photocoagulation for macular edema 12. The Branch Vein Occlusion Study supported the use of grid laser photocoagulation of edematous area 13. In addition, The Branch Vein Occlusion Study Group recommended sectoral panretinal photocoagulation for the development of retinal neovascularization 14.
Surgery complications
Complications associated with intravitreal injections include infection, bleeding, retinal detachment, cataract, and both infectious and sterile uveitis; however, these complicatations remain relatively rare. Triamcinolone acetonide can also cause a steroid-induced glaucoma.
Retinal vein occlusion prognosis
The outcome varies. People with retinal vein occlusion often regain useful vision.
It is important to properly manage conditions such as macular edema and glaucoma. However, having either of these complications is more likely to lead to a poor outcome.
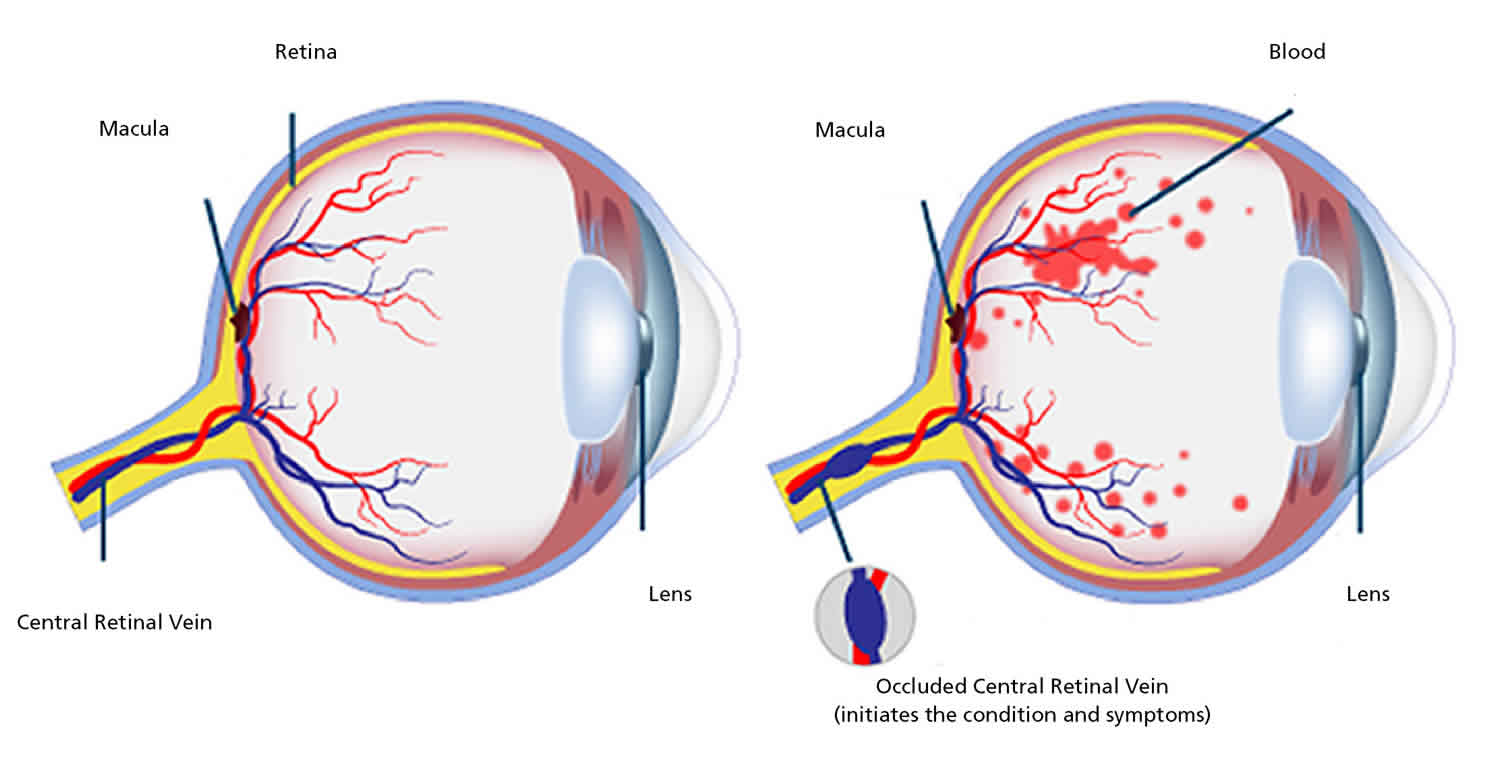
Central retinal vein occlusion
When the main retinal vein becomes blocked, it is called central retinal vein occlusion (CRVO). When the vein is blocked, blood and fluid spills out into the retina. The macula can swell from this fluid, affecting your central vision. Eventually, without blood circulation, nerve cells in the eye can die and you can lose more vision.
Central retinal vein occlusion (CRVO) is a common cause of marked or total loss of vision in the middle-aged and elderly population, but no age group is immune to it 15. Although central retinal vein occlusion (CRVO) has been known since 1878 and a large volume of literature has been published on the subject, its management is still ill-understood and controversial.
Studies 16 have showed that central retinal vein occlusion is actually of two types, with very different prognoses and management.
The two central retinal vein occlusion types are:
- Non-ischemic type or venous stasis retinopathy —a milder type characterized by leaky retinal vessels with macular edema. Non-ischemic central retinal vein occlusion can worsen and become ischemic, so when central retinal vein occlusion is diagnosed, monthly checkups are initially recommended. It’s important to note that early detection of macular edema or abnormal blood vessels is important; most patients can avoid severe vision loss if treatment is begun before substantial damage develops in the eye.
- Ischemic type or hemorrhagic retinopathy —a more severe type with closed-off small retinal blood vessels. Patients with ischemic central retinal vein occlusion have worse vision with less chance for improvement. They have a tendency for the eye to cause new blood vessels to grow and in the front of the eye, these new vessels can clog the outflow of normal eye fluids. The eye pressure goes up and glaucoma develops. In the back of the eye, new blood vessels may cause bleeding.
Classification of central retinal vein occlusion into non-ischemic and ischemic central retinal vein occlusion is essential because non-ischemic central retinal vein occlusion is a comparatively benign disease, with permanent central scotoma as the major complication from cystoid macular edema. This type of central retinal vein occlusion does not develop the most dreaded complication of ocular neovascularization. In contrast to that, ischemic central retinal vein occlusion is a seriously blinding disease, and anterior segment neovascularization leading to neovascular glaucoma is its major complication.
In a series of 620 consecutive central retinal vein occlusion cases, we have found that 81% of the patients have the non-ischemic type, and only 19% are ischemic type 16. That is the fortunate part of the condition: only one fifth of the patients suffer the serious type.
The first crucial step in the management of central retinal vein occlusion is to find out what type of central retinal vein occlusion an eye has because the prognosis, management and outcome of the two are totally different.
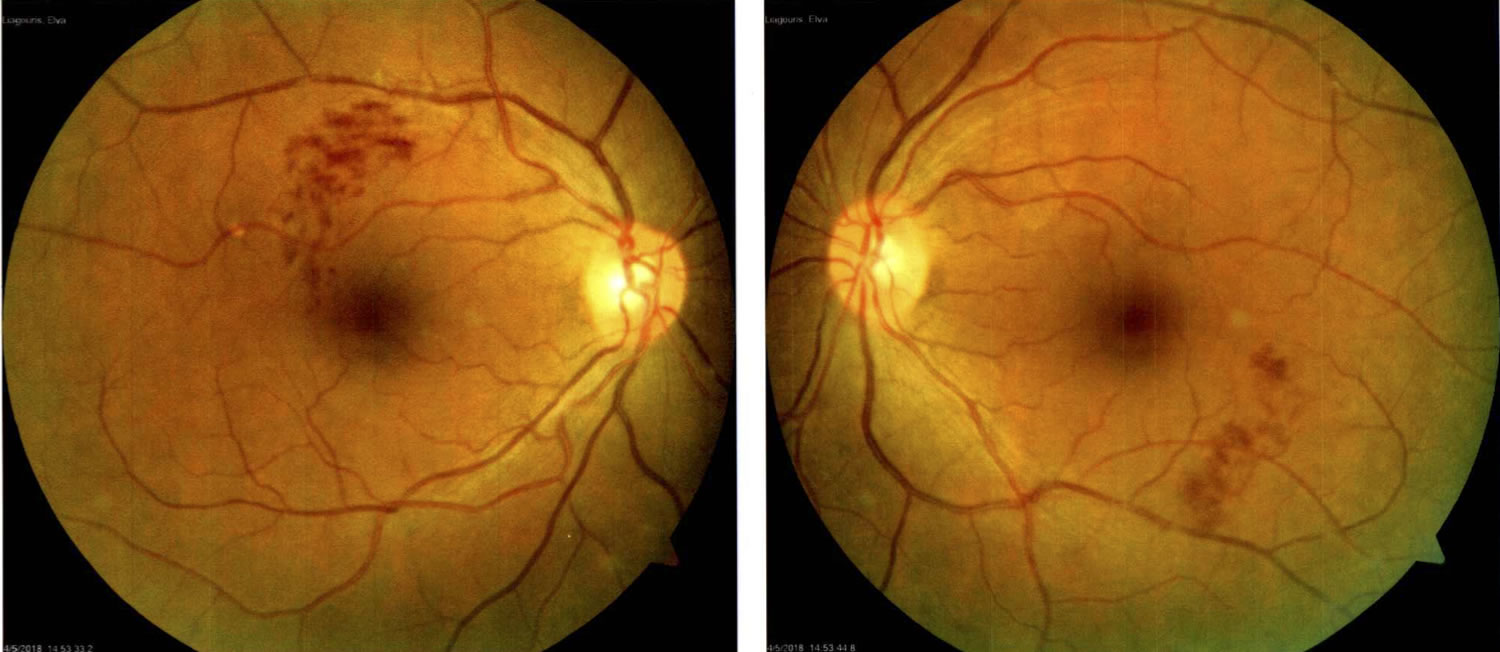
Figure 1. Central retinal vein occlusion (central retinal vein occlusion with Flame Hemorrhages)
What is the risk of the same thing happening to the other eye and how soon?
The cumulative chance of developing the same type of central retinal vein occlusion in the other eye (after the onset of first episode) is: for non-ischemic central retinal vein occlusion, 6.6% within 2 years, and for ischemic central retinal vein occlusion 5.6% at 2.8 years.
What is the risk of recurrence of the same thing in the same eye once the central retinal vein occlusion has resolved?
The cumulative chance of this for non-ischemic central retinal vein occlusion is 0.9% within 2.5 years from onset and 2.2% within 5 years.
What are the chances of a non-ischemic central retinal vein occlusion changing to ischemic central retinal vein occlusion, and after how long?
It is 9.4% within 6 months and 12.6% within 18 months from onset of non-ischemic central retinal vein occlusion. When this risk was categorized by age at onset of non-ischemic central retinal vein occlusion, the cumulative proportion of conversion in persons 65 or older was 13.2% at 6 months and 18.6% at 18 months, while in persons 45 to 64 years it was 6.7% and 8.1% respectively.
What is the age distribution at first onset of central retinal vein occlusion? Does central retinal vein occlusion occur in young persons? – and, if so, how frequently?
No age is immune to central retinal vein occlusion; I have seen patients as young as 14 years of age with central retinal vein occlusion. Ischemic central retinal vein occlusion develops significantly more often than non-ischemic central retinal vein occlusion in persons aged 65 years or older (ischemic: 67% vs. non-ischemic: 44%). However, 18% of non-ischemic central retinal vein occlusion and 7% of ischemic central retinal vein occlusion in our study were seen in persons under the age of 45 years.
Central retinal vein occlusion causes
Central retinal vein occlusion happens when a blood clot blocks the flow of blood through the retina’s main vein. Disease can make the walls of your veins more narrow, which can lead to central retinal vein occlusion.
Central retinal vein occlusion usually happens in people who are aged 50 and older.
People who have the following health problems have a greater risk of central retinal vein occlusion:
- high blood pressure
- diabetes
- glaucoma
- hardening of the arteries (called arteriosclerosis)
Most patients with central retinal vein occlusion develop it in one eye. And, although diabetes and high blood pressure are risk factors for central retinal vein occlusion, its specific cause is still unknown. What eye doctors (ophthalmologists) do know is that central retinal vein occlusion develops from a blood clot or reduced blood flow in the central retinal vein that drains the retina. And ophthalmologists have learned that a large number of conditions may increase the risk of blood clots. Some eye doctors advise testing for them. However, it is not certain how these health conditions are related to central retinal vein occlusion—and some of them, if diagnosed, have no agreed-to or necessary recommended treatment.
Many eye doctors do not advise testing for a central retinal vein occlusion in one eye, but do recommend a visit with a family doctor to be sure there is no diabetes or high blood pressure.
Central retinal vein occlusion that occurs in both eyes at the same time can be related to systemic disease; in these cases, a tendency toward abnormal blood clotting is definitely more common and medical testing to detect so-called “hypercoagulable states” is indicated. While some eye doctors coordinate such testing, most refer patients to their family doctors, internists, or hematologists (physicians specializing in diseases of the blood) for testing.
To lower your risk for central retinal vein occlusion, you should do the following:
- eat a low-fat diet
- get regular exercise
- maintain an ideal weight
- don’t smoke
Central retinal vein occlusion symptoms
The most common symptom of central retinal vein occlusion is vision loss or blurry vision in part or all of one eye. It can happen suddenly or become worse over several hours or days. Sometimes, you can lose all vision suddenly.
You may notice floaters. These are dark spots, lines or squiggles in your vision. These are shadows from tiny clumps of blood leaking into the vitreous from retinal vessels.
In some more severe cases of central retinal vein occlusion, you may feel pain and pressure in the affected eye.
Central retinal vein occlusion almost always happens only in one eye.
Mild central retinal vein occlusion may show no symptoms. However:
- Many patients with central retinal vein occlusion have symptoms such as blurry or distorted vision due to swelling of the center part of the retina, known as the macula.
- Some patients have mild symptoms that wax and wane, called transient visual obscurations.
- Patients with severe central retinal vein occlusion and secondary complications such as glaucoma (a disease characterized by increased pressure in the eye) often have pain, redness, irritation and other problems.
Central retinal vein occlusion diagnosis
Central retinal vein occlusion is typically a clinical diagnosis—that is, one based on medical signs and patient reported symptoms. Your ophthalmologist will widen (dilate) your pupils with eye drops and check your retina. Common conditions that can take on an appearance of central retinal vein occlusion include diabetic retinopathy (retina disease) and retinopathy related to low blood counts, such as anemia and thrombocytopenia (a deficiency of blood platelets).
Swelling of the center of the retina, called macular edema is common, and to detect this and measure the amount of swelling, an optical coherence tomography (OCT) image is often obtained. To help distinguish central retinal vein occlusion from conditions that may mimic it, and to assess closure of small blood vessels, or to search for or confirm growth of new abnormal vessels, fluorescein angiography imaging may be performed. Yellow dye (called fluorescein) is injected into a vein, usually in your arm. The dye travels through your blood vessels. A special camera takes photos of your retina as the dye travels throughout the vessels. This test shows if the retinal vein is blocked.
People under the age of 40 with central retinal vein occlusion may be tested to look for a problem with their blood clotting or thickening.
Central retinal vein occlusion treatment
The blocked vein in central retinal vein occlusion cannot be unblocked. The main goal of treatment is to keep your vision stable. This is usually done by sealing off any leaking blood vessels in the retina. This helps prevent further swelling of the macula.
In patients with central retinal vein occlusion, vascular endothelial growth factor (VEGF) is elevated; this leads to swelling as well as new vessels that are prone to bleeding. Your ophthalmologist may treat your central retinal vein occlusion with medication injections in the eye called “anti-VEGF injections.” The medicine can help reduce the swelling of the macula. Sometimes steroid medicine may be injected in the eye to help treat the swelling. Based on results from powerful randomized clinical trials, involves periodic injections into the eye of an anti-VEGF drug to reduce the new blood vessel growth and swelling. Anti-VEGF drugs include bevacizumab (Avastin®), ranibizumab (Lucentis®), and aflibercept (Eylea®).
Although anti-VEGF drugs reduce the swelling, they are not a cure. As the drug leaves the eye and moves into the bloodstream, the effect in the eye wears off, so re-injection is often needed. A rare lucky patient needs only one injection, but the norm is a series of periodic injections over the course of a few years.
If your central retinal vein occlusion is very severe, your ophthalmologist may do a form of laser surgery. This is called panretinal photocoagulation (PRP). A laser is used to make tiny burns to areas of the retina. This helps lower the chance of bleeding in the eye and keeps eye pressure from rising too much.
When there is ischemic central retinal vein occlusion with new vessels, anti-VEGF injections lead to prompt, but often temporary, control of the new vessels. Laser treatment tends to offer a more permanent effect. In some cases, both treatments are used.
It usually takes a few months after treatment before you notice your vision improving. While most people see some improvement in their vision, some people won’t have any improvement.
Central retinal vein occlusion prognosis
Central retinal vein occlusion has a better prognosis in young people. In older patients who receive no treatment, about one-third improve on their own, about one-third wax and wane and stay about the same, and about one-third get worse. If there is macular edema, it may improve on its own.
Branch retinal vein occlusion
When branches of the retinal vein become blocked, it is called branch retinal vein occlusion (BRVO). Branch retinal vein occlusion can be further classified as major or macular depending on the anatomical location. Major branch retinal vein occlusion refers to an occlusion of a retinal vein that drains one of the quadrants, and macular branch retinal vein occlusion refers to an occlusion of a venule within the macula. Venous obstruction may be sufficiently severe to cause non-perfusion and macular ischemia. Retinal vein occlusions can be further characterized as non-ischemic (i.e., perfused) or ischemic (i.e., non-perfused) depending on the status of retinal perfusion. Branch retinal vein occlusion is generally considered to be ischemic whenever there is an area of retinal capillary non-perfusion of five disc areas or greater on fluorescein angiography 17. Perfusion status has important implications in therapy and prognosis, as discussed below 17.
When the retinal vein is blocked, blood and fluid spills out into the retina. The macula can swell from this fluid, affecting your central vision. Eventually, without blood circulation, nerve cells in the eye can die and you can lose more vision.
The most common symptom of branch retinal vein occlusion is vision loss or blurry vision in part or all of one eye. It can happen suddenly or become worse over several hours or days. Sometimes, you can lose all vision suddenly.
Figure 2. Branch retinal vein occlusion
Branch retinal vein occlusion causes
Most branch retinal vein occlusions occur at an arteriovenous crossing, an intersection between a retinal artery and vein. These vessels share a common sheath (connective tissue), so when the artery loses flexibility, as with atherosclerosis (hardening of the arteries), the vein is compressed.
The narrowed vein experiences turbulent blood flow that promotes clotting, leading to a blockage or occlusion. This obstruction blocks blood drainage and may lead to fluid leakage in the center of vision (macular edema) and ischemia—poor perfusion (flow) in the blood vessels supplying the macula.
Branch retinal vein occlusion usually happens in people who are aged 50 and older.
People who have the following health problems have a greater risk of branch retinal vein occlusion:
- high blood pressure
- diabetes
- glaucoma
- hardening of the arteries (called arteriosclerosis)
- being overweight or obese (increased body mass index)
- cardiovascular (heart) disease
- in younger patients who suffer branch retinal vein occlusion, an abnormal tendency to develop blood clotting is also possible
To lower your risk for branch retinal vein occlusion, you should do the following:
- eat a low-fat diet
- get regular exercise
- maintain an ideal weight
- don’t smoke
Branch retinal vein occlusion symptoms
Branch retinal vein occlusion causes a sudden, painless loss of vision. If the affected area is not in the center of the eye, branch retinal vein occlusion can go unnoticed with no symptoms. In rare cases of an undetected vein occlusion, visual floaters from a vitreous hemorrhage (blood vessels leaking into the vitreous gel of the eye) can be the main symptom; this is caused by development of abnormal new blood vessels (neovascularization) in the retina.
You may notice floaters. These are dark spots, lines or squiggles in your vision. These are shadows from tiny clumps of blood leaking into the vitreous from retinal vessels.
Branch retinal vein occlusion almost always happens only in one eye.
Branch retinal vein occlusion complications
Retinal neovascularization is a potentially serious complication of branch retinal vein occlusion in which an inadequate blood supply (ischemia) causes abnormal new blood vessels to grow on the surface of the retina. This growth can further decrease vision by causing vitreous hemorrhage that causes floaters and loss of vision, retinal detachment, and glaucoma.
When neovascularization develops, scatter laser photocoagulation therapy is used to create burns in the area of the vein occlusion (blockage). The aim is to try to lower the oxygen demand of the retina and thus stop the abnormal blood vessels from growing. Patients receive an anesthetic to numb the eye and make the treatment more comfortable.
Scatter photocoagulation has been shown to reduce neovascularization-related complications from 60% to 30%. Because only a few patients develop abnormal new blood vessels in the retina, not many need scatter photocoagulation treatment.
Branch retinal vein occlusion diagnosis
Most often, branch retinal vein occlusion is diagnosed by an eye exam that shows retinal hemorrhage (blood vessels leaking into the retina), thickened and twisted blood vessels, and retinal edema (swelling with fluid). Your ophthalmologist will widen (dilate) your pupils with eye drops and check your retina.
Two types of retinal imaging tests aid the diagnosis of branch retinal vein occlusion:
- Fluorescein angiography: Yellow dye (called fluorescein) is injected into a vein, usually in your arm. The dye travels through your blood vessels. A special camera takes photos of your retina as the dye travels throughout the vessels. This test shows if any retinal blood vessels are blocked.
- Optical coherence tomography (OCT)
Fluorescein angiography provides images of fluid leaking from damaged or abnormal retinal vessels, demonstrating:
- Venous stasis (congestion and slowing of circulation)
- Edema (swelling with fluid)
- Ischemia (inadequate blood supply) or
- Retinal neovascularization (abnormal growth of new blood vessels in the retina)
Optical coherence tomography (OCT) provides detailed images of the central retina, allowing detection of macular edema and fluid outside the macula.
Fluorescein angiography is very valuable for detecting branch retinal vein occlusion and the flow of the blood vessels. Once branch retinal vein occlusion has been found, optical coherence tomography (OCT) is used to provide a better assessment of whether macular edema is present, and if so, how severe it is.
Also, your blood sugar and cholesterol levels may be tested.
People under the age of 40 with branch retinal vein occlusion may be tested to look for a problem with their blood clotting or thickening.
Branch retinal vein occlusion treatment
Branch retinal vein occlusion cannot be cured. Treatment begins with identifying underlying risk factors and treating them. Risk factors are assessed using several methods:
- Blood pressure monitoring
- Determining if blood cholesterol or lipid levels are elevated
- Blood tests, if appropriate, to determine if there is an abnormal tendency to form blood clots
Eye treatment is aimed at treating retinal complications and keeping your vision stable, rather than at trying to relieve the blockage itself. This is usually done by sealing off any leaking blood vessels in the retina. This helps prevent further swelling of the macula.
Macular edema, the main reason for visual loss from branch retinal vein occlusion, is often treated with intraocular (in-the-eye) injections of anti-VEGF drugs designed to stop the growth of abnormal new blood vessels in the eye and decrease leakage. Local anesthetic eye drops are given before the injections to numb the eye and minimize discomfort.
There are currently 3 anti-VEGF drugs:
- Avastin® (bevacizumab®)
- Lucentis® (ranibizumab®)
- Eylea® (aflibercept®)
In several large clinical studies, all 3 of these anti-VEGF drugs have demonstrated good results, with over 50% of patients enjoying significant visual improvement. The use of these drugs may require frequent retreatment, but injection schedules are determined on a case-by-case basis. Injections need to be given regularly for one to two years for the benefit to last.
Laser treatment called focal laser treatment may be used along with anti-VEGF therapy in hard-to-treat cases. A laser is used to make tiny burns to areas around the macula. This helps stop fluid from leaking from the vessels. Laser therapy for macular edema involves applying light laser pulses to the macula in a grid pattern. In a large multi-center clinical trial, after 3 years of follow up, this treatment showed improvement of vision in approximately two-thirds of patients.
Intraocular injections of steroids are another potential treatment for eyes that don’t respond to anti-VEGF drugs. A clinical trial that evaluated steroid treatment using a slow-releasing steroid implanted in the eye (dexamethasone or Ozurdex®), showed that approximately 30% of branch retinal vein occlusion patients enjoyed significant visual improvement following treatment.
It usually takes a few months before you notice your vision improving after treatment. While most people see some improvement in their vision, some people won’t have any improvement.
While intraocular steroids can have some side effects such as an increase in eye pressure and cataract progression, in most cases, these side effects can be controlled.
Overall, branch retinal vein occlusion carries a generally good prognosis. In fact, some branch retinal vein occlusion patients don’t require treatment at all, either because the blockage did not involve the macula, or because they have not experienced a decrease in vision. Over 60% of patients, treated and untreated, maintain vision better than 20/40 after 1 year.
References- Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol 1984;98(3):271-282.
- Ciftci S, Sakalar YB, Unlu K, et al. Intravitreal bevacizumab combined with panretinal photocoagulation in the treatment of open angle neovascular glaucoma. European Journal of Ophthalmology. 19(6):1028-33, 2009.
- Spaide RF, Chang LK, Klancnik JM, et al. Prospective study of intravitreal ranibizumab as a treatment for decreased visual acuity secondary to central retinal vein occlusion. American Journal of Ophthalmology. 147(2):298-306, 2009.
- Ip MS, Scott IU, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 5. Archives of Ophthalmology. 127(9):1101-14, 2009.
- Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Archives of Ophthalmology. 127(9):1115-28, 2009.
- Varma R, Bressler NM, Suñer I, Lee P, Dolan CM, Ward J, Colman S, Rubio RG; BRAVO and CRUISE Study Groups. Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the BRAVO and CRUISE trials. Ophthalmology. 2012 Oct;119(10):2108-18.
- Campochiaro PA, Clark WL, Boyer DS, Heier JS, Brown DM, Vitti R, Kazmi H, Berliner AJ, Erickson K, Chu KW, Soo Y, Cheng Y, Haller JA. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: the 24-week results of the VIBRANT study. Ophthalmology. 2015 Mar;122(3):538-44
- Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li XY, Whitcup SM; Ozurdex GENEVA Study Group, Li J. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011 Dec;118(12):2453-60.
- Scott IU, VanVeldhuisen PC, Ip MS, Blodi BA, Oden NL, Awh CC, Kunimoto DY, Marcus DM, Wroblewski JJ, King J; SCORE2 Investigator Group. Effect of Bevacizumab vs Aflibercept on Visual Acuity Among Patients With Macular Edema Due to Central Retinal Vein Occlusion: The SCORE2 Randomized Clinical Trial JAMA 2017;317(20):2072-2087
- Scott IU, VanVeldhuisen PC, Ip MS, Blodi BA, Oden NL, Altaweel M, Berinstein DM; SCORE2 Investigator Group. Comparison of Monthly vs Treat-and-Extend Regimens for Individuals With Macular Edema Who Respond Well to Anti–Vascular Endothelial Growth Factor Medications Secondary Outcomes From the SCORE2 Randomized Clinical Trial. JAMA Ophthalmol. 2018;136(4):337-345
- The Central Vein Occlusion Study Group: A randomized clinical trial of early panretinal photocoagulation for ischemic central vein occlusion: the CVOS Group N Report, Ophthlamology 102:1434-44, 1995.
- The Central Vein Occlusion Study Group: Evaluation of grid-pattern photocoagulation for macular edema in central vein occlusion: the CVOS Group M Report. Ophthalmology 102:1425-33, 1995.
- Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. American Journal of Ophthalmology. 98:271-82, 1984.
- Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. Archives of Ophthalmology. 104:34-41, 1986.
- Central Retinal Vein Occlusion. https://webeye.ophth.uiowa.edu/eyeforum/article/CRVO/index.htm
- Hayreh SS, Zimmerman MB, Podhajsky P: Incidence of various types of retinal vein occlusion and their recurrent and demographic characteristics. Amer J Ophthalmol 1994;117:429-41.
- Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol 1986;104(1):34-41.