What is the rhythm method
The rhythm method is also called the calendar method or the calendar rhythm method, is a form of natural family planning. Rhythm method of birth control means not using a type of birth control but instead avoiding sex and/or using birth control only on the days when you are most fertile (most likely to get pregnant). An ovulation home test kit or a fertility monitor can help you find your most fertile days.
To use the rhythm method, you track your menstrual history to predict when you’ll ovulate. This helps you determine when you’re most likely to conceive. You may want to use an ovulation calendar (https://www.marchofdimes.org/pregnancy/ovulation-calendar.aspx) to help you figure out when you ovulate. If you’re preventing pregnancy, don’t have unprotected sex.
If you’re hoping to get pregnant, you can use the rhythm method to determine the best days to have sex. Similarly, if you’re hoping to avoid pregnancy, you can use the rhythm method to determine which days to avoid unprotected sex.
Using the rhythm method for birth control requires careful record keeping and persistence. If you don’t want to conceive, you and your partner must avoid having sex or use a barrier method of contraception during your fertile days each month.
The rhythm method can be used as a way to promote fertility or as a method of contraception, by helping you determine the best days to have or avoid unprotected sex. Some women choose to use the rhythm method if a complex medical history limits traditional birth control options, or for religious reasons.
The rhythm method has no side effects. It doesn’t protect you from STIs (sexually transmitted infections), and it doesn’t prevent pregnancy as well as other kinds of birth control. Each year, about 24 in 100 women (24 percent) who use the rhythm method contraception get pregnant.
If your periods are irregular (the number of days apart varies from month to month), it may be hard to figure out when you ovulate. You can get pregnant up to 5 days before and the day of ovulation. So if you’re preventing pregnancy with natural family planning, don’t have unprotected sex on these days.
How does the rhythm method work?
Tracking your menstrual history doesn’t require special preparation. However, if you want to use the rhythm method for birth control, talk to your health care provider first if:
- You recently had your first period
- You just had a baby
- You’ve recently stopped taking birth control pills or other hormone contraceptives
- You’re breast-feeding
- You’re approaching menopause
- You have irregular menstrual cycles
Rhythm method safe days
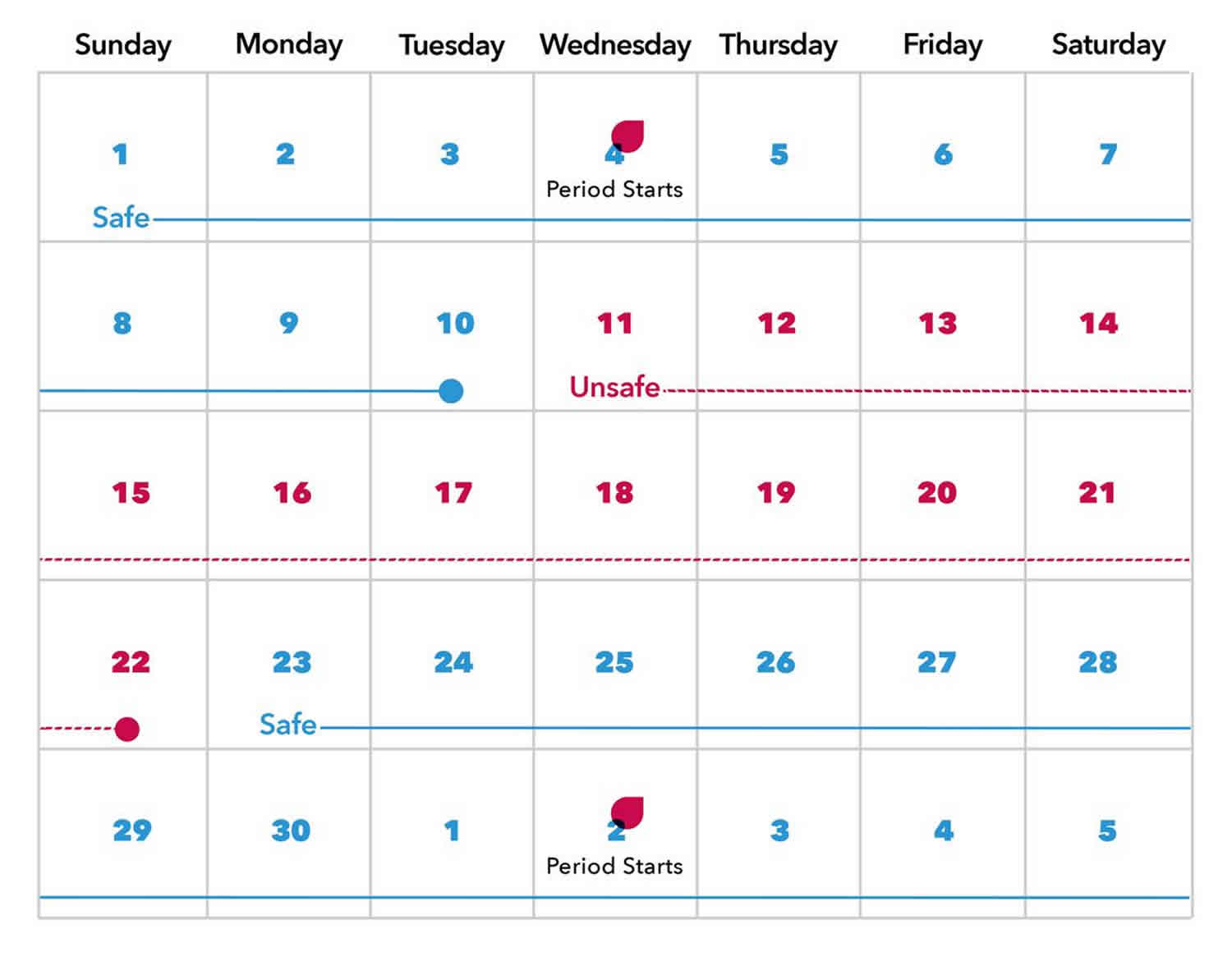
- Record the length of 6 to 12 of your menstrual cycles. Using a calendar, write down the number of days in each menstrual cycle — counting from the first day of your period to the first day of your next period.
- Determine the length of your shortest menstrual cycle. Subtract 18 from the total number of days in your shortest cycle. This number represents the first fertile day of your cycle. For example, if your shortest cycle is 26 days long, subtract 18 from 26 — which equals 8. In this example, the first day of your cycle is the first day of menstrual bleeding and the eighth day of your cycle is the first fertile day.
- Determine the length of your longest menstrual cycle. Subtract 11 from the total number of days in your longest cycle. This number represents the last fertile day of your cycle. For example, if your longest cycle is 32 days long, subtract 11 from 32 — which equals 21. In this example, the first day of your cycle is the first day of menstrual bleeding and the 21st day of your cycle is the last fertile day.
- Plan sex carefully during fertile days. If you’re hoping to avoid pregnancy, unprotected sex is off-limits during your fertile days — every month. On the other hand, if you’re hoping to get pregnant, have sex regularly during your fertile days.
- Update your calculations every month. Continue recording the length of your menstrual cycles to make sure you’re properly determining your fertile days.
Keep in mind that many factors, including medications, stress and illness, can affect the exact timing of ovulation. Using the rhythm method to predict ovulation can be inaccurate, especially if your cycle is irregular.
Fertility awareness: The menstrual cycle
Being aware of your menstrual cycle and the changes in your body that happen during this time can help you know when you are most likely to get pregnant. See how the menstrual cycle works.
The average menstrual cycle lasts 28 days. But normal cycles can vary from 21 to 35 days. The amount of time before ovulation occurs is different in every woman and even can be different from month to month in the same woman, varying from 13 to 20 days long. Learning about this part of the cycle is important because it is when ovulation and pregnancy can occur. After ovulation, every woman (unless she has a health problem that affects her periods or becomes pregnant) will have a period within 14 to 16 days.
Charting your fertility pattern
Knowing when you’re most fertile will help you plan pregnancy. There are three ways you can keep track of your fertile times. To most accurately track your fertility, use a combination of all three methods. This is called the symptothermal method. You can also purchase over-the-counter ovulation kits or fertility monitors to help find the best time to conceive. These kits work by detecting surges in a specific hormone called luteinizing hormone, which triggers ovulation.
Basal body temperature method
Basal body temperature is your temperature at rest as soon as you awake in the morning. A woman’s basal body temperature rises slightly with ovulation. So by recording this temperature daily for several months, you’ll be able to predict your most fertile days.
Basal body temperature differs slightly from woman to woman. Anywhere from 96 to 98 degrees Fahrenheit orally is average before ovulation. After ovulation most women have an oral temperature between 97 and 99 degrees Fahrenheit. The rise in temperature can be a sudden jump or a gradual climb over a few days.
Usually a woman’s basal body temperature rises by only 0.4 to 0.8 degrees Fahrenheit. To detect this tiny change, women must use a basal body thermometer. These thermometers are very sensitive. Most pharmacies sell them for about $10.
The rise in temperature doesn’t show exactly when the egg is released. But almost all women have ovulated within three days after their temperatures spike. Body temperature stays at the higher level until your period starts.
You are most fertile and most likely to get pregnant:
- Two to three days before your temperature hits the highest point (ovulation)
and - 12 to 24 hours after ovulation
A man’s sperm can live for up to three days in a woman’s body. The sperm can fertilize an egg at any point during that time. So if you have unprotected sex a few days before ovulation, you could get pregnant.
Many things can affect basal body temperature. For your chart to be useful, make sure to take your temperature every morning at about the same time. Things that can alter your temperature include:
- Drinking alcohol the night before
- Smoking cigarettes the night before
- Getting a poor night’s sleep
- Having a fever
- Doing anything in the morning before you take your temperature — including going to the bathroom and talking on the phone
Calendar method
This involves recording your menstrual cycle on a calendar for eight to 12 months. The first day of your period is Day 1. Circle Day 1 on the calendar. The length of your cycle may vary from month to month. So write down the total number of days it lasts each time. Using this record, you can find the days you are most fertile in the months ahead:
- To find out the first day when you are most fertile, subtract 18 from the total number of days in your shortest cycle. Take this new number and count ahead that many days from the first day of your next period. Draw an X through this date on your calendar. The X marks the first day you’re likely to be fertile.
- To find out the last day when you are most fertile, subtract 11 from the total number of days in your longest cycle. Take this new number and count ahead that many days from the first day of your next period. Draw an X through this date on your calendar. The time between the two Xs is your most fertile window.
This method always should be used along with other fertility awareness methods, especially if your cycles are not always the same length.
Cervical mucus method (also known as the ovulation method)
This involves being aware of the changes in your cervical mucus throughout the month. The hormones that control the menstrual cycle also change the kind and amount of mucus you have before and during ovulation. Right after your period, there are usually a few days when there is no mucus present or “dry days.” As the egg starts to mature, mucus increases in the vagina, appears at the vaginal opening, and is white or yellow and cloudy and sticky. The greatest amount of mucus appears just before ovulation. During these “wet days” it becomes clear and slippery, like raw egg whites. Sometimes it can be stretched apart. This is when you are most fertile. About four days after the wet days begin the mucus changes again. There will be much less and it becomes sticky and cloudy. You might have a few more dry days before your period returns. Describe changes in your mucus on a calendar. Label the days, “Sticky,” “Dry,” or “Wet.” You are most fertile at the first sign of wetness after your period or a day or two before wetness begins.
The cervical mucus method is less reliable for some women. Women who are breastfeeding, taking hormonal birth control (like the pill), using feminine hygiene products, have vaginitis or sexually transmitted infections (STIs), or have had surgery on the cervix should not rely on this method.
Rhythm method effectiveness
The rhythm method is an inexpensive and safe way to help you chart your fertility — the time of month when you’re most likely to be able to get pregnant.
Using the rhythm method as a form of birth control doesn’t pose any direct risks. However, it’s considered one of the least effective forms of birth control. How well the rhythm method works varies between couples. In general, as many as 24 out of 100 women who use natural family planning for birth control become pregnant the first year. Also, the rhythm method doesn’t protect you from sexually transmitted infections.
Table 1. Types of birth control comparison chart
| Method | Number of pregnancies per 100 women within their first year of typical use1 | Side effects and risks* *These are not all of the possible side effects and risks. Talk to your doctor or nurse for more information. | How often you have to take or use |
|---|---|---|---|
| Abstinence (no sexual contact) | Unknown (0 for perfect use) | No medical side effects | No action required, but it does take willpower. You may want to have a back-up birth control method, such as condoms. |
| Permanent sterilization surgery for women (tubal ligation, “getting your tubes tied”) | Less than 1 |
| No action required after surgery |
| Permanent sterilization implant for women (Essure®) The Essure® birth control device will no longer be sold or distributed in the United States after December 31, 2018. | Less than 1 |
| No action required after surgery |
| Permanent sterilization surgery for men (vasectomy) | Less than 1 |
| No action required after surgery |
| Implantable rod (Implanon®, Nexplanon®) | Less than 1 |
| No action required for up to 3 years before removing or replacing |
| Copper intrauterine device (IUD) (ParaGard®) | Less than 1 |
| No action required for up to 10 years before removing or replacing |
| Hormonal intrauterine devices (IUDs) (Liletta, Mirena®, and Skyla®) | Less than 1 |
| No action required for 3 to 5 years, depending on the brand, before removing or replacing |
| Shot/injection (Depo-Provera®) | 6 |
| Get a new shot every 3 months |
| Oral contraceptives, combination hormones (“the pill”) | 9 |
| Take at the same time every day |
| Oral contraceptives, progestin-only pill (“mini-pill”) | 9 |
| Take at the same time every day |
| Skin patch (Xulane®) | 9 May be less effective in women weighing 198 pounds or more2 |
| Wear for 21 days, remove for 7 days, replace with a new patch |
| Vaginal ring (NuvaRing®) | 9 |
| Wear for 21 days, remove for 7 days, replace with a new ring |
| Diaphragm with spermicide (Koromex®, Ortho-Diaphragm®) | 12 If you gain or lose than 15 pounds, or have a baby, have your doctor check you to make sure the diaphragm still fits. |
| Insert each time you have sex |
| Sponge with spermicide (Today Sponge®) | 12 (among women who have never given birth before) or 24 (among women who have given birth)3 |
| Insert each time you have sex |
| Cervical cap with spermicide (FemCap®) | 233 |
| Insert each time you have sex |
| Male condom | 18 |
| Use each time you have sex |
| Female condom | 21 |
| Use each time you have sex |
| Withdrawal — when a man takes his penis out of a woman’s vagina (or “pulls out”) before he ejaculates (has an orgasm or “comes”) | 22 |
| Use each time you have sex |
| Natural family planning (rhythm method) | 24 |
| Depending on method used, takes planning each month |
| Spermicide alone | 28 Works best if used along with a barrier method, such as a diaphragm |
| Use each time you have sex |