Rickettsialpox
Rickettsialpox also known as Kew Gardens spotted fever or vesicular rickettsiosis, is an illness caused by Rickettsia akari bacteria. Rickettsialpox is characterized by fever, headache, papulovesicular rash over the trunk and extremities, and in 80% of cases, appearance of an eschar (dark scab) (see Figure 6). Rickettsia akari is an obligate intracellular gram-negative coccobacillus 1. Rickettsialpox Rickettsia akari is commonly transmitted by the bite of the infected house-mouse mite, Liponyssoides sanguineus (see Figure 1). In Greek, akari means mite, hence the name. Human cases of rickettsialpox, as well as infected house-mouse mites and potential reservoirs of Rickettsia akari, have been found in several countries, including the United States, Turkey, Croatia, and Ukraine (mainly in urban locations) and often arises after the extermination of infected rodents as the mites seek new hosts 2. Rickettsialpox is typically asymptomatic or mild, with a sparse papulovesicular rash. However, central nervous system features have been reported, such as a stiff neck and photophobia.
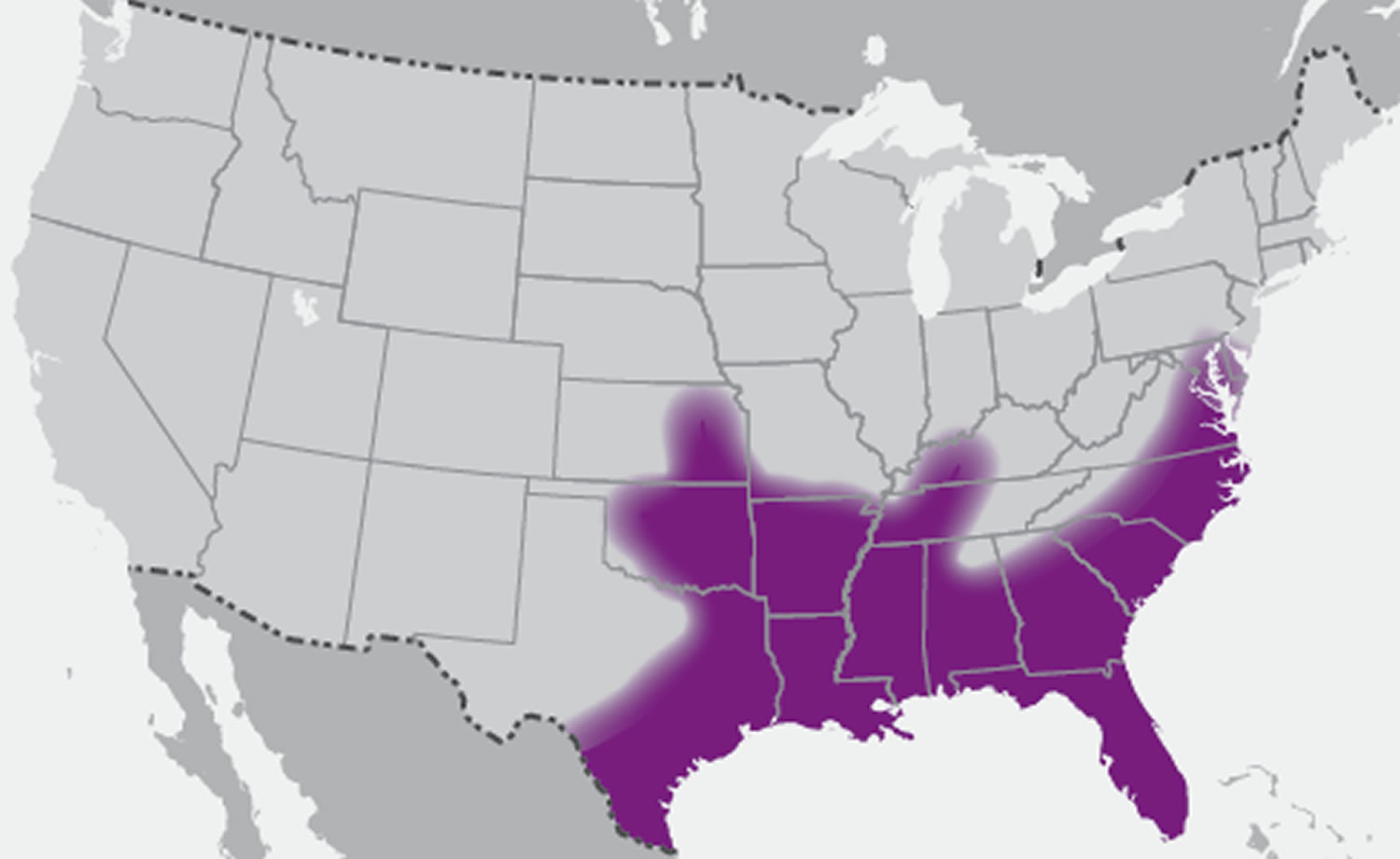
During 2004–2015, at least 40 patients with Rickettsialpox (Rickettsia parkeri rickettsiosis) were identified from 10 states 3. The median age of patients from case reports was 53 years (range: 23–83 years) 4; Rickettsialpox (Rickettsia parkeri rickettsiosis) has not been documented in children, and no fatal cases have been reported 3. Rickettsia parkeri is also transmitted by the Gulf Coast tick, Amblyomma maculatum (Figure 2). The geographic range of A. maculatum extends across the southern United States from Texas to South Carolina and as far north as Kansas, Maryland, Oklahoma, and Virginia (Figure 3). The Gulf Coast tick is typically found in prairie grassland and coastal upland habitats 5. Rickettsialpox (Rickettsia parkeri rickettsiosis) cases have been documented during April–October, with most cases occurring during July–September 3.
The mortality risk with Rickettsialpox is very low. Rickettsialpox is a benign, self-limiting disease that usually resolves within 14–21 days; no deaths from rickettsialpox have been reported 2. However, the severity of the clinical features could have caused death had the correct treatment not been instituted promptly. Although hemorrhages have not been described for rickettsialpox, dissimilarities in the clinical features of rickettsial disease among countries have been reported 6. Organ infections caused by increased vascular permeability have been described in rickettsial infections with different degrees of severity. Rickettsialpox has even been associated with hepatitis, a not well-documented complication of rickettsialpox 7.
Figure 1. Rickettsialpox tick (house-mouse mite)
[Source 8 ]Figure 2. Gulf Coast tick (Amblyomma maculatum)
[Source 3. ]Figure 3. U.S. distribution of Gulf Coast tick (Amblyomma maculatum)
[Source 3. ]Figure 4. Rickettsialpox rash
[Source 9 ]Figure 5. Rickettsialpox rash closeup view
[Source 9 ]Figure 6. Rickettsialpox eschar (site of bite of the house-mouse mite, Liponyssoides sanguineus)
[Source 9 ]Rickettsialpox transmission
Rickettsialpox Rickettsia akari bacteria is transmitted among house mice (Mus musculus) and other rodents and to humans by the house mouse colorless mite (Liponyssoides sanguineus) 10. These hosts serve as the reservoir for the Rickettsialpox disease. A house mouse colorless mite (Liponyssoides sanguineus) will bite humans when mice hosts are scarce. About 7-10 days after the painless bite, a papular skin lesion appears at the bite location and becomes vesicular with a surrounding area of erythema. An eschar forms and slowly heals. About 3-7 days after the initial skin lesion develops, patients may suddenly develop high-grade fever, chills, headaches, and myalgias with subsequent development of a sparse generalized papulovesicular rash. No human-to-human transmission occurs.
Rickettsialpox disease in humans was first described in 1946 in residents of apartments clustered in a three-block area in the borough of Queens, New York City 11. Subsequently, small outbreaks of rickettsialpox were recognized in several U.S. cities, including Boston, Cleveland, Philadelphia, Pittsburgh, and West Hartford 12. Most cases to date have occurred in large metropolitan areas of the northeastern United States; about half the described cases have occurred in New York City. However, rickettsialpox is likely more common in the United States than suggested by the relatively small number of reported cases during the past 50 years 13.
Recently, cases of rickettsialpox have been reported in residents of the Ukraine 14 and Croatia 15. Isolations have also been made from Korean voles in an area where rickettsialpox has not been reported 16. These data suggest that silent sylvan cycles of Rickettsia akari infection exist and that the organism is more widely distributed than currently appreciated.
Rickettsialpox symptoms
Rickettsialpox is an illness characterized by acute febrile illnesses often accompanied by headache, myalgia, and papulovesicular rash over the trunk and extremities, and, in 80% of cases, appearance of an ulcerated, necrotic region at the site of mite attachment, called eschar (see Figure 6). Eschars often appear before the onset of fever and can be non-tender or mildly tender.
Rickettsialpox disease begins at the site of the mite bite as a painless, firm, red lump (nodule) 17. The nodule develops into a fluid-filled blister that bursts and crusts over. This lump may be up to 1 inch (2.5 centimeters) wide. These lumps usually appear on the face, trunk, arms, and legs. They do not appear on the palms of hands and soles of feet. Symptoms usually develop 6 to 15 days after coming in contact with the bacteria.
Rickettsialpox disease other symptoms may include 17:
- Discomfort in bright light (photophobia)
- Fever and chills
- Headache
- Muscle pain
- Rash that looks like chickenpox
- Sweating
- Runny nose
- Sore throat
- Cough
- Enlarged lymph nodes
- Loss of appetite
- Nausea or vomiting
The rash is not painful and usually clears within a week.
Rickettsialpox diagnosis
Your health care provider will do an examination to look for a rash similar to the one in chickenpox.
If rickettsialpox is suspected, these tests will likely be done:
- Complete blood count (CBC). Routine laboratory test results are nonspecific for rickettsialpox, but leukopenia with relative lymphocytosis and mild proteinuria are common. Thrombocytopenia is also a frequently reported finding.
- Tests of blood serum (serologic studies)
- Swabbing and culture of the rash
A diagnosis of rickettsialpox is usually confirmed with a combination of clinical, epidemiological, and serological testing. In the presence of compatible illness in the context of mite exposure, perform serologic tests for antibodies to the spotted-fever group of rickettsiae. If possible, send a biopsy specimen for direct fluorescent antibody (DFA) testing, culture, and polymerase chain reaction (PCR). Sensitivity of the direct fluorescent antibody (DFA) is better for the eschar site than for secondary papulovesicular lesions.
The most common method of diagnosis of Rickettsia akari infections in clinical practice is to detect a four-fold rise in the convalescent titers of complement fixation or indirect fluorescent antibodies using spotted fever group antigens as Rickettsia akari is linked genetically to the potted fever group of Rickettsiae 18. These tests are available through the Centers for Disease Control and Prevention (CDC).
Organism culture, immunohistochemical staining, protein gel electrophoresis, and molecular analysis via polymerase chain reaction (PCR) may be performed, usually at the reference laboratory level 19. A newer multiplex real-time PCR of skin biopsy specimens has been shown to yield higher sensitivity in the diagnosis of rickettsialpox 20.
Giemsa stains of tissue specimens may reveal extremely small coccobacillary intracellular bacteria.
Weil-Felix test findings are negative.
If acute titer results are negative, obtain convalescent sera after 6-8 weeks.
Rickettsialpox treatment
Doxycycline is the treatment of choice for all suspected rickettsial infections, including rickettsialpox 21. Doxycycline treatment is most effective at preventing death and severe illness when doxycycline is started within the first 5 days of symptoms.
Treatment with antibiotics shortens the duration of symptoms usually to 24 to 48 hours.
Without treatment, the disease resolves itself within 7 to 10 days.
Treatment duration
When a patient is treated within the first 5 days of illness, fever generally subsides within 24-48 hours. In fact, failure to respond to doxycycline suggests that the patient’s condition might not be caused by rickettsial infection. Severely ill patients may require longer periods before their fever resolves, especially if they have experienced damage to organ systems. Resistance to doxycycline or relapses in symptoms after the completion of the recommended course of treatment have not been documented.
Recommended treatment and dosage for rickettsialpox
Doxycycline is the first line treatment for adults and children of all ages:
- Adults: 100 mg every 12 hours
- Children under 45 kg (100 lbs): 2.2 mg/kg body weight given twice a day
Patients should be treated for at least 3 days after the fever subsides and until there is evidence of clinical improvement. Minimum total course of 5–7 days for uncomplicated cases.
Treating children
The use of doxycycline to treat suspected rickettsial disease in children is standard practice recommended by both the Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics Committee on Infectious Diseases 3. Use of antibiotics other than doxycycline increases the risk of severe illness and patient death in cases of Rocky Mountain spotted fever. In a recent study, experts at the CDC and the Indian Health Service found that short courses of doxycycline do not result in staining of permanent teeth or enamel hypoplasia. Use doxycycline as the first-line treatment for suspected spotted fever rickettsioses in patients of all ages 3.
Antibiotics as prophylaxis
Post-tick bite antibiotic prophylaxis is not recommended to prevent rickettsial infection. Persons who experience a tick bite should watch for symptoms suggestive of tickborne illness and consult a health care provider if fever, rash, eschar, or other symptoms develop within 2 weeks of tick bite 3.
Rickettsialpox prognosis
Prognosis is excellent.
Rickettsialpox is usually a self-limited disease.
No fatalities have been reported.
References- Rickettsialpox. https://emedicine.medscape.com/article/227956-overview
- Zavala-Castro, J. E., Zavala-Velázquez, J. E., Peniche-Lara, G. F., & Uicab, J. E. (2009). Human Rickettsialpox, Southeastern Mexico. Emerging Infectious Diseases, 15(10), 1665-1667. https://dx.doi.org/10.3201/eid1510.081507
- Biggs HM, Behravesh CB, Bradley KK, et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis — United States. MMWR Recomm Rep 2016;65(No. RR-2):1–44. https://www.cdc.gov/mmwr/volumes/65/rr/rr6502a1.htm
- Paddock CD, Goddard J. The evolving medical and veterinary importance of the Gulf Coast tick (Acari: Ixodidae). J Med Entomol 2015;52:230–52
- Teel PD, Ketchum HR, Mock DE, Wright RE, Strey OF. The Gulf Coast tick: a review of the life history, ecology, distribution, and emergence as an arthropod of medical and veterinary importance. J Med Entomol 2010;47:707–22.
- Galvao MA, Mafra CL, Chamone Ch B, Calic SB, Zavala-Velázquez JE, Walker DH. Clinical and laboratorial evidence of Rickettsia felis infections in Latin America. Rev Soc Bras Med Trop. 2004;37:238–40.
- Madison G, Kim-Schluger L, Braverman S, Nicholson WL, Wormser GP. Hepatitis in association with rickettsialpox. Vector Borne Zoonotic Dis. 2008;8:111–5.
- Rahdar, Mahmoud & Vazirianzadeh, Babak & Rointan, Elham & Amraei, Kamyar. (2015). Identification of collected ectoparasites of rodents in the west of Khuzestan Province (Ahvaz and Hovizeh), southwest of Iran. Asian Pacific Journal of Tropical Disease. 5. 627-631. 10.1016/S2222-1808(15)60902-1.
- Krusell A, Comer JA, Sexton DJ. Rickettsialpox in North Carolina: a case report. Emerg Infect Dis. 2002;8(7):727–728. doi:10.3201/eid0807.010501 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2730333
- Lackman DB A review of information on rickettsialpox in the United States. Clin Pediatr. 1963;2:296–301 10.1177/000992286300200602
- Greenberg M, Pellitteri OJ, Jellison WL Rickettsialpox—a newly recognized rickettsial disease. III. Epidemiology. Am J Public Health. 1947;37:860–8 10.2105/AJPH.37.7.860
- Lackman DB A review of information on rickettsialpox in the United States. Clin Pediatr. 1963;2:296–301 10.1177/000992286300200602
- Kass EM, Szaniawski WK, Levy H, Leach J, Srinivasan K, Rives C Rickettsialpox in a New York City hospital, 1980 to 1989. N Engl J Med. 1994;331:1612–7 10.1056/NEJM199412153312403
- Eremeeva M, Balayeva N, Ignatovich V, Raoult D Genomic study of Rickettsia akari by pulsed-field gel electrophoresis. J Clin Microbiol. 1995;33:3022–4
- Radulovic S, Feng H-m, Morovic M, Djelalija B, Popov V, Crocquet-Valdes P, et al. Isolation of Rickettsia akari from a patient in a region where Mediterranean spotted fever is endemic. Clin Infect Dis. 1996;22:216–20
- Jackson EB, Danauskas JX, Coale MC, Smadel JE Recovery of Rickettsia akari from the Korean vole Microtus fortis pelliceus. Am J Hyg. 1957;66:301–8
- Rickettsialpox. https://medlineplus.gov/ency/article/001351.htm
- Akram SM, Jamil RT, Gossman WG. Rickettsia Akari (Rickettsialpox) [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448081
- Trout Fryxell RT, Steelman CD, Szalanski AL, Billingsley PM, Williamson PC. Molecular Detection of Rickettsia Species Within Ticks (Acari: Ixodidae) Collected from Arkansas United States. J Med Entomol. 2015 May. 52 (3):500-8.
- Denison AM, Amin BD, Nicholson WL, Paddock CD. Detection of Rickettsia rickettsii, Rickettsia parkeri, and Rickettsia akari in skin biopsy specimens using a multiplex real-time polymerase chain reaction assay. Clin Infect Dis. 2014 Sep 1. 59 (5):635-42.
- Other Spotted Fever Group Rickettsioses. Information for Health Care Providers. https://www.cdc.gov/otherspottedfever/healthcare-providers/