Rolando fracture
Rolando fracture is a three-part or comminuted intra-articular fracture-dislocation of the base of the thumb (proximal first metacarpal) 1. Rolando fracture can be thought of as a comminuted Bennett fracture. The mechanism is usually an axial blow to a partially flexed metacarpal, such as a fistfight. The fracture line is typically T- or Y-shaped. The volar fragment remains attached to the carpometacarpal joint, while the main dorsal fragment subluxes or dislocates dorsally and radially due to the unopposed pull of abductor pollicis longus. Rolando fracture initially was described in 1910 in a series of 12 metacarpal base fractures, of which three involved a Y-shaped split of the joint surface 2. The fracture was described as having three major fragments, as follows:
- Metacarpal shaft
- Dorsal metacarpal base
- Volar metacarpal base
Since the original description, the term has come to include essentially all comminuted thumb metacarpal base fractures 3.
Rolando fracture is at risk for further displacement because of the resting tone present in the multiple tendons that act on the thumb. The extensor pollicis brevis and extensor pollicis longus shorten the thumb ray, as does the pull of the flexor pollicis longus. The adductor pollicis tends to pull the distal metacarpal toward the palm, which, in conjunction with the abductor pollicis longus acting on the metacarpal base, commonly produces varus at the metaphyseal-diaphyseal junction.
Rolando fracture is an unstable injury that requires surgical reduction and fixation.
Figure 1. Rolando fracture X-ray
Thumb anatomy
The thumb has two bones. The first bone (distal phalange) extends from the tip of the thumb to the knuckle. The second bone (proximal phalange) extends from the knuckle to the base of the thumb. This is the area of webbing between the thumb and the first finger. The thumb connects with a bone in the hand (first metacarpal), which articulates with the trapezium bone in the distal carpal row.
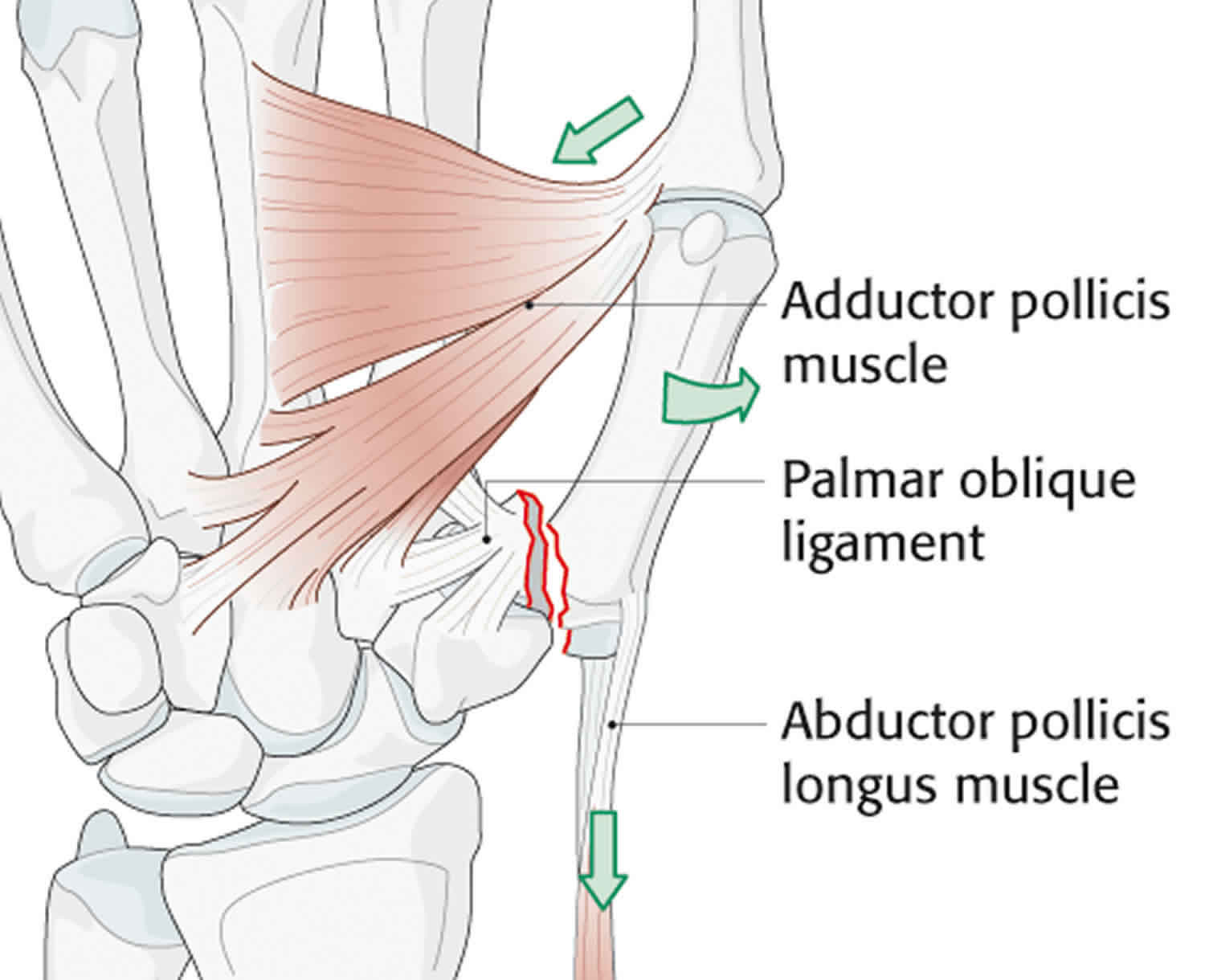
The first carpometacarpal joint is unique in that it includes only an articulation between the trapezium and the base of the first metacarpal. The first carpometacarpal joint is completely isolated from the rest of the carpometacarpal joints of the hand. The articulation is saddle-shaped which allows greater motion, but consequently there is less inherent stability from the bony anatomy. Ligamentous stability at the trapeziometacarpal joint is maintained by the anterior (volar) and posterior oblique ligaments, the anterior and posterior intermetacarpal ligaments, and the dorsal radial ligament. The anterior (volar) oblique ligament originates on the trapezium and inserts into the volar ulnar beak of the thumb metacarpal. This is the most important ligament in maintaining carpometacarpal stability. The dorsal ligament is not as strong as the volar ligament but is reinforced by the abductor pollicis longus. Of significance in Rolando fracture is the volar oblique ligament, or beak ligament, which inserts at the base of the first metacarpal and opposes the action of the abductor pollucis longus 4. When a fracture occurs this opposing action is interrupted, an intra-articular fracture propagates separating a fragment which remains attached to this strong ligament and the pull of the abductor pollucis longus dislocates the remaining base of the thumb metacarpal 5. Figure 2 illustrates the anatomy of a Rolando fracture.
Figure 2. Rolando fracture anatomy
Rolando fracture causes
Rolando fracture appears to be secondary to a significant axial load that splits and crushes the metacarpal articular surface. Rolando described two cases that occurred secondary to a fall on the radial side of the hand, with the thumb in adduction, and a third case that was caused by a closed fist, with the thumb folded and held in the palm, striking an adversary’s head 6.
Rolando fracture symptoms
Rolando fracture symptoms may include:
- Severe pain at the fracture site
- Swelling
- Limited or no ability to move the thumb
- Extreme tenderness
- A misshapen or deformed look to the thumb
- Numbness or coldness in the thumb
Following injury, patients present with a swollen, tender thumb base. If significant varus has developed, a clinically visible deformity may be present. However, swelling can mask a surprising amount of angulation. Neurovascular and tendon injuries are not commonly associated with this fracture.
Rolando fracture complications
Stiffness and osteoarthritis are the main long term consequences of Rolando’s fracture. Multi-fragmentary forms are considered the most severe forms and those most at risk of joint stiffness and osteoarthritis 7.
Rolando fracture diagnosis
Diagnosis requires radiography in the two orthogonal projections, but since the thumb lies on a different plane from the rest of the hand 8, the use of specific views can help to identify and classify the lesion 9. In particular, the projection of Robert and that of Bett, help to evaluate the articular congruence and the degree of displacement of the fragments.
- Robert view (true AP of the thumb)
- The forearm is in maximum pronation with the dorsum of the thumb lying against the cassette
- True lateral of the thumb
- Hand pronated 30 degrees; radiographic beam angled 15 degrees distally
- Oblique view
In particular, the Robert view allows us to obtain an accurate anteroposterior view; it requires that the back aspect of the thumb rests on the radiographic plate, with the hand in overpronation. The Bett view, instead, allows an actual lateral image of the tarsometatarsal joint. It can be obtained by placing the palmar aspect of the hand on the radiographic cassette, pronated with an inclination between 15 and 35 degrees with the beam inclined at 15 degrees distal to proximal 8.
CT scans obtained with collimation, and slice thickness between 0.5 and 1.0 mm, complemented by multiplanar and 3D reconstructions can provide valuable information for surgical planning 10. The associated ligaments and tendons injuries, as well as osseous abnormalities, can be examined with MRI. For this purpose, MRI should be performed using small fields of view (FOVs) and small extremity coils to optimize the signal-to-noise ratios 10.
Rolando fracture treatment
Rolando fracture is much more complex to treat than Bennett fracture patterns due to its intrinsic instability 11. The choice of the most appropriate treatment method is influenced mainly by the number of fragments and the degree of displacement. In general, the following treatment algorithm is recommended 12:
- Closed reduction and thumb spica splinting/immobilization
- Indicated for extra-articular fractures or minimally displaced 2-part articular fractures (i.e., Bennett fractures) with less than 1mm displacement
- Closed reduction and percutaneous pinning
- Percutaneous reduction pinning with K-wire fixation is necessary to set either:
- Extra-articular fractures with more than 30 degrees of angulation following closed reduction
- Rolando fracture patterns with minimal (i.e., less than 1 mm) of displacement or when fracture patterns are comminuted fracture patterns not amenable to screw fixation
- Percutaneous reduction pinning with K-wire fixation is necessary to set either:
- Open reduction internal fixation (ORIF)
- Indicated when greater than 1 mm displacement in intra-articular fractures (Bennett or Rolando fracture patterns) and comminuted fracture fragments involving the metacarpal base when the fragments are large enough and amenable to screw fixation
- Distraction and external fixation
- Indicated for the following:
- Rolando fracture with >1mm displacement and significant soft tissue injury not amenable to open reduction internal fixation (ORIF)
- Bennett, Rolando, or severely comminuted fractures with fragments too small for open reduction internal fixation (ORIF)
- Indicated for the following:
Surgery can be open or arthroscopic, but in both cases, it requires an articular approach 13. Open reduction is possible through a Wagner incision, radial to the thenar skin creases 14. Fixation may be obtained by means of a plate and screw, tension banding and K-wires 8. The surgical approach allows ligaments to be freed, eliminating any capsular interpositions, and the fracture reduction process to be visually monitored to obtain a temporary fixation with Kirshner wire and the application of screws or mini T-plates to fix the diaphysis and epiphysis together. If the strength of the construct allows it, early and even immediate mobilization is encouraged, prescribing a removable commissural splint for the first month 7.
Surgical therapy
If open reduction is thought to be a reasonable choice for the patient with a Rolando fracture, a curvilinear incision is made at the thumb base. Branches of the superficial radial nerve dorsally and the lateral antebrachial cutaneous nerve volarly are identified with loupe magnification, isolated, and protected.
The periosteum is split along the first metacarpal shaft, and the joint is entered in the interval between the abductor pollicis longus and extensor pollicis brevis tendons. Large articular fragments are identified. The articular surface is reconstructed in a piecemeal fashion with fine Kirschner wires (K-wires) and then secured to the metacarpal shaft by using a small T plate (see the image below). Intraoperative radiographs are obtained to confirm a satisfactory reduction, and the limb is placed in a thumb spica splint.
Comminuted metacarpal base fractures that cannot be secured with pins or screws can be treated with external fixation 15. One technique involves a quadrilateral frame with two pins each in the thumb and index metacarpals, limited K-wire fixation of the articular surface, and bone grafting of any metaphyseal void that has been created after length restoration. Another technique involves placing fixator pins in the trapezium and metacarpal shaft to maintain distraction.
Byrne et al 16 recommended dynamic “S”-Quattro (Stockport Serpentine Spring System) as a primary and definitive treatment modality for external fixation of complex fractures of the base of the thumb when conservative and other surgical interventions have failed.
Spangberg and Thoren 17 described the use of oblique K-wire traction in the treatment of Bennett fracture. Gelberman expanded this to include comminuted metacarpal base fractures and trapezial fractures 18. The technique involves use of a single K-wire that is passed from the metacarpal base out of the thumb web, with a small hook on the proximal end of the wire. The distal end is then attached to an outrigger through rubber bands. Active motion is started to mold the joint surface. This traction neutralizes displacing muscle forces and maintains reduction through ligamentotaxis.
Complications
Complications are often directly related to the extent of the comminution. Hardware-related issues can develop, such as pin-tract infection or screw pullout with resultant loss of fixation. Soft-tissue complications include damage to the branches of the superficial radial or lateral antebrachial cutaneous nerve. Some degree of joint stiffness is inevitable, given the articular nature of the fracture.
Rolando fracture recovery time
Secure plate fixation can allow early motion of the joint surface. However, if the comminution requires grafting and stability is a concern, immobilization in a thumb spica cast for 4-6 weeks is the safest course of action. External fixators, K-wires, or both can be removed at approximately 6 weeks postoperatively, and active motion can begin.
Langhoff et al 19 studied 16 patients who underwent open reduction with fine Kirschner wires (K-wires). At a mean follow-up of 5.8 years, nine had no residual symptoms, six had symptoms with moderate activity, and one had significant symptoms necessitating a change in occupation. Eight had reduced range of motion (ROM), and three had a visible deformity of the thenar base region that was related to large residual angulations of 35-55º. Osteoarthritic changes were present in six (55%) of the 11 patients with radiographs at follow-up; this did not appear to correlate with the quality of reduction or with late symptoms.
Proubasta 20 reported the results of five patients treated with a mini external fixator. Pins were placed in the trapezium and thumb metacarpal shaft, and the fracture was reduced with distraction. At short-term follow-up at 3 months, no complications were noted, and the patients all were free from pain and had a full range of thumb movements.
Buchler et al 21 reviewed their experience in the management of 13 complex thumb metacarpal base fractures in which multiple fragments were involved. The authors treated the fractures with external fixation between the index and thumb metacarpals and limited internal fixation of the joint surface using pins, screws, or both. They performed bone grafting of the metaphyseal void present after distraction.
The average duration of follow-up in this study was 35 months 21. There were no significant complications, and no loss of reduction, malalignment, or secondary subluxation developed. Grip and pinch strength were 81% and 88% of the contralateral side, respectively. Rotation of the thumb metacarpal was 79% of the unaffected side. No diffuse degenerative changes occurred.
References- Hong E. Hand injuries in sports medicine. Prim Care. 2005;32(1):91–103.
- Rolando S. Fracture of the base of the first metacarpal and a variation that has not yet been described: 1910. (Translated by Roy A. Meals). Clin Orthop Relat Res. 2006 Apr. 445:15-8.
- Huang JI, Fernandez DL. Fractures of the base of the thumb metacarpal. Instr Course Lect. 2010. 59:343-56.
- Dial WB, Berg E. Bennett fracture. Hand 1972;4:229–35.
- Pollen AG. The conservative treatment of Bennett fracture – subluxation of the thumb metacarpal. J Bone Joint Surg 1968;50B:91–101.
- Kadow TR, Fowler JR. Thumb Injuries in Athletes. Hand Clin. 2017 Feb. 33 (1):161-173.
- Liverneaux PA, Ichihara S, Hendriks S, Facca S, Bodin F. Fractures and dislocation of the base of the thumb metacarpal. J Hand Surg Eur Vol. 2015 Jan;40(1):42-50.
- Carlsen BT, Moran SL. Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. J Hand Surg Am. 2009 May-Jun;34(5):945-52.
- Kapandji A, Moatti E, Raab C. [Specific radiography of the trapezo-metacarpal joint and its technique (author’s transl)]. Ann Chir. 1980 Nov;34(9):719-26.
- Peterson JJ, Bancroft LW. Injuries of the fingers and thumb in the athlete. Clin Sports Med. 2006 Jul;25(3):527-42, vii-viii.
- Marsland D, Sanghrajka AP, Goldie B. Static monolateral external fixation for the Rolando fracture: a simple solution for a complex fracture. Ann R Coll Surg Engl. 2012 Mar;94(2):112-5.
- Alam J, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Mar 15, 2019. Thumb Spica Splinting.
- Zemirline A, Lebailly F, Taleb C, Facca S, Liverneaux P. Arthroscopic assisted percutaneous screw fixation of Bennett’s fracture. Hand Surg. 2014;19(2):281-6.
- Arenas-Prat JM. Wagner approach for first carpometacarpal joint denervation. Tech Hand Up Extrem Surg. 2012 Jun;16(2):107-9.
- Duan W, Zhang X, Yu Y, Zhang Z, Shao X, Du W. Treatment of comminuted fractures of the base of the thumb metacarpal using a cemented bone-K-wire frame. Hand Surg Rehabil. 2019 Feb. 38 (1):44-51.
- Byrne AM, Kearns SR, Morris S, Kelly EP. “S” Quattro external fixation for complex intra-articular thumb fractures. J Orthop Surg (Hong Kong). 2008 Aug. 16 (2):170-4.
- SPANGBERG O, THORTEN L. BENNETT’S FRACTURE. A METHOD OF TREATMENT WITH OBLIQUE TRACTION. J Bone Joint Surg Br. 1963 Nov. 45 (4):732-6.
- Gelberman RH, Vance RM, Zakaib GS. Fractures at the base of the thumb: treatment with oblique traction. J Bone Joint Surg Am. 1979 Mar. 61 (2):260-2.
- Langhoff O, Andersen K, Kjaer-Petersen K. Rolando’s fracture. J Hand Surg Br. 1991 Nov. 16 (4):454-9.
- Proubasta IR. Rolando’s fracture of the first metacarpal. Treatment by external fixation. J Bone Joint Surg Br. 1992 May. 74 (3):416-7.
- Buchler U, McCollam SM, Oppikofer C. Comminuted fractures of the basilar joint of the thumb: combined treatment by external fixation, limited internal fixation, and bone grafting. J Hand Surg Am. 1991 May. 16 (3):556-60.