Ruptured quadriceps tendon
Ruptured quadriceps tendon is usually associated with forced flexion of the knee or a direct blow, although spontaneous ruptures are reported. Tendons are strong cords of fibrous tissue that attach muscles to bones. The quadriceps tendon works with the muscles in the front of your thigh to straighten your leg. The degree that a quadriceps tendon rupture limits lower leg extension is based on the severity of tendon damage. Minor tendon tears may have minimal impact on extensor function, while complete tendon tears may totally impede lower leg extension 1.
Quadriceps tendon tears can be either partial or complete:
- Partial tears. Many tears do not completely disrupt the soft tissue. This is similar to a rope stretched so far that some of the fibers are frayed, but the rope is still in one piece.
- Complete tears. A complete tear will split the soft tissue into two pieces.
When the quadriceps tendon completely tears, the muscle is no longer anchored to the kneecap. Without this attachment, the knee cannot straighten when the quadriceps muscles contract.
The quadriceps tendon is derived from the muscular junction of the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius muscles at the anterior superior pole of the patella 2. The quadriceps tendon in combination with patellar tendon and the patella bone make up the extensor mechanism of the lower leg. These muscles derive their neurovascular innervation from the femoral nerve and artery. Specifically, the rectus femoris, vastus intermedius, and vastus lateralis gain their arterial supply from the lateral femoral circumflex artery. The vastus medialis gains its arterial supply from the femoral artery, superior medial genicular branch of the popliteal artery, and the profunda femoris artery. The vastus lateralis, vastus medialis, and the vastus intermedius act both as knee extenders as well as assist with patellar tracking. The vastus lateralis is the largest of the quadriceps muscles. It helps to pull the patella laterally. This action must be counterbalanced by the vastus medialis, which is the smallest of the quadriceps muscles and acts to pull the patella medially. The vastus intermedius acts to help stabilize midline tracking of the patella. The combined contraction of this group of anterior thigh muscles causes extension of the lower leg. The rectus femoris also plays a role in hip flexion. A rupture of this central tendon drastically hinders knee extension and directly effects functionality. Small tears of the quadriceps tendon can make it difficult to walk and participate in other daily activities. A large tear of the quadriceps tendon is a disabling injury. It usually requires surgery and physical therapy to regain full knee function.
Lower leg extensor mechanism ruptures as a whole are very rare, but are reported to have high morbidity and are often debilitating 3. Quadriceps tendon ruptures are reported to have an incidence of 1.37/100,000 and 0.68/100,000 for patellar tendon ruptures. Extensor mechanism ruptures are most common unilaterally. However, there are several case reports of this injury occurring bilaterally, from one precipitating event.
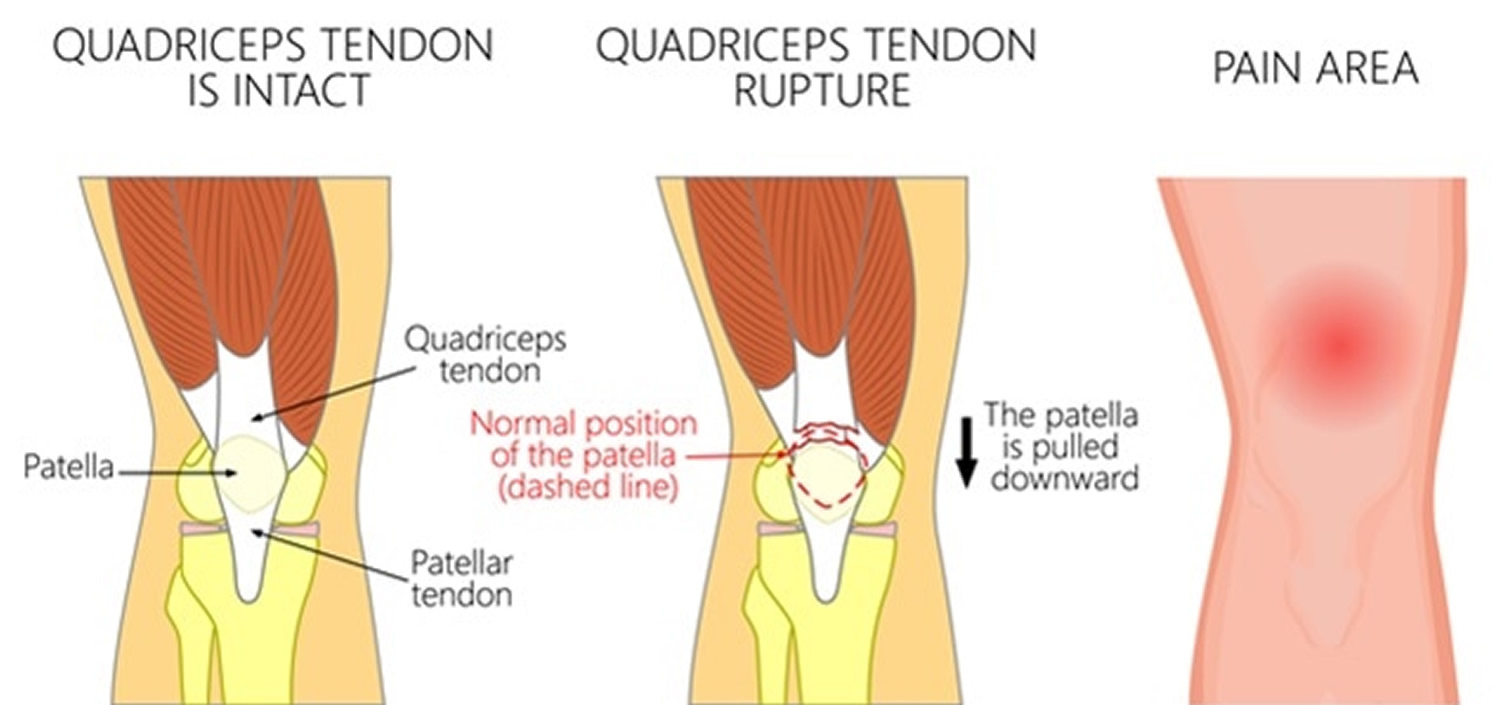
Figure 1. Quadriceps tendon anatomy
Quadriceps tendon tear causes
Injury
A quadriceps tear often occurs when there is a heavy load on the leg with the foot planted and the knee partially bent. Think of an awkward landing from a jump while playing basketball. The force of the landing is too much for the tendon and it tears.
Tears can also be caused by falls, direct force to the front of the knee, and lacerations (cuts).
Tendon weakness
A weakened quadriceps tendon is more likely to tear. Several things can lead to tendon weakness.
- Tendinitis. Inflammation of the quadriceps tendon, called quadriceps tendinitis, weakens the tendon. It may also cause small tears. Quadriceps tendinitis is most common in people who run and participate in sports that involve jumping.
- Chronic disease. Weakened tendons can also be caused by diseases that disrupt blood supply. Chronic diseases which may weaken the tendon include:
- Chronic renal failure
- Conditions associated with renal dialysis
- Hyperparathyroidism
- Gout
- Leukemia
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Diabetes mellitus
- Infection
- Metabolic disease
- Steroid use. Using corticosteroids has been linked to increased muscle and tendon weakness.
- Fluoroquinolones. This special type of antibiotic has been associated with quadriceps tendon tears.
- Immobilization. When you are off your feet for a prolonged period of time, the muscles and tendons supporting your knees lose strength and flexibility.
- Surgery. Although it is rare, quadriceps tears have occurred after a knee surgery or dislocation.
Quadriceps tendon ruptures have a positive correlation with age and multiple medical comorbidities. This injury historically is more prevalent in males, with susceptibility increasing proportionally with age after 40 years. This is in opposition to patellar tendon ruptures, which commonly occur before age 40, and are often related to sports injuries. Medications and medical comorbidities associated with quadriceps tendon ruptures include fluoroquinolones, corticosteroids, anabolic steroids, hyperparathyroidism, gout, diabetes, obesity, chronic kidney disease, hypercholesterolemia, hyperuricemia, rheumatoid arthritis, systemic lupus erythematosus, and osteogenesis imperfecta 4.
Quadriceps tendon ruptures in athletes are the direct result of a sudden and strong contraction of the quadriceps muscles from a jump and land mechanism or sudden change in direction while running. Quadriceps tendon ruptures in non-athletes are usually the direct result of a fall or other trauma in individuals with predefined medical comorbidities which are thought to cause pathologic tendon degeneration. One proposed biomechanical mechanism involves knee flexion with simultaneous quadriceps contraction. Another proposed mechanism involves extensive rotation as well as hyperflexion of the lower leg. The majority of quadriceps tendon ruptures occur at the myotendinous junction with patellar tendon ruptures occurring most commonly within the tendon itself. End-stage renal disease patients on dialysis have the highest association with tendon degeneration resulting in ruptures. The pathophysiologic mechanism involved in chronic kidney disease is theorized to involve uremic toxins, renal osteodystrophy, and hyperparathyroidism 5. As renal function declines, there is often a homeostatic imbalance of calcium, phosphorus, vitamin D, and parathyroid hormone. Elevated parathyroid hormone results in increased bone turnover. Over time, this is thought to weaken myotendinous junctions, resulting in increased potential for tendon rupture with minimal tensile stress. In patients receiving dialysis with insufficiently permeable filters, there has been higher reported serum beta-2 microglobulin. Beta-2-microglobulin collects in bones, joints, and tendons. This phenomenon is known as dialysis-related amyloidosis. Beta-2 microglobulin accumulation results in functional impairment in tissue elasticity and therefore a higher potential for tendon rupture with minimal trauma. The proposed mechanism involved in diabetes involves the accumulation of advanced glycation end products. Advanced glycation end products form covalent bonds with collagen fibers. This results in the release of inflammatory cytokines which cause progressive tendon damage. As one ages there is also decreased arterial capillaries per unit surface area. This results in a decreased healing potential after repeat microtrauma.
Quadriceps tendon tear symptoms
Patients presenting with potential quadriceps tendon ruptures usually report hearing an audible pop or experiencing a tearing sensation. This is immediately followed by a decreased ability to bear weight and is commonly accompanied by pain, swelling and effusion. A palpable defect can usually be felt at the superior pole of the patella. Patients with complete tears have an impaired ability to perform a straight leg raise. With partial tears, there is impaired knee extension. With complete tears, knee extension is usually absent. There is usually no impaired range of motion at the hip or ankle.
Torn quadriceps tendon symptoms include:
- An indentation at the top of your kneecap where the tendon tore
- Bruising
- Tenderness
- Cramping
- Your kneecap may sag or droop because the tendon is torn
- Difficulty walking due to the knee buckling or giving way
Quadriceps tendon tear diagnosis
Your doctor will discuss your general health and the symptoms you are experiencing. He or she will also ask you about your medical history. Questions you might be asked include:
- Have you had a previous injury to the front of your knee?
- Have you ever injured a quadriceps muscle?
- Do you have quadriceps tendinitis?
- Do you have any medical conditions that might predispose you to a quadriceps injury?
After discussing your symptoms and medical history, your doctor will conduct a thorough examination of your knee. To determine the exact cause of your symptoms, your doctor will test how well you can extend, or straighten, your knee. While this part of the examination can be painful, it is important to identify a quadriceps tendon tear.
Imaging tests
To confirm the diagnosis, your doctor may order some imaging tests, such as an x-ray or magnetic resonance imaging (MRI) scan.
- X-rays. The kneecap moves out of place when the quadriceps tendon tears. This is often very obvious on a “sideways” x-ray view of the knee. Complete tears can often be identified with these x-rays alone.
- MRI. This scan creates better images of soft tissues like the quadriceps tendon. The MRI can show the amount of tendon torn and the location of the tear. Sometimes, an MRI is required to rule out a different injury that has similar symptoms.
Torn quadriceps tendon treatment
Your doctor will consider several things when planning your treatment, including:
- The type and size of your tear
- Your activity level
- Your age
Like most musculoskeletal injuries, initial management of suspected quadriceps tendon ruptures includes rest, ice, compression, and elevation (RICE). Partial quadriceps tendon ruptures may be managed non-operatively. However, the majority of complete quadriceps tendon ruptures require early diagnosis and surgical treatment to limit long-term morbidity and disability. The timing of surgical repair has been attributed to optimal recovery and functionality than the specific surgical approach 6.
Nonsurgical treatment
Most small, partial tears respond well to nonsurgical treatment.
- Immobilization. Your doctor may recommend you wear a knee immobilizer or brace. This will keep your knee straight to help it heal. You will most likely need crutches to help you avoid putting all of your weight on your leg. You can expect to be in a knee immobilizer or brace for 3 to 6 weeks.
- Physical therapy. Once the initial pain and swelling has settled down, physical therapy can begin. Specific exercises can restore strength and range of motion.
Exercises will gradually be added to your program. Straight leg raises to strengthen your quadriceps are often central to a physical therapy plan. As time goes on, your doctor or therapist will unlock your brace. This will allow you to move more freely with a greater range of motion. You will be prescribed more strengthening exercises as you heal.
Your doctor will discuss with you when it is safe to return to sports activity.
Surgical treatment
Most people with complete tears will require surgery to repair the torn tendon. If you have a large partial tear or a partial tear associated with tendon degeneration, your doctor may also recommend surgery. This will likely depend upon your age, your activities, and your previous level of function.
Surgical repair reattaches the torn tendon to the top of the kneecap. People who require surgery do better if the repair is performed soon after the injury. Early repair may prevent the tendon from scarring and tightening into a shortened position.
Hospital stay
Although tendon repairs are sometimes done on an outpatient basis, most people do stay in the hospital at least one night after this operation. Whether or not you will need to stay overnight will depend on your medical needs.
The surgery may be performed with regional (spinal) anesthetic which numbs your lower body, or with a general anesthetic that will put you to sleep.
Procedure
To reattach the tendon, sutures are placed in the tendon and then threaded through drill holes in the kneecap. The sutures are tied at the bottom of the kneecap. Your surgeon will carefully tie the sutures to get the right tension in the tendon. This will also make sure the position of the kneecap closely matches that of your uninjured kneecap.
A recent development in quadriceps tendon repair is the use of suture anchors. Surgeons attach the tendon to the bone using small metal implants called suture anchors. Using these anchors means that drill holes in the kneecap are not necessary. This is a new technique, so data is still being collected on its effectiveness. Most orthopaedic research on quadriceps tendon repair involves the direct suture repair with the drill holes in the kneecap.
To provide extra protection to the repair, some surgeons use sutures or cables to help hold the kneecap in position while the tendon heals. If your surgeon does this, the wires or cables may need to be removed during a later, scheduled operation.
Your surgeon will discuss your need for this extra protection before your operation. Sometimes, surgeons make this decision for additional protection during surgery. It is then that they see the tendon shows more damage than expected, or the tear is more extensive.
If your tendon has shortened too much before surgery, it will be hard to re-attach it to your kneecap. Your surgeon may need to add tissue graft to lengthen the tendon. This is often the case if more than a month has passed since your injury. Severe damage from the injury or underlying disease can also make the tendon too short. Your surgeon will discuss this additional procedure with you prior to surgery.
Figure 2. Ruptured quad tendon surgery
Footnote: To reattach the tendon, small holes are drilled in the kneecap (left) and sutures are threaded through the holes to pull the tendon back to the bone (right).
Complications
The most common complications of quadriceps tendon repair include weakness and loss of knee motion. It is also possible to re-rupture the tendon after it has been repaired. In addition, the position of your kneecap may be different after the procedure.
As with any surgery, the other possible complications include infection, wound breakdown, a blood clot, or anesthesia complications.
Ruptured quad tendon recovery
After surgery you will require some type of pain management, including ice and medications. About 2 weeks after surgery, your skin sutures or staples will be removed in the surgeon’s office.
Most likely, your repair will be protected with a knee immobilizer or a long leg cast. You may be allowed to put your weight on your leg with the use of a brace and crutches (or a walker). Over time, your doctor or therapist will unlock your brace. This will allow you to move more freely with a greater range of motion. Strengthening exercises will be added to your rehabilitation plan.
In some cases, an “immediate motion” protocol (treatment plan) is prescribed. This is a more aggressive approach and not appropriate for all patients. Most surgeons protect motion early on after surgery.
The exact timeline for physical therapy and the type of exercises prescribed will be individualized to you. Your rehabilitation plan will be based on the type of tear you have, your surgical repair, your medical condition, and your needs.
Quadriceps tendon rupture recovery time
Complete recovery takes at least 4 months. Most repairs are nearly healed in 6 months. Many patients have reported that they required 12 months before they reached all their goals.
Despite the surgical approach or postoperative course, the most common complications involve pain and quadriceps weakness. Patients report pain and weakness most commonly associated with prolonged standing, squatting, or ascending and descending stairs. However, few patients who receive timely medical intervention report significant functional debility.
Ruptured quadriceps tendon prognosis
Most people are able to return to their previous occupations and activities after recovering from a quadriceps tendon tear. Slightly over half of people have thigh weakness and soreness at the site of the tear. People who require surgery do better if the repair is performed early after the injury 7. In a large study, Konrath et al 8 found that 83% of patients returned to their previous occupations, 51% were unable to return to their preinjury activity levels, and 53% had persistent quadriceps strength deficits (>20% in comparison with the uninjured leg). The injured leg had a mean thigh atrophy of 1.5 cm as compared with the uninjured leg.
In a retrospective continuous study that included 25 knees with acute quadriceps tendon rupture (22 patients; 17 males, 5 females; mean age, 64 years; age range, 52-87 years), Brossard 9 compared the outcomes of suture-anchor fixation and the gold standard technique (ie, transosseous patellar suture). Variables studied included active range of motion, muscle strength, patient satisfaction, Lysholm score, return to work, and radiologic behavior of the anchors. At a mean follow-up of 7 years (range, 3-9 years), the outcomes with anchors were comparable to those with the gold-standard technique.
If you are a competitive athlete, your surgeon will most likely want to test your leg strength before giving a go-ahead to return to sports. Your surgeon will compare your leg strength using some functional knee testing (like hopping). The goal is that your strength be at least 85-90% of your uninjured side. In addition to leg strength, your surgeon will assess your leg’s endurance, your balance, and if you are having any swelling.
Your return to competitive status will be addressed very carefully with you by your surgeon.
References- Barge-Caballero G, López-Bargiela P, Pombo-Otero J, Pardo-Martínez P. Quadriceps tendon rupture in wild-type transthyretin amyloidosis (ATTRwt). Eur. Heart J. 2019 Mar 12
- Pope JD, Plexousakis MP. Quadriceps Tendon Rupture. [Updated 2019 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482389
- Nori S. Quadriceps tendon rupture. J Family Med Prim Care. 2018 Jan-Feb;7(1):257-260.
- Wu W, Wang C, Ruan J, Wang H, Huang Y, Zheng W, Chen F. Simultaneous spontaneous bilateral quadriceps tendon rupture with secondary hyperparathyroidism in a patient receiving hemodialysis: A case report. Medicine (Baltimore). 2019 Mar;98(10):e14809
- Glick R, Epstein DS, Aponso DT. Spontaneous bilateral quadriceps tendon rupture associated with norfloxacin. Intern Med J. 2015 Dec;45(12):1313-5.
- Boublik M, Schlegel TF, Koonce RC, Genuario JW, Kinkartz JD. Quadriceps tendon injuries in national football league players. Am J Sports Med. 2013 Aug;41(8):1841-6.
- Ramseier LE, Werner CM, Heinzelmann M. Quadriceps and patellar tendon rupture. Injury. 2006 Jun. 37(6):516-9.
- Konrath GA, Chen D, Lock T. Outcomes following repair of quadriceps tendon ruptures. J Orthop Trauma. 1998 May. 12(4):273-9.
- Brossard P, Le Roux G, Vasse B, Orthopedics, Traumatology Society of Western France (SOO). Acute quadriceps tendon rupture repaired by suture anchors: Outcomes at 7 years’ follow-up in 25 cases. Orthop Traumatol Surg Res. 2017 Jun. 103 (4):597-601.