What is saccharomyces boulardii
Saccharomyces boulardii is a probiotic regulated as a dietary supplement intended for use by the general healthy population, not as a drug to prevent, treat, or mitigate disease. For dietary supplements, premarketing demonstration of safety and efficacy and approval by the Food and Drug Administration (FDA) are not required; only premarket notification is required. Probiotics are defined by the Food and Agriculture Organization (FAO) of the World Health Organization as live microorganisms that, when administered in adequate amounts, confer a health benefit on the host 1, 2. The term probiotic can be subcategorized to include probiotic drugs, probiotic foods (e.g., foods, food ingredients, and dietary supplements), direct-fed microbials (probiotics for animal use), and designer probiotics (genetically modified probiotics) 3. In the United States, probiotic products are marketed to a generally healthy population as foods or dietary supplements 4.
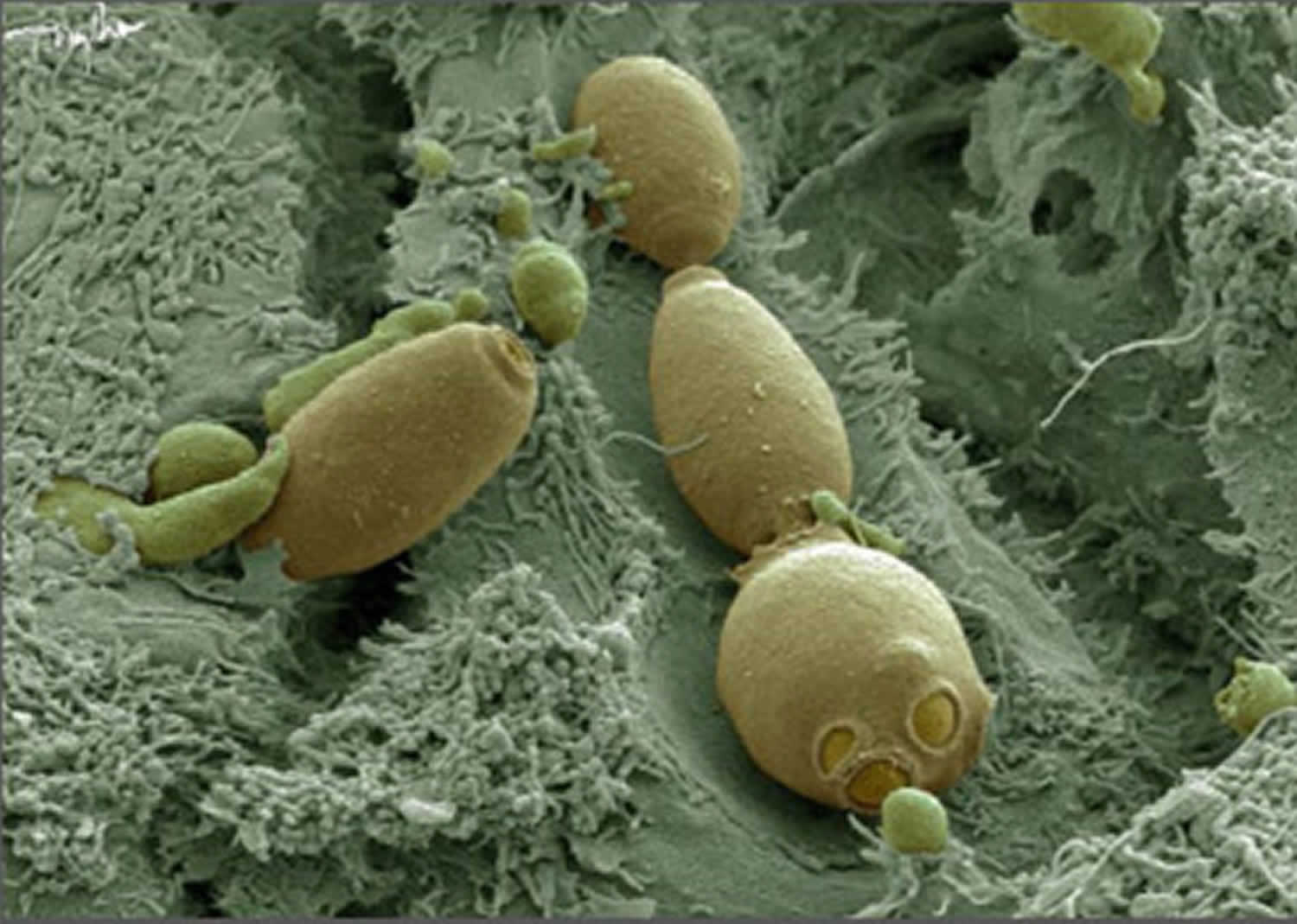
Saccharomyces boulardii CNCM I-745 is a fungus classified as a yeast, which routinely cannot be distinguished from Saccharomyces cerevisiae and at present is regarded as a subtype of Saccharomyces cerevisiae HANSEN CBS 5926 (a strain of baker’s yeast) 5. These yeasts are widespread in nature and can be found on plants, fruit and in soil, being also used in the baking and brewing industry 6. Usually, they are considered to be nonpathogenic commensals of the digestive tract, administered as probiotics for several indications, including Clostridium difficile-associated disease 7. Saccharomyces boulardii CNCM I-745, the probiotic yeast is efficient for the treatment and prevention of diarrhea of various causes 8. Saccharomyces boulardii CNCM I-745 has also been used in a variety of different clinical conditions, including human immunodeficiency virus (HIV) 9 and Helicobacter pylori infection 10.
Saccharomyces boulardii CNCM I-745 has an optimal growth temperature around 37°C and a relatively high acid tolerance 11, resulting in a good survival after gastric passage. A spectrum of favorable effects, including prebiotic effects 12, toxin degradation effects 13, pathogen binding effects 14, anti-secretory effects 15, physical barrier effects 16, effects on the microbiota 17, and on the immune system 18 reduces the risk to develop diarrhea or counteract diarrhea.
Prebiotic effects are accomplished by cell wall components of Saccharomyces boulardii CNCM I-745, consisting of glucans, mannoproteins, and chitin which serve short-chain fatty acid producing bacteria as suitable substrates for fermentation 19. Also, Saccharomyces boulardii CNCM I-745 restores intestinal barrier integrity by regulation of E-cadherin recycling 20. In several animal and human studies, a protective and stabilizing effect on the intestinal microbiota has been demonstrated, including the prevention of antibiotic-associated diarrhea by decreasing the antibiotic-induced reduction in the intestinal microbiota, as well as by supporting a faster regeneration of the intestinal microbiota following antibiotic therapy 21.
Saccharomyces boulardii CNCM I-745 influences the infection-induced signalling cascades of its human host as well as the innate and adaptive immune system. In a healthy host, Saccharomyces boulardii CNCM I-745 leads to a general unspecific immune system activation 22, which can be considered advantageous in preventing diarrhea. During diarrhea, it attenuates an over-reacting inflammatory immune response and diarrheic leakage of fluids into the intestinal lumen 18. The combined effects by the yeast reduce colonization by pathogens and preservation of the integrity of the intestinal epithelial cell layer.
However, since the 1990s, an increasing number of publications of fungemia and invasive infections caused by Saccharomyces boulardii, particularly among intensive care unit (ICU) patients and individuals with multiple co-morbidities, have been reported in literature in patients treated with a probiotic preparation containing this yeast 23. Furthermore, it can also cause infections in otherwise healthy individuals 24.
Since recent increases in incidence and severity of Clostridium difficile infection, probiotics have been used to treat recurrent and/or refractory disease in hospitalized patients. Albeit rare, serious complications (i.e., fungemia) in other than healthy populations receiving probiotics have been reported in the literature. Specifically, most complications related to the administration of Saccharomyces boulardii have occurred in immunocompromised or critically ill patients or in those who had central venous catheters serving as a portal of entry of organisms from healthcare workers’ contaminated hands to patients’ bloodstream during administration 25. Careful risk assessment for patients and proper handling of the probiotic during administration need to be conducted before using probiotics as drugs in institutional settings. Vigilant reporting of adverse events resulting from probiotic use is necessary to establish the safety profile of these agents when they are used in other than healthy populations. Before use of a probiotic is considered for hospitalized patients, careful assessment of risk versus benefit must be made. To ensure patient safety, probiotics should be properly handled during administration 25. It has been postulated that further studies are needed to evaluate the efficacy of probiotic preparations, to determine the optimal dose and strain of probiotic, and possible adverse events related to their use in hospitalised patients 26.
Depending on the intended use of a probiotic, whether as a drug or a dietary supplement, regulatory requirements differ. According to the Food and Drug Administration (FDA) definition, a drug is an article intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease 27. If a probiotic is intended for use as a drug, then it must undergo the regulatory process as a drug, which is similar to that of any new therapeutic agent. An Investigational New Drug application must be submitted and authorized by FDA before an investigational or biological product can be administered to humans. The probiotic drug must be proven safe and effective for its intended use before marketing 28.
If a probiotic is intended for use as a dietary supplement, it is placed under the umbrella of “foods,” and as such is regulated by FDA’s Center for Food Safety and Applied Nutrition 29. A dietary supplement is defined by the Dietary Supplement Health and Education Act of 1994 as a product taken by mouth that contains a “dietary ingredient” intended to supplement the diet. Supplements must contain >1 of the following dietary ingredients: a vitamin; a mineral; an herb or other botanical (excluding tobacco); an amino acid; a dietary substance for use by persons to supplement the diet by increasing the total dietary intake; a concentrate, metabolite, constituent, extract; or combination of any of the above 30.
In contrast to drugs, dietary supplements do not need FDA approval before being marketed. However, manufacturers need to notify FDA before marketing a product. According to Dietary Supplement Health and Education Act of 1994, the manufacturer is responsible for determining that the dietary supplements that it manufactures or distributes are safe and that any representations or claims made about them are substantiated by adequate evidence to show that they are not false or misleading; the manufacturers need not provide FDA with evidence that substantiates the safety or purported benefits of their products, either before or after marketing. If a dietary supplement contains a new dietary ingredient that was not sold before October 15, 1994, then the manufacturer is required to notify FDA and demonstrate to FDA before marketing why the ingredient is reasonably expected to be safe for use in a dietary supplement. On June 22, 2007, FDA announced a final rule establishing Current Good Manufacturing Practice requirements for dietary supplements. To ensure the identity, purity, quality, strength, and composition of dietary supplements, those who manufacture, package, or hold dietary supplements must follow these regulations 31. Also, since implementation of the Dietary Supplement and Nonprescription Drug Consumer Protection Act in 2006, manufacturers and distributors of dietary supplements have been required to record and forward to FDA any directly received reports of serious adverse events associated with use of their products.
Be watchful with this combination
Medications for fungal infections (Antifungals): Saccharomyces boulardii is a fungus. Medications for fungal infections help reduce fungus in and on the body. Taking Saccharomyces boulardii with medications for fungal infections can reduce the effectiveness of Saccharomyces boulardii. Some medications for fungal infection include fluconazole (Diflucan), caspofungin (Cancidas), itraconazole (Sporanox) amphotericin (Ambisome), and others.
Saccharomyces boulardii benefits
Saccharomyces boulardii and diarrhea
Acute diarrhea
Two randomized controlled trials using Saccharomyces boulardii showed that this probiotic may be effective in treating acute adult diarrhea due to a variety of causes and can significantly lower diarrhea severity score compared with controls 32. Unfortunately, since the number of trials in this area is small and the causes were different in the two trials, only limited conclusions can be reached.
A recent randomized controlled trial conducted in 100 hospitalized children showed that Saccharomyces boulardii treatment for 5 days significantly reduces the mean duration of acute diarrhea and frequency of stools, and normalizes stool consistency 33. One randomized controlled trial regarding the efficacy of Saccharomyces boulardii for the prevention of acute diarrhea involved 100 children with acute watery diarrhea and reported a significant difference in the incidence of diarrheal episodes in the group receiving Saccharomyces boulardii compared with the control group during 2 months follow up 34.
A meta-analysis based on 5 randomized controlled trials (619 participants) 34 indicated that Saccharomyces boulardii significantly reduces the duration of acute childhood diarrhea and the risk of prolonged diarrhea compared with control 35. A meta-analysis of seven randomized controlled trials (944 participants) showed a reduction in the duration of acute childhood diarrhea by approximately 1 day in those treated with Saccharomyces boulardii compared with placebo 36. The absence of blinding as well as other factors such as ambulatory care may explain why Saccharomyces boulardii had no effect in a European randomized controlled trial 37. In summary, the findings from randomized controlled trials and guidelines from professional pediatric societies indicate that Saccharomyces boulardii may be an effective adjunct therapy in managing acute gastroenteritis in children 38.
Persistent diarrhea
Results from two clinical trials indicate that Saccharomyces boulardii improves outcomes in children with persistent diarrhea 39. The relative significant reduction in persistent diarrhea in the Saccharomyces boulardii group compared with controls was approximately 50% 40. These results indicate that Saccharomyces boulardii is useful in the management of persistent diarrhea in children. However, studies with larger populations are needed to determine whether Saccharomyces boulardii therapy alone is also effective in children with persistent diarrhea.
Traveler’s diarrhea
A meta-analysis of 12 randomized controlled trials of various probiotics (including Saccharomyces boulardii) for the prevention of traveler’s diarrhea found a significant reduction in the risk of traveler’s diarrhea when probiotics are used 41. The relative significant reduction in traveler’s diarrhea in the Saccharomyces boulardii group compared with controls in two randomized controlled trials ranged between 5% and 11% 42. These limited numbers of studies indicate that probiotics may be more effective in preventing traveler’s diarrhea, rather than treating diarrhea once it becomes symptomatic.
Diarrhea is a significant problem in patients on total enteral nutrition (TEN) and may involve changes in intestinal short chain fatty acids (SCFAs) 43. Schneider and colleagues reported a significant increase in short chain fatty acids (SCFAs) in 10 enteral-fed patients receiving Saccharomyces boulardii compared with 15 healthy controls 43. Saccharomyces boulardii-induced increase of fecal short chain fatty acid concentrations may explain the preventive effects of this yeast on total enteral nutrition (TEN)-induced diarrhea 43. In three randomized controlled trials the relative significant reduction in enteral nutrition-related diarrhea in the Saccharomyces boulardii group compared with controls ranged between 5% and 8.2% 44. More studies are needed to elucidate the mechanisms of how Saccharomyces boulardii can prevent total enteral nutrition (TEN)-induced diarrhea.
Antibiotic-associated diarrhea
Antibiotic-associated diarrhea is defined as otherwise unexplained diarrhea that occurs in association with the administration of antibiotics 45. Measures to prevent antibiotic-associated diarrhea include the use of probiotics. Of the 10 controlled trials in adults using Saccharomyces boulardii for the prevention of antibiotic-associated diarrhea, 8 (80%) showed significant efficacy for the prevention of antibiotic-associated diarrhea 46. The protective effect of Saccharomyces boulardii and the significant relative reduction in antibiotic-associated diarrhea compared with controls ranged between 7.4% and 25% 46. Other studies failed to demonstrate a significant protective effect of Saccharomyces boulardii and this may be secondary to short or no follow-up after antibiotic exposure 47. Two randomized controlled trials have assessed the ability of Saccharomyces boulardii to prevent antibiotic-associated diarrhea in children and the relative significant increase in prevention of antibiotic-associated diarrhea in the Saccharomyces boulardii group compared with controls ranged between 7.6% and 30.1% 48.
A recent meta-analysis of the 10 randomized, controlled trials in adults found that Saccharomyces boulardii was significantly protective for antibiotic-associated diarrhea with a pooled relative risk of 0.47 46. Relative risk or risk ratio (RR) is the ratio of the probability of an event occurring (for example, developing a disease, being injured) in an exposed group to the probability of the event occurring in a comparison, non-exposed group. A relative risk of less than 1 means the event is less likely to occur in the experimental group than in the control group. Finally, in another meta-analysis from five trials involving 1076 subjects, a significantly protective effect of Saccharomyces boulardii was found (pooled RR = 0.43) 49. However, although many meta-analyses have concluded that probiotics are effective for preventing antibiotic-associated diarrhea 47, most probiotic meta-analyses have focused on one type of disease indication (e.g. antibiotic associated diarrhea) with a variety of probiotic strains. Thus, the summarized data from meta-analyses that are focused only on the use of Saccharomyces boulardii in preventing antibiotic-associated diarrhea and conclude that this probiotic is efficacious for this indication.
Patients with HIV-associated diarrhea seem to be one group that requires a higher than typical dose of Saccharomyces boulardii. In a blinded, placebo-controlled study in 11 HIV-positive patients who had chronic diarrhea, lower doses of Saccharomyces boulardii were not as effective compared with 6 patients who reported that diarrhea was controlled while taking 3 g/day Saccharomyces boulardii after 1 month 50. In a randomized controlled trial of 35 adult patients with acquired immune deficiency syndrome (AIDS) and chronic diarrhea, 61% of patients given Saccharomyces boulardii had their diarrhea resolved compared with patients on placebo (12%) 51. Further confirmation on whether higher doses of Saccharomyces boulardii may benefit patients with HIV-related diarrhea is needed since this observation is based on very limited data.
Crohn’s disease
Recently, the use of probiotics for maintaining remission from active disease in patients with Crohn’s disease was given a ‘C’ recommendation rating level by a panel of experts evaluating the efficacy of the supplements, mostly due to a scarcity of data 52. In a small pilot study of 31 patients with Crohn’s disease in remission all patients continued their maintenance medications and were randomized to either Saccharomyces boulardii for 3 months or placebo [Garcia et al. 2008]. Those treated with Saccharomyces boulardii were found to have a significant reduction in colonic permeability compared with those given placebo, thus reducing the risk of bacterial translocation in these patients 53. Two randomized controlled trials tested Saccharomyces boulardii for patients with Crohn’s disease 54. In a small randomized study of 20 patients with Crohn’s disease all patients continued their maintenance medications and were randomized to either Saccharomyces boulardii for 7 weeks or placebo. Patients treated with Saccharomyces boulardii were significantly improved compared with the placebo group 55. Finally, in a study of 32 patients with Crohn’s disease who were in remission, significantly fewer patients treated with Saccharomyces boulardii (6%) relapsed than the control group (38%) 54. Further studies to establish the efficacy of Saccharomyces boulardii in treatment of Crohn’s disease are needed.
Ulcerative colitis
Probiotics have been used as an adjunct treatment in an attempt to induce remission in patients with active ulcerative colitis flares 56. In a small pilot study of 25 adults with mild to moderate ulcerative colitis that were treated with a combination of mesalazine and Saccharomyces boulardii for 4 weeks, most (68%) of the patients responded to the probiotic treatment 57. This pilot study had a promising result, but the implications were uncertain as patients were treated for only a short time, were not followed up for subsequent disease flare ups, and no control group was included. In a small pilot study of 6 patients with ulcerative colitis, a therapeutic regimen including Saccharomyces boulardii and rifaximin for 3 months seemed effective in preventing early flare ups of ulcerative colitis 58. Further controlled studies on a larger number of patients treated for longer periods with this probiotic agent are warranted. Overall, based upon current consensus, the level of evidence for use of probiotics either to maintain remission or induce remission of ulcerative colitis symptoms is presently limited to a ‘C’ rating 52.
Irritable bowel syndrome
Recent evidence suggests a role of the microflora in irritable bowel syndrome (IBS) pathogenesis 59. A meta-analysis of 20 RCTs including 1404 subjects found a pooled relative risk (RR) for improvement in global IBS symptoms in 14 probiotic treatment arms (RR = 0.77) 60. In a double-blind trial of Saccharomyces boulardii versus placebo in the treatment of IBS patients, the probiotic agent significantly improved the quality of life, but did not improve intestinal symptoms 61. These findings are inconsistent with those reported in double-blind, randomized controlled trials performed earlier in France 62. Along these lines, a recent retrospective analysis suggested that addition of Saccharomyces boulardii to mebeverine can provide superior results in IBS treatment and that the probiotic agent does exert beneficial effects on the quality of life and IBS symptoms 63. More trials using Saccharomyces boulardii for IBS are required to allow solid conclusions for its use in this condition.
Parasitic infections
Little is known about the efficacy of Saccharomyces boulardii against protozoal infections but this probiotic seems to have a beneficial effect in amebiasis, giardiasis and infection with Blastocystis hominis. In adults, co-administration of lyophilized Saccharomyces boulardii with conventional treatment in acute amebic colitis significantly decreased the duration of symptoms and cyst carriage after 4 weeks 64. A prospective randomized controlled trial in patients with amebic colitis showed that addition of Saccharomyces boulardii to metronidazole enhanced clearance of cysts and decreased the mean duration of diarrhea, fever and abdominal pain 65.
In a small clinical study of symptomatic children with Blastocystis hominis infection Saccharomyces boulardii had potential beneficial effects in symptoms and number of parasites 66.
The combination therapy of Saccharomyces boulardii in addition to metronidazole in patients with giardiasis resulted in a disappearance of Giardia cysts 2 weeks after start of the treatment in contrast to 17.1% of patients treated with 10 days metronidazole as monotherapy who still had Giardia lamblia cysts in the stool 67. In another clinical trial of 40 children who received tinidazole for giardiasis of 3 or 4 weeks duration, the percentage of children with only one to three bowel movements per day was significantly higher in the Saccharomyces boulardii group compared with the placebo group (65% versus 15%) 40. However, all of the studies regarding use of Saccharomyces boulardii for treatment of parasitic infections are small and the reported results need to be confirmed by larger studies.
Saccharomyces boulardii dosage
Saccharomyces boulardii at 5 to 40 billion colony forming units/day may be appropriate given the modest number needed to treat to prevent one case of diarrhea is ten and the likelihood that adverse events are very rare 68.
Adults by mouth:
- For diarrhea in people taking antibiotics: 250-500 mg of Saccharomyces boulardii taken 2-4 times daily for up to 2 weeks is most commonly used. In most cases, daily doses do not exceed 1000 mg daily.
- For diarrhea caused by Clostridium difficile: For preventing recurrence, 500 mg of Saccharomyces boulardii twice daily for 4 weeks along with antibiotic treatment has been used.
- For diarrhea caused by Helicobacter pylori: 500-1000 mg of Saccharomyces boulardii daily for 1-4 weeks is most commonly used.
- For diarrhea associated with HIV: 3 grams of Saccharomyces boulardii daily.
- For traveler’s diarrhea: 250-1000 mg of Saccharomyces boulardii daily for 1 month.
Children by mouth:
- For diarrhea in people taking antibiotics: 250 mg of Saccharomyces boulardii once or twice daily for the duration of antibiotics has been used.
- For general diarrhea: For treating acute diarrhea, 250 mg of Saccharomyces boulardii once or twice daily for 5 days has been used. For treating persistent diarrhea, 1750 billion to 175 trillion colony-forming units of Saccharomyces boulardii twice daily for 5 days has been used. For preventing diarrhea in people receiving tube feedings, 500 mg of Saccharomyces boulardii four times daily has been used.
- For rotaviral diarrhea: 200-250 mg of Saccharomyces boulardii twice daily for 5 days has been used.
Saccharomyces boulardii side effects
Although no adverse effects were observed in any of the clinical trials with Saccharomyces boulardii, the administration of Saccharomyces boulardii is not without risk. A recent systematic review documented that probiotic products such as Saccharomyces boulardii, have been shown to increase the risk of complications in specific patient groups such as immunocompromised subjects 69. Saccharomyces fungemia is the most severe complication secondary to administration of the probiotic especially in patients with severe general or intestinal disease who had an indwelling catheter 70.
Up to now, almost 100 cases of Saccharomyces boulardii-associated fungemia have been reported 71. The origin of the fungemia is thought to be either a digestive tract translocation or a contamination of the central venous line by the colonized hands of health workers 72. Indeed, the simple act of opening a packet of Saccharomyces boulardii can produce air contamination that may pose environmental risk especially for immunocompromised patients 70. Once the diagnosis is made, fungemia with Saccharomyces boulardii can effectively be treated with antimycotic medication, although treatment failure with fluconazole has been reported 73.
A rare gastrointestinal allergic reaction was also recently reported after Saccharomyces boulardii was given to an infant with a prior diagnosis of food protein-induced enterocolitis syndrome 74.
Pregnancy and breast-feeding: There is not enough reliable information about the safety of taking Saccharomyces boulardii if you are pregnant or breast feeding. Stay on the safe side and avoid use.
Overall, Saccharomyces boulardii is safe for use in otherwise healthy populations and fungemia with Saccharomyces boulardii has not been reported, to the best of the authors’ knowledge, in immunocompetent patients 75. Caution should be taken in patients with risk factors for adverse events (e.g. patients with central venous catheters or increased bacterial translocation) 76. Institutional guidelines are needed to address the potential safety issues related to Saccharomyces boulardii use 76.
References- Probiotics. http://www.fao.org/food/food-safety-quality/a-z-index/probiotics/en/
- Probiotics in food. Health and nutritional properties and guidelines for evaluation. FAO FOOD AND NUTRITION PAPER 85. http://www.fao.org/3/a-a0512e.pdf
- Sanders ME. How do we know when something called “probiotic” is really a probiotic? A guideline for consumers and health care professionals. Functional Food Reviews. 2009;1:3–12.
- California daily research foundation and dairy and food culture technologies; 2007. http://cdrf.org/home/checkoff-investments/usprobiotics/
- Graf C, Gavazzi G. Saccharomyces cerevisiae fungemia in an immunocompromised patient not treated with Saccharomyces boulardii preparation. J Inf Secur. 2007;54(3):310–311.
- Enache-Angoulvant A, Hennequin C. Invasive Saccharomyces infection: a comprehensive review. Clin Infect Dis. 2005;41(11):1559–1568. doi: 10.1086/497832
- Doron S, Snydman DR. Risk and safety of probiotics. Clin Infect Dis. 2015;60:S129–S134. doi: 10.1093/cid/civ085
- Wan CM, Yu H, Liu G, et al. A multicenter randomized controlled study of Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea in infants and young children. Zhonghua Er Ke Za Zhi. 2017;55:349–354. doi:10.3760/cma.j.issn.0578-1310.2017.05.008
- Villar-Garcia J, Hernandez JJ, Guerri-Fernandez R, et al. Effect of probiotics (Saccharomyces boulardii) on microbial translocation and inflammation in HIV-treated patients: a double-blind, randomized, placebo-controlled trial. J Acquir Immune Defic Syndr. 2015;68:256–263. doi:10.1097/QAI.0000000000000468
- Wang F, Feng J, Chen P, et al. Probiotics in Helicobacter pylori eradication therapy: systematic review and network meta-analysis. Clin Res Hepatol Gastroenterol. 2017;41:466–475. doi:10.1016/j.clinre.2017.04.004
- Graff S, Chaumeil JC, Boy P, Lai-Kuen R, Charrueau C. Influence of pH conditions on the viability of Saccharomyces boulardii yeast. J Gen Appl Microbiol. 2008;54:221–227. https://www.jstage.jst.go.jp/article/jgam/54/4/54_4_221/_pdf/-char/en
- Breves G, Faul K, Schroder B, et al. Application of the colon-simulation technique for studying the effects of Saccharomyces boulardii on basic parameters of porcine cecal microbial metabolism disturbed by clindamycin. Digestion. 2000;61:193–200. doi:10.1159/000007757
- Buts JP, De Keyser N, Stilmant C, et al. Saccharomyces boulardii produces in rat small intestine a novel protein phosphatase that inhibits Escherichia coli endotoxin by dephosphorylation. Pediatr Res. 2006;60:24–29. doi:10.1203/01.pdr.0000220322.31940.29
- Tiago FC, Martins FS, Souza EL, et al. Adhesion to the yeast cell surface as a mechanism for trapping pathogenic bacteria by Saccharomyces probiotics. J Med Microbiol. 2012;61:1194–1207. doi:10.1099/jmm.0.042283-0
- Czerucka D, Rampal P. Effect of Saccharomyces boulardii on cAMP- and Ca2+ -dependent Cl- secretion in T84 cells. Dig Dis Sci. 1999;44:2359–2368
- Terciolo C, Dobric A, Ouaissi M, et al. Saccharomyces boulardii CNCM I-745 restores intestinal barrier integrity by regulation of E-cadherin recycling. J Crohns Colitis. 2017;11:999–1010. doi:10.1093/ecco-jcc/jjx030
- Yu L, Zhao XK, Cheng ML, et al. Saccharomyces boulardii administration changes gut microbiota and attenuates D-galactosamine-induced liver injury. Sci Rep. 2017;7:1359. doi:10.1038/s41598-017-01271-9
- Stier H, Bischoff SC. Influence of Saccharomyces boulardii CNCM I-745 on the gut-associated immune system. Clin Exp Gastroenterol. 2016;9:269–279. doi:10.2147/CEG.S111003
- Schneider SM, Girard-Pipau F, Filippi J, et al. Effects of Saccharomyces boulardii on fecal short-chain fatty acids and microflora in patients on long-term total enteral nutrition. World J Gastroenterol. 2005;11:6165–6169
- Gedek BR. Adherence of Escherichia coli serogroup O 157 and the Salmonella typhimurium mutant DT 104 to the surface of Saccharomyces boulardii. Mycoses. 1999;42:261–264
- Swidsinski A, Loening-Baucke V, Schulz S, et al. Functional anatomy of the colonic bioreactor: impact of antibiotics and Saccharomyces boulardii on bacterial composition in human fecal cylinders. Syst Appl Microbiol. 2016;39:67–75. doi:10.1016/j.syapm.2015.11.002
- Hudson LE, McDermott CD, Stewart TP, et al. Characterization of the probiotic yeast Saccharomyces boulardii in the healthy mucosal immune system. PLoS ONE. 2016;11:e0153351. doi:10.1371/journal.pone.0153351
- Atıcıa S, Soysala A, Karadeniz Ceritb K, Yılmazc S, Aksuc B, Kıyanb G, Bakır M. Catheter-related Saccharomyces cerevisiae fungemia following Saccharomyces boulardii probiotic treatment: in a child in intensive care unit and review of the literature. Med Mycol Case Rep. 2017;15:33–35. doi: 10.1016/j.mmcr.2017.02.002
- Martin IW, Tonner R, Trivedi J, et al. Saccharomyces boulardii probiotic-associated fungemia: questioning the safety of this preventive probiotic’s use. Diagn Microbiol Infect Dis. 2017;87:286–288. doi: 10.1016/j.diagmicrobio.2016.12.004
- Venugopalan V, Shriner KA, Wong-Beringer A. Regulatory Oversight and Safety of Probiotic Use. Emerging Infectious Diseases. 2010;16(11):1661-1665. doi:10.3201/eid1611.100574
- Sulik-Tyszka B, Snarski E, Niedźwiedzka M, et al. Experience with Saccharomyces boulardii Probiotic in Oncohaematological Patients. Probiotics and Antimicrobial Proteins. 2018;10(2):350-355. doi:10.1007/s12602-017-9332-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5973998/
- Food and Drug Administration. Federal Food, Drug, and Cosmetic Act (FD&C Act). 21 U.S.C. 321. Sect 201
- Food and Drug Administration. Development & approval process (drugs). https://www.fda.gov/Drugs/DevelopmentApprovalProcess/default.htm
- Food and Drug Administration. Overview of dietary supplements. https://www.fda.gov/default.htm
- Dietary Supplement Health and Education Act, Pub L. No.103-417
- Current Good Manufacturing Practice in Manufacturing, Packaging, Labeling, or Holding Operations for Dietary Supplements. 21 C.F.R. 111, 2007.
- Efficacy of saccharomyces boulardii with antibiotics in acute amoebiasis. Mansour-Ghanaei F, Dehbashi N, Yazdanparast K, Shafaghi A. World J Gastroenterol. 2003 Aug; 9(8):1832-3.
- Effect of Saccharomyces boulardii in the treatment of acute watery diarrhea in Myanmar children: a randomized controlled study. Htwe K, Yee KS, Tin M, Vandenplas Y. Am J Trop Med Hyg. 2008 Feb; 78(2):214-6.
- Role of a probiotic (Saccharomyces boulardii) in management and prevention of diarrhoea. Billoo AG, Memon MA, Khaskheli SA, Murtaza G, Iqbal K, Saeed Shekhani M, Siddiqi AQ. World J Gastroenterol. 2006 Jul 28; 12(28):4557-60.
- Szajewska H., Skorka A., Dylag M. (2007) Meta-analysis: Saccharomyces boulardii for treating acute diarrhoea in children. Aliment Pharmacol Ther 25: 257–264
- Saccharomyces boulardii for treating acute gastroenteritis in children: updated meta-analysis of randomized controlled trials. Szajewska H, Skórka A. Aliment Pharmacol Ther. 2009 Nov 1; 30(9):960-1.
- Probiotics for treatment of acute diarrhoea in children: randomised clinical trial of five different preparations. Canani RB, Cirillo P, Terrin G, Cesarano L, Spagnuolo MI, De Vincenzo A, Albano F, Passariello A, De Marco G, Manguso F, Guarino A. BMJ. 2007 Aug 18; 335(7615):340.
- European Society for Paediatric Gastroenterology, Hepatology, and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe. Guarino A, Albano F, Ashkenazi S, Gendrel D, Hoekstra JH, Shamir R, Szajewska H, European Society for Paediatric Gastroenterology, Hepatology, and Nutrition., European Society for Paediatric Infectious Diseases. J Pediatr Gastroenterol Nutr. 2008 May; 46 Suppl 2():S81-122.
- Effect of Lactobacillus strains and Saccharomyces boulardii on persistent diarrhea in children. Gaón D, García H, Winter L, Rodríguez N, Quintás R, González SN, Oliver G. Medicina (B Aires). 2003; 63(4):293-8.
- Castaneda C., Garcia E., Santa Cruz M., Fernandez M., Monterrey P. (1995) Effects of Saccharomyces boulardii in children with chronic diarrhea, especially cases due to giardiasis. Rev Mex Pueric Pediatr 2: 12–16
- Meta-analysis of probiotics for the prevention of traveler’s diarrhea. McFarland LV. Travel Med Infect Dis. 2007 Mar; 5(2):97-105.
- Kollaritsch H., Kremsner P., Wiedermann G., Scheiner O. (1989) Prevention of traveller’s diarrhea: comparison of different non-antibiotic preparations. Travel Med Internat 7: 9–18
- Schneider S.M., Girard-Pipau F., Filippi J., Hebuterne X., Moyse D., Hinojosa G.C., et al. (2005) Effects of Saccharomyces boulardii on fecal short-chain fatty acids and microflora in patients on long-term total enteral nutrition. World J Gastroenterol 11: 6165–6169
- Saccharomyces boulardii prevents diarrhea in critically ill tube-fed patients. A multicenter, randomized, double-blind placebo-controlled trial. Bleichner G, Bléhaut H, Mentec H, Moyse D. Intensive Care Med. 1997 May; 23(5):517-23.
- Bartlett J.G. (2002) Clinical practice. Antibiotic-associated diarrhea. N Engl J Med 346: 334–339
- McFarland L.V. (2010) Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol 16: 2202–2222
- McFarland L.V. (2009) Unraveling the causes of negative studies: a case of S boulardii for the prevention of antibiotic-associated diarrhea. Rev Med Chil 137: 719–720
- Can M., Besirbellioglu B.A., Avci I.Y., Beker C.M., Pahsa A. (2006) Prophylactic Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea: a prospective study. Med Sci Monit 12: I19-I22
- Szajewska H., Mrukowicz J. (2005) Meta-analysis: non-pathogenic yeast Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea. Aliment Pharmacol Ther 22: 365–372
- Elmer G.W., Moyer K.A., Vega R., Surawicz C.M., Collier A.C., Hooton T.M., et al. (1995) Evaluation of Saccharomyces boulardii for patients with HIV-related chronic diarrhoea and in healthy volunteers receiving antifungals. Microb Ther 25: 23–31
- Saint-Marc T., Rossello-Prats L., Touraine J.L. (1991) [Efficacy of Saccharomyces boulardii in the treatment of diarrhea in AIDS]. Ann Med Interne (Paris) 142: 64–65
- Floch M.H., Walker W.A., Guandalini S., Hibberd P., Gorbach S., Surawicz C., et al. (2008) Recommendations for probiotic use—2008. J Clin Gastroenterol 42(Suppl. 2): S104-S108
- Garcia V.E., De Lourdes De, Abreu F., Oswaldo Da, Gama T.H., Guerra P.A., Carolina Carneiro A.A., Paiva M.F., et al. (2008) Influence of Saccharomyces boulardii on the intestinal permeability of patients with Crohn’s disease in remission. Scand J Gastroenterol 43: 842–848
- Guslandi M., Mezzi G., Sorghi M., Testoni P.A. (2000) Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci 45: 1462–1464
- Plein K., Hotz J. (1993) Therapeutic effects of Saccharomyces boulardii on mild residual symptoms in a stable phase of Crohn’s disease with special respect to chronic diarrhea—a pilot study. Z Gastroenterol 31: 129–134
- Cain A.M., Karpa K.D. (2011) Clinical utility of probiotics in inflammatory bowel disease. Altern Ther Health Med 17: 72–79
- Guslandi M., Giollo P., Testoni P.A. (2003) A pilot trial of Saccharomyces boulardii in ulcerative colitis. Eur J Gastroenterol Hepatol 15: 697–698
- Guslandi M. (2010) Saccharomyces boulardii plus rifaximin in mesalamine-intolerant ulcerative colitis. J Clin Gastroenterol 44:385
- Parkes G.C., Brostoff J., Whelan K., Sanderson J.D. (2008) Gastrointestinal microbiota in irritable bowel syndrome: their role in its pathogenesis and treatment. Am J Gastroenterol 103: 1557–1567
- McFarland L.V., Dublin S. (2008) Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol 14: 2650–2661
- Choi C.H., Jo S.Y., Park H.J., Chang S.K., Byeon J.S., Myung S.J. (2011) A randomized, double-blind, placebo-controlled multicenter trial of Saccharomyces boulardii in irritable bowel syndrome: effect on quality of life. J Clin Gastroenterol, in press
- Bennani A. (1990) Randomised trial of Saccharomyces boulardii in the treatment of functional colon disorders. L’Objectif Medical 73: 56–61
- Guslandi M. (2011) Treatment of irritable bowel syndrome with Saccharomyces boulardii. J Clin Gastroenterol, in press
- Mansour-Ghanaei F., Dehbashi N., Yazdanparast K., Shafaghi A. (2003) Efficacy of Saccharomyces boulardii with antibiotics in acute amoebiasis. World J Gastroenterol 9: 1832–1833
- Dinleyici E.C., Eren M., Yargic Z.A., Dogan N., Vandenplas Y. (2009) Clinical efficacy of Saccharomyces boulardii and metronidazole compared with metronidazole alone in children with acute bloody diarrhea caused by amebiasis: a prospective, randomized, open label study. Am J Trop Med Hyg 80: 953–955
- Dinleyici E.C., Eren M., Dogan N., Reyhanioglu S., Yargic Z.A., Vandenplas Y. (2011) Clinical efficacy of Saccharomyces boulardii or metronidazole in symptomatic children with Blastocystis hominis infection. Parasitol Res 108: 541–545
- Besirbellioglu B.A., Ulcay A., Can M., Erdem H., Tanyuksel M., Avci I.Y., et al. (2006) Saccharomyces boulardii and infection due to Giardia lamblia. Scand J Infect Dis 38: 479–481
- Goldenberg JZ, Lytvyn L, Steurich J, Parkin P, Mahant S, Johnston BC. Probiotics for the prevention of pediatric antibiotic‐associated diarrhea. Cochrane Database of Systematic Reviews 2015, Issue 12. Art. No.: CD004827. DOI: 10.1002/14651858.CD004827.pub4
- Whelan K., Myers C.E. (2010) Safety of probiotics in patients receiving nutritional support: a systematic review of case reports, randomized controlled trials, and nonrandomized trials. Am J Clin Nutr 91: 687–703
- Hennequin C., Kauffmann-Lacroix C., Jobert A., Viard J.P., Ricour C., Jacquemin J.L., et al. (2000) Possible role of catheters in Saccharomyces boulardii fungemia. Eur J Clin Microbiol Infect Dis 19: 16–20
- Vandenplas Y., Brunser O., Szajewska H. (2009) Saccharomyces boulardii in childhood. Eur J Pediatr 168: 253–265
- Herek O., Kara I.G., Kaleli I. (2004) Effects of antibiotics and Saccharomyces boulardii on bacterial translocation in burn injury. Surg Today 34: 256–260
- Burkhardt O., Kohnlein T., Pletz M., Welte T. (2005) Saccharomyces boulardii induced sepsis: successful therapy with voriconazole after treatment failure with fluconazole. Scand J Infect Dis 37: 69–72
- Hwang J.B., Kang K.J., Kang Y.N., Kim A.S. (2009) Probiotic gastrointestinal allergic reaction caused by Saccharomyces boulardii. Ann Allergy Asthma Immunol 103: 87–88
- Kelesidis T, Pothoulakis C. Efficacy and safety of the probiotic Saccharomyces boulardii for the prevention and therapy of gastrointestinal disorders. Therapeutic Advances in Gastroenterology. 2012;5(2):111-125. doi:10.1177/1756283X11428502. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296087/
- Venugopalan V., Shriner K.A., Wong-Beringer A. (2010) Regulatory oversight and safety of probiotic use. Emerg Infect Dis 16: 1661–1665