Baby co sleep in bed with parents
Co-sleeping also called bed sharing, is when parents bring their babies into bed with them. However, the term ‘co-sleeping’ is broadly used to refer to children who sleep in close proximity to parents and often includes bed sharing (sharing a sleeping surface with a family member for all or a portion of the sleep period 1. Co-sleeping where parents bring their babies into bed with them can be dangerous for babies. Co-sleeping is associated with an increased risk of sudden unexpected death in infancy (SUDI) including sudden infant death syndrome (SIDS) and fatal sleeping accidents in some circumstances. The safest place for babies to sleep is in a cot next to a parent’s bed, for the first year of life or at least for the first six months. But parents choose to have their babies in bed with them for several reasons. For example, some parents who co-sleep with their babies believe that it helps their babies feel safe and secure. They like the close body contact, feel that it’s rewarding and satisfying, and believe it’s good for their relationships with their babies. Also, some parents co-sleep because they find it more practical. Breastfeeding and resettling during the night can be easier. Some parents feel that it helps with establishing breastfeeding.
Six ways to reduce the risk of sudden unexpected death in infancy (SUDI) and sleep baby safely:
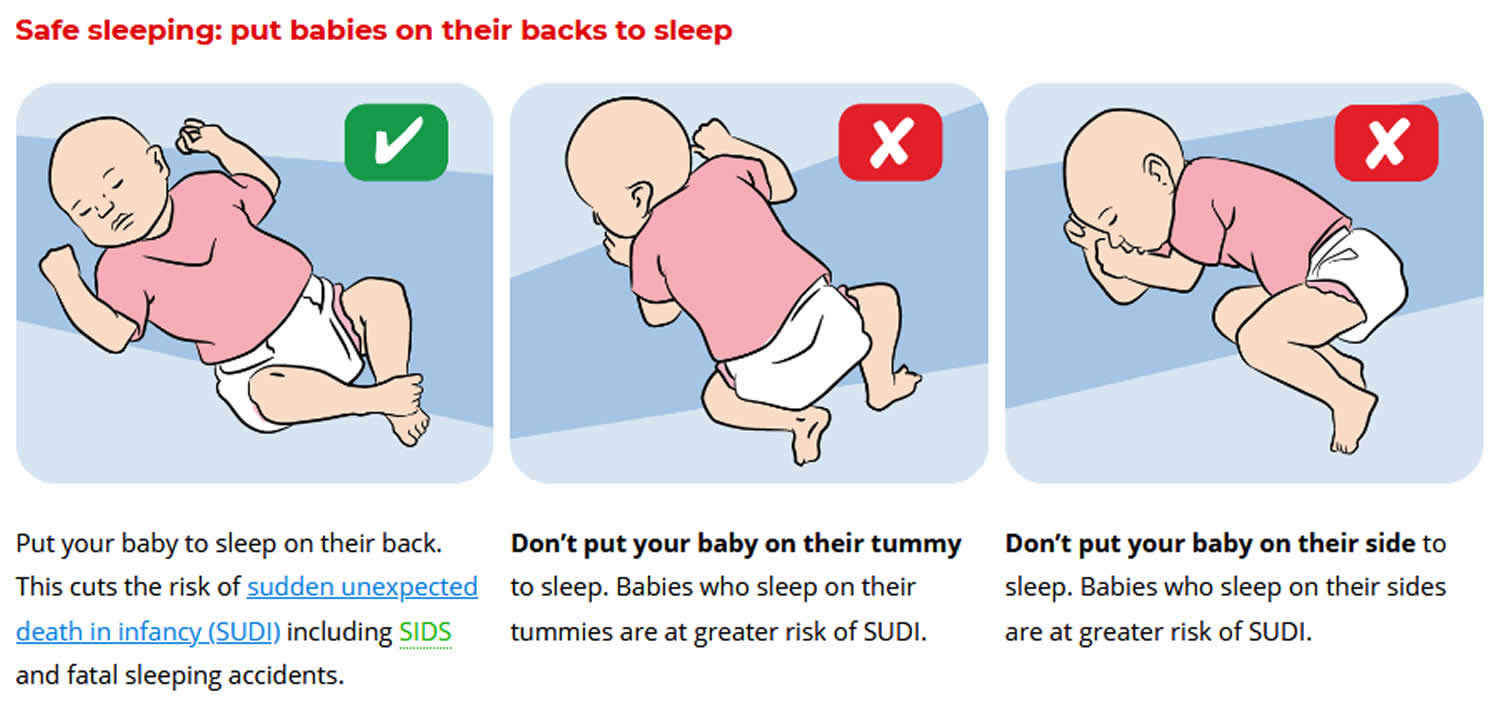
- Sleep baby on the back from birth, not on the tummy or side
- Sleep baby with head and face uncovered
- Keep baby smoke free before birth and after
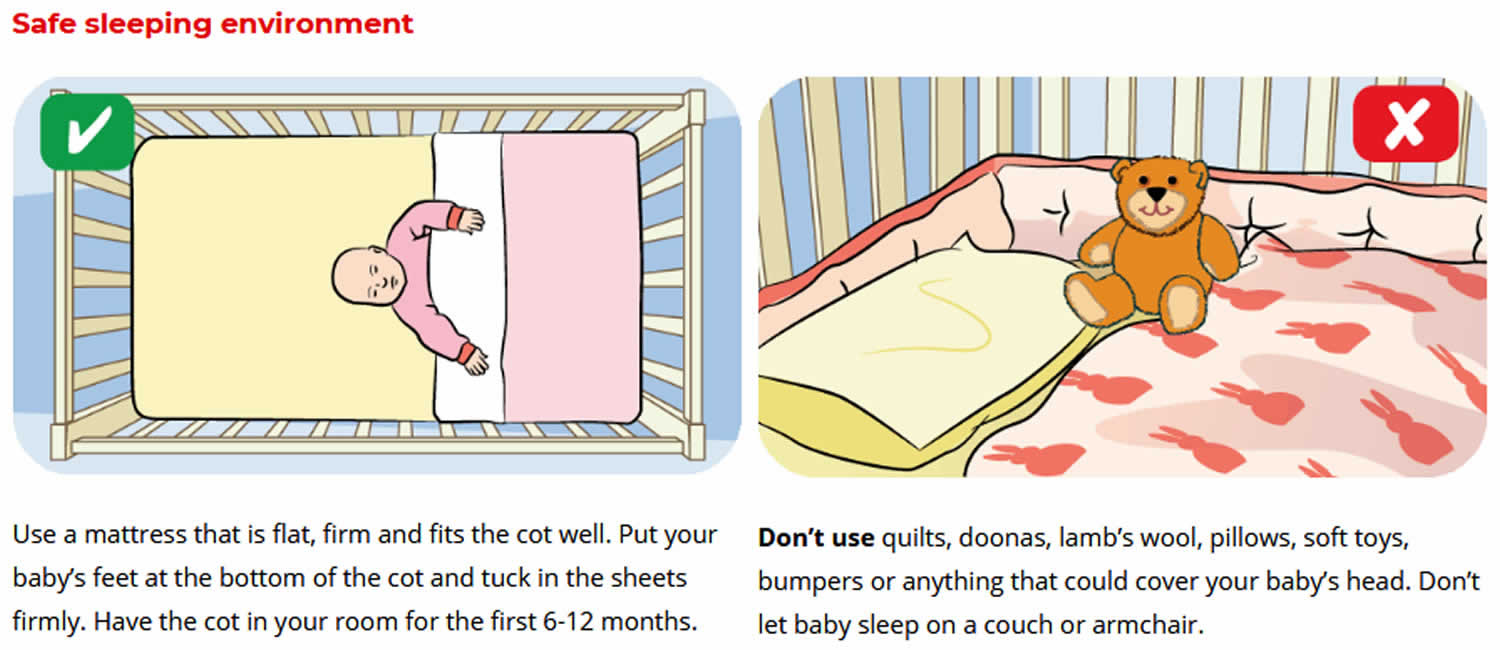
- Provide a safe sleeping environment night and day
- Sleep baby in their own safe sleeping place in the same room as an adult care-giver for the first six to twelve months
- Breastfeed baby
Babies often wake up because they’re worried about being separated from you. A reassuring touch or cuddle can build your baby’s attachment to you and help her learn that you’re close by, even if she can’t see you. As babies develop they gradually overcome this worry.
Parents sometimes bring a baby into bed because the baby is waking or unsettled at night. For some families, this works well. For others, it might work in the short term but can lead to problems with settling the baby later on. Also, the parents’ bed might not be safely set up for the baby.
Co-sleeping might be a problem if there’s a lack of agreement or tension between partners about co-sleeping.
Finally, a problem could come up if parents want their child to sleep in a separate bed before the child wants to move. Many parents who sleep with their children report that children usually want their own beds by the age of 2-3 years. It can take longer than this, though, and sometimes parents want to stop co-sleeping before their child does.
If you’re experiencing any of these problems, co-sleeping might not be the best option for you and your child. There are other options for settling your baby to sleep.
If you’re concerned that your baby isn’t getting enough sleep, you should discuss your concerns with a health care professional by talking with your doctor. It can also be a good idea to track your baby’s sleep for a week or so. This can help you get a clear picture of what’s going on. You can do this by drawing up a simple chart with columns for each day of the week. Divide the days into hourly blocks, and color the intervals when your baby is asleep. Keep your chart for 5-7 days.
Once completed, the chart will tell you things like:
- when your baby is sleeping
- how much sleep your baby is getting
- how many times your baby is waking during the night over the course of a week
- when your baby is waking at night
- how long your baby is taking to settle after waking.
You can also record how you tried to resettle your baby and what worked or didn’t work.
Then you can compare the information in your chart with the general information about baby sleep needs below:
- How does your child compare to other babies the same age? All babies are different, but if your baby is getting much less sleep than others, your baby might be tired and need more opportunities for sleep.
- How many times is your baby waking up during the night? If your baby is waking only once or twice, your baby isn’t that different from most babies the same age. But if it’s 3-4 times a night or more, you might be feeling very tired. You might want to think about changing your baby’s sleep patterns.
If you decide you need to see a professional for help with your baby’s sleep, take your chart with you.
Keep your chart going as you look into ways to handle your baby’s sleep problems. It will allow you to assess your progress and see just how much change is occurring.
Figure 1. Safe sleeping for newborns
How to safely co sleep?
Separate surface co-sleeping where infants do not have to be in the same bed in order to “co-sleep”, such as using a bassinet next to your bed or a crib, where baby and mother or father are within range of detecting each others signals and cues is all that is necessary.
Do recall that co-sleeping with an infant on a couch, recliner or sofa, though also forms of co-sleeping are dangerous and should be avoided as they increase the chances of suffocation, regardless of your sobriety.
Figure 2. How to safely co sleep
What are baby sleep habits?
Baby sleep habits are the things babies need to settle for sleep. Sleep habits can be pacifiers, music, mobiles, fan noise or other white noise, night-lights, rocking, cuddling, feeding and so on.
Baby sleep habits are usually the same at the start of the night and after waking during the night. So if your baby’s sleep habit is being rocked to sleep at the start of the night, she’ll want to be rocked back to sleep in the middle of the night.
Sleep habits aren’t necessarily something you need to phase out or change. But some babies are difficult to settle or wake a lot at night. If this sounds like your baby and it’s something you’d like to change, you could look at your baby’s sleep habits and think about whether a change might help with sleep and settling.
On the other hand, if you’re happy to resettle your baby each time he wakes during the night, that’s just fine.
But babies and toddlers can have trouble settling to sleep by themselves, so they cry. This can happen for many different reasons. Before trying to settle your crying baby, it’s a good idea to first check whether your baby is hungry, uncomfortable or sick.
- Some babies or toddlers cry when they’re tired or overtired and can’t settle to sleep.
- Many babies or toddlers cry when they need help to settle back to sleep after waking in the night.
- Many babies or toddlers cry when they’re getting used to a new or different way of going to sleep.
- Sometimes happy, healthy babies or toddlers develop rapidly, which means they find it harder than usual to settle.
Babies and toddlers who are crying while trying to settle also need comfort.
Identifying your baby’s sleep habits
If you want to phase out your baby’s sleep habits, the first step is to work out what they are. For example, to settle for sleep your baby might need:
- a pacifier
- music or a mobile above her head
- breastfeeding or bottle-feeding
- cuddling or rocking
- a particular place in your home, like the family room.
When you know what your baby’s sleep habits are, the next step is to work on phasing them out. There are tips below for different baby sleep habits.
It’s important to respond to your baby’s or toddler’s needs for:
- Sleep – for example, by putting a baby to sleep when you see baby’s tired signs
- Comfort – for example, by not leaving a crying baby alone for long periods.
Consistently responding to your baby’s or toddler’s needs for both sleep and comfort is an important part of bonding with your baby and helping your child grow up feeling safe, secure and cared for.
Working out how to meet your child’s needs and your needs
There are many ways to meet your child’s needs for both sleep and comfort, as well as your own need for rest. You might have to try a few different approaches to sleep, settling and comforting to work out what’s right for you and your child.
It might help to know that all the strategies on this website are thoroughly researched. The evidence says that these strategies are safe. And if you have plenty of warm and loving interactions with your child while they’re awake, these strategies can support your child’s wellbeing and development, and also your relationship with your child.
Phasing out your baby’s sleep habits
Most babies cry while they’re getting used to a new way of going to sleep. That’s because they like their usual way of getting to sleep and might be upset by change. Be prepared for crying for the first few nights.
It might take anything from three days to three weeks to change baby sleep habits, depending on the approach you use and your baby’s temperament.
After that, sleep usually improves for everyone.
Pacifiers
- Pacifiers can be a tricky sleep habit, especially if your baby loses the pacifier during the night and needs you to find it and put it back in.
- One thing you can do is help your baby learn to manage his own pacifier during the night. But if you want to phase out pacifiers, you can help your baby give up the pacifier.
Music and mobiles
- If your baby’s sleep habit is going to sleep with music playing or a mobile moving overhead, it’s probably best to stop using music or mobiles at bedtime – especially if you have to get out of bed to turn the music or mobile back on in the night.
- You can phase out these sleep habits gradually. For example, you could use music as part of your bedtime routine, but turn it off when your baby starts to look drowsy.
Night feeds
- If your baby routinely falls asleep at the breast or with the bottle, she might depend on feeding to help her get to sleep.
- From six months of age, if your baby is developing well, it’s OK to think about night weaning for breastfed babies and phasing out night feeds for bottle-fed babies.
- But if you’re comfortable with feeding your baby during the night, there’s no hurry to phase out night feeds. You can choose what works best for you and your baby.
Rocking, cuddling or going to sleep in the family room
- Some babies are used to being rocked or cuddled to sleep. Or they might want to be with the rest of the family until they fall asleep – for example, in the family room. These babies might find it hard to resettle when they wake up in a different place from where they went to sleep.
- It can help to put your baby to bed drowsy but awake. This gives him the chance to associate falling asleep with being in bed. And it means he’ll be more likely to settle himself when he wakes in his bed in the night.
- The patting settling technique is one way to help babies learn to go to sleep in their own beds.
Looking after yourself
- Phasing out baby sleep habits can be tiring, so it helps to look after yourself. You could try resting during the day when you can, going to bed early and asking family and friends for help.
How healthcare professionals can help with baby sleep and toddler sleep
First, your healthcare professional will talk with you to understand both the problem and your family’s needs. The professional will ask you about your baby, your concerns about your baby’s sleep, and the things you’ve tried so far.
A good professional always finds out what your goals are for your child and your family – there isn’t a one-size-fits-all solution to baby sleep problems.
Your healthcare professional will then work with you to develop and put in place a baby sleep plan. A good plan covers:
- good bedtime and sleep habits
- positive bedtime routines
- settling strategies that you’re comfortable using.
A good sleep plan also covers what to do if the strategies in your baby sleep plan aren’t working.
The settling strategies in your baby’s sleep plan might seem to upset your baby for the first few nights. This will pass as she gets used to the changes. Before too long, you’ll have a more rested, contented baby. You’ll feel better too. If you’re concerned, contact the professional who gave you the sleep plan.
How much sleep do babies need?
Just like grown-ups, babies all sleep for different amounts of time. But your baby’s mood and wellbeing is often a good guide to whether he’s getting enough sleep.
If your baby is:
- wakeful and grizzly, she probably needs more sleep
- wakeful and contented, she’s probably getting enough sleep.
Remember that your baby is unique. He might be doing fine with more or less sleep than other babies the same age.
As children get older, their night-time sleeps get longer and they need fewer naps during the day. Babies and younger children tend to have shorter sleeps at night and more naps during the day. They often wake during the night to feed and might need help to settle themselves to sleep again.
Babies under 12 months sleep needs
0-3 months
- Most newborns don’t have definite day and night sleep patterns. They’re still learning to tell the difference between day and night.
- Newborns generally sleep for 16-20 hours in a 24-hour period, but they wake every 2-4 hours to be fed. They need lots of feeds because they have tiny tummies.
- Over the first 12 weeks most newborns start to develop day and night sleep patterns. By three months, babies are averaging 14-15 hours of sleep in each 24-hour period.
3-6 months
- At this age, most babies sleep 10-18 hours in a 24-hour period. On average, they sleep around 14 hours.
- Although they’re growing quickly, babies still need to wake for feeding at this age.
- Sleeping patterns vary a lot, but babies generally nap three times during the day. Most babies need help to settle to sleep.
6-12 months
- During these months most babies still sleep for around 14 hours in a 24-hour period.
- Here’s what to expect during the day:
- Most babies nap during the day.
- Naps usually last 1-2 hours. Some babies sleep longer. Up to a quarter of all babies of this age nap for less than an hour.
- And here’s what to expect at night:
- Most babies are ready for bed between 6 pm and 10 pm.
- Most babies take less than 30 minutes to get to sleep.
- Many babies wake during the night and need an adult to settle them back to sleep. About 1 in 10 babies will do this 3-4 times a night.
More than a third of parents say they have problems with their baby’s sleep at this age.
Babies over 12 months sleep needs
At 12-18 months old, babies generally sleep 13-15 hours over a 24-hour period. Most babies have naps twice a day until around 18 months. Around this time babies often go from having two naps to having one longer daytime nap.
Some babies start to resist going to sleep at night, preferring to stay up with the family. This peaks at around 18 months and tends to go away with age.
Factors that increase co-sleeping risks
Co-sleeping always increases the risk of sudden unexpected death in infancy (SUDI) including SIDS (sudden infant death syndrome) and fatal sleeping accidents. Co-sleeping increases this risk even more if:
- you’re very tired or you’re unwell
- you or your partner uses drugs, alcohol or any type of sedative medication that causes heavy sleep
- you or your partner is a smoker
- your baby is unwell
- your baby is less than three months old, or was premature or smaller than most babies at birth.
Sleeping with a baby on a couch or chair is always unsafe. Move your baby to a safe sleep environment if you think you might fall asleep in a chair or couch while holding your baby.
Risk factors for sudden unexpected death in infancy when co-sleeping
Under certain circumstances, some studies have reported an increased risk of sudden unexpected death in infancy (SUDI) in co-sleeping babies. The following risk factors have been identified:
- Smoking: A baby exposed to cigarette smoke (eg if the mother or father smokes, or the mother smoked during pregnancy) increases the risk of SIDS, regardless of where the baby sleeps. Smoking parents (or a mother who smoked during pregnancy) should never co-sleep with their baby 2. Parents who smoke are encouraged to room-share as long as the room the baby sleeps in is kept smoke-free, as their babies have an increased risk of sudden infant death (SIDS) and therefore require closer observation.
- Alcohol, drugs or extreme fatigue: Babies are at increased risk of a fatal sleeping accident if they co-sleep with someone who is has consumed alcohol or illegal or sleep-inducing drugs or who is experiencing extreme fatigue 3. A parent should not co-sleep with their baby if they have consumed alcohol or illegal or sleep-inducing drugs, or when extremely fatigued.
- Sharing a sleeping surface with a sibling(s) or a pet(s): Babies are at increased risk of death if they co-sleep with more persons than their parents (eg other siblings) 4 or with a pet. Co-sleeping with a sibling raises the risk 5. Babies should not co-sleep if anyone other than the parents is in the bed.
- Obesity: Parents who are obese may not be able to feel exactly where or how close their baby is and so may wish to room-share with their baby 6. Obese parents should not co-sleep with their baby.
- Formula-fed babies: Experts recommend that formula-fed babies room-share with their parents rather than co-sleep, because mothers who formula feed their babies do not demonstrate the same responsive night-time parenting practices as breastfeeding mothers 6.
- Sofa-sharing: Using a sofa, couch, beanbag or armchair as a sleeping place for a baby increases the risk of a fatal sleeping accident 6. Caregivers should never co-sleep with a baby on a sofa, couch or armchair. Babies can suffocate against cushions or become wedged between the seat and the back of the sofa whether or not a sleeping adult is present.
- Young baby and overheating or head covering: It has been thought that the risk of death in a young baby who co-sleeps with a parent may be increased if the baby overheats or if the baby’s head becomes covered 7. Some studies have reported a higher risk of death when a young baby (ie under the age of 12 weeks) shares a bed with a parent 8. These studies did not however consider all known risk factors such as alcohol or drug use, or multiple bed-sharers. In addition, the peak age for SIDS has always been within this range no matter where the baby sleeps.
- Baby alone on an adult bed: Leaving a baby unattended on an adult bed also increases the risk of a fatal sleeping accident 9.
- Infant wrapping and swaddling: Do not wrap baby if sharing a sleep surface as this restricts arm and leg movement.
Reducing the risk of sudden unexpected death in infancy including SIDS and fatal sleeping accidents
There are some things you can do to reduce the risk of sudden unexpected death in infancy (SUDI) including SIDS and fatal sleeping accidents if you choose to co-sleep with your baby:
- Put your baby on their back to sleep (never on their tummy or side).
- Make sure the mattress is clean and firm. Don’t use a waterbed, or anything soft underneath – for example, a lamb’s wool underlay or pillows.
- Keep pillows and adult bedding like sheets and blankets away from your baby. Make sure your bedding can’t cover your baby’s face. Consider using a safe infant sleeping bag so your baby doesn’t share adult bedding.
- Use lightweight blankets, not heavy quilts or duvets.
- Never wrap or swaddle your baby if you’re co-sleeping.
- Tie up long hair and remove anything else that could be a strangling risk, including all jewellery and teething necklaces.
- Move the bed away from the wall, so baby can’t get trapped between the bed and wall.
- Make sure your baby can’t fall out of bed. The safest spot is on the side of a big bed, away from the edge. Consider sleeping on your mattress on the floor if it’s possible your baby might roll off the bed.
- Place your baby to the side of one parent, never in the middle of two adults or next to other children or pets. Your baby might get rolled on or overheat.
- Goldberg WA, Keller MA. Parent-infant co-sleeping: why the interest and concern? Infant and Child Development. 2007;16:331–339.
- Vennemann, M.M., Hense, H.W., Bajanowski, T., Blair, P.S., Complojer, C., Moon, R.Y et al 2012, Bed Sharing and the risk of sudden infant death syndrome: can we resolve the debate? Pediatr. 160(1),44-48.e2.
- Carpenter, R.G., Irgens, L.M., Blair, P.S., England, P.D., Fleming, P., Huber, J., Jorch, G., Schreuder, P 2004, Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 363,185-191.
- Hauck, F. R., Herman, S. M., Donovan, M., Iyasu, S., Moore, C., Donoghue, E., et al. (2003). Sleep environment and the risk of sudden infant death syndrome in an urban population: The Chicago Infant Mortality Study. Pediatrics, 111(5), 1207–1214.
- https://cosleeping.nd.edu/frequently-asked-questions
- James J. McKenna and Sarah Mosko. Ch. 16 in Sudden Infant Death Syndrome: Puzzles, Problems and Possibilities. R. Byard and H. Krous, eds. London: Arnold Publishers. https://cosleeping.nd.edu/assets/25448/ch_16_mother_infant.pdf
- Vennemann, M.M., Hense, H.W., Bajanowski, T., Blair, P.S., Complojer, C., Moon, R.Y., et al 2012, Bed Sharing and the risk of sudden infant death syndrome: can we resolve the debate? Pediatr. 160(1),44-48.e2.
- Ruys, J.H., de Jonge, G.A., Brand, R., Engelbert,s A.C., Semmekrot, B.A 2007, Bed-sharing in the first four months of life: a risk factor for sudden infant death. Acta Paediatr 96,1399-1403.
- McKenna, J.J., McDade, T 2005, Why babies should never sleep alone: a review of the co-sleeping controversy in relation to SIDS, bedsharing and breast feeding Paediatr Respir Rev 6(2),134-152.