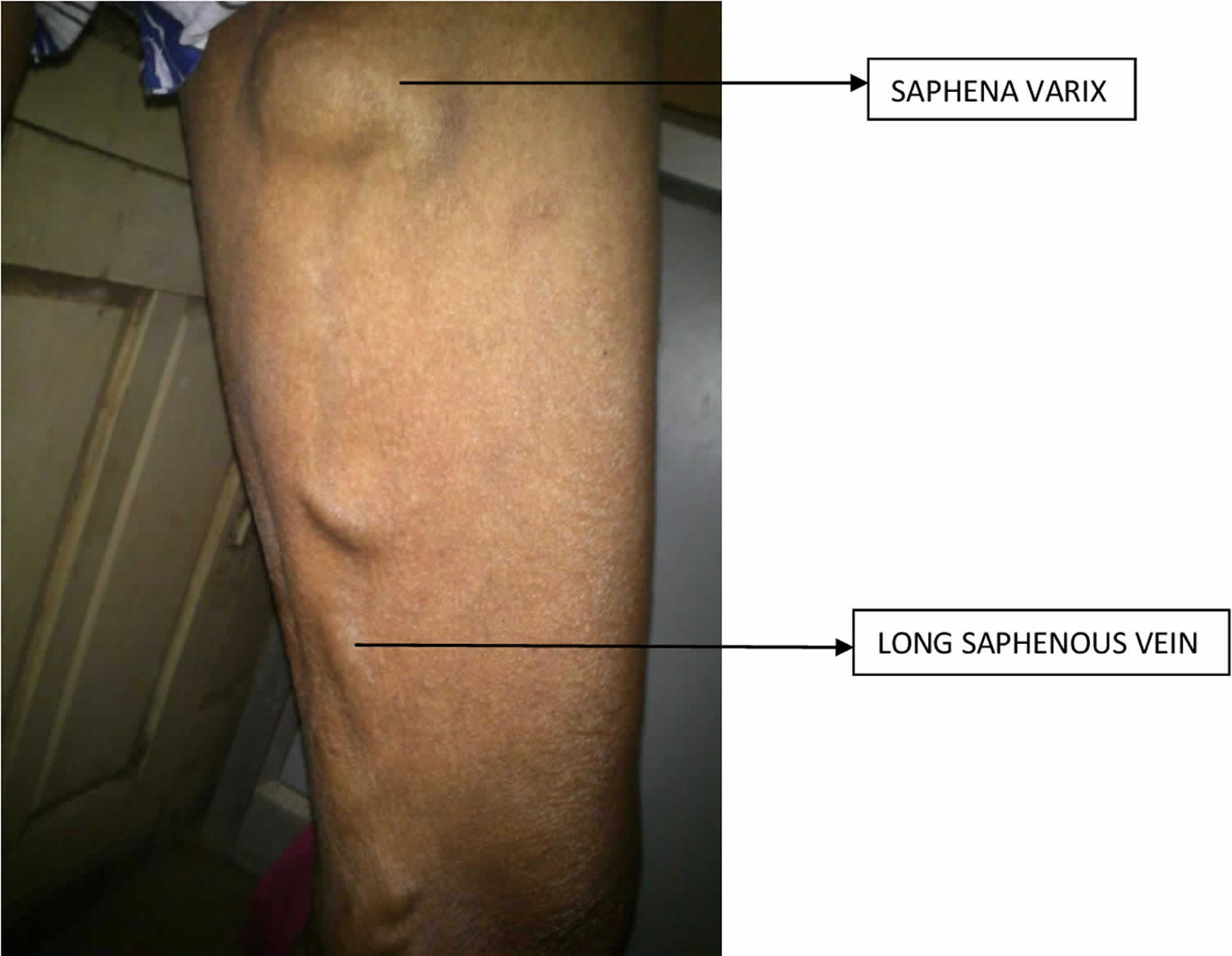
Saphena varix
Saphena varix also called saphenous varix is saccular varicose swelling arising from the proximal end of the long saphenous vein. Saphena varix presents as a reducible swelling in the groin situated in the femoral canal region. A cough impulse may be elicited and the swelling disappears when the patient lies down.
Saphena varix is best described as a solitary area of venous dilatation that communicates with a main venous structure by a single channel, and it must have no association with an arteriovenous communication or a pseudoaneurysm 1. Most importantly, it should not be contained within a segment of varicose vein 2. Saphena varix may occur in the presence or absence of varicose veins 3.
A history of deep vein thrombosis (DVT) and examination findings of other venous varicosities in the leg adds further support to the diagnosis.
There as a classification proposed by Pascarella et al. 4 that divide the great saphena vein aneurysms in four types:
- Type 1 (52%) is located at the proximal third of the saphena vein, but not at saphenofemoral junction.
- Type II aneurysms were located in the shaft of the saphenous vein in the distal third of the thigh (35%).
- Type III of superficial saphenous vein aneurysms was an occurrence of types I and II in the same lower extremity (7%).
- Superficial venous aneurysms of the short saphenous system are classified as type IV (6%).
According to this author, superficial venous aneurysms are found in association with saphenous vein reflux in both men and women 4.
There are several reasons to recommend surgical treatment of most venous aneurysms 2. The most common complications of venous aneurysms are thrombus formation, severe recurrent pulmonary embolism, spontaneous rupture, and thrombophlebitis, but all of them are quite rare 2. Rupture, the most expected complication in arterial aneurysms, has not been reported in peripheral or venous aneurysms of the superficial extremity, but pain, swelling, or undefined mass are common indications for surgery 1. Thromboembolic complications are common in aneurysms involving the deep system 5, however they are very rare in superficial venous aneurysms and therefore not a important reason to indicate surgical treatment.
Several operative techniques have been used in venous aneurysm of the extremities: ligation and simple excision; excision and vein patching; excision with interposition vein or prosthetic grafting; tangential excision with lateral venorrhaphy; autologous vein patch; and complete resection. Due to the low number of cases, it is difficult to establish treatment guidelines on the basis of the experience of one institution. The method of treatment is usually dictated by the anatomical location. In deep vein aneurysms it is preferred to use excision (either tangential or conventional) with reconstruction (either with prostheses or autologous graft). In the superficial system, there is usually no need to reconstruct the vessel 6. Aneurysm resection with venorrhaphy has been associated with subsequent early occlusion and would therefore seem to have little to offer over simple ligation.
Saphena varix causes
The cause of venous aneurysms remains unknown, although several theories have been proposed. Lev and Saphir characterized the structural changes that occurred with age and concluded that there are two changes that can lead to aneurysm formation: endophlebohypertrophy 6 (progressive intimal proliferation of elastic, muscle, and connective tissue), which occurs as a normal response to mechanical stress; and endophlebosclerosis (a degenerative pathologic process characterized by alterations in ground substance, disruption and loss of elastic fibers, loss of medial muscle cells, and fibrosis) [11]. This results from the pressure exerted by the adjacent arterial wall and the flow disturbance produced by continuous pulsations.
Another theory claims that complete absence of medial smooth muscle is clearly congenital 7. This has been associated with decreased amounts of smooth muscle cells and elastin fibers, fibrous connective tissue and elastic fibers in the vein wall 8.
It is likely that a combination of congenital and acquired mechanisms are involved 7. Gillespie et al. 2 noted a reduction in the number and size of muscle and elastic fiber and intimal hyalinization in 4 cases of subcutaneous venous aneurysm. They also described histologic changes in the adjacent nonaneurysmal portions of these veins consisting of intimal hyperplasia, alterations in elastic fiber content, and ground substance with medial hypertrophy 7. A significant diminution in the number and size of muscle and elastic fibers in the walls of these aneurysms is a common finding. Fragmentations of the internal elastic lamella and replacement by fibrous connective tissue have been noted. These findings help to distinguish a venous aneurysm from a varicose vein. In varicose veins, fibrous tissue is increased; in particular the muscle layers and the vessel wall are thickened, and tissue fibrinolytic activity is reduced in the varicose vein 9. Venous aneurysm occurs as a single lesion regardless of sex, age, and site in the body.
Saphena varix symptoms
Saphena varix presents as a reducible swelling in the groin situated in the femoral canal region. A cough impulse may be elicited and the swelling disappears when the patient lies down.
The differential diagnosis for a nontender, fluctuant groin lump with a cough impulse is a hernia or a saphena varix 10. The position of the swelling inferior and lateral to the pubic tubercle narrows the differential to a femoral hernia or saphena varix 11. A history of deep vein thrombosis and examination findings of other venous varicosities in the leg adds further support to the diagnosis. Diagnosis can be confusing clinically, particularly if the varix is thrombosed, and presents as an “irreducible femoral hernia” 12. Femoral hernia by far is the most common differential for saphena varix and is described as herniation of abdominal viscera through the femoral canal. An incarcerated femoral hernia often requires prompt operative management to decrease the risk of bowel strangulation, perforation, and peritonitis. Thrombosed saphena varix has been rarely described in literature.
Saphena varix diagnosis
Saphena varix diagnosis is readily available by duplex ultrasound 3; however, in most cases, the diagnosis is done only in the operative field.
Saphena varix treatment
Treatment of the saphena varix is surgical disconnection and ligation of the saphenofemoral junction. The operative repair is a uniformly successful form of therapy, but satisfactory venous function in the limbs should not be forgotten. Major deep vein occlusion may predispose to venous outflow impedance, venous hypertension, and venous ulceration 8.
Saphena varix surgery
The surgical options available are stripping and ligation of the great saphenous vein, varicose vein ligation, phlebectomy, endovenous vein obliteration, and perforator vein surgery 13.
References- de Miranda JS, Damous SH, Júnior MP, et al. Great saphenous vein aneurysm: A differential diagnosis of femoral hernia and review. Int J Surg Case Rep. 2015;8C:154-157. doi:10.1016/j.ijscr.2015.01.041 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4353965
- Gillespie D.L., Villavicencio J.L., Gallagher C., Chang A., Hamelink J.K., Fiala L.A. Presentation and management of venous aneurysms. J. Vasc. Surg. 1997;26(5):845–852.
- Ekim H., Gelen T., Karpuzoglu G. Multiple aneurysms of the cephalic vein. A case report. Angiology. 1995;46(3):265–267.
- Pascarella L., Al-Tuwaijri M., Bergan J.J., Mekenas L.M. Lower extremity superficial venous aneurysms. Ann. Vasc. Surg. 2005;19(1):69–73.
- Hurwitz R.L., Gelabert H. Thrombosed iliac venous aneurysm: a rare cause of left lower extremity venous obstruction. J. Vasc. Surg. 1989;9(6):822–824.
- Friedman S.G., Krishnasastry K.V., Doscher W., Deckoff S.L. Primary venous aneurysms. Surgery. 1990;108(1):92–95.
- Aldridge S.C., Comerota A.J., Katz M.L., Wolk J.H., Goldman B.I., White J.V. Popliteal venous aneurysm: report of two cases and review of the world literature. J. Vasc. Surg. 1993;18(4):708–715.
- Dawson K., Hamilton G. Primary popliteal venous aneurysm with recurrent pulmonary emboli. J. Vasc. Surg. 1991;14(3):437.
- Calligaro K.D., Ahmad S., Dandora R., Dougherty M.J., Savarese R.P., Doerr K.J. Venous aneurysms: surgical indications and review of the literature. Surgery. 1995;117(1):1–6.
- Scott TE, LaMorte WW, Gorin DR, Menzoian JO. Risk factors for chronic venous insufficiency: A dual case-control study. J Vasc Surg. 1995;22:622–8.
- Zelikovski A, Zamir B, Hadar H, Urca I. Sapheno-femoral valve insufficiency in varicose veins of the lower limb. Angiology. 1981;32:807–11.
- Jamieson WG. State of the art of venous investigation and treatment. Can J Surg. 1993;36:119–28.
- Ravikanth R. Thrombosed Saphena Varix. J Med Ultrasound. 2019;27(1):54-55. doi:10.4103/JMU.JMU_35_18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6445035