Soy allergy
Soy allergy is a common food allergy, but is relatively uncommon compared with peanut, egg or milk allergy. Soy comes from soybeans, which are in the legume family along with beans, lentils, peas, and peanuts. Some people are allergic to just one type of legume; others are allergic to more than one. When someone is allergic to soy, the body’s immune system, which normally fights infections, overreacts to proteins in soy. If the person eats something made with soy, the body thinks these proteins are harmful invaders and responds by working very hard to fight off the invader. This causes an allergic reaction.
Allergy to soy is more common in infants and kids with atopic dermatitis (eczema), than teens and adults, but can develop at any age. Often, soy allergy starts in infancy with reaction to soy-based infant formula. Around 2-3 percent of young children may have positive allergy tests to soy, however less than 10 percent of these will develop symptoms when they eat soy. Although most children may grow out of the soy allergy 1, some carry the allergy into adulthood and sensitization to soy tends to increase rather than diminish with age.
Mild signs and symptoms of soy allergy include hives or itching in and around the mouth. In rare cases, soy allergy can cause a life-threatening allergic reaction (anaphylaxis).
Soy allergy can range from mild to severe. Mild to moderate reactions may be any one or more of the following:
- Hives or welts, swelling of the lips/face/eyes
- Tingling of the mouth
- Abdominal pain or vomiting.
Severe reactions (anaphylaxis) include one or more of the following:
- Difficulty/noisy breathing
- Swelling of the tongue
- Swelling or tightness in the throat
- Difficulty talking and or hoarse voice
- Wheeze or persistent cough
- Persistent dizziness or collapse, pale and floppy (in young children).
It is rare (but possible) for these symptoms to occur alone without hives and/or vomiting. Delayed reactions to soy which are not due to IgE allergy antibodies can cause a flare of eczema and/or bowel symptoms in some children.
If you or your child has a reaction to soy, let your doctor know. Tests can help confirm a soy allergy.
Having a soy allergy means avoiding products that contain soy, which can be difficult. Many foods, such as meat products, bakery goods, chocolate and breakfast cereals, may contain soy.
Highly refined soy oil may not cause a reaction because it doesn’t contain soy proteins. Similarly, you might not react to foods that contain soy lecithin. But generally, if a label includes the word “soy,” avoid it. Products to avoid include, but are not limited to:
- Soy milk, soy cheese, soy ice cream and soy yogurt
- Soy flour
- Tofu
- Miso
- Natto
- Shoyu
- Tempeh
- Soy sauce and tamari
- Edamame
- Vegetable oil, vegetable gum, vegetable broth and vegetable starch
- Cold-pressed, expelled or extruded soy oil. Highly refined soy oil is not required to be labeled as an allergen. Studies show that most people with soy allergy can safely eat highly refined soy oil as well as soy lecithin. If you are allergic to soy, ask your doctor whether you need to avoid soy oil or soy lecithin. But avoid cold-pressed, expelled or extruded soy oil—sometimes called gourmet oils. These ingredients are different and are not safe to eat if you have a soy allergy.
Besides “soy,” “soya” and “soybeans,” other words on food labels may indicate that the product contains soy, including:
- Glycine max
- Hydrolyzed vegetable protein (HVP)
- Hydrolyzed plant protein
- Textured vegetable protein (TVP)
- Monodiglyceride
- Monosodium glutamate (MSG)
- Artificial flavoring
- Natural flavoring
Soy is one of the eight allergens that fall under the labeling requirements of the Food Allergen Labeling and Consumer Protection Act of 2004. This means that manufacturers of packaged food items sold in the United States and containing soy or a soy-based ingredient must state, in clear language, the presence of soy in the product.
Soy or derivatives of soy are found in some infant formulas, canned broths, soups, canned tuna, processed meats and hot dogs, energy bars, baked goods and many other processed foods. Soy also is a common ingredient in Asian cuisine and is sometimes contained in chicken nuggets, low-fat peanut butter, alternative nut butters and even vodka. People with a soy allergy should not consume soy milk, soy yogurt or ice cream, edamame, miso, tempeh and tofu.
Most individuals allergic to soy can safely consume highly refined soybean oil. Ask your allergist about avoiding this ingredient. Also, be cautious when eating foods that have been fried in any type of oil, due to the risk of cross-contact: If a soy-containing food is fried in oil, that oil will absorb certain soy proteins; if a different food that doesn’t contain soy is then fried in that same oil, consuming it could trigger an allergic reaction.
People with a soy allergy often can eat foods that contain soy lecithin — a mixture of fatty substances derived from soybean processing. If you have a soy allergy, ask your allergist if soy lecithin is safe for you.
People with a soy allergy sometimes wonder if they should also avoid peanuts — another legume that is a common allergy trigger. The answer is “not necessarily.” They are separate foods and their allergen triggers are unrelated. Soybeans also are unrelated to tree nuts such as almonds, walnuts and cashews. Those allergic to soy are no more likely to be allergic to tree nuts or peanuts than they would be to another food.
Talk to an allergist to take control of your soy allergy and live the life you want.
See your primary care doctor or a doctor who specializes in treating allergies (allergist) if you experience food allergy symptoms shortly after eating. If possible, see your doctor during an allergic reaction.
Seek emergency treatment if you develop signs or symptoms of anaphylaxis, such as:
- Difficulty breathing
- Rapid, weak pulse
- Dizziness or lightheadedness
- Drooling and inability to swallow
- Full-body redness and warmth (flushing)
- Trouble breathing or noisy breathing
- Difficulty talking more than a few words and/or hoarse voice
- Wheeze
- Cough
- Swelling and tightness of the throat
- Collapse
- Light-headedness or dizziness
- Diarrhea
- Tingling in the hands, feet, lips or scalp
- Swelling of tongue
- Pale and floppy (in young children)
A severe allergic reaction (anaphylaxis) is a medical emergency. Call your local emergency immediately. Lay the person down. If they have an adrenaline injector and you are able to administer it, do so.
Anaphylaxis is a medical emergency. It can be very serious if not treated quickly.
If someone has symptoms of anaphylaxis, you should:
- Call your local emergency number for an ambulance immediately – mention that you think the person has anaphylaxis
- Remove any trigger if possible – for example, carefully remove any wasp or bee sting stuck in the skin
- Lie the person down flat and elevate his or her legs – unless they’re unconscious, pregnant or having breathing difficulties
- Use an adrenaline auto-injector if the person has one – but make sure you know how to use it correctly first
- Check the person’s pulse and breathing and, if necessary, administer CPR (cardiopulmonary resuscitation) or other first-aid measures
- Give another injection after 5-15 minutes if the symptoms don’t improve and a second auto-injector is available
If you’re having an anaphylactic reaction, you can follow these steps yourself if you feel able to.
Are all foods made from soy equally allergenic?
No. High levels of some soy allergens may be found in soy milk drinks or in soy powder, lesser amounts in textured soy protein, tofu and soy flakes and very low amounts of allergen in fermented products such as soy sauce or miso and in strongly heated products such as roasted soybeans. There is no need to avoid soy lecithin No 322. Research studies show that most people with soy allergy can safely eat soy lecithin and soyabean oil.
What about soy sauce?
Soy sauce is prepared by fermentation which reduces the ability of the food to cause an allergic reaction. Therefore some allergic children may not react to soy sauce, yet react to other soy products. Also some soy sauces are actually made from wheat products.
What about soy in processed foods?
Almost half of soy allergic patients have had an allergic reaction due to ingestion of “hidden” soy. “Hidden” soy allergens are found in foods such as:
- boiled ham,
- sausages,
- cheese puffs,
- cakes and sweets,
- breakfast cereals,
- taco shells,
- precooked dishes,
- desserts and
- gravy and stock cubes
What about foods that may contain traces of soy?
In general the amount of the food needed to trigger an allergic reaction is much higher for soy than for other food allergies. Therefore soy allergic patients are at less risk for allergic reactions to traces of soy in processed foods.
For patients allergic to soy, do they need to watch out for soy lecithin?
Soy lecithin is derived from highly processed soy oil and has very little, if any, soy protein (100-500 ppm). Most allergists do not recommend that patients with soy allergy avoid soy lecithin. Organizational on-line sources (FARE, FAARP, CoFAR) indicate that food products containing soy lecithin can be consumed safely by nearly all patients with soy allergy. A literature search found few case reports of allergic reactions that have been attributed to soy lecithin. The degree of risk for use of soy lecithin-containing medications in patients who have soy allergy has not been extensively studied. Considering the small amount of protein present, the risk of a reaction from these medications is thought to be very small, yet there are case reports of reactions. Consequently, the use of these medications in highly sensitive soy-allergic patients is usually avoided. However, if no alternatives exist and the medication is necessary, after a discussion of risks vs benefits, one might consider administration of the first dose under medical observation.
What are soy free bread alternatives?
Most breads are made with a starter containing soy. This can make avoiding soy very difficult. Options for soy free breads are:
- Home-made using a breadmaker and allowed flours
- Check your local baker, greengrocer, delicatessen or supermarket for soy free breads
- Crumpets
- Many flat breads e.g. Lebanese or Indian bread, wraps, mountain breads.
Are children with cow’s milk allergy usually allergic to soy as well?
No. Only a small amount of children with cow’s milk allergy (about 15%) will also have or will develop allergy to soy.
What if my child is allergic to cow’s milk and soy milk?
Cow’s milk and dairy products or soy drinks are the main source of calcium in our diet. When it isn’t possible to use cow’s milk or soy milk it is essential to make sure your child gets it from other sources. You need to discuss other options with your doctor and possibly a dietitian to make sure your child meets their daily requirement for calcium that is so important for your child growing up.
Table 1. Soy milk substitutes
| Instead of: | Use |
| Soy milk infant formula for a child less than one year of age. NB rice drink is NOT suitable for a child less than 1 year. | Breast milk, cow’s milk formula, hydrolysed formula or amino acid formula. Speak with a medical professional to choose the right one based on your child’s diagnosis |
| Soy drink for a child over one year of age NB rice drink is NOT suitable for a child less than one year. | Cow’s milk Rice drink – choose one with more than 120 mg calcium /100 ml rice drink Speak with a medical professional to choose the right one based on your child’s diagnosis |
| Soy yogurt | Cow’s milk yogurt |
| Soy cheese, soy sour cream | Cow’s milk cheese, and sour cream |
| Soy ice cream | Cow’s milk ice cream, sorbet, gelato |
Does exposure to soy increase the risk of peanut allergy?
No. There is no good evidence that eating soy products increases the risk of developing peanut allergy even though both peanuts and soy are legumes.
Can my child grow out of soy allergy?
Children with soy allergy may outgrow their allergy 1. About 0.4 percent of children are allergic to soy. Studies show an allergy to soy usually occurs early in childhood and often is outgrown by age three. The majority of children with soy allergy will outgrow the allergy by age 10 1. Children with a particular form of soy allergy called “food protein induced enterocolitis” (FPIES) usually grow out of the allergy by 2-3 years of age. Your doctor will discuss what sort of soy allergy your child has and whether your child is likely to grow out of it. In cases of soy allergy due to IgE allergy antibodies, your doctor may see if the allergy is still present by performing allergy tests every 12 months or so.
What is an Epipen?
An Epipen is an emergency device called an adrenaline autoinjector (watch the Epipen adrenaline autoinjector below). It injects a dose of adrenaline into the muscle. Epipens are used to treat severe allergic reactions (anaphylaxis). The drug adrenaline reverses the severe allergic reaction and can be lifesaving.
Should my child carry an adrenaline autoinjector?
All allergists agree that children who have had a serious reaction with involvement of the breathing passages should have an adrenaline autoinjector. The need for other children to have an adrenaline autoinjector depends on a number of factors which should be discussed with your doctor.
If you have an adrenaline autoinjector it is very important that you understand how and when to use it and that you have a written anaphylaxis action plan provided by your doctor.
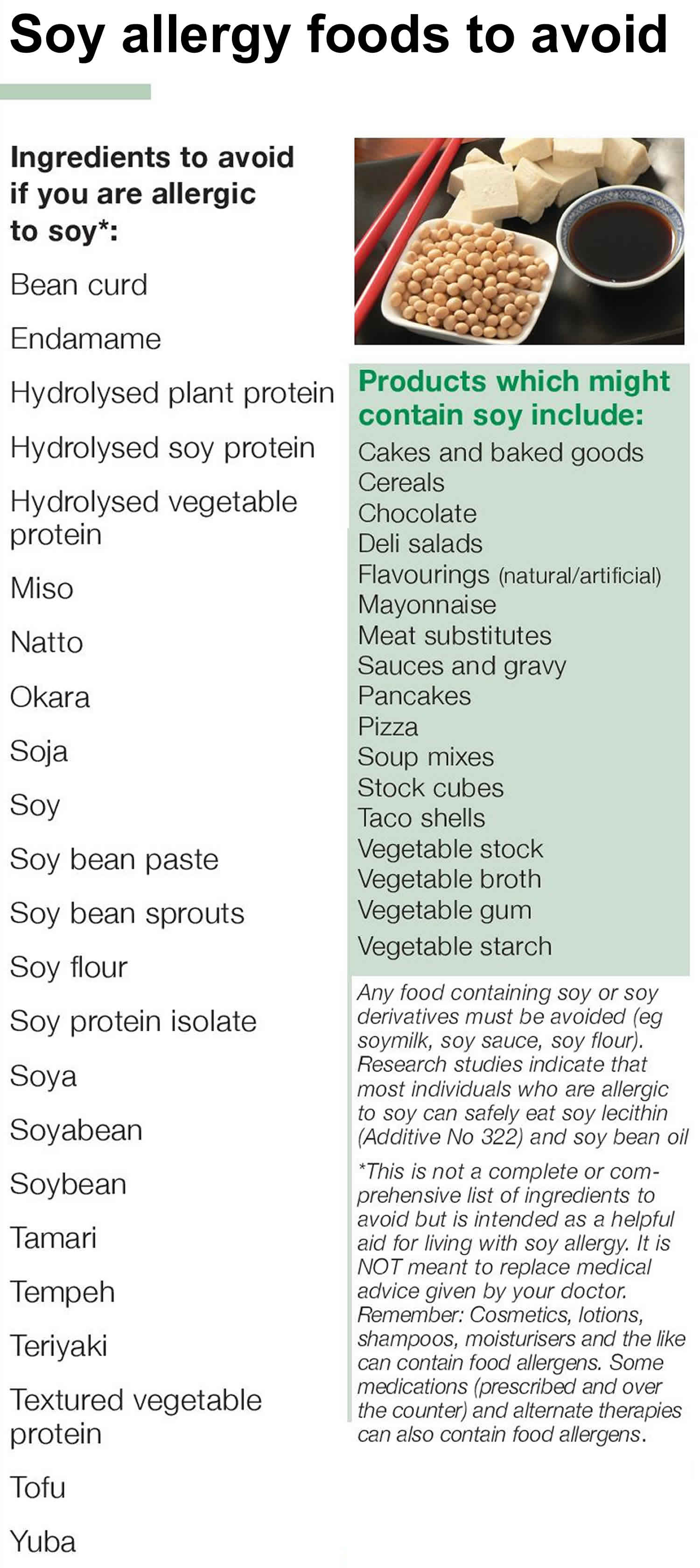
Soy allergy foods to avoid
Having a soy allergy means avoiding products that contain soy, which can be difficult. Soya beans are used widely in the manufacture of processed foods, foods such as meat products, bakery goods, chocolate and breakfast cereals, may contain soy.
Highly refined soy oil may not cause a reaction because it doesn’t contain soy proteins. Similarly, you might not react to foods that contain soy lecithin. But generally, if a label includes the word “soy,” avoid it.
Avoid foods that contain soy or any of these ingredients:
- Edamame
- Miso
- Natto
- Soy (soy albumin, soy cheese, soy fiber, soy flour, soy grits, soy ice cream, soy milk, soy nuts, soy sprouts, soy yogurt)
- Soya
- Soybean (curd, granules)
- Soy flour
- Soy milk, soy cheese, soy ice cream and soy yogurt
- Soy protein (concentrate, hydrolyzed, isolate)
- Shoyu
- Soy sauce
- Tamari
- Tempeh
- Textured vegetable protein (TVP)
- Tofu
- Vegetable oil, vegetable gum, vegetable broth and vegetable starch
Foods that sometimes (but not always) contain soy include:
- Asian cuisine
- Bread (soy flour is used in many commercial breads)
- Breakfast cereals
- Bread crumbs
- Cakes and biscuits
- Chocolate flavourings
- Chocolates and sweets (check for HVP)
- Crumbed meats,
- Deli meats and salads
- Fish
- Flavorings
- Many meat substitutes
- Mayonnaise type dressings
- Packaged sauces and gravy mixes
- Sausages, sausage rolls, frankfurts, pizza
- Soups
- Taco shells
- Unlabelled processed foods eg. takeaway food
- Vegetable gum
- Vegetable starch
- Vegetable broth.
Besides “soy,” “soya” and “soybeans,” other words on food labels may indicate that the product contains soy, including:
- Glycine max
- Hydrolyzed vegetable protein (HVP)
- Hydrolyzed plant protein
- Textured vegetable protein (TVP)
- Monodiglyceride
- Monosodium glutamate (MSG)
- Artificial flavoring
- Natural flavoring
Keep the following in mind:
- The U.S. Food and Drug Administration (FDA) exempts highly refined soybean oil from being labeled as an allergen. Studies show most allergic individuals can safely eat soy oil that has been highly refined (not cold pressed, expeller pressed, or extruded soybean oil).
- Most individuals allergic to soy can safely eat soy lecithin.
- Follow your doctor’s advice regarding these ingredients.
It is important to:
- Learn to how to read food labels carefully. Always check the food list for ‘soy’ on the label even if it says “soy-free”.
- Avoid foods that don’t have a food label or that you haven’t made yourself, as there is no guarantee that the food doesn’t contain soy
- Plan eating out and travelling and talk to staff serving you about your child’s allergy
- Avoid food that is served using spoons/tongs that are also used to serve food containing soy (e.g. some takeaway meals)
- Prepare safe meals at home for your child to take out
- Teach your child about their allergy
Figure 1. Soy allergy foods to avoid
Soy allergy causes
An immune system reaction causes food allergies. With a soy allergy, your immune system identifies certain soy proteins as harmful, triggering the production of immunoglobulin E (IgE) antibodies to the soy protein (allergen). The next time you come in contact with soy, these IgE antibodies recognize it and signal your immune system to release histamine and other chemicals into your bloodstream.
Histamine and other body chemicals cause a range of allergic signs and symptoms. Histamine is partly responsible for most allergic responses, including a runny nose, itchy eyes, dry throat, rashes and hives, nausea, diarrhea, difficulty breathing, and anaphylactic shock.
Food protein-induced enterocolitis syndrome (FPIES)
A food allergen can also cause what’s sometimes called a delayed food allergy. Although any food can be a trigger, soy is one of the more common in children. The reaction, commonly vomiting and diarrhea, usually occurs within hours after eating the trigger, rather than minutes.
Unlike some food allergies, food protein-induced enterocolitis syndrome usually resolves over time. As with typical soy allergies, preventing a reaction involves avoiding foods with soy.
Risk factors for soy allergy
Certain factors may put you at greater risk of developing a soy allergy:
- Family history. You’re at increased risk of allergy to soy or other foods if other allergies, such as hay fever, asthma, hives or eczema, are common in your family.
- Age. Soy allergy is most common in children, especially toddlers and infants.
- Other allergies. In some cases, people who are allergic to wheat, beans (legumes), milk or other foods can also have an allergic reaction to soy. Also, people who are allergic to soy may have test results showing allergy to other legumes, but may be able to eat them with no problem.
If you’re not nursing, ask your doctor for advice on what to feed your child until your appointment to reduce the risk of symptoms.
If you have symptoms of soy allergy, avoid foods that contain soy.
Soy allergy prevention
There’s no way to prevent a food allergy. If you have an infant, breast-feeding instead of using a soy-based or milk-based formula may help.
If you’re allergic to soy, the only way to avoid a reaction is to avoid soy products. It’s not always easy to know which foods contain soy, a common ingredient in many foods.
Read food labels carefully. Soy is often present in unexpected foods, including canned tuna and meat, baked goods, crackers, energy bars, low-fat peanut butter, and canned soups. Read labels every time you buy a product, because ingredients can change. Also, check for the statement “contains soy” or “may contain soy” on product labels.
Highly refined soy oil may not cause a reaction because it doesn’t contain soy proteins. Similarly, you might not react to foods that contain soy lecithin. But generally, if a label includes the word “soy,” avoid it. Products to avoid include, but are not limited to:
- Soy milk, soy cheese, soy ice cream and soy yogurt
- Soy flour
- Tofu
- Miso
- Natto
- Shoyu
- Tempeh
- Soy sauce and tamari
- Edamame
- Vegetable oil, vegetable gum, vegetable broth and vegetable starch
Soy allergy symptoms
For most people, soy allergy is uncomfortable but not serious. Rarely, however, an allergic reaction to soy can be frightening and even life-threatening. Signs and symptoms of a food allergy usually develop within a few minutes to hours after eating a food containing the allergen.
Soy allergy symptoms can include:
- Tingling in the mouth
- Hives; itching; or itchy, scaly skin (eczema)
- Swelling of the lips, face, tongue and throat, or other body parts
- Tightness in throat, hoarse voice
- Wheezing, a runny nose
- Shortness of breath, difficulty breathing
- Repetitive cough
- Abdominal pain or stomach cramps
- Stomach cramps
- Diarrhea
- Nausea
- Vomiting
- Skin redness (flushing)
- Weak pulse
- Pale or blue coloring of the skin
- Hives
- Dizziness
- Confusion
Rarely, a soy allergy will cause anaphylaxis, a potentially life-threatening reaction that impairs breathing, causes a sudden drop in blood pressure and can send the body into shock. The only medication that can treat anaphylaxis is epinephrine (adrenaline), administered through an auto-injector as soon as symptoms are apparent.
A severe allergic reaction (anaphylaxis) is more likely to occur in people who also have asthma or who are allergic to other foods besides soy, such as peanuts.
If you or your child experiences any of these symptoms after eating soybeans or a product containing soy, see an allergist.
Anaphylaxis causes more-extreme signs and symptoms including:
- Difficulty breathing, caused by throat swelling
- Shock, with a severe drop in blood pressure
- Rapid pulse
- Dizziness, lightheadedness or loss of consciousness
Soy allergy diagnosis
Diagnosing soy allergies can be as complicated as the medical condition itself. Symptoms can vary from person to person, and a single individual may not always experience the same symptoms during every reaction.
Allergic reactions to soy can affect the skin, respiratory tract, gastrointestinal tract and/or cardiovascular system.
When a food allergy is suspected, it’s important to consult an allergist, who can determine which tests to perform, decide if an allergy exists and counsel patients on managing exposure and symptoms once the diagnosis has been confirmed.
To make a diagnosis, allergists ask detailed questions about the history of allergy symptoms. Be prepared to answer questions about what and how much you ate, how long it took for symptoms to develop, which symptoms you experienced and how long the symptoms lasted. The allergist will usually perform skin-prick tests and/or order a blood test (such as an ImmunoCAP test), which indicate whether food-specific immunoglobulin E (IgE) antibodies are present in your body.
Soy allergy test
Skin-prick tests are conducted in a doctor’s office and provide results within 15 to 30 minutes. A drop of a liquid containing the suspected allergen is placed on the patient’s forearm or back. The skin is then pricked with a small, sterile probe, allowing the liquid to seep under the skin. The tests, which are not painful but can be uncomfortable, are considered positive if a wheal (resembling a bump from a mosquito bite) develops at the site. Allergy specialists usually are best equipped to perform and interpret allergy skin tests.
Blood tests, another testing option for food allergy, measure the amount of immunoglobulin E (IgE) antibody to the specific food(s) being tested. Results are typically available in about one to two weeks and are reported as a numerical value.
Your allergist will interpret these results and use them to aid in a diagnosis. While both of these diagnostic tools can signal a food allergy, neither is conclusive. A positive test result to a specific food does not always indicate that a patient will react to that food when it’s eaten. A negative test is more helpful to rule out a food allergy. Neither test, by size of the skin test wheal or the level of IgE antibodies, necessarily predicts the severity of an allergic reaction to soy.
An allergist may use these tests and the patient’s history to make a food allergy diagnosis. For a definitive diagnosis, the allergist may wish to conduct an oral food challenge, in which the patient is fed gradually increasing amounts of the suspected allergy-causing food under strict supervision. Experienced personnel, emergency medication and emergency equipment must be on hand during this procedure.
Oral food challenges also may be performed to determine if a patient has outgrown a food allergy.
Soy allergy treatment
As with other food allergies, the best way to manage a soy allergy is to avoid consuming products that contain soy and soy proteins.
Medications, such as antihistamines, may reduce signs and symptoms of minor soy allergies. Taking an antihistamine after exposure to soy may control your reaction and help relieve discomfort. Over-the-counter antihistamines include: diphenhydramine (Benadryl, Banophen Complete Allergy Medication), chlorpheniramine (Chlor-Trimeton, Aller-Chlor), cetirizine (Zyrtec, Equate Allergy Relief) and loratadine (Alavert, Claritin).
Despite your best efforts, you can eat soy unknowingly. If you have a serious allergic reaction, you may need an emergency injection of epinephrine and to go to the emergency room.
Lifestyle and home remedies
If you’re at risk of having a severe reaction or have had one:
- Carry injectable epinephrine (EpiPen, Auvi-Q, others) with you always. Make sure you know when and how to use portable epinephrine.
- Wear a medical alert bracelet to let others know about your allergy.
Managing soy allergies in children
Because soy allergy reactions, like other food allergy symptoms, can develop when a child is not with his or her parents, parents need to make sure that their child’s school, day care or other program has a written emergency action plan with instructions on preventing, recognizing and managing these episodes in class and during activities such as sporting events and field trips.
If your child has been prescribed an auto-injector, be sure that you and those responsible for supervising your child understand how to use it.
Future treatments
A number of treatments are in clinical trials. Promising treatments include oral (swallowed) immunotherapy (OIT) and sublingual (under the tongue) immunotherapy (SLIT) to increase tolerance to foods that cause allergic reactions. But more research is needed.
Managing a severe food reaction with epinephrine
Soy is among the most common food allergens. But all food allergies can be dangerous.
Epinephrine is the first-line treatment for anaphylaxis, a severe whole-body allergic reaction that causes symptoms, including tightening of the airway. Anaphylaxis can occur within seconds or minutes of exposure to the allergen, can worsen quickly, and can be deadly.
Once a food allergy diagnosis is made, your allergist likely will prescribe an epinephrine auto-injector and teach you how to use it. Check the expiration date of your auto-injector, note the expiration date on your calendar and ask your pharmacy about reminder services for prescription renewals.
Be sure to have two doses available, as the severe reaction may recur. Epinephrine should be used immediately if you experience severe symptoms such as shortness of breath, repetitive coughing, weak pulse, generalized hives, tightness in the throat, trouble breathing or swallowing, or a combination of symptoms from different body areas such as hives, rashes or swelling on the skin coupled with vomiting, diarrhea or abdominal pain. Repeated doses of epinephrine may be necessary.
If you are uncertain whether a reaction warrants epinephrine, use it right away, because the benefits of epinephrine far outweigh the risk that a dose may not have been necessary.
Common side effects of epinephrine may include transient anxiety, restlessness, dizziness and shakiness. Rarely, the medication can lead to an abnormal heart rate or rhythm, a heart attack, a sharp increase in blood pressure and fluid buildup in the lungs, but these adverse effects are generally caused by errors in dosing which is unlikely to occur with use of epinephrine autoinjectors. Patients with certain pre-existing conditions who may be at higher risk for adverse effects should speak to their allergist about epinephrine use.
Your allergist will provide you with a written emergency treatment plan that outlines which medications should be administered and when (note that between 10 and 20 percent of life-threatening severe allergic reactions have no skin symptoms). Be sure you understand how to properly and promptly use an epinephrine auto-injector.
Once epinephrine has been administered, immediately call your local emergency services number and inform the dispatcher that epinephrine was given and that more may be needed from the emergency responders.
Other medications, such as antihistamine and corticosteroids, may be prescribed to treat mild symptoms of a food allergy, but it is important to note that there is no substitute for epinephrine — this is the only medication that can reverse the life-threatening symptoms of anaphylaxis.
References