Sperm motility
Sperm motility is the ability of the sperm to move. For conception to occur, the sperms need to swim forward towards the egg and fertilize it before it disintegrates. According to World Health Organization (WHO) latest criteria, at least 40% of the sperms should be moving in a given semen sample 1. This is called the total motile sperm count. And among them 32% should have a rapid forward movement, this is called progressive motility. Sperm motility is an important factor along with sperm count and sperm morphology, which is looked at in semen analysis test because sperm needs to travel forward through the woman’s reproductive tract to reach and fertilize an egg. A man with poor sperm motility may be diagnosed with male factor infertility because if the sperm are lazy and have reduced movement, they won’t be able to reach the egg in time and fertilize it. Normal sperm counts are typically greater than 15 million/mL and sperm motility with at least 40% of sperm should be motile and should comprise more of the progressive motile ones. Sperm are of 2 types – those which swim, and those which don’t. Remember that only those sperm which move forward fast are able to swim up to the egg and fertilize it, the others are of little use.
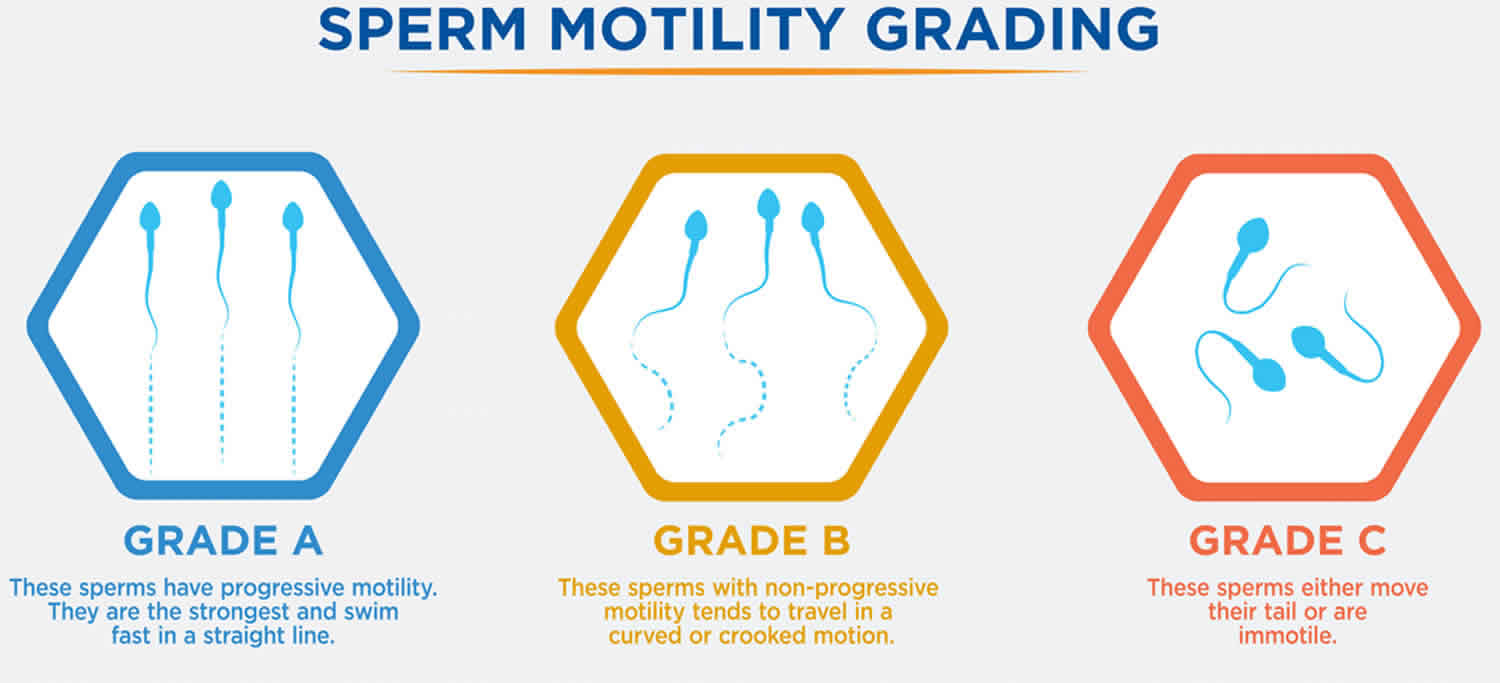
Sperm motility is graded from a to d, according to the World Health Organization (WHO) Manual criteria, as follows 1:
- Grade a (fast progressive): sperms are those which swim forward fast in a straight line – like guided missiles.
- Grade b (slow progressive): sperms swim forward, but either in a curved or crooked line, or slowly (slow linear or non linear motility).
- Grade c (nonprogressive): sperms move their tails, but do not move forward (local motility only).
- Grade d (immotile ): sperms do not move at all.
Sperms of grade c and d are considered poor. If sperm motility is poor this is called asthenospermia or asthenozoospermia, and is diagnosed when the sperms that can move efficiently are less than 32%. It means that the sperms find it difficult to move towards the egg due to its limited motility. This suggests that the testis is producing poor quality sperm and is not functioning properly and this may mean that even the apparently motile sperm may not be able to fertilize the egg.
Sperm motility becomes critical at the time of fertilization because it allows or at least facilitates passage of the sperm through the zona pellucida of the egg. Without technologic intervention, a non-motile or abnormally-motile sperm is not going to fertilize the egg. Hence, assessing the fraction of a sperm population that is motile is perhaps the most widely-used measure of semen quality.
If a man has low sperm motility, then he might be diagnosed with male factor infertility. Because after ovulation an egg stays in the fallopian tube for 12-24 hours waiting for the sperm to fertilize it. If the sperms have low motility, then they would not be able to swim up the uterus to reach the fallopian tubes in time to fertilize the egg, thereby affecting pregnancy.
This is why fertility doctors worry when the sperm motility is only 20%, when it should be 60% to 80% actively moving. Many men with a low sperm count ask is – ” But doctor, I just need a single sperm to fertilize my wife’s egg. If my count is 10 million and motility is 20%, this means I have 2 million motile sperm in my ejaculate – why can’t I get her pregnant ? ” The problem is that the sperm in infertile men with a low sperm count are often not functionally competent – they cannot fertilize the egg. The fact that only 20% of the sperm are motile means that 80% are immotile and if so many sperm cannot even swim, one worries about the functional ability of the remaining sperm.
What is motile sperm?
Motile sperms are the sperms that can move efficiently. For every ejaculate sample, the sperms need to be motile, in order to move through the woman’s reproductive tract and fertilize her eggs.
What is motility in sperm?
Motility of sperm refers to the sperm’s ability to move. 90% of male infertility issues are caused due to low sperm count or poor sperm motility.
Can low sperm motility cause infertility?
Sperm motility is important for male fertility. If a man’s sperm is unable to swim effectively, then natural pregnancy would be difficult. The sperm will not be able to reach the egg because of its poor motility.
Can low sperm motility cause miscarriage?
Unhealthy lifestyle choices can lead to many factors that can decrease the chances of a successful pregnancy. These factors may include poor sperm motility, lower sperm counts and abnormal morphology. And any damage to sperm quality can cause fertility problems, even if an egg is fertilized it may lead to a miscarriage.
What are the chances of pregnancy with low sperm motility?
The chances of pregnancy with low motility are minimal where one must resort to assisted reproductive techniques. Intrauterine insemination (IUI) also called artificial insemination, is recommended in couples where the motility ranges from 30-40%. If the motility range is less than 30%, In Vitro Fertilization (IVF) is recommended, and in cases of severe motility problems, Intracytoplasmic Sperm Injection (ICSI) is recommended.
Sperm motility test
When analyzing motility, it is important to know whether the semen sample has been abused in any way. Exposure to heat, cold, any kind of residue on collection equipment, or the wrong pH or osmolality of an extender can adversely affect sperm motility. Sperm motility is also affected by periods of sexual inactivity – males that have not ejaculated for prolonged periods often have poor motility on the first ejaculate, but much better motility for a second ejaculate collected soon thereafter.
There are several means for evaluating sperm motility. Which technique to use depends on experience of the operator, the desire for precision and repeatability, and availability of equipment. In almost all cases, motility is reported as the percentage of sperm that manifest motility (usually progressive motility).
Manual motility estimates (wet mount)
This commonly-used technique involves placing a sample of diluted semen on a microscope slide, examining it with a microscope and estimating the fraction of the population that is motile.
More specifically, a sample of semen is diluted in warm extender or buffered saline, and about 10 to 20 microliters of this sample is pipetted onto a clean, prewarmed microscope slide. A coverslip is lowered onto the sample, avoiding formation of air bubbles if possible, and the slide is examined using a microscope with a 20X objective. At least ten widely-spaced fields are examined to provide an estimate of the percentage of motile cells. If estimating motility is a commonly required technique, a microscope warm stage may be worth purchasing.
A bright field microscope can be used for evaluating motility if the field diaphragm is closed to enhance contrast and ability to visualize sperm. A much better choice is a phase contrast microscope or a microscope equipped for differential interference contrast. Examine the images above to appreciate the difference in these three types of microscopy – clearly, unstained sperm are difficult to observe using bright field.
Manual motility estimates are easy to perform and require minimal equipment. In the hands of an experienced evaluator, manual estimates generally provide good estimates of motility. The chief limitation of this technique is its subjective nature. Samples with outstanding motility tend to be scored lower than they should be and poor samples tend to be scored higher than they should.
Track motility estimates
A wet mount of diluted semen is prepared as described for a manual estimate, and sperm are photographed using an exposure time long enough for motile sperm to leave tracks across the image (roughly 0.2 seconds). Using this technique, non-motile sperm appear non-motile, and sperm with non-progressive motility leave tracks that are circular or otherwise abnormal. If a digital camera is used, the image can be displayed on a computer monitor for convenient tabulation.
Track motility estimates require more time to perform that manual estimates, but they are objective and repeatable. Additionally, one can save the images for a permanent record.
Computer-aided motility analysis
A number of systems have been developed that allow motility to be analyzed with the aid of a computer. These systems acquire an image in essentially the same manner as described for the track motility technique, and image processing software detects and tabulates the tracks and immotile cells. Other information is readily obtained, including sperm velocity and other motion characteristics.
What affects sperm motility?
The most important factor affecting the quality of sperm is stress and some health conditions. Also, excess heat around the genitals increases scrotal temperature that can affect the motility of sperm.
Other factors that can affect sperm motility include:
- Health and lifestyle factors such as smoking, excessive drinking (more than 2 drinks per day), drugs including steroids and recreational marijuana use, and being overweight and high body mass index (BMI).
- Past medical conditions such as an undescended testes, hernia, sexually transmitted disease (STD) or severe trauma.
- Acute viral illness can also temporarily affect sperm health.
- Some prescription medications.
- Cancer treatment.
There is no scientific evidence that wearing tight clothes or bike shorts affects the quality of your sperm. Diet, vitamins and supplements actually have very little impact on your sperm count – but they may help you stay healthy.
Sports injuries to the groin will only have an impact on sperm production in extremely severe cases.
While the effect of age on a man’s fertility is not as significant as it is with women, there is a decline in the quality of sperm after the age of 45. After this age, sperm volume, motility and morphology declines and damage to sperm DNA increases.
Other causes of male infertility
Male infertility is caused by problems that affect sperm production or the transport process such as:
- Blocked / absent vas deferens (tubes)
- Low sperm number and/or poor sperm production
- High numbers of abnormally shaped sperm
- Failure of sperm production
- Anti-sperm antibodies
- Sperm DNA fragmentation
In rare cases, a genetic disease such as cystic fibrosis or a chromosomal abnormality could affect male fertility.
Some men may have more serious medical problems, such as low male sex hormones, or testosterone levels.
Retrograde ejaculation
Retrograde ejaculation is a condition in which some or all semen flows backwards into the bladder rather than out through the urethra during ejaculation. Symptoms include producing little or no semen during ejaculation and can be diagnosed with a urine sample and semen analysis. If you are trying to conceive, retrograde ejaculation can be treated using assisted reproductive technology such as intrauterine insemination, In Vitro Fertilization (IVF) or Intracytoplasmic Sperm Injection (ICSI) procedures. Sperm can be collected from the urine or surgically retrieved from the testis. A fertility specialist can explain your options and help you choose the best path for you.
Immunological infertility
Male immunological infertility occurs when a man develops antibodies against his own sperm. These anti-sperm antibodies attach to the sperm affecting the way they move and their ability to penetrate a woman’s cervical mucus and fertilise the egg. The presence of anti-sperm antibodies is commonly the result of vasectomy, injury or injection but it does not mean a man won’t be able to conceive a child. Intracytoplasmic Sperm Injection (ICSI) can be used to help achieve a pregnancy.
Hyperprolactinemia
Hyperprolactinemia refers to elevated levels of the prolactin hormone in the blood stream. In men this can cause infertility by affecting the function of the testicles, decreased testosterone levels, decreased sex drive and abnormal sperm production. If hyperprolactinemia is affecting your fertility there are treatments available and your fertility specialist will guide you on the one most appropriate for you.
Occlusion
Occulsion refers to a blockage in a man’s reproductive system, often in the epididymis or vas deferens, which prevents sperm reaching the urethra. Occlusions in men could be a result of injury, vasectomy or a congenital condition. It can be treated using a Vasovasectomy which is a surgical procedure which reconnects the ends of the vas deferens together or a testicular biopsy to surgically retrieve sperm from the testis for use in IVF or ICSI treatment.
Sperm motility treatment
Some lifestyle changes like having a proper diet, taking vitamin C and zinc supplements have been shown to increase sperm count, sperm motility and even testosterone levels in men, thus improving the chances of fertility.
How can you boost male fertility and increase sperm count naturally, and change lifestyle factors which can impact male fertility:
- Reduce chemical exposure
- Improve diet
- Exercise regularly
- Take nutritional supplements
- Try herbal helpers to boost male fertility
- Prevent yourself from smoking tobacco
- Stop usage of marijuana
- Avoid drinking alcohol
- Stop using any anabolic steroids including any testosterone supplements
If a couple is facing an issue of low semen motility while trying to conceive and has tried all the home remedies, taken vitamin supplements and even managed lifestyle changes without any luck, then the best course of action would be to visit an infertility specialist. During investigations, if low motility is found due to some hormonal disorders, then treatment might be possible but if a genetic cause is responsible for low or no motility then assisted reproductive techniques (ART) might be recommended. The available options for low sperm motility treatment are discussed below.
The available options are:
- Intrauterine Insemination (IUI) is recommended when the sperm motility range is between 30-40%. Intrauterine insemination (IUI) is a procedure where healthy and active sperm are injected directly into the uterus. This procedure saves the sperm from taking the long journey from the cervix to the fallopian tube, thus making it easier to reach the egg. But this procedure is recommended in males who have less than 30-40% sperm motility range.
- In Vitro Fertilization (IVF) is recommended when IUI fails and when the sperm motility rate is lower than 30%. In this process, the egg is fertilized directly with the sperm in a lab. The embryo that is fertilized is then transferred to the uterus to establish a successful pregnancy.
- Intracytoplasmic Sperm Injection (ICSI) is recommended in men with severe motility issues that is when the motile sperm count is less than 5 million in the ejaculate. Intracytoplasmic Sperm Injection (ICSI) is performed as an additional part of an IVF treatment cycle where a single sperm is injected into each egg to assist fertilization using very fine micro-manipulation equipment. In most cases, ICSI can be used to overcome severe male infertility. This option has a successful fertilization rate of 70-90% and can be done as long as one normal motile sperm is found in the ejaculate.
Intrauterine Insemination (IUI)
Artificial insemination or intrauterine insemination (IUI) involves inserting the male partner’s (or donor’s) prepared semen through the neck of the womb (cervix) and into the uterus, close to the time of ovulation. It is a simpler, less invasive form of fertility treatment.
Intrauterine insemination (IUI) treatment can be performed in a couple of different ways:
- Natural cycle: This option does not involve any medication and works with the woman’s natural menstrual cycle.
- Artificial hormone stimulation (or ovulation induction): This option involves the use of medication to stimulate the ovaries and cause or regulate ovulation with either Letrozole or FSH (follicle stimulating hormones) injections.
The semen sample is analyzed and washed to concentrate the motile sperm. The final prepared sample is used for insemination where it is gently inserted into the uterine cavity using a speculum and a small catheter.
An intrauterine insemination procedure is performed by a nurse and is usually not painful, although sometimes you might feel mild cramping and/or discomfort. You should be able to return to work straight away.
Who is intrauterine insemination suitable for?
If you or your partner has been diagnosed with unexplained infertility, hostile cervical mucus, minor sperm abnormalities or other male disorders, intrauterine insemination is sometimes a successful option.
It can also be used when semen has been frozen due to a husband’s absence or before chemotherapy or radiotherapy.
It is more beneficial in women who are not of an advanced maternal age.
Insemination with donor sperm
Artificial insemination is also used when couples need to use a sperm donor. Donor sperm may be recommended when the male partner has problems with sperm quality or production, including when the sperm is of very poor quality, or if there is a high risk of passing on a genetic disease.
Artificial insemination using a sperm donor is also an option for single women or same sex couples.
In Vitro Fertilization (IVF)
IVF or In Vitro Fertilization, is a procedure, used to overcome a range of fertility issues, by which an egg and sperm are joined together outside the body, in a specialized laboratory. The fertilized egg (embryo) is allowed to grow in a protected environment for some days before being transferred into the woman’s uterus increasing the chance that a pregnancy will occur. Fertilized embryos are transferred to the woman’s uterus in a simple procedure call an embryo transfer (a very similar technique to a pap smear). If more than two embryos develop, your medical team can freeze those that are surplus for use in subsequent cycles.
If there is any concern about sperm quality, the process of fertilization is carried out by Intracytoplasmic Sperm Injection (ICSI). This is where one sperm is inserted into each egg.
In Vitro Fertilisation (IVF) can be used to overcome a range of fertility issues and for many couples, gives them the best chance of having a baby.
In Vitro Fertilisation (IVF) treatment protocols
IVF treatment is tailored to your specific needs by your fertility specialist. Most patients who undergo IVF will be prescribed one of two main treatment protocols Long Down Regulation and Antagonist treatment cycles.
Long Down Regulation [Agonist] treatment cycle
Long down regulation treatment is the process of suppressing a woman’s natural hormones before fertility medications.
Approximately 3 weeks after your period starts you will have a blood test and begin pre-IVF treatment [GnRH analogue] in the form of a Synarel nasal spray or Lucrin injection to control your natural hormones before the fertility medication starts.
About 12 days later another blood test will be taken to make sure your own hormones are low [or down regulated] and you will be instructed when to begin daily hormone Follicle Stimulating Hormone injections [Gonal-F or Puregon]. You will continue taking the Synarel or Lucrin throughout this time.
5 days after you begin Follicle Stimulating Hormone (FSH) injections you will have a blood test and ultrasound of your ovaries. You will be monitored closely with blood tests and ultrasounds until you have an optimum number and size of developed follicles. Once you are ready will we advise when to have your hCG (human chorionic gonatrophin) trigger injection and schedule your egg collection 36 hours later.
After egg collection you will use supplemental progesterone either as a vaginal gel, pessary or subcutaneous injections until your pregnancy test two weeks later.
Antagonist treatment cycle
Antagonist treatment uses injectable drugs called antagonists to prevent premature ovulation. It is the most commonly used treatment protocol because the shorter cycle makes it more convenient for patients and reduces the risk of hyper-stimulation.
Starting on the second day of your period you will have a blood test and providing all your hormone levels are low, you will be advised to begin Follicle Stimulating Hormone (FSH) injections [Gonal-F or Puregon] that day.
After four days of injections you start a second injection [Cetrotide or Orgalutron] to switch off your own hormones and prevent premature release of the eggs. 6-8 days after you begin FSH injections you will have a blood test and ultrasound of your ovaries. You will be monitored closely with blood tests and ultrasounds until you have an optimum number and size of developed follicles.
Once you are ready will your medical team will advise you when to have your hCG (human chorionic gonatrophin) trigger injection and schedule your egg collection 36 hours later After egg collection you will use supplemental progesterone either as a vaginal gel, pessary or subcutaneous injections until your pregnancy test two weeks later.
The In Vitro Fertilisation (IVF) process step by step
Each IVF treatment cycle takes around six weeks.
Step 1: Initial Specialist Appointment
At your initial appointment, your fertility specialist will review your medical history and all previous investigations and treatments.
You and your partner should both attend your first appointment with your fertility specialist. They will review your medical history, all previous investigations and treatment, and will provide preliminary advice about your treatment options.
Step 2: Pre-treatment consultation
You’ll meet again with your fertility specialist, confirm your treatment plan, have any questions answered and sign the relevant consent forms. Discuss any complementary medicines you are taking now, as these may interfere with your treatment.
Step 3: Treatment begins
Your fertility nurse gives you the medication you need, explains the treatment cycle timeline, and shows you how to self-administer the Follicle Stimulating Hormone (FSH) injections. We recommend both you and your partner attend this appointment.
Step 4: Hormone stimulation
Follicle Stimulating Hormone (FSH) is administered through a diabetic-style pen, stimulating your ovaries to produce more eggs than usual. You’ll have a higher chance of achieving fertilization and pregnancy when your medical team can collect more eggs.
Step 5: Treatment monitoring
Throughout your cycle, regular blood tests measure your hormone levels and ultrasounds measure the size and number of your ovarian follicles. This also helps your medical team determine the appropriate time for egg collection. All your blood and ultrasound tests are conducted by nurses within your chosen IVF clinic, and are included as part of your treatment costs.
Step 6: Trigger injecton
Once you have the optimum number and size of follicles, your medical team plan your egg collection. You’ll have a trigger injection of hCG (human chorionic gonatrophin) in the evening, and the operation for egg collection will occur 36 to 38 hours later. The hCG injection replaces the natural Luteinizing Hormone (LH) in the body and ‘triggers’ or instigates ovulation.
Step 7: Egg collection in day surgery
Egg collection is undertaken in day surgery, usually under ultrasound guidance. Most women prefer a light general anesthetic, but you can have a local anesthetic with sedation if you prefer. You will be at the hospital for about 4 hours and will need someone to drive you home afterwards. Make sure you can take the rest of the day off work.
On the morning of your egg collection your partner will need to provide a fresh semen (sperm) sample, so your medical team can immediately fertilize your eggs.
Step 8: Egg fertilization
Collected eggs are taken to the laboratory and placed in culture medium to prepare them for fertilization later that day. In IVF, prepared sperm and eggs are placed together in a dish where fertilization occurs. In ICSI, an individual sperm is selected by a highly experienced embryologist, and, under very delicate microscopic control, the egg is injected with this single sperm.
Step 9: Embryo development
The egg and sperm are then placed in individual incubators at 37 degrees to mimic the temperature of the human body. The next day, scientists will examine the eggs to determine if fertilization has occurred, and will call you to advise you of the development of the embryos.
Step 10: Embryo transfer
Embryo transfer is a simple day surgery procedure and usually takes place five days after the egg collection. The embryos are transferred into the uterus through a very fine catheter passed through the cervix, a procedure similar to a pap smear. In some cases we may recommend transferring embryos earlier.
Step 11: Embryo freezing
Any extra embryos not used during a treatment cycle that are suitable for freezing can be stored for the future.
Step 12: Pregnancy test
Your nurse will organize an appointment for you to have a blood test two weeks after the embryo transfer. Occasionally, women can still have a period despite being pregnant, so this blood test will occur even if your period has commenced. Your fertility medical team does not recommend the use of urinary pregnancy test kits, as the hormone medication given throughout treatment could produce an incorrect reading.
Your pregnancy blood test results are usually available by mid afternoon. If the pregnancy test is positive, your fertility medical team will arrange an ultrasound scan approximately three weeks later.
Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection (ICSI) is performed as an additional part of an IVF treatment cycle where a single sperm is injected into each egg to assist fertilisation using very fine micro-manipulation equipment. In most cases, ICSI can be used to overcome severe male infertility.
Who is suitable for intracytoplasmic sperm injection (ICSI)?
Intracytoplasmic sperm injection is recommended for couple’s who have been diagnosed with male fertility issues such as low sperm count, low sperm morphology or motility, anti-sperm antibodies or have previously had a vasectomy or unsuccessful vasectomy reversal.
Your fertility medical team can also use this technique for couples who have experienced poor or no fertilization rates using standard IVF.
What are the success rates for intracytoplasmic sperm injection (ICSI)?
Together with IVF, Intracytoplasmic Sperm Injection (ICSI) is one of the most common techniques used in Assisted Reproductive Technology (ART). Since it was introduced, it has led to the birth of many thousands of babies worldwide that otherwise might not have been conceived.
The success rates for ICSI are similar to those of standard IVF.
While success rates can give you an indication of your chance of conceiving they are not specific to your situation. Your fertility specialist will be able to give you an indication of your individual chance of success using ICSI.
Are there potential risks with intracytoplasmic sperm injection (ICSI)?
There is no convincing evidence that the rate of birth defects in children born from the ICSI process is any different to the general population. However there is slight increase in the chance that a male child born from the ICSI process will also have a male fertility issue.
What is PICSI (ICSI-HA)?
Physiological Intracytoplasmic Sperm Injection (PICSI) is an extension of the ICSI technique which involves a functional test for sperm to aid in their selection for ICSI. The test is based on a sperms ability to bind to Hyaluron (HA) mimicking the natural binding of mature sperm to oocytes (eggs).
It involves adding prepared sperm to a special dish containing small dots of Hyaluron on the bottom. Sperm that bind to the HA are then isolated and selected from for ICSI.
People that might benefit from PICSI are those with poor fertilization in a previous ICSI cycle, poor embryo development in previous ICSI cycle, high levels of Sperm DNA fragmentation and reduced sperm morphology or motility.
References