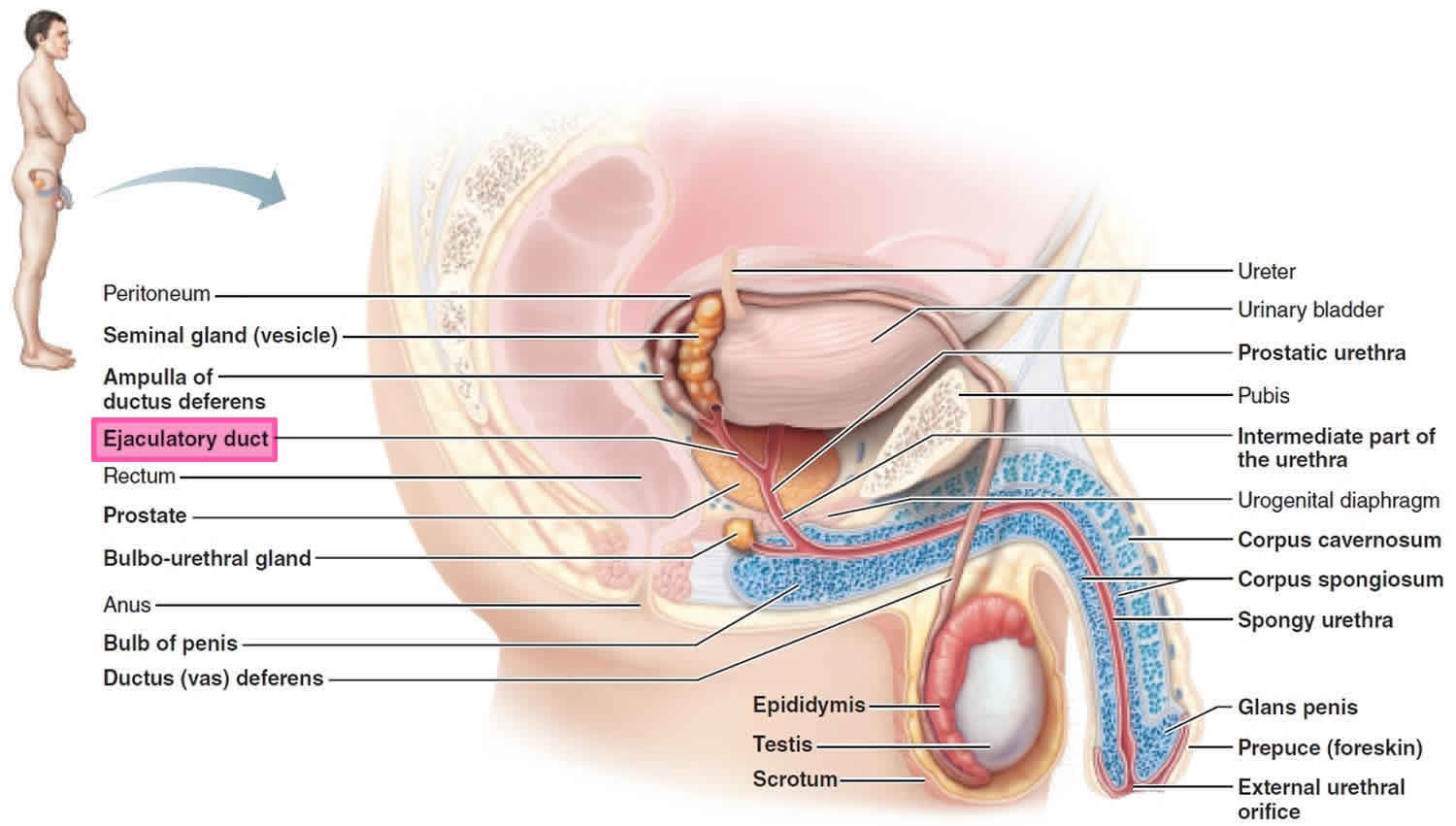
Ejaculatory duct
Ejaculatory duct delivers sperm into the urethra, adding secretions and additives from the prostate necessary for sperm function, while providing an interface between the reproductive and urinary systems in men. Each ejaculatory duct is formed by the union of the vas deferens with the excretory duct of a seminal vesicle. Each ejaculatory duct runs within the prostate, where it empties into the prostatic urethra at the verumontanum, either side of the utricle, about halfway through the prostate gland. During ejaculation, semen passes through the prostate gland, enters the prostatic urethra and exits the body via the external urethral orifice.
Figure 1. Ejaculatory duct
 Ejaculatory duct function
Ejaculatory duct function
Ejaculatory duct function is to mix the sperm stored in the ampulla with fluids secreted by the seminal vesicles and to transport these substances to the prostate.
Ejaculatory duct obstruction
Ejaculatory duct obstruction is a relatively rare cause of infertility as male factor and is surgically correctable following an appropriate treatment 1. Complete ejaculatory duct obstruction has been reported in 1% of all infertile men. Patients with complete ejaculatory duct obstruction shows absent or low ejaculate, and azoospermia in the presence of a palpable vas deferens 2. Ejaculatory duct obstruction may show various symptoms including dysuria, hematospermia, pain during or after ejaculation, and perineal or testicular pain or discomfort 3. Ejaculatory duct obstruction may be congenital or acquired. The causes of ejaculatory duct obstruction include congenital atresia, duct cysts, trauma, infection, inflammation and calculus formation 4. The standard method of establishing the diagnosis of ejaculatory duct obstruction is seminal vesiculography. Dilated seminal vesicles can be fllled with a dye solution under transrectal ultrasonography (TRUS) guidance; if duct obstruction is complete, the efflux of the dye solution cannot be seen during cystoscopy 5. With advances in noninvasive diagnostic methods, such as high-resolution TRUS (transrectal ultrasonography) and magnetic resonance imaging (MRI), the seminal vesicles can be accurately evaluated, thereby facilitating the diagnosis of ejaculatory duct obstruction.
The treatment of choice for distal seminal tract obstruction is transurethral resection of the ejaculatory duct. Approximately half of men undergoing this procedure for ejaculatory duct obstruction show improvement of their semen parameters and half of the men who improve achieve a subsequent pregnancy 6.
References- Lee JY, Diaz RR, Choi YD, Cho KS. Hybrid method of transurethral resection of ejaculatory ducts using holmium:yttriumaluminium garnet laser on complete ejaculatory duct obstruction. Yonsei Med J. 2013;54(4):1062–1065. doi:10.3349/ymj.2013.54.4.1062 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3663216
- Jarow JP. Seminal vesicle aspiration in the management of patients with ejaculatory duct obstruction. J Urol. 1994;152:899–901.
- Ozgök Y, Tan MO, Kilciler M, Tahmaz L, Kibar Y. Diagnosis and treatment of ejaculatory duct obstruction in male infertility. Eur Urol. 2001;39:24–29.
- Pryor JP, Hendry WF. Ejaculatory duct obstruction in subfertile males: analysis of 87 patients. Fertil Steril. 1991;56:725–730.
- Yurdakul T, Gokce G, Kilic O, Piskin MM. Transurethral resection of ejaculatory ducts in the treatment of complete ejaculatory duct obstruction. Int Urol Nephrol. 2008;40:369–372.
- Donkol RH. Imaging in male-factor obstructive infertility. World J Radiol. 2010;2:172–179.




