What is a splenectomy
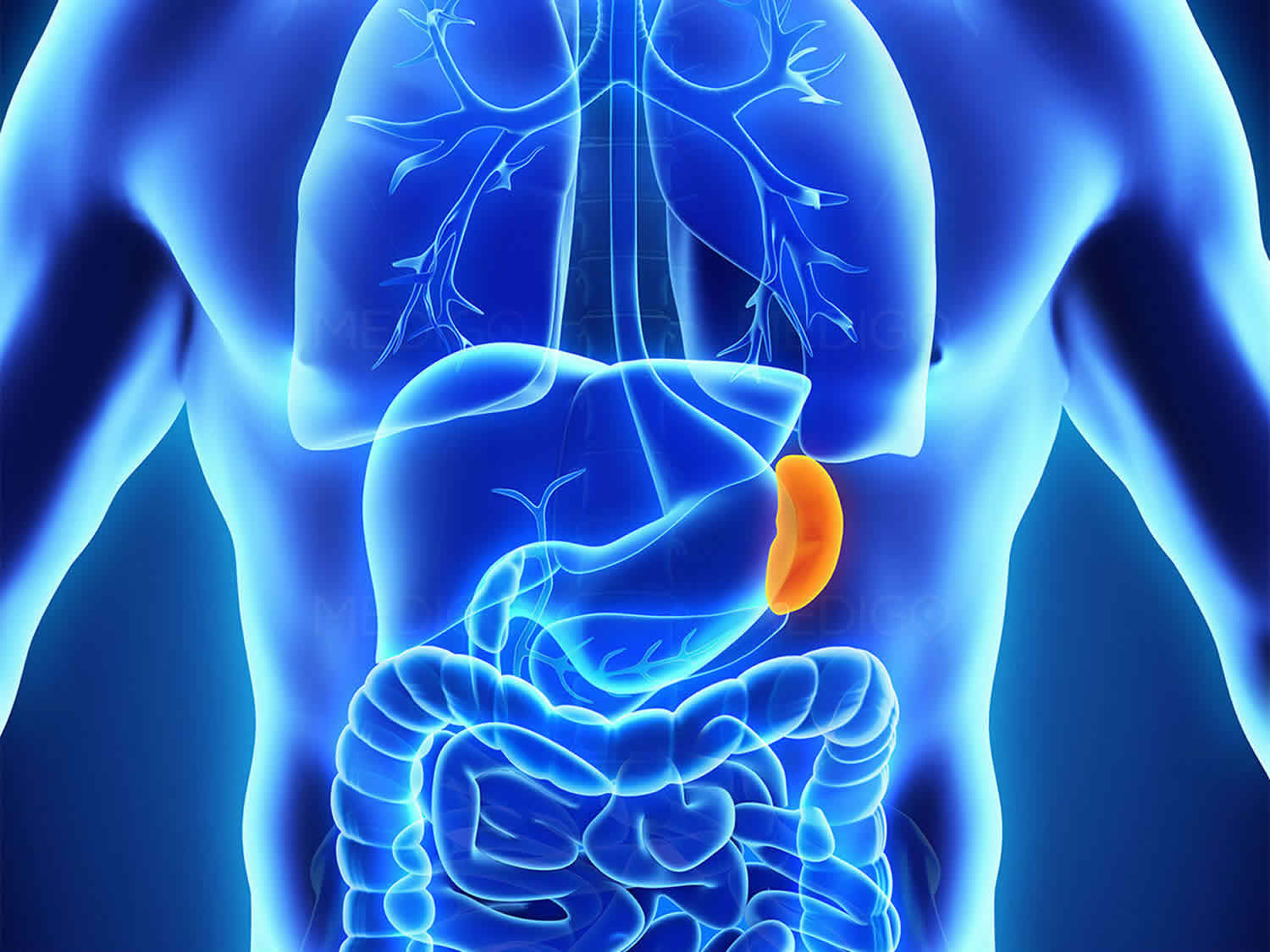
Splenectomy is a surgical procedure to remove your spleen. The spleen is an organ that sits under your rib cage on the upper left side of your abdomen (Figures 1 and 2). The spleen helps fight infection and filters unneeded material, such as old or damaged blood cells, from your blood.
The most common reason for splenectomy is to treat a ruptured spleen due to an abdominal injury, causes bleeding. Splenic rupture and/or lacerations may lead to life-threatening internal bleeding warranting a splenectomy. Splenectomy may be used to treat other conditions, including an enlarged spleen that is causing discomfort (splenomegaly), hypersplenism (overactive spleen), some blood disorders, such as idiopathic thrombocytopenia purpura (ITP), thalassemia, hemolytic anemia, sickle cell anemia), infection, noncancerous cysts or tumors and certain cancers such as lymphoma, Hodgkin disease, and leukemia 1.
A splenectomy may be performed via laparoscopy or laparotomy. Splenectomy is most commonly performed using a tiny video camera and special surgical tools (laparoscopic splenectomy) as it typically results in less scarring and faster recovery time for the patient as a less invasive approach compared to laparotomy. With this type of surgery, you may be able to leave the hospital the same day and recover fully in two weeks. Partial splenectomy may also be considered based on the vascular segmentation of the spleen via the un-anastomosed arterial supply.
Laparoscopic splenectomy procedure involves:
- Making several incisions in your abdomen (tummy area).
- Guiding a laparoscope into your body through one of the incisions, so doctors can see what they’re doing.
- Passing thin instruments into your abdomen through the other incisions, to remove your spleen. Gas will be pumped into your abdomen to make this easier.
The incisions will then be stitched up or sometimes glued together. You may be able to go home the same day, or may need to stay in hospital overnight. If you go home the same day, someone will need to stay with you for the first 24 hours.
Call your local emergency services number anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You are short of breath.
Call your doctor or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have loose stitches, or your incision comes open.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
- You are sick to your stomach and cannot drink fluids or keep them down.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness and swelling in your leg or groin.
- Bright red blood has soaked through the bandage.
- You cannot pass stools or gas.
Watch closely for changes in your health, and be sure to contact your doctor if you have any problems.
What is a spleen
The spleen is the largest lymphoid organ and has a crucial function in the immune system. The spleen is responsible for the production and maturation of IgM, B lymphocytes, and opsonins 2. The spleen most importantly protects against infections from polysaccharide-encapsulated bacteria including Streptococcus pneumoniae, Haemophilus influenzae type B, Neisseria meningitidis, Escherichia coli, Salmonella, Klebsiella, and group B Streptococci (SHiNE SKiS) 2. The spleen also acts as the primary reservoir for platelets and as a filter for red blood cells (RBCs), removing damaged or malformed red blood cells from the circulation. In addition, the spleen performs extramedullary hematopoiesis.
The normal position of the spleen is within the peritoneal cavity in the left upper quadrant of the abdominal cavity adjacent to ribs nine through 12, just beneath the left diaphragm. The spleen lies behind and to the left side of your stomach (see Figure 1). The normal sized spleen abuts the stomach, colon, and left kidney The spleen resembles a large lymph node and is subdivided into lobules (see Figure 3). However, unlike the lymphatic sinuses of a lymph node, the spaces in the spleen, called venous sinuses, are filled with blood instead of lymph.
A normal spleen ranges in length from 6 to 13 cm and in weight from 75 to 200 g 3. The spleen is not normally palpable except in slender young adults 3. When the spleen can be felt below the left costal (rib) margin, at rest or on inspiration, spleen enlargement should be assumed and the explanation sought. Although the normal-size or even the abnormally small, spleen can be involved in pathologic processes, with the exception of rubs associated with splenic infarcts, physical examination is generally not helpful in identifying the problem. Nevertheless, the enlarged and palpable spleen is an important clue to the presence of a variety of illnesses 3.
Figure 1. Spleen
Figure 2. Spleen location
Figure 3. Spleen and the lymphatic system
 Spleen function
Spleen function
The spleen has several functions, including the filtering of blood, removing microbes and inadequate red blood cells (RBCs), producing white blood cells (WBCs), and antibody synthesis. As a filter organ, it strains senescent and/or defective red blood cells out of the circulating blood. Its “pitting” function removes cellular inclusions like Heinz and Howell Jolly bodies without destruction of erythrocytes. The spleen is the largest reservoir and disposal site for blood platelets 4. It is important to note, that while the spleen does have a wide range of functions, it is not a vital organ. Individuals can survive without a spleen as other organs of the body, such as the liver, can adapt in its absence to serve just about the same functions. The spleen consists of 2 different tissue types, termed white pulp and red pulp, with each tissue type serving unique functions (Figure 4). White pulp is composed of periarteriolar lymphoid sheaths (PALS) and lymphatic nodules. The white pulp tissue is involved with the production and maturity of white blood cells, particularly lymphocytes (B and T lymphocytes) and thereby the production of antibodies. The red pulp is composed of splenic sinusoids (wide blood vessels) and cords/threads of connective tissue. The red pulp tissue is involved more so with the filtering aspect of the blood. The red pulp removes old, damaged, and/or useless red blood cells. Contained within the red pulp are also white blood cells, particularly phagocytes (macrophages in particular) which destroy microorganisms such as viruses, bacteria, and fungi. The red pulp also acts as a storage area for white blood cells and platelets, which are typically released to injury sites to aid in healing and inflammation regulation or to assist in blood loss compensation. The white and red pulp regions are separated by a border known as the marginal zone which functions as a filter, filtering pathogens out of the blood and into the white pulp 5.
Figure 4. Spleen anatomy
Reasons for spleen removal
Splenectomy is used to treat a wide variety of diseases and conditions. Your doctor may recommend splenectomy if you have one of the following:
Table 1. Indications for total or partial splenectomy
| Diagnostic reasons | Therapeutic reasons |
|---|---|
| – Splenomegaly of unknown etiology | – Congenital red cell disorders |
| – Intrasplenic lesions of unknown significance | – Autoimmune hemolytic anemia |
| – Evaluation of residual disease after chemo–radiotherapy for a malignancy | – Idiopathic thrombocytopenia |
| – Thrombotic thrombocytopenic purpura | |
| – Myeloproliferative syndrome (myelofibrosis) | |
| – Hypersplenism | |
| – Gaucher’s disease |
- Ruptured spleen. If your spleen ruptures due to a severe abdominal injury or because of an enlarged spleen (splenomegaly), the result may be life-threatening, internal bleeding.
- Enlarged spleen. Splenectomy may be done to ease the symptoms of an enlarged spleen, which include pain and a feeling of fullness.
- Blood disorder. Blood disorders that may be treated with splenectomy include idiopathic thrombocytopenic purpura, polycythemia vera and thalassemia. But splenectomy is typically performed only after other treatments have failed to reduce the symptoms of these disorders.
- Cancer. Cancers that may be treated with splenectomy include chronic lymphocytic leukemia, Hodgkin’s lymphoma, non-Hodgkin’s lymphoma and hairy cell leukemia.
- Infection. A severe infection or the development of a large collection of pus surrounded by inflammation (abscess) in your spleen may require spleen removal if it doesn’t respond to other treatment.
- Cyst or tumor. Noncancerous cysts or tumors inside the spleen may require splenectomy if they become large or are difficult to remove completely.
The spleen is one of the abdominal organs with the greatest incidence of injury, with rupture being a big concern possibly justifying splenectomy to avoid excessive hemorrhaging into the peritoneal cavity. A rupture is characterized by a break of the capsule encasing the spleen and disruption of the parenchyma beneath. Such rupture may be caused by blunt force or penetrating trauma. It is also important to note that splenic rupture should be watched for in the presence of left rib fractures as it is not uncommon for a rib bone fragment to puncture the spleen.
The spleen may also become enlarged (splenomegaly) for a variety of reasons. Some of these reasons include viral or bacterial infection, vein blockages and related increased venous pressure, cancer, and circulations issues relate to abnormal cells. Splenic enlargement poses a risk for splenic rupture which may warrant surgical removal. An enlarged spleen may be palpable allowing for detection upon physical examination and may be further evaluated via radiographic imaging studies.
Your doctor may also remove your spleen to help diagnose a condition, especially if you have an enlarged spleen and he or she can’t determine why.
Spleen removal side effects
Splenectomy is generally a safe procedure. But as with any surgery, splenectomy carries the potential risk of complications, including:
- Bleeding
- Blood clots
- Infection
- Injury to nearby organs, including your stomach, pancreas and colon
Post-splenectomy syndrome
Post-splenectomy syndrome can occur after surgery to remove the spleen. It consists of a group of symptoms and signs such as:
- Blood clots
- Destruction of red blood cells
- Increased risk for severe infections from bacteria such as Streptococcus pneumoniae and Neisseria meningitidis
- Thrombocytosis (increased platelet count, which can cause blood clots)
Spleen removal procedure
Before the procedure
If you have time before the surgery, you may need to receive blood transfusions to ensure that you have enough blood cells after your spleen is removed.
Your doctor may also recommend that you receive a pneumococcal vaccine and possibly other vaccines to help prevent infection after your spleen is removed.
Right before your surgery, you will be given a general anesthetic. The anesthesiologist or anesthetist gives you an anesthetic medication such as a gas — to breathe through a mask — or as a liquid injected into a vein. The surgical team monitors your heart rate, blood pressure and blood oxygen throughout the procedure. You will have heart monitor leads attached to your chest and a blood pressure cuff on your arm.
During the procedure
After you’re unconscious, your surgeon begins the surgery using either a minimally invasive (laparoscopic) or open (traditional) procedure. The method used often depends on the size of the spleen. The larger the spleen, the more likely your surgeon will choose to do an open splenectomy.
Laparoscopic splenectomy
Most splenectomies are carried out using laparoscopy (keyhole surgery) and you will still need a general anesthetic. During laparoscopic splenectomy, the surgeon makes four small incisions in your abdomen. He or she then inserts a tube with a tiny video camera into your abdomen through one of the incisions. A laparoscope is long, thin, flexible instrument with its own light source. It is attached to a camera and will relay high definition, magnified pictures back to a TV screen to guide the surgeon’s instruments. Your surgeon watches the video images on a monitor and removes the spleen with special surgical tools that are put in the other three incisions. Then he or she closes the incisions. Laparoscopic splenectomy isn’t appropriate for everyone. A ruptured spleen usually requires open splenectomy. In some cases a surgeon may begin with a laparoscopic approach and find it necessary to make a larger incision because of scar tissue from previous operations or other complications.
Open surgery (laparotomy) splenectomy
During open splenectomy, the surgeon makes one large incision in the middle of your abdomen and moves aside muscle and other tissue to reveal your spleen. He or she then removes the spleen and closes the incision.
Open surger may be needed if the spleen is too large or too damaged to be removed via keyhole surgery. Often, in emergencies, this will be the preferred method to rapidly control bleeding.
You’ll need a general anaesthetic and may need to stay in hospital for a few days to recover.
Partial removal of the spleen
A partial resection of the spleen may be necessary as a diagnostic procedure in suspected hematological disorders with inconclusive hematologic findings, or in Gaucher’s disease with significant splenomegaly 6.
After full mobilization and rotation onto the abdominal wall, the vessels of the part to be resected are selectively ligated and severed. The spleen is compressed digitally at the demarcation line and the parenchyma is thereby squeezed toward the part to be removed. A stapler is used to perform the resection 7. The cut edge is sealed with fibrin glue and collagen fleece.
After the procedure
- In the hospital. After surgery, you’re moved to a recovery room. If you had laparoscopic surgery, you’ll likely go home the same day or the day after. If you had open surgery, you may be able to go home after two to six days.
- After you go home. Talk to your doctor about how long to wait until resuming your daily activities. If you had laparoscopic surgery, it may be two weeks. After open surgery, it may be six weeks.
If you had splenectomy due to a ruptured spleen, further treatment usually isn’t necessary. If it was done to treat another disorder, additional treatment may be required.
Spleen removal recovery time
It’s normal to feel sore and be bruised after a splenectomy, but you’ll be given pain relief medication.
You should be able to eat and drink as normal soon after the operation.
Like any operation, a splenectomy carries a small risk of complications, including bleeding and infection.
Your doctor will run through these risks with you.
You should be given breathing and leg movement exercises to do at home, to reduce your risk of getting a blood clot or a chest infection.
Another risk is the surgical wound becoming infected. If you spot any signs of infection, contact your doctor or hospital immediately, as you may need antibiotics.
Recovery usually takes a few weeks. Your doctor or nurse will advise when you can go back to your usual activities, such as driving.
The scars from your operation will gradually fade.
How you can care for yourself at home
Activity
- Rest when you feel tired. Getting enough sleep will help you recover.
- Try to walk each day. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- Avoid strenuous activities, such as biking, jogging, weight lifting, or aerobic exercise, until your doctor says it is okay.
- Avoid lifting anything that would make you strain. This may include heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, a vacuum cleaner, or a child.
- Ask your doctor when you can drive again.
- You will probably need to take 4 to 6 weeks off from work. It depends on the type of work you do and how you feel.
- You may shower 24 to 48 hours after surgery, if your doctor says it is okay. Pat the cut (incision) dry. Do not take a bath for the first 2 weeks, or until your doctor tells you it is okay.
Spleen removal diet
- Eat several small meals each day. Slowly increase the amount you eat. It’s common to feel full quickly after having this surgery.
- If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- Your doctor may tell you to take iron supplements.
- Drink plenty of fluids to avoid becoming dehydrated.
- You may notice that your bowel movements are not regular right after your surgery. This is common. Avoid constipation and straining with bowel movements. You may want to take a fiber supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
Medicines
- Your doctor will tell you if and when you can restart your medicines. He or she will also give you instructions about taking any new medicines.
- If you take blood thinners, such as warfarin (Coumadin), clopidogrel (Plavix), or aspirin, be sure to talk to your doctor. He or she will tell you if and when to start taking those medicines again. Make sure that you understand exactly what your doctor wants you to do.
- Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- You will need to take antibiotics for a while after surgery. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
- You may need blood transfusions if the number of blood cells is too low.
Wound care
- If you have strips of tape on the incision, leave the tape on for a week or until it falls off. Or follow your doctor’s instructions for removing the tape.
- Wash the area daily with warm, soapy water and pat it dry. Don’t use hydrogen peroxide or alcohol, which can slow healing.
- Take showers instead of baths for the next 2 weeks.
Life after splenectomy
After splenectomy, other organs such as the liver in your body take over most of the functions previously performed by your spleen. You can be active without a spleen, but you’re at increased risk of becoming sick or getting serious infections for the rest of your life. This risk is highest shortly after surgery. People without a spleen may also have a harder time recovering from an illness or injury.
To reduce your risk of infection, your doctor may recommend vaccines against pneumonia, influenza, Haemophilus influenzae type b (Hib) and meningococci. In some cases, he or she may also recommend preventive antibiotics, especially for children under 5 and those with other conditions that increase the risk of serious infections.
After splenectomy, call your doctor at the first sign of an infection, such as:
- A fever of 100.4 °F (38 °C) or higher
- Redness or tender spots anywhere on the body
- A sore throat
- Chills that cause you to shake or shiver
- A cold that lasts longer than usual
- Unexplained cough
- Severe abdominal pain
- Headache
- Drowsiness.
Make sure anyone caring for you knows that you’ve had your spleen removed. Consider wearing a medical alert bracelet that indicates that you don’t have a spleen.
Vaccination after splenectomy
With the absence of a spleen, individuals lose some of their immunological potentials, resulting in the lesser potential to combat disease and infection. After spleen removal you’re more likely to contract serious or life-threatening infections including those brought upon by Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Thus, it is recommended that patients who have a surgical history of splenectomy be vaccinated accordingly to reduce vulnerability.
Your doctor may recommend that you receive vaccines against pneumonia, influenza, Haemophilus influenzae type b (Hib) and meningococci. He or she may also recommend that you take preventive antibiotics, especially if you have other conditions that increase your risk of serious infections.
Make sure you have had all your routine childhood vaccinations. You should also be vaccinated against:
- Pneumococcal infections such as pneumonia, with regular boosters at least every five years
- Flu or influenza (get the seasonal flu jab every autumn)
- Haemophilus influenzae type b (Hib)
- Meningitis C
Antibiotics
It’s recommended that you take low-dose antibiotics for the rest of your life to prevent bacterial infections. Children who have a splenectomy might need to take antibiotics for at least 2 years after the procedure. If you plan to travel to remote areas or won’t have a doctor available, you should have a supply of antibiotics with you in case of infection. Talk to your doctor about which antibiotics are right for you.
Antibiotics are particularly important:
- for children under the age of 16
- for the first two years after your spleen is removed
- if your immune system doesn’t work properly
Be alert for signs of infection:
Watch out for signs of infection, such as:
- high temperature (fever)
- sore throat
- cough
- severe headache
- headache with drowsiness or a rash
- abdominal pain
- redness and swelling around the surgical wound
Your doctor can prescribe a course of antibiotics for you to use if you get an infection. You should start taking them at the first sign of an infection, so see your doctor as soon as possible.
If your infection becomes serious, you will be admitted to hospital.
Animal and tick bites
If you travel to tropical countries, you are at higher risk of contracting malaria. You are more likely to get babesiosis, an infection transmitted by deer ticks. Let your doctor know if you plan to travel to areas where these conditions are common. You are also at higher risk of infection from a dog bite. Seek care immediately if a dog bites you, or if you notice a rash that forms after you are bitten by a tick.
Bites from animals and ticks (small blood-sucking parasites) can cause infections.
If you get bitten by an animal, particularly a dog, start your course of antibiotics and seek medical advice urgently.
If you go trekking or camping regularly, you may be at risk of babesiosis, which is a rare disease transmitted by ticks. Try to avoid tick bites by wearing clothes that cover your skin, particularly long trousers. If you become ill, get medical advice straight away.
Telling medical staff about your condition
Healthcare professionals will mark your health records to show that you don’t have a working spleen. However, always remember to tell any medical professionals that you see, including your dentist.
Carry medical ID
It’s a good idea to carry or wear some medical ID. For example:
- if your spleen is removed, the hospital may give you a splenectomy card to take home with you
- you may want to buy your own medical ID, such as a MedicAlert or Medi-Tag bracelet or pendant
If you need help or emergency treatment, your medical ID will alert the staff to your condition.
Travel abroad
If you’re traveling abroad:
- you may be advised to take a course of antibiotics with you
- find out if you need an extra meningitis vaccination (types ACWY)
- check if you need any travel vaccinations
People without a working spleen have an increased risk of developing a severe form of malaria. If possible, avoid countries where malaria is present. If you can’t, speak to your doctor or local pharmacist about anti-malaria medicine before you travel. You should also use mosquito nets and insect repellent.
Splenectomy complications
Possible long-term medical problems include:
- Hardening of the arteries (atherosclerosis)
- Pulmonary hypertension (a disease affecting the blood vessels in your lungs)
Young children have a higher risk of serious infection than adults, but the risk is still small. The risk is also increased if you have a medical condition such as sickle cell anemia, celiac disease or a condition that affects your immune system, such as HIV.
This risk can be minimized by following simple precautions to prevent infection.
References- Akoury T, Whetstone DR. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 27, 2018. Splenic Rupture.
- Hijazi LS, Mead T. Functional Asplenism. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499949
- Armitage JO. Spleen. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 150. Available from: https://www.ncbi.nlm.nih.gov/books/NBK258/
- Uranüs S (1995) Current spleen surgery. Zuckschwerdt, Munich, p 11
- Bajwa SA, Kasi A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 13, 2018. Anatomy, Abdomen and Pelvis, Accessory Spleen.
- Uranüs S, Sill H. Splenectomy for hematological disorders. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001. Available from: https://www.ncbi.nlm.nih.gov/books/NBK6913
- Uranüs S, Mischinger H J, Pfeifer J, Kronberger L, Rabl H, Werkgartner G, Steindorfer P. Hemostatic methods for the management of spleen and liver injuries. World J Surg. (1996);20:1107–1111.