Still’s murmur
Still’s murmur is an innocent heart murmur (harmless/functional sound produced by a flow of blood through the heart) named for the doctor, Dr. George Frederic Still, who first described it in 1909 1. Still’s murmur murmur is most often heard in healthy children 3 to 7 years old, but it can be present at any age. Still’s heart murmur will not cause any symptoms or problems. Innocent murmurs DO NOT need treatment. However, Still’s murmur is also the most commonly misdiagnosed murmur, resulting in a high number of unnecessary referrals to pediatric cardiologist 2.
A normal heart murmur can get louder when the blood flows faster through the heart, like when kids have a fever or run around. That’s because an increase in body temperature or activity makes the heart pump more blood. When your temperature goes down, the murmur may get quieter or even disappear.
It can be easier to hear heart murmurs in children because they have less fat, muscle, and bone between the heart murmur and the doctor’s stethoscope. Many normal murmurs become harder to hear as children grow older, and some eventually disappear.
Even though most heart murmurs do not mean anything is wrong, sometimes a heart problem can cause a murmur. The heart may have a hole in it, a heart valve may leak, or a valve may not open all the way.
If your doctor thinks your heart murmur could be due to a heart problem, you will need to see a pediatric cardiologist. Referral of a child to a pediatric cardiologist for evaluation of innocent heart murmur has a significant impact that extends beyond the patient. Diagnosis of heart murmur, even if innocent, is associated with significant healthcare resource utilization and parental/caregiver anxiety 3. Appropriate use criteria for initial transthoracic echocardiography were released by the American Academy of Pediatrics, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, etc. in the year 2014 which clearly notes transthoracic echocardiogram for presumed innocent heart murmur as “rarely appropriate” indication 4. Despite published guidelines, there is a significant utilization of transthoracic echocardiography as well as recurrent cardiology visits for innocent heart murmur 3. Giuffre et al. 5 and Bardsen et al. 6 looked at parental anxiety after a diagnosis of childhood heart murmur. Both studies reported significantly higher anxiety level in parents after the initial diagnosis. Even when the parents were given a handout regarding innocent heart murmur prior to the evaluation by a cardiologist, it did not decrease the anxiety significantly. Parental anxiety was significantly relieved after evaluation and counseling by a pediatric cardiologist. It should be further explained to parents that child may never “outgrow” the murmur and murmur may only be intermittently audible.
- Symptoms such as chest pain
- Family history of Marfan syndrome or sudden death in young family members
- Malformation syndrome (e.g., Down syndrome)
- Increased precordial activity
- Decreased femoral pulses
- Abnormal second heart sound
- Clicks
- Loud or harsh murmur
- Increased intensity of murmur when patient stands
A patient who has a pathologic cardiac examination or who has cardiac symptoms and questionable findings on the cardiac examination should be referred to a pediatric cardiologist. A child with a malformation syndrome associated with congenital heart disease should also be referred for additional evaluation. Conversely, an asymptomatic patient whose physical findings on a conscientiously performed cardiac examination indicate a low probability of cardiac pathology should be followed by the primary care physician. Referral is indicated if possibly pathologic findings emerge on serial examinations 7.
Still’s murmur diagnosis
Your healthcare provider can listen to your heart sounds by placing a stethoscope on your chest. You will be asked questions about your medical history and symptoms, such as:
- Have other family members had murmurs or other abnormal heart sounds?
- Do you have a family history of heart problems?
- Do you have chest pain, fainting, shortness of breath, or other breathing problems?
- Have you had swelling, weight gain, or bulging veins in the neck?
- Does your skin have a bluish color?
A detailed birth history, past medical history, growth chart assessment, detailed family history, and head-to-toe assessment are essential components that help with making a competent clinical diagnosis 8.
Your healthcare provider may ask you to squat, stand, or hold your breath while bearing down or gripping something with your hands to listen to your heart.
Things your healthcare provider will look for in the exam include:
- Does the murmur occur when the heart is resting or contracting?
- Does it last throughout the heartbeat?
- Does it change when you move?
- Can it be heard in other parts of the chest, on the back, or in the neck?
- Where is the murmur heard the loudest?
The following tests may be done:
- Chest x-ray to see if your heart looks bigger than normal.
- Electrocardiogram (ECG) which measures electrical activity of the heart.
- Echocardiography. This test uses sound waves to make a picture of the heart as blood is pumped through its chambers and valves. It takes about 20 minutes and it doesn’t hurt either.
Your doctor will take the information from the tests and exam and determine if your murmur is likely to cause a problem for you.
Heart anatomy
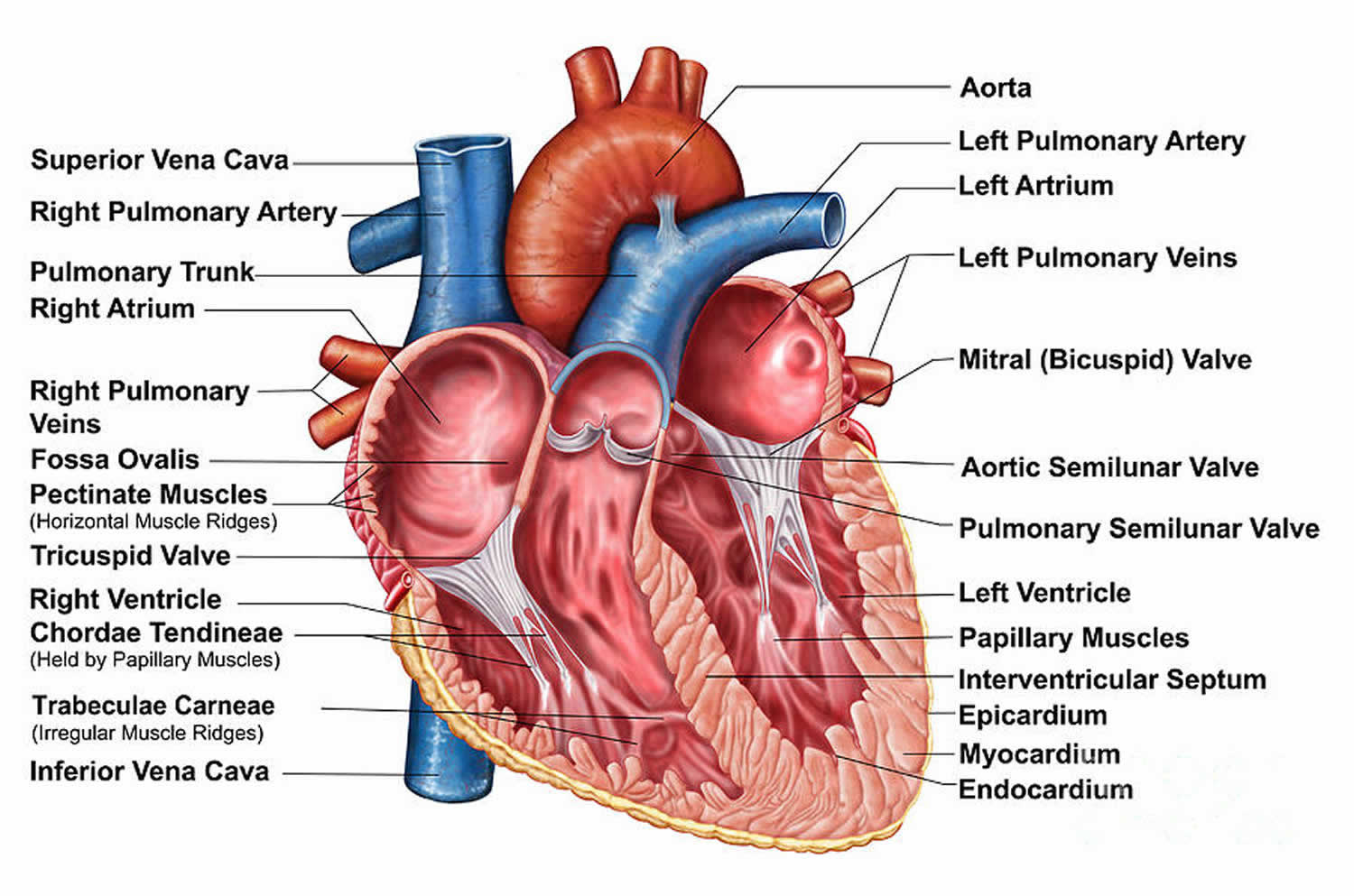
The heart has 4 chambers (Figure 1):
- Two upper chambers (atria)
- Two lower chambers (ventricles)
The heart has valves that close with each heartbeat, causing blood to flow in only one direction. The valves are located between the chambers.
Figure 1. Heart chambers
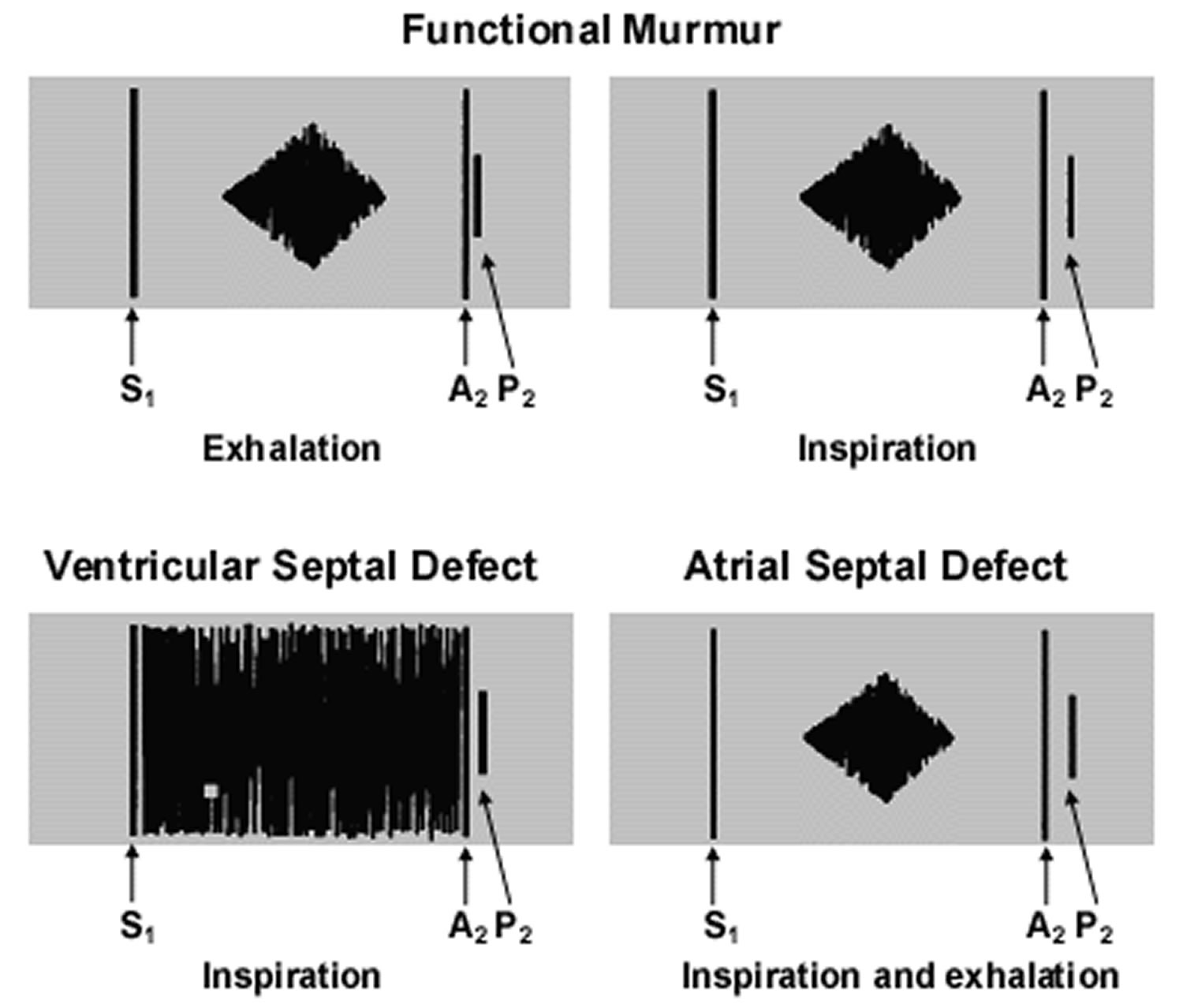
Figure 2. Innocent murmurs
Footnote: Graphic representation of common pediatric murmurs. The diamond-shaped murmurs are crescendo/decrescendo. The murmur of a ventricular septal defect obscures the closure sound of the mitral and tricuspid valves and is termed “holosystolic.” (S1 = first heart sound; P2= pulmonic second sound; A2 = aortic second sound)
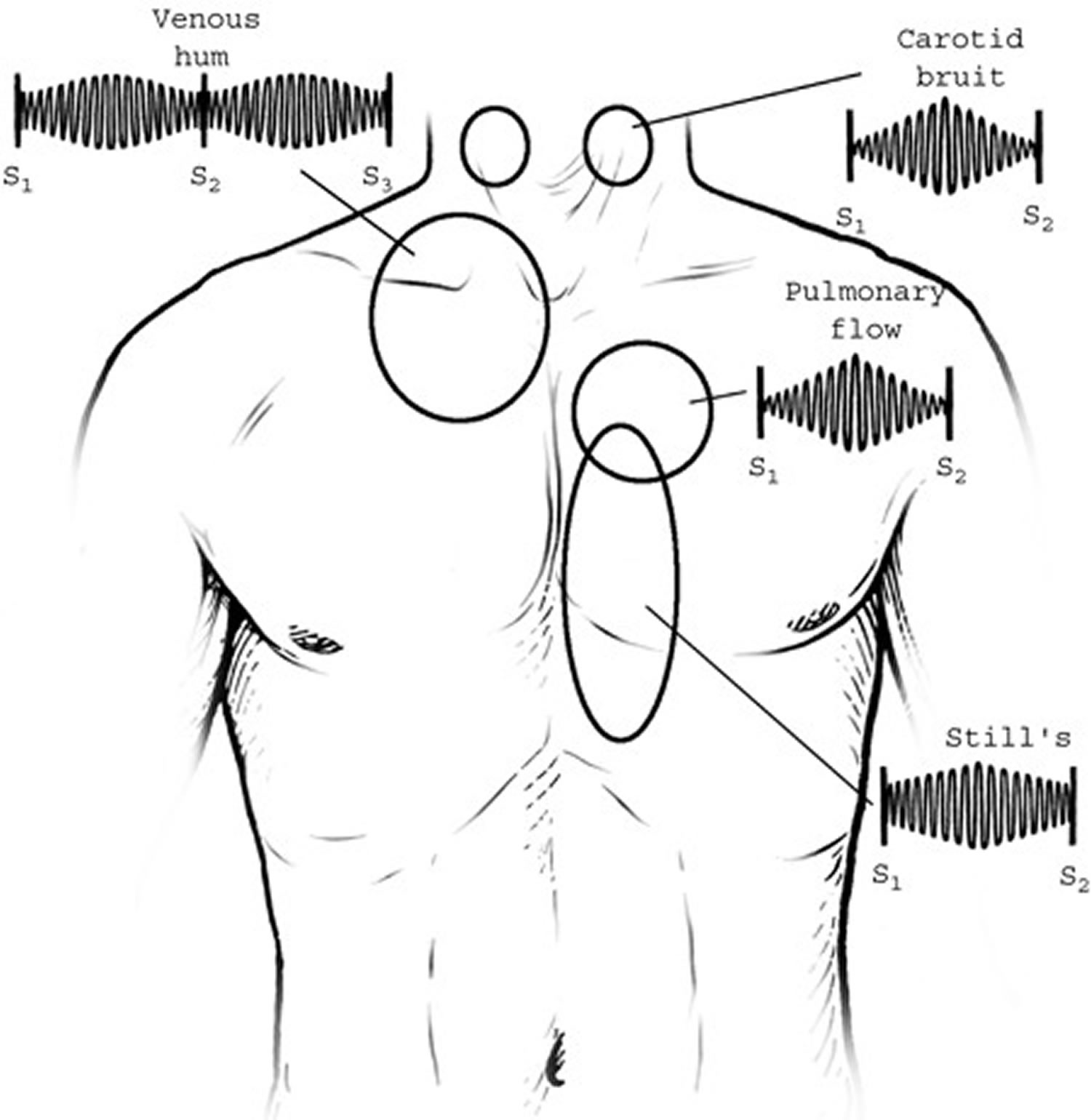
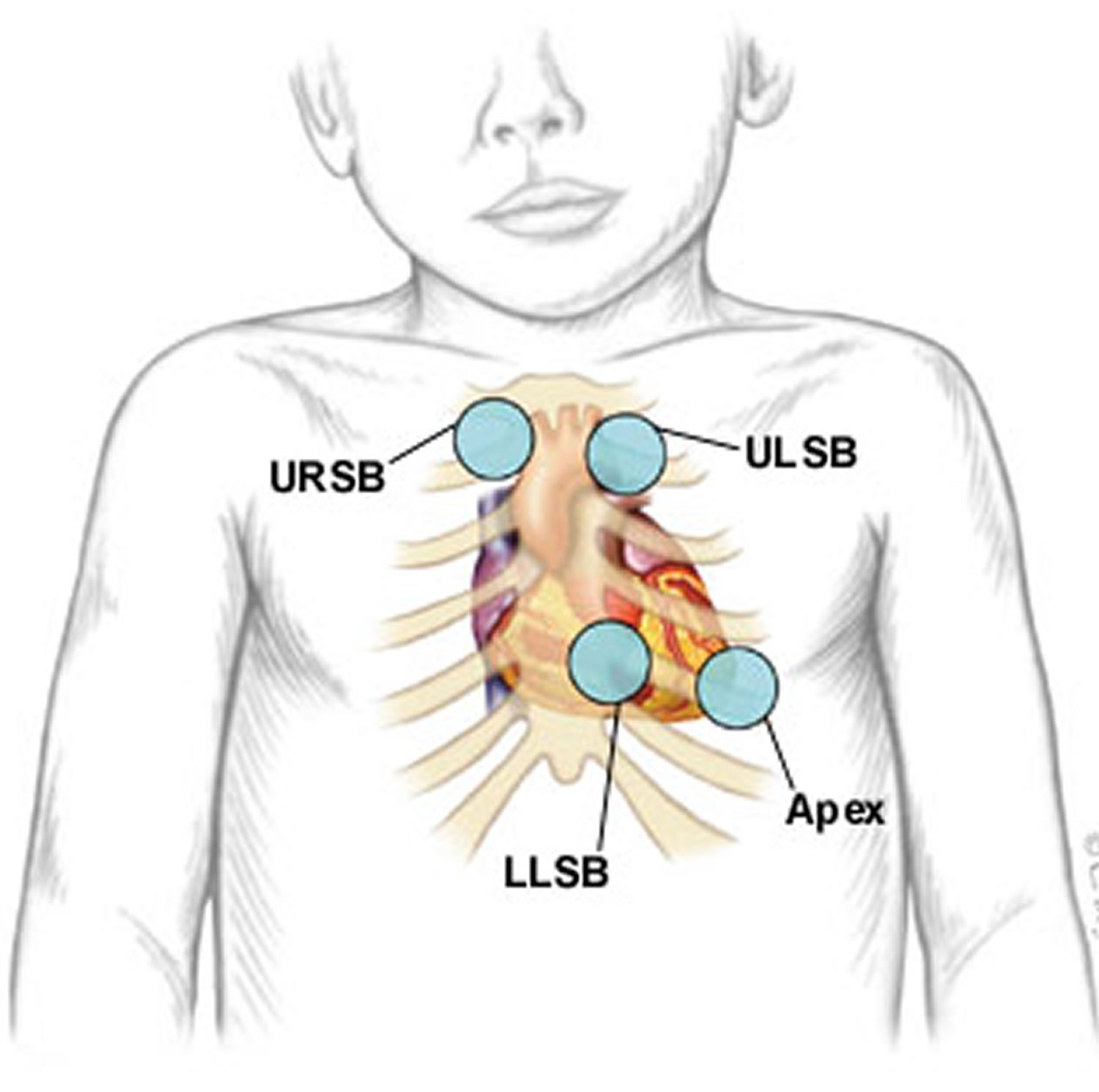
Figure 3. Listening areas for heart clicks
Footnote: Upper right sternal border (URSB) for aortic valve clicks; upper left sternal border (ULSB) for pulmonary valve clicks; lower left sternal border (LLSB), or the tricuspid area, for ventricular septal defects; apex for aortic or mitral valve clicks.
Precordial palpation
The cardiac examination begins with palpation to assess precordial activity and femoral pulses. Increased precordial activity is commonly felt in patients with increased right or left ventricular stroke volume. Increased pre-cordial activity occurs in patients with an atrial septal defect, a moderate or large ventricular septal defect or significant patent ductus arteriosus. This increased activity should raise the possibility that the auscultatory findings may be pathologic. Other explanations for increased precordial activity include patient anxiety, anemia and hyperthyroidism.
Once both brachial pulses have been palpated, the right brachial pulse should then be palpated simultaneously with the femoral pulse. If the timing and intensity of the two pulses are equal and blood pressure in the right arm is normal, coarctation of the aorta is unlikely.
Precordial palpation is also necessary to feel “thrills,” which are the palpable consequence of blood flowing rapidly from high pressure to lower pressure. Some ventricular septal defects result in thrills at the lower left sternal border. Moderate to severe pulmonary valve stenosis may cause a thrill at the upper left sternal border. A thrill resulting from aortic stenosis is frequently palpable in the suprasternal notch.
There are several ways in which your health care provider may describe a murmur:
- A murmur is described by the stage of the heartbeat when the murmur is heard. A heart murmur may be described as systolic or diastolic. Systole is when the heart is squeezing out blood and diastole is when it is filling up with blood.
- Systolic murmurs have only a few possible causes: blood flow across an outflow tract (pulmonary or aortic), a ventricular septal defect; atrioventricular valve regurgitation, or persistent patency of the arterial duct (ductus arteriosus). Systolic murmurs can also be functional (benign).
- All diastolic murmurs are pathologic and therefore warrant referral.
- Murmurs are classified (“graded”) depending on how loud the murmur sounds with a stethoscope. Systolic murmurs are graded on a six-point scale. Grade 1 murmur is barely audible, a grade 2 murmur is louder and a grade 3 murmur is loud but not accompanied by a thrill. A grade 4 murmur is loud and associated with a palpable thrill. A grade 5 murmur is associated with a thrill, and the murmur can be heard with the stethoscope partially off the chest. Finally, the grade 6 murmur is audible without a stethoscope. All murmurs louder than grade 3 are pathologic. An example of a murmur description is a “grade 2/6 murmur.” This means the murmur is grade 2 on a scale of 1 to 6.
- Description of character or tone, of a murmur. The character, or tone, of a murmur may aid in the diagnosis. Words such as “harsh,” “whooping,” “honking,” “blowing,” “musical” and “vibratory” may be useful, albeit somewhat subjective, in describing murmurs. A “harsh” murmur is consistent with high-velocity blood flow from a higher pressure to a lower pressure. “Harsh” is often appropriate for describing the murmur in patients with significant semilunar valve stenosis or a ventricular septal defect. “Whooping” or “blowing” murmurs at the apex occur with mitral valve regurgitation. The term “flow murmur” is often used to describe a crescendo/decrescendo murmur that is heard in patients with a functional murmur (see Figure 2). However, similar systolic ejection murmurs may be heard in patients with atrial septal defect, mild semilunar valve stenosis, subaortic obstruction, coarctation of the aorta or some very large ventricular septal defects. Many functional or innocent murmurs are “vibratory” or “musical” in quality. Still’s murmur is the innocent murmur most frequently encountered in children. This murmur is usually vibratory or musical 9.
- First heart sound (S1). Auscultation begins with listening for the first heart sound (S1) at the lower left border of the sternum. The first heart sound (S1) is caused by closure of the mitral and tricuspid valves and is normally a single sound. An inaudible S1 indicates that some sound is obscuring the closure sound of these valves. The differential diagnosis for murmurs that obscure S1 includes ventricular septal defects, some murmurs caused by atrioventricular valve regurgitation, patent ductus arteriosus and, occasionally, severe pulmonary valve stenosis in a young child. These S1-coincident murmurs are also known as “holosystolic” murmurs.
- Heart Clicks. If S1 is audible but appears to have two components at some spots in the precordium, the patient has either a click or an asynchronous closure of the mitral and tricuspid valves. Clicks may originate from any valve in the heart. Depending on their origin, clicks have different identifying characteristics.
- Ejection clicks originating from the pulmonic valve begin shortly after the atrioventricular valves close, vary with respiration and are best heard at the upper to middle area of the left sternal border. Aortic valve ejection clicks begin shortly after S1 and are best heard at the apex. They do not vary with respiration.
- Systolic clicks originating from the mitral valve are best heard at the apical area when the patient is standing. Occasionally, the tissue closing a ventricular septal defect can pop or click early in systole (Figure 3).
- Second heart sound (S2). Second heart sound (S2) is caused by closure of the aortic and pulmonic valves. After auscultation for clicks throughout the four listening areas, the next step is to return to the upper left sternal border and listen to the second heart sound (S2). The S2 should split into two components when the patient inspires. The first component, aortic second sound (A2), is closure of the aortic valve. The second component, pulmonic second sound (P2), is caused by closure of the pulmonary valve. The splitting of S2 occurs because inspiration brings more blood into the right ventricle. Right ventricular ejection is prolonged, and the pulmonary valve closes later. An awareness of this phenomenon is helpful in understanding the physical examination features of the patient with an atrial septal defect. A loud, single S2 indicates either pulmonary hypertension or congenital heart disease involving one of the semilunar valves.
Characteristics of pathologic murmurs include a sound level of grade 3 or louder, a diastolic murmur or an increase in intensity when the patient is standing. Most children with any of these findings should be referred to a pediatric cardiologist.
When a murmur is more noticeable, your healthcare provider may be able to feel it with the palm of the hand over the heart. This is called a “thrill”.
Location of the highest intensity of a murmur
The location of the highest intensity of a murmur is also important (Table 1). A murmur caused by aortic stenosis is often best heard at the upper sternal border, usually on the right side. A murmur resulting from pulmonary stenosis is heard best at the upper left sternal border. A murmur caused by a ventricular septal defect or tricuspid valve insufficiency is heard at the lower left sternal border. A murmur resulting from mitral valve regurgitation is best heard at the apex.
Table 1. Listening Areas for Common Pediatric Heart Murmurs
| Area | Murmur |
|---|---|
Upper right sternal border | Aortic stenosis, venous hum |
Upper left sternal border | Pulmonary stenosis, pulmonary flow murmurs, atrial septal defect, patent ductus arteriosus |
Lower left sternal border | Still’s murmur, ventricular septal defect, tricuspid valve regurgitation, hypertrophic cardiomyopathy, subaortic stenosis |
Apex | Mitral valve regurgitation |
Position changes in differentiation of murmurs
Position changes are very helpful in differentiating functional and pathologic murmurs. The vibratory functional murmur heard in a young child (Still’s murmur) decreases in intensity when the patient stands.
Most pathologic murmurs do not change significantly with standing. An important exception is the murmur of hypertrophic cardiomyopathy, a potentially life-threatening condition. This murmur increases in intensity when the patient stands. In the upright position, venous return to the heart is reduced, decreasing the left ventricular end diastolic volume. As left ventricular size decreases, the left ventricular outflow tract narrows, and the systolic outflow obstruction increases. This narrowing increases the intensity of the murmur. Overall, hypertrophic cardiomyopathy is rare; however, it is one of the leading causes of sudden death in athletes 11.
Physical findings in Innocent Heart Murmur and Atrial Septal Defect
Many normal children have heart murmurs, but all of these children do not require referral to a pediatric cardiologist. Atrial septal defect is the pathologic diagnosis that is frequently missed or easily confused with a innocent murmur.
Perhaps the best way to decide whether a patient needs to be referred to a pediatric cardiologist is to know confidently the clinical findings of the atrial septal defect (ASD) 10. The abnormal findings in patients with atrial septal defects are often quite subtle and thus are easily confused with the physical findings in patients with functional or innocent murmurs (Table 2). Loud murmurs from ventricular septal defects or significant aortic or pulmonic stenosis are not subtle and are not often confused with innocent murmurs.
Table 2. Physical findings in Innocent Heart Murmur and Atrial Septal Defect
| Physical finding | Innocent murmur | Atrial septal defect |
|---|---|---|
Precordial activity | Normal | Increased |
First heart sound (S1) | Normal | Normal |
Second heart sound (S2) | Splits and moves with respiration | Widely split and fixed (i.e., does not move with inspiration) |
Systolic murmur (supine) | Crescendo/decrescendo | Crescendo/decrescendo |
Possibly vibratory at lower left sternal border | “Flow” at upper left sternal border | |
Systolic murmur (standing) | Decreases in intensity | Does not change |
Diastolic murmur | Venous hum | Inflow “rumble” across tricuspid valve area |
The first step in the examination is palpation for the precordial activity at the left sternal border, feeling for increased activity that may be present from right ventricular enlargement. The examination is performed with the patient in a supine position.
Auscultation at the lower left sternal border should reveal a normal, single and easily audible S1. Listening at the upper left sternal border for S2 should reveal variable splitting with respiration. A widely split S2 that does not change with respiration indicates either complete right bundle branch block or an atrial septal defect.
Because of the increased volume of blood in the right ventricle in the patient with an atrial septal defect, the S2 always sounds as if the patient has taken a deep breath. This means that the volume of blood in the right ventricle is increased and it takes longer for the ventricle to eject its contents, thus leading to a fixed, widely split S2.
Murmurs heard in patients with atrial septal defects are often of low pitch and intensity. However, the intensity of the murmur is not a reliable basis for the diagnosis. The systolic murmur is caused by an increased volume of blood coursing across the right ventricular outflow tract. If the murmur is audible, it can be heard at the upper left sternal border.
Patients with atrial septal defects may also have a diastolic murmur. In this situation, increased diastolic blood flow across the tricuspid valve may cause a soft, often barely audible low-frequency “diastolic rumble.” This sound is heard best with the bell of the stethoscope placed at the lower left sternal border. Pushing down with the bell causes the skin beneath the stethoscope to act as a diaphragm. Consequently, only the high-frequency sounds are heard. Releasing the tension on the bell allows the low-frequency rumbling sound to become audible at the lower left sternal border.
After the supine examination, the examination should be repeated with the patient standing. If the patient has an atrial septal defect, the features of increased precordial activity, a widely split S2, a systolic murmur at the upper left sternal border and a diastolic rumble should still be present when the patient is standing. If the patient has an innocent or functional murmur, the precordial activity should be normal, the S2 should split and move with respiration, the systolic murmur should decrease in intensity and no diastolic murmur should be present in the tricuspid valve area.
If no symptoms are present, the S1 is normal, the S2 splits and is of normal intensity, and no clicks are heard, the differential diagnosis of a grade 1 to grade 2 systolic murmur is frequently a choice between an atrial septal defect and a functional murmur.
In young children, it can be difficult to confidently distinguish the respiratory variation of S2 splitting in the patient with a normal murmur from the fixed S2 splitting in the patient with an atrial septal defect. Because the patient with an asymptomatic atrial septal defect will not develop pulmonary hypertension or other permanent sequelae early in life, careful yearly follow-up examination by the primary care physician can be recommended. By the time a child reaches preschool age, the normal or abnormal splitting of the S2 usually becomes clear.
Still’s murmur description
McKusick et al. 12 very appropriately suggested the musical instrument, Aeolian Island harp, as an analogue for Still’s murmur. Still’s murmur is a brief, vibratory quality, grade 1-3, midsystolic, and low-pitched murmur. This is best heard with the bell of a stethoscope. Still’s murmur is heard at the left lower sternal border and occasionally radiates to the cardiac apex. Typical age group for Still’s murmur is three years to early adolescence, but it can be present at any age. Because the innocent murmurs are produced by normal flow dynamics, any alteration in the flow with a change in patient position will change the murmur characteristics. Still’s murmur is the loudest in the supine (lying down) position and it diminishes in intensity when a child is made to sit or stand up, as these positions diminish the venous return to the heart. This could be a valuable tool while examining Still’s murmur in the clinic.
Some of the proposed mechanisms for the development of Still’s murmur are the presence of “fibrous bands” or “false tendon” in the left ventricle 13, smaller aortic size causing increase in the flow velocity 14, insertion of tricuspid valve chordae into the right ventricular outflow tract 15, increased left ventricular output with relative bradycardia 16, vibrations from cardiac structures 16, and lower aortic arterial elastance with a higher left ventricular contractility 17. There is no clear consensus on the mechanism of its origin at this time.
Types of innocent heart murmurs
Innocent heart murmurs in children can be categorized under four distinct groups 18:
- Still’s vibratory murmur,
- Pulmonary flow murmur,
- Supraclavicular systemic flow murmur,
- Venous hums.
Many high output states like anemia, fever, arteriovenous malformation, etc. can also result in heart murmur 1. Innocent murmurs DO NOT need treatment.
Pulmonary flow murmur
This is a harsh quality, grade 2-3, medium-high pitched, ejection systolic murmur. This murmur is best heard with the diaphragm of a stethoscope. It is thought to originate from the right ventricular outflow. It is best heard at the left upper sternal border over the “pulmonary area” and it often radiates to the back and/or axillae. This murmur can be very prominent in high output states and in patients with pectus excavatum deformity of the chest. Pulmonary flow murmur can be differentiated from pulmonary valve stenosis murmur by its quality and absence of pulmonary valve click. Pulmonary flow murmur is also very responsive to change in flow dynamics. The intensity increases with inspiration and lying down due to an increase in venous return, and decreases with standing up and Valsalva maneuver.
Supraclavicular systemic flow murmur
Supraclavicular systemic flow murmur is a harsh quality, crescendo-decrescendo, medium-high pitched, grade 2-3 murmur heard over the supraclavicular region with radiation to the carotids. This murmur is best heard with the diaphragm of a stethoscope and can be present in any pediatric age group as well as young adults. In contrast to aortic valve stenosis murmur, this is not accompanied by the systolic click of the aortic valve. This murmur is thought to arise from the normal flow of blood from the aorta into head-and-neck vessels 19. Supraclavicular systemic flow murmur is loudest in a supine position and it diminishes in intensity with hyperextension of the neck.
Venous hums
Many children with functional murmurs have venous hums. Venous hums is a continuous low-pitched murmur best heard over the lower neck, just lateral to the sternocleidomastoid muscles. Venous hum originates from the systemic venous return of the superior vena cava, by the flow of venous blood from the head and neck into the thorax. Due to its low-pitch, it is best heard with the bell of a stethoscope. Venous hums is very sensitive to position and disappears with making the child look down or to the side. Venous hums is most prominent in the sitting position and are heard continuously when the child is sitting. The sounds should disappear or diminishes on lying down. The sounds should disappear when light pressure is applied over the jugular vein, when the child’s head is turned or when the child is lying supine 10. Venous hums are common and are not pathologic. Patients with venous hums do not require pediatric cardiology referral. This can be easily differentiated by patent ductus arteriosus murmur which is harsh machinery in character and does not change or disappear with changing neck position.
References- Innocent murmurs: a suspect diagnosis in non-pregnant adults. Am J Cardiol. 2009 Sep 1;104(5):735-7. doi: 10.1016/j.amjcard.2009.04.031. Epub 2009 Jun 24. https://www.ajconline.org/article/S0002-9149(09)00999-0/fulltext
- S. Kang, R. Doroshow, J. McConnaughey and R. Shekhar, “Automated Identification of Innocent Still’s Murmur in Children,” in IEEE Transactions on Biomedical Engineering, vol. 64, no. 6, pp. 1326-1334, June 2017. doi: 10.1109/TBME.2016.2603787
- Recurrent cardiology evaluation for innocent heart murmur: echocardiogram utilization. Dalal NN, Dzelebdzic S, Frank LH, et al. Clin Pediatr. 2018;57:1436–1441.
- ACC/AAP/AHA/ASE/HRS/SCAI/SCCT/SCMR/SOPE 2014 appropriate use criteria for initial transthoracic echocardiography in outpatient pediatric cardiology: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Academy of Pediatrics, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. Campbell RM, Douglas PS, Eidem BW, Lai WW, Lopez L, Sachdeva R. J Am Coll Cardiol. 2014;64:2039–2060.
- Parental anxiety related to referral of childhood heart murmur; an observational/interventional study. Bardsen T, Sorbye MH, Tronnes H, Greve G, Berg A. BMC Pediatr. 2015;15:193.
- Opening Pandora’s box: parental anxiety and the assessment of childhood murmurs. Can J Cardiol. 2002 Apr;18(4):406-14. https://www.ncbi.nlm.nih.gov/pubmed/11992134
- Rosenthal A. How to distinguish between innocent and pathologic murmurs in childhood. Pediatr Clin North Am. 1984;31:1229–40.
- Innocent murmurs. Biancaniello T. Circulation. 2005;111:20–22.
- Pelech AN. The cardiac murmur: when to refer? Pediatr Clin North Am. 1998;45:107–22.
- Heart Murmurs in Pediatric Patients: When Do You Refer? Am Fam Physician. 1999 Aug 1;60(2):558-564. https://www.aafp.org/afp/1999/0801/p558.html
- Maron BJ, Epstein SE, Roberts WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol. 1986;7:204–14.
- Musical murmurs. Bull Johns Hopkins Hosp. 1955 Aug;97(2):136-76. https://www.ncbi.nlm.nih.gov/pubmed/13250286
- The possible etiology of the vibratory systolic murmur. Darazs B, Hesdorffer CS, Butterworth AM, Ziady F. Clin Cardiol. 1987;10:341–346.
- Still’s-like innocent murmur can be produced by increasing aortic velocity to a threshold value. Klewer SE, Donnerstein RL, Goldberg SJ. Am J Cardiol. 1991;68:810–812.
- Innocent murmurs: a suspect diagnosis in non-pregnant adults. Guntheroth WG. Am J Cardiol. 2009;104:735–737.
- Genesis of Still’s murmurs: a controlled Doppler echocardiographic study. Gardiner HM, Joffe HS. Br Heart J. 1991;66:217–220.
- Ventriculo-arterial coupling in children with Still’s murmur. Engel J, Baumgartner S, Novak S, Male C, Salzer-Muhar U. Physiol Rep. 2014;2:2–10.
- Doshi AR. Innocent Heart Murmur. Cureus. 2018;10(12):e3689. Published 2018 Dec 5. doi:10.7759/cureus.3689 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6368429
- Auscultatory and phonocardiographic findings in healthy children with systolic murmurs. Leatham A, Segal B, Shafter H. Br Heart J. 1963;25:451–459.