Tendon transfer surgery
Tendon transfer surgery is a highly specialized surgical procedure designed to restore function to either the elbow, ankle or to the wrist and hand, to improve control and function of upper or lower limbs. Tendon transfers are undertaken to restore muscle function and can be used for any kind of nerve injury. Tendon transfer surgery moves ‘spare’ muscles that are under voluntary control and uses them to compensate for paralyzed muscles. Surgeons perform tendon transfers by releasing one end of a tendon from bone or soft tissue and reconnecting it to another bone or tendon. Instead of moving the nerve supply from one muscle to another muscle — as is done with a nerve transfer — the surgeon takes the end of a tendon, cuts it and moves it to perform a different function.
As an example, a tendon transfer is commonly used to treat a radial nerve injury that limits mobility in the wrist and fingers. A surgeon will take some expendable tendons from the front of the forearm, which are innervated by a different nerve and normally produce flexion, and connect them to tendons on the back of the forearm to enable the patient to extend the wrist and fingers.
Tendon transfers are used to treat many conditions. They are indicated when muscle function is lost due to nerve injury, and the nerve can no longer send signals to the muscle and cannot be repaired. Some common injuries treated with tendon transfers are radial, ulnar and median nerve injury; foot drop due to peroneal nerve injury; and spine injury as well as hand paralysis due to spinal cord injury.
One benefit of moving tendons is that there is no time limitation. The window for successfully repairing nerves is about a year, but a tendon transfer can restore muscle function many years after the initial injury.
Tendon transfer surgery will usually mean a period of reduced mobility and restricted upper limb movement. This increased dependence is temporary, but frustrating and needs to be supported with extra assistance from others.
Your surgeon will select tendon transfer or other treatments based on your condition and which technique offers the best chance of recovery.
Tendon transfer surgery will not prevent any benefits from other spinal cord injury treatments. If in doubt about the potential benefit of tendon transfer surgery, ask for a specialized assessment so that you are given accurate information – the decision to go ahead with surgery remains with the individual.
Figure 1. Flexor digitorum longus tendon
What is a tendon?
The tendon is the strong fibrous cord made of collagen at either end of a muscle that is attached to bone. Tendons, combined with their muscles, allow you to move your joints.
Tendons have blood vessels and cells to maintain tendon health and repair injured tendon. Tendons are attached to muscles and to bone. As the muscle contracts it pulls on the tendon and the tendon moves the bone to which it is attached as well as any joints it crosses.
In the forearm and hand there are over forty different muscles. Many of these muscles perform overlapping functions. After an injury, some of your muscles may not move correctly. A tendon transfer is a surgery that moves a working muscle and tendon to replace a non-working muscle and tendon.
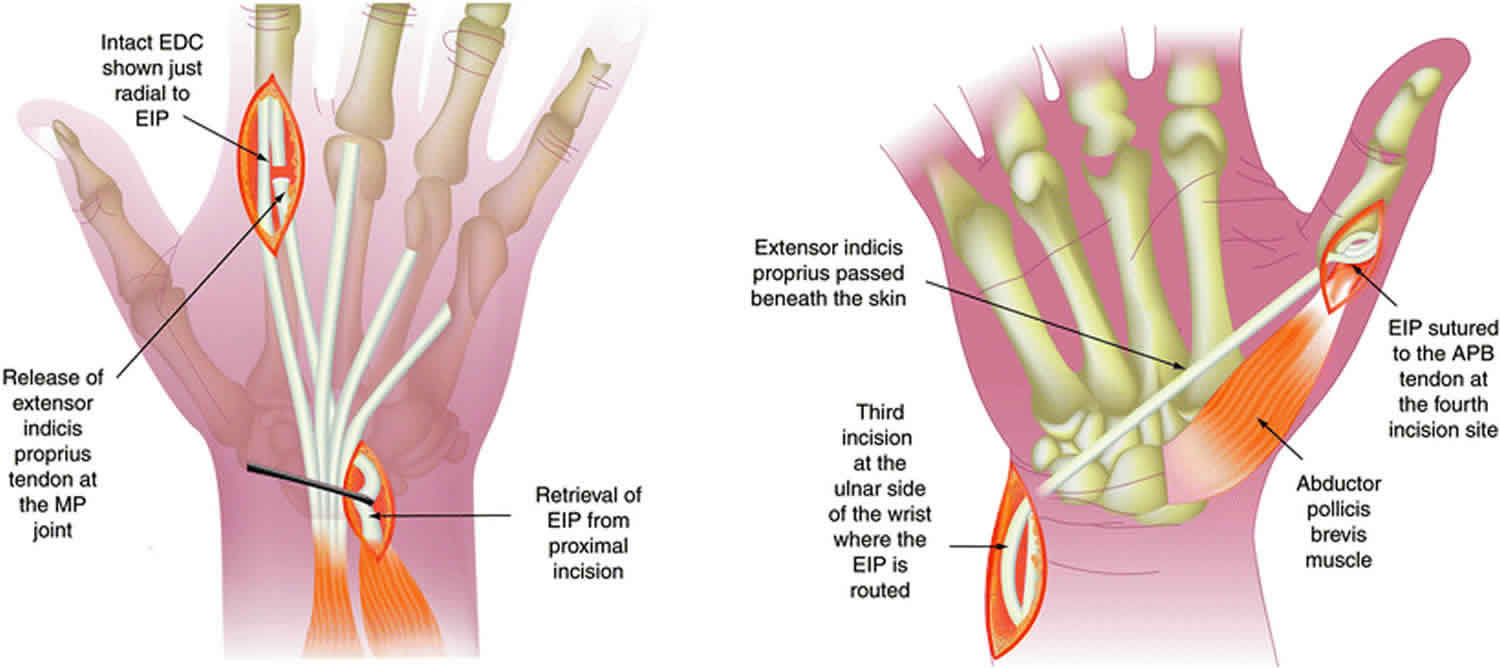
For example, after a broken wrist, the tendon to the thumb (extensor pollicis longus tendon) that allows you to make a “thumbs-up” can break. Often, the two ends of the tendon are very damaged and cannot be sewn back together. There are two tendons that extend the index finger, and this finger can function adequately with just one. A hand surgeon can transfer one of the index finger tendons to the thumb to allow you to give a “thumbs-up” again.
Who needs tendon transfer surgery?
Many different conditions can be treated by tendon transfer surgery. Tendon transfer surgery is necessary when a certain muscle function is lost because of a nerve injury. If a nerve is injured and cannot be repaired, then the nerve no longer sends signals to certain muscles. Those muscles are paralyzed and their muscle function is lost. Tendon transfer surgery can be used to attempt to replace that function. Common nerve injuries that are treated with tendon transfer surgery are spinal cord, radial nerve, ulnar nerve, or median nerve injury.
Tendon transfer surgery may also be necessary when a muscle has ruptured or been lacerated and cannot be repaired. Common muscle or tendon injuries that are treated with tendon transfer surgery are tendon ruptures due to rheumatoid arthritis or fractures. Also, tendon lacerations that cannot be repaired after injury may be treated with tendon transfer surgery.
Tendon transfer surgery may also be needed if a muscle function has been lost due to a disorder of the nervous system. In this situation, the nervous system disease or injury prevents normal nerve signals from being sent to a muscle, and imbalance in hand function occurs. The muscle imbalance or muscle loss due to nervous system disease may be treated with tendon transfers. Common nervous system disorders treated with tendon transfer surgery are cerebral palsy, stroke, traumatic brain injuries, and spinal muscle atrophy.
Finally, there are some conditions in which babies are born without certain muscle functions. In these situations, the missing muscle functions can sometimes be treated with tendon transfer surgery. Common conditions treated this way include hypoplastic thumbs and birth brachial plexopathy.
What happens during tendon transfer surgery?
During tendon transfer surgery, the origin of the muscle is left in place; the nerve supply and blood supply to the muscle is left in place. The tendon insertion onto bone is detached and re-sewn into a different place. It can be sewn into a different bone, or it can be sewn into a different tendon. After its insertion has been moved, when the muscle fires, it will produce a different action, depending on where it has been inserted.
Tendon transfer principles
Three important principles should be emphasized in tendon transfer operations 1.
- First, tendon transfer should not significantly decrease the remaining function of the hand.
- Second, tendon transfer should not create a deformity if significant return of function occurs following a nerve repair.
- Third, tendon transfer should be phasic or capable of phase conservation.
Fundamental principles of muscle-tendon units include the following.
Correction of contracture
In any patient with peripheral nerve palsy, all joints must be kept supple because soft-tissue contracture is far easier to prevent than it is to correct. Maximum passive motion of all joints must be present before a tendon transfer because no tendon transfer can move a stiff joint.
Adequate strength
The tendon chosen as a donor for transfer must be strong enough to perform its new function in its altered position. Selecting an appropriate motor is important because a muscle will lose one grade of strength following transfer. Do not transfer muscle that has been reinnervated or muscle that was paralyzed and has returned to function.
Amplitude of motion
Consider the amplitude of tendon excursion for each muscle. A wrist flexor with an excursion of 33 mm cannot substitute fully for a finger extensor with an amplitude of 50 mm. Although the true amplitude of a tendon cannot be increased, its effective amplitude can be augmented in either of the following two ways:
- The natural tenodesis effect can be used by converting a muscle from monoarticular to biarticular or multiarticular
- Extensively dissecting a muscle from its surrounding fascial attachments can increase amplitude
Straight line of pull
In the most effective transfer, the muscle passes in a direct line from its origin to the insertion of the tendon being substituted. Although not always possible, this configuration is desirable.
One tendon, one function
A single tendon cannot be expected to simultaneously perform diametrically opposing actions, eg, flex and extend the same joint. If a muscle is inserted into two tendons with separate functions, the force of amplitude of the donor tendon is dissipated and less effective than that of a muscle motored by a single tendon.
Synergism
The use of synergistic muscles, eg, finger flexors acting in concert with wrist extensors and finger extensors with wrist flexors, has been advocated for transfer. Muscle function is easier to retain after synergistic muscle transfer.
Expendable donor
The removal of a tendon for transfer must not result in an unacceptable loss of function. Sufficient muscle must remain to substitute for the donor muscle.
Timing of tendon transfer
No transfer should be performed until the local tissues are in optimal condition. The term often used to describe this is tissue equilibrium. Tissue is in equilibrium when soft-tissue induration has resolved, when any reaction in the wound is absent, when joints are supple, and when the scars are as soft as they are likely to become.
Tendon transfers function best when passed between subcutaneous fat and the deep fascial layer; they are not likely to be functional if placed in the pathway of a scar.
Tendon transfer for foot drop
Foot drop is an inability to lift the forefoot due to the weakness of dorsiflexors of the foot 2. This, in turn, can lead to an unsafe antalgic gait, potentially resulting in falls.
Foot drop is a deceptively simple name for a potentially complex problem. It can be defined as a significant weakness of ankle and toe dorsiflexion. The foot and ankle dorsiflexors include the tibialis anterior, the extensor hallucis longus (EHL), and the extensor digitorum longus (EDL). These muscles help the body clear the foot during swing phase and control plantarflexion of the foot on heel strike. Weakness in this group of muscles results in an equinovarus deformity. This is sometimes referred to as steppage gait, because the patient tends to walk with an exaggerated flexion of the hip and knee to prevent the toes from catching on the ground during swing phase. During gait, the force of heel strike exceeds body weight, and the direction of the ground reaction vector passes behind the ankle and knee center.
This causes the foot to plantarflex and, if uncontrolled, to slap the ground. Ordinarily, eccentric lengthening of the tibialis anterior, which controls plantar flexion, absorbs the shock of heel strike. Foot drop can result if there is injury to the dorsiflexors or to any point along the neural pathways that supply them.
The causes of foot drop may be divided into three general categories: neurologic, muscular, and anatomic. These causes may overlap. The causes behind foot drop are varied and include muscular including dorsiflexor injuries, neurologic such as peripheral nerve injuries, stroke, neuropathies, drug toxicities, or diabetes, spinal, autoimmune and musculoskeletal disorders.
Among the neurological factors, common peroneal nerve neuropathy (of idiopathic etiology), diabetic neuropathy, compression at the level of the neck of the fibula, lumbar disc prolapse, and nerve injury form the bulk of neurologic causes 3. In leprosy, the nerve gets compressed at the site where it winds around the fibular neck. At this place the nerve is also susceptible to injury as it lies comparatively superficially. Tumors of the nerve or fibula, cerebral palsy, poliomyelitis, multiple sclerosis, Charcot–Marie–Tooth disease, stroke, and spinal cord lesions are some of the other causes. Muscle injury, rupture of the tibialis anterior tendon, compartment syndrome, muscular dystrophy, and amyotrophic lateral sclerosis are some of the muscular causes. In a multi centric study done in Italy, the cause and predisposing factors of common peroneal nerve mono-neuropathy were studied. It was found that in 16% of patients, the cause of peroneal mono-neuropathy was idiopathic, 20.3% patients had developed neuropathy after surgery around the knee and trauma was the cause in 11.6% patients, surprisingly weight loss contributed to peroneal mono-neuropathy in 14.5% in their series 4.
Treatment is variable and is directed at the specific cause.
A thorough understanding of the underlying pathophysiology is necessary before designing a treatment plan.
In trauma cases, for nerve transection, nerve reconstruction should take place within 72 hours of injury. Primary nerve repair techniques, autologous nerve graft are usually performed.
For complete nerve compression, necrolysis and nerve decompression should be performed. Return to function has been reported in about 97% 5. A surgical release may be necessary for patients with equinus deformity.
In cases of significant nerve dysfunction, nerve or tendon transfers may be required 6.
For the other causes, treatment is initially conservative because there may be a chance of partial or complete resolution of symptoms spontaneously overtime.
Tendon transfer procedure requires very specific patient selection in the subgroup with persistent traumatic peroneal nerve palsy 7. The common peroneal nerve lesion must be at or distal to the branching from the tibial nerve (to guarantee that intact motor fibers proximal to the lesion are available for transposition). Paralysis must be permanent.
Specifically, there must be no recovery of function for at least 18 months after injury or after the most recent attempt at exploration or repair. Electrodiagnostic changes indicative of permanent damage must be present. Also, there must be good passive range of motion, with at least 90° of dorsiflexion. The muscles innervated by the tibial nerve must be normal. Finally, soft-tissue coverage must be adequate.
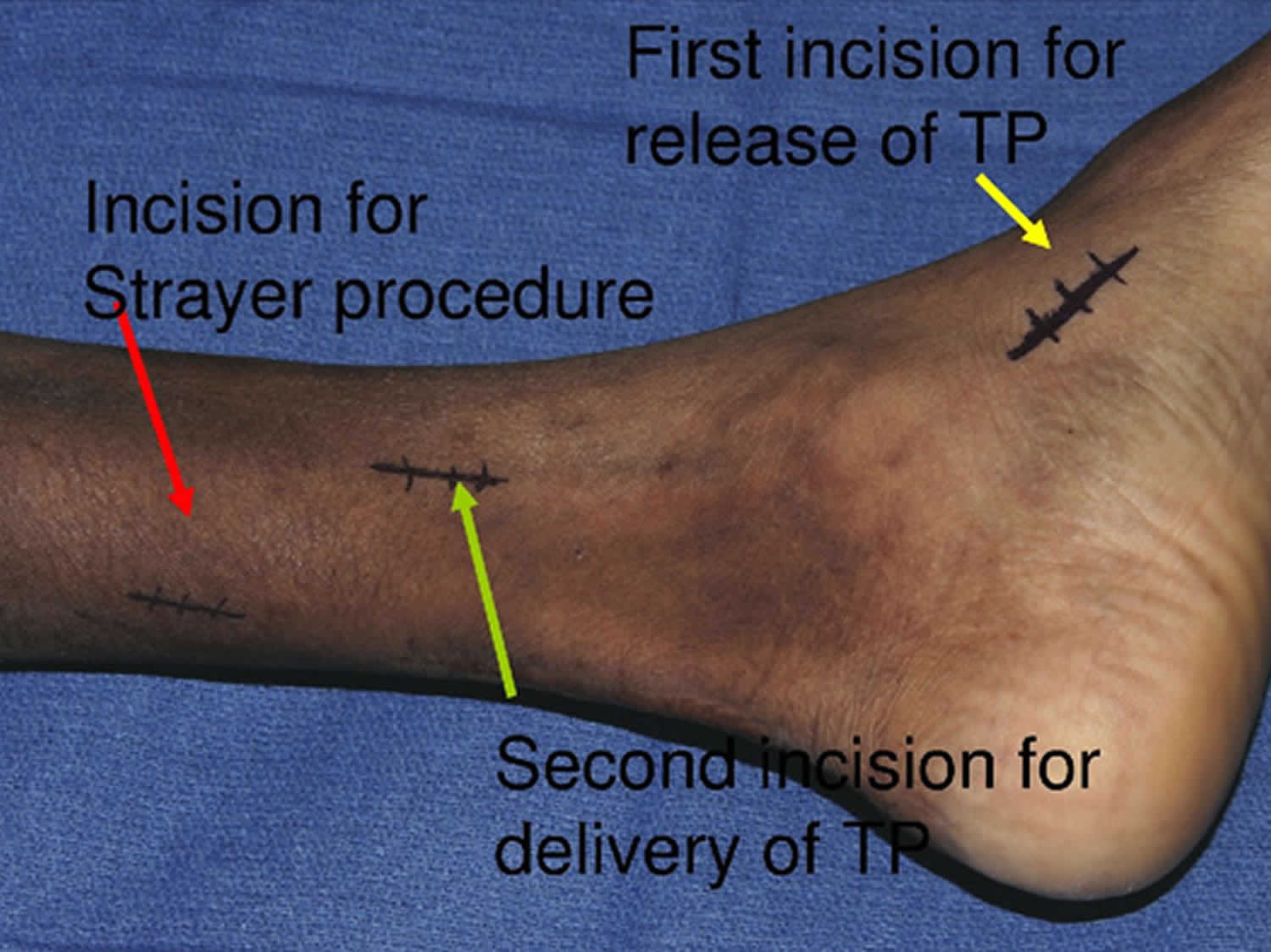
A common method of tendon transfer moves the posterior tibial tendon (PTT), with or without complementary lengthening of the Achilles tendon. This procedure is accomplished via an open Z-lengthening of the Achilles tendon to allow a minimum of 15° of passive dorsiflexion.
The route by which the posterior tibial tendon is transferred may be either through the intraosseous membrane or circumtibial. One series that included patients with leprosy concluded that the circumtibial route had an unacceptably high rate of recurrent inversion, leading to ulceration of the lateral border of the foot 8. Other series have found either method to be acceptable, but a 2009 study argued that the interosseous membrane route is preferred in this patient population 9.
The circumtibial route is technically easier, but it may be less appealing cosmetically. The intraosseous membrane route can be prone to adhesions if the window in the membrane is too narrow. In addition to discouraging adhesions, a generous window produces a straight line of pull of the posterior tibial muscle-tendon unit from its origin to its new insertion on the dorsum of the foot.
Once a transfer route is selected, the point of fixation of the split posterior tibial tendon may be either tendon-to-tendon or tendon-to-bone. In tendon-to-tendon fixation, the points of attachment are as follows:
- Lateral slip – Peroneus brevis, peroneus tertius, or extensor digitorum longus (EDL) tendons
- Medial slip – Tibialis anterior or extensor hallucis longus (EHL)
In tendon-to-bone fixation, an osseous tunnel in the tarsal or metatarsal bones serves as the point of attachment. One study cited a report of a consequent neuropathic arthropathy of the tarsal joints.
A popular approach to tendon-to-bone attachment is the Bridle procedure, a modification of the Riordan technique described by Rodriguez 10. The Bridle procedure involves insertion of the posterior tibial tendon into the second cuneiform bone, combined with anastomosis of the posterior tibial tendon transfer to the anterior tibial tendon (ATT) and a rerouted peroneus longus tendon in front of the lateral malleolus to balance the foot in dorsiflexion.
The Bridle procedure makes use of five incisions (see Figure 2 below). The posterior tibial tendon insertion is secured through incision 1 on the medial foot. Incision 2 is used to retrieve the end of the posterior tibial tendon proximal to the tarsal canal into the posterior compartment of the leg.
Incision 3, on the anterior leg proximal to the ankle, provides wide exposure of the interosseous membrane. The posterior tibial tendon is pulled through the interosseous membrane and a longitudinally split anterior tibial tendon, then into the anterior compartment between the tibia and the anterior tibial tendon. The posterior tibial tendon is anastomosed to the anterior tibial tendon with the foot in full dorsiflexion.
Incision 4, posterior to the lateral malleolus, accesses the peroneus longus and brevis tendons proximal to the lateral retinaculum. The peroneus longus is transected about 5 cm proximal to the tip of the lateral malleolus. The distal transected end of the peroneus longus is retrieved into the foot distal to the superior and inferior peroneal retinaculum, then transposed via a direct subcutaneous tunnel that is anterior to the lateral malleolus. The proximal end of the transected peroneus longus is anastomosed to the peroneus brevis tendon.
Incision 5 accesses the distal stump of the posterior tibial tendon as it is brought to the dorsum of the foot via a subcutaneous tunnel. Here, the tendon is secured to the second cuneiform bone while full dorsiflexion of the foot is maintained. Ideally, if the tendon has sufficient length, it should be anastomosed to itself through a tunnel in the second cuneiform bone. If this is not feasible, the tendon may be secured to the bone with sutures or tunneled through and secured with a button.
Figure 2. Bridle procedure
Figure 3. Posterior tibial tendon transfer
Footnote: Posterior tibial tendon (C) is pulled through slit in anterior tibial tendon (A) and inserted into second cuneiform. Posterior tibial tendon is anastomosed to anterior tibial tendon and distal stump of peroneus longus (B) that has been rerouted anterior to lateral malleolus.
In a study comparing 19 patients with foot drop who underwent the Bridle procedure with 10 matched control subjects, Johnson et al found that although the procedure did not restore foot and ankle strength and balance to normal, it was successful in that patients with a functional posterior tibial muscle had significantly better outcomes and were able to discontinue using an Ankle-Foot Orthosis (AFO) 11. All of the Bridle-procedure patients had good-to-excellent outcomes and stated that they would undergo the operation again.
Werner et al 12, in a study of 10 patients with peroneal nerve injury resulting from multiligament instability, evaluated nonoperative treatment (n=5) against posterior tibial tendon transfer (n=5); there was also a control group (n=4) who did not have peroneal nerve injury. Compared with the nonoperative group, the posterior tibial tendon-transfer group showed increased dorsiflexion at initial contact and at mid-late swing phase. Compared with the control group, the posterior tibial tendon-transfer group had similar gait patterns but tended to be more everted. Overall, gait analysis demonstrated significantly improved sagittal-plane ankle kinematics with posterior tibial tendon transfer, with some degree of subtle instability as the tradeoff.
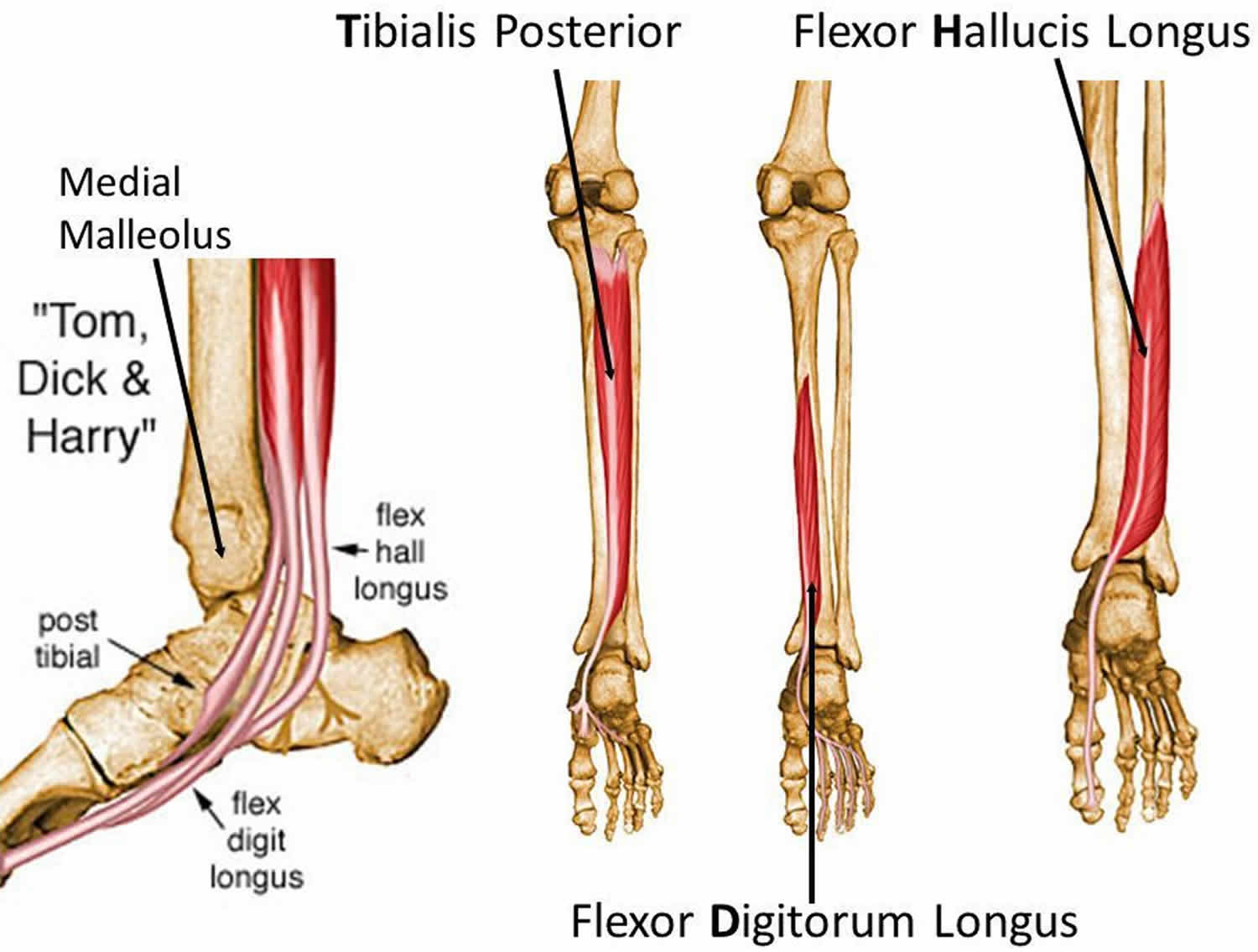
A series of hemiplegic patients demonstrated favorable results when anterior transfer of the long-toe flexors (flexor hallucis longus [FHL] or flexor digitorum longus [FDL]) was combined with Achilles-tendon lengthening. The flexor was transferred intraosseously to the fourth metatarsal. If the foot drop was accompanied by a marked varus deformity, lengthening of the posterior tibial tendon was also performed. Short-toe flexors were released if the patient had severe hammertoes.
Another method of reconstruction involving the coaptation of the extensor hallucis longus (EHL) to the tibialis anterior was investigated in eight patients who had had polio. At final review, only two of the patients maintained efficient dorsiflexion. These poor results were thought to be due to stretching of the coaptation.
During neurotendinous transposition, the lateral head of the gastrocnemius is transposed to the tendons of the anterior muscle group simultaneously with transposition of the proximal end of the deep peroneal nerve. The nerve is sutured to the motor nerve of the lateral head of the gastrocnemius, restoring active voluntary foot dorsiflexion and automatic walking. By avoiding use of an antagonist muscle to the paralytic group of muscles, this transfer avoids retraining to achieve dorsiflexion, providing physiologic muscle balance and fully automatic walking.
Mohavedi Yeganeh et al 13 described the use of a triple tendon transfer (involving the posterior tibial tendon, the FHL tendon, and the FDL tendon) to correct toe drop associated with common peroneal nerve palsy, which is not addressed by anterior posterior tibial tendon transfer alone. Excellent postoperative results for foot drop correction were achieved in nine cases (60%), good results in five (33%), and moderate results in one (7%). Excellent postoperative extension of the toes was achieved in seven cases (47%), good extension in five (33%), and moderate extension in three (20%).
Cho et al 14 reported on 17 patients who underwent posterior tibial tendon transfer for foot drop secondary to peroneal nerve palsy (follow-up, ≥3 years). Mean American Orthopaedic Foot & Ankle Society (AOFAS) score, Foot and Ankle Outcome Score (FAOS), and Foot and Ankle Ability Measure (FAAM) improved significantly at final follow-up: from 65.1 to 86.2, from 55.6 to 87.8, and from 45.7 to 84.4, respectively. However, all functional evaluation scores were significantly lower than in the control group. Mean peak torque was 7.1 Nm for ankle dorsiflexors, 39.2 Nm for plantarflexors, 9.8 Nm for invertors, and 7.3 Nm for evertors at final follow-up. These values were significantly lower than corresponding values in the control group.
No significant differences in radiographic measurements were found, and no patients presented with a postoperative flatfoot deformity 14. One patient (5.9%) needed an AFO (ankle-foot orthosis) for occupational activity. Cho et al 14 concluded that although restoration of dorsiflexion strength postoperatively was about 33% of the normal ankle, function in daily activities and gait ability were satisfactorily improved. In addition, posterior tibial tendon transfer demonstrated no definitive radiographic or clinical progression to postoperative flatfoot deformity at intermediate-term follow-up.
After a tendon transfer procedure, the patient is placed in a cast and restricted to nonweightbearing ambulation for 6 weeks. Subsequently, the patient receives physical therapy for gait training.
With a tendon transfer, retraining of the transferred tendon and stretching exercises for the Achilles tendon are advocated. Retraining may be avoided with a neurotendinous transposition of the gastrocnemius and the proximal end of the deep peroneal nerve.
Tendon transfer surgery risks
All surgery has some risk, although those risks may be small. All surgeries produce a surgical scar. Surgical incisions may develop infection. All surgeries require the use of anesthesia, and will require a complete history and physical examination by your primary care physician to determine if you have medical risks associated with anesthesia. Evaluation by the anesthesiologist will help outline your risks and options.
When a tendon is transferred and sewn into another position, the tendon transfer will need a period of time to heal, usually about one to two months. A splint or cast may be used, followed by therapy to teach you the new tendon function. Finally, exercises will be needed to strengthen the muscle after your hand surgeon feels the tendon transfer has sufficiently healed. You will need to follow post-operative instructions. Movement too early can lead to rupture of the tendon transfer. Movement too late can lead to excessive scarring of the tendon with resultant stiffness. Discussion of your individual case with your surgeon will help you further understand the risks and benefits associated with tendon transfer surgery.
References- Wilbur D, Hammert WC. Principles of Tendon Transfer. Hand Clin. 2016 Aug. 32 (3):283-9.
- Nori SL, Stretanski MF. Foot Drop. [Updated 2020 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554393
- Krishnamurthy S, Ibrahim M. Tendon Transfers in Foot Drop. Indian J Plast Surg. 2019;52(1):100-108. doi:10.1055/s-0039-1688105 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6664842
- Aprile I, Caliandro P, La Torre G. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005;10(03):259–268.
- Matejcik V, Penzesova G. Surgery of the peripheral nerves. Bratisl Lek Listy. 2006;107(3):89-92.
- Carolus AE, Becker M, Cuny J, Smektala R, Schmieder K, Brenke C. The Interdisciplinary Management of Foot Drop. Dtsch Arztebl Int. 2019 May 17;116(20):347-354.
- Foot Drop Treatment & Management. https://emedicine.medscape.com/article/1234607-treatment#d14
- Soares D. Tibialis posterior transfer for the correction of foot drop in leprosy. Long-term outcome. J Bone Joint Surg Br. 1996 Jan. 78 (1):61-2.
- Shah RK. Tibialis posterior transfer by interosseous route for the correction of foot drop in leprosy. Int Orthop. 2009 Dec. 33 (6):1637-40.
- Rodriguez RP. The Bridle procedure in the treatment of paralysis of the foot. Foot Ankle. 1992 Feb. 13 (2):63-9.
- Johnson JE, Paxton ES, Lippe J, Bohnert KL, Sinacore DR, Hastings MK, et al. Outcomes of the Bridle Procedure for the Treatment of Foot Drop. Foot Ankle Int. 2015 Nov. 36 (11):1287-96.
- Werner BC, Norte GE, Hadeed MM, Park JS, Miller MD, Hart JM. Peroneal Nerve Dysfunction due to Multiligament Knee Injury: Patient Characteristics and Comparative Outcomes After Posterior Tibial Tendon Transfer. Clin J Sport Med. 2017 Jan. 27 (1):10-19.
- Movahedi Yeganeh M. Triple Tendon Transfer for Correction of Foot Deformity in Common Peroneal Nerve Palsy. Foot Ankle Int. 2016 Jun. 37 (6):665-9.
- Cho BK, Park KJ, Choi SM, Im SH, SooHoo NF. Functional Outcomes Following Anterior Transfer of the Tibialis Posterior Tendon for Foot Drop Secondary to Peroneal Nerve Palsy. Foot Ankle Int. 2017 Jun. 38 (6):627-633.