What is testicular torsion
Testicular torsion occurs when a testicle rotates, twisting the spermatic cord and its contents that brings blood to the testicle. The reduced blood flow causes sudden and often severe pain and swelling. Testicular torsion is a surgical emergency most commonly affecting 3.8 per 100,000 males younger than 18 years (between ages 12 and 18) annually, but it can occur at any age, even before birth 1. Testicular torsion accounts for 10% to 15% of acute scrotal disease in children, and results in an orchidectomy (surgical removal of testicle) rate of 42% in boys undergoing surgery for testicular torsion. Prompt recognition and treatment are necessary for testicular salvage, and testicular torsion must be excluded in all patients who present with acute testicular pain.
Testicular torsion is a clinical diagnosis, and patients typically present with severe acute one-sided testicular pain, nausea, and vomiting 2. Physical examination may reveal a high-riding testicle with an absent cremasteric reflex. If history and physical examination suggest testicular torsion, immediate surgical exploration is indicated and should not be postponed to perform imaging studies. There is typically a four- to eight-hour window before permanent ischemic damage occurs. Delay in testicular torsion treatment may be associated with decreased fertility, or may necessitate orchiectomy (surgical removal of testicle).
Testicular torsion usually requires emergency surgery. If treated quickly, the testicle can usually be saved. But when blood flow has been cut off for too long, a testicle might become so badly damaged that it has to be removed.
The viability of the testicle in cases of torsion is difficult to predict; hence, emergent surgical treatment is indicated despite many patients presenting beyond the four- to eight-hour time frame 3. Reported testicular salvage rates are 90% to 100% if surgical exploration is performed within six hours of symptom onset, decrease to 50% if symptoms are present for more than 12 hours, and are typically less than 10% if symptom duration is 24 hours or more 4. These percentages should be considered approximate rather than absolute for the purpose of counseling patients or making clinical decisions.
Seek emergency care for sudden or severe testicle pain. Prompt treatment can prevent severe damage or loss of your testicle if you have testicular torsion.
You also need to seek prompt medical help if you’ve had sudden testicle pain that goes away without treatment. This can occur when a testicle twists and then untwists on its own (intermittent torsion and detorsion). Surgery is frequently needed to prevent the problem from happening again.
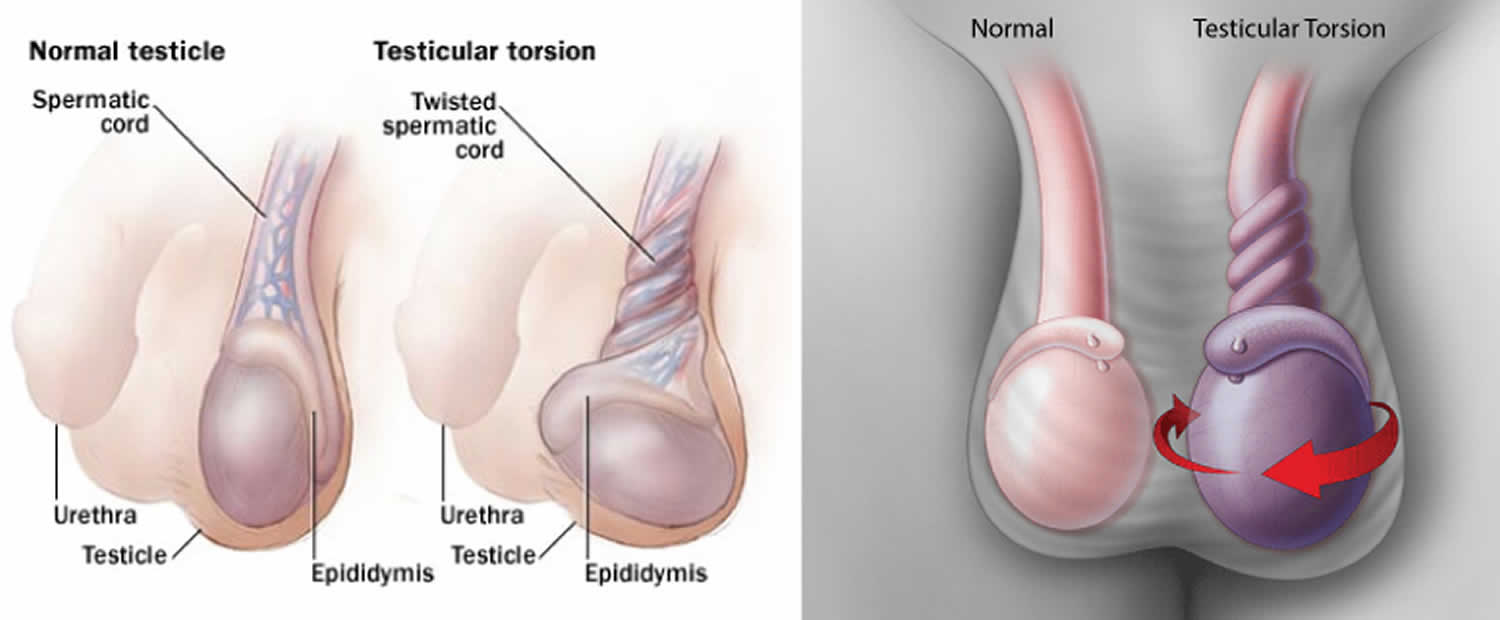
Figure 1. Testicles and scrotum anatomy
Figure 2. Testicle anatomy
Figure 4. Bell-Clapper deformity with abnormal fixation of the tunica vaginalis to the testicle
[Source 2 ]What causes testicular torsion
Testicular torsion occurs when the testicle rotates on the spermatic cord, which brings blood to the testicle from the abdomen. If the testicle rotates several times, blood flow to it can be entirely blocked, causing damage more quickly.
It’s not clear why testicular torsion occurs. Most males who get testicular torsion have an inherited trait that allows the testicle to rotate freely inside the scrotum. This inherited condition often affects both testicles. But not every male with the trait will have testicular torsion.
Testicular torsion often occurs several hours after vigorous activity, after a minor injury to the testicles or while sleeping. Cold temperature or rapid growth of the testicle during puberty also might play a role.
The testes develop from condensations of tissue within the urogenital ridge at approximately six weeks of gestation. With longitudinal growth of the embryo, and through endocrine and paracrine signals, which have not yet been well described, the testes ultimately descend into the scrotum by the third trimester of pregnancy. As the testes leave the abdomen, the peritoneal lining covers them, creating the processus vaginalis. The spermatic arteries and pampiniform venous plexus enter the inguinal canal proximal to the testes, and with the vas deferens, form the spermatic cord 5. The testicle is tethered to the scrotum distally by the gubernaculum.
Testicular torsion may be intravaginal or extravaginal 6. Intravaginal torsion occurs when the testicle can freely rotate within the tunica vaginalis; this can be due to a congenital anomaly called the Bell-Clapper deformity. This deformity is due to failure of posterior anchorage of the gubernaculum, epididymis, and testis, thus allowing the testis to freely rotate within the tunica vaginalis, ultimately pinching off arterial blood supply to the testicle leading to ischemia and infarction. Extravaginal torsion is seen almost exclusively in neonates, occurs when the testis rotates within the scrotum owing to inadequate fusion of the testicle to the scrotal wall via the tunica vaginalis or increased mobility of the testicle before the descent into the scrotum 7. The torsion follows rotation of the spermatic cord and results in ischemia. The degree of testicular torsion is directly correlated with the possibility of salvage after torsion and time to necrosis. The degree of torsion may be variable, usually causing venous occlusion and congestion first. Most cases of spermatic cord torsion leading to infarction are twisted at least 720 degrees. Torsion of the testicular appendages, often presenting in 7- to 13-year-old children, presents similarly to testicular torsion and accounts for 24% to 46% of acute scrotal presentations 8.
Risk factors for testicular torsion
- Age. Testicular torsion is most common between ages 12 and 18.
- Previous testicular torsion. If you’ve had testicular pain that went away without treatment (intermittent torsion and detorsion), it’s likely to occur again.
- The more frequent the bouts of pain, the higher the risk of testicular damage.
- Family history of testicular torsion. The condition can run in families.
Who’s at risk of testicular torsion
The age distribution of testicular torsion is bimodal, with one peak in the neonatal period and the second peak around puberty. In neonates, extravaginal torsion predominates, with the entire cord, including the processus vaginalis, twisting 9. Extravaginal torsion may occur antenatally or in the early postnatal period and typically presents as painless scrotal swelling, with or without acute inflammation. Testicular viability in neonatal torsion is universally poor; one literature review of 18 case series with 284 patients found a salvage rate of about 9% 10. Contralateral orchiopexy has been recommended at the time of surgical exploration because the etiology for extravaginal torsion remains unclear.12 Although no specific risk factors have been identified, poorer fixation of the neonatal tissues to one another has been implicated, and term infants with difficult or prolonged deliveries may be at higher risk 9.
In older children and adults, testicular torsion is usually intravaginal (twisting of the cord within the tunica vaginalis) 11. The Bell-clapper Deformity (Figure 4), in which there is abnormal fixation of the tunica vaginalis to the testicle, results in increased mobility of the testicle within the tunica vaginalis 12. Whether testicular torsion is intravaginal or extravaginal, twisting of the spermatic cord initially increases venous pressure and congestion, with subsequent decrease in arterial blood flow and ischemia 13. Although symptoms are typically unilateral, the anatomic conditions that predispose a persion to torsion must be presumed to be bilateral 12.
Testicular torsion prevention
Having testicles that can rotate in the scrotum is a trait inherited by some males. If you have this trait, the only way to prevent testicular torsion is surgery to attach both testicles to the inside of the scrotum.
Testicular torsion signs and symptoms
The classic presentation of testicular torsion is sudden onset of severe unilateral testicular pain associated with nausea and vomiting 14. Patients may also have nonspecific symptoms such as fever or urinary problems. Although there are no clear precipitating factors, many patients describe a recent history of trauma or strenuous physical activity 15. The ipsilateral scrotal skin may be indurated, erythematous, and warm, although changes in the overlying skin reflect the degree of inflammation and may change over time 16. A high-riding testicle can indicate a twisted, foreshortened spermatic cord 17.
The affected testicle can also have an abnormal horizontal orientation. The cremasteric reflex, which is elicited by pinching the medial thigh, causes elevation of the testicle. Presence of the reflex suggests, but does not confirm, the absence of testicular torsion 16. Comparison of the affected and unaffected sides may help delineate abnormal clinical findings, although scrotal edema and patient discomfort may limit physical examination 18. Patients in whom the components of the spermatic cord can be distinctly appreciated, whose testes are normally oriented, who have minimal to no scrotal edema, and who have no systemic symptoms (particularly with examination) are unlikely to have acute testicular torsion 16.
In cases of intermittent torsion, patients typically report recurrent episodes of acute unilateral scrotal pain 14. The pain usually resolves spontaneously within a few hours. Clinical examination and imaging are often normal if the patient presents after resolution of torsion. Chronic intermittent torsion may result in segmental ischemia of the testicle and warrants urologic evaluation 19.
Signs and symptoms of testicular torsion include:
- Sudden, severe pain in the scrotum — the loose bag of skin under your penis that contains the testicles
- Swelling of the scrotum
- Abdominal pain
- Nausea and vomiting
- A testicle that’s positioned higher than normal or at an unusual angle
- Frequent urination
- Fever
Young boys who have testicular torsion typically wake up due to scrotal pain in the middle of the night or early in the morning.
The appendix testis and appendix epididymis are embryologic remnants of the Müllerian and Wolffian systems, respectively. These vestigial structures may twist, with subsequent infarction. Clinically, torsion of an appendix can be difficult to differentiate from torsion of the spermatic cord in the patient with acute scrotal pain; the onset of pain may be similarly abrupt, and systemic symptoms (although less common) may be present 20. The classic presentation of a torsed appendage is the blue dot sign, where the inflamed and ischemic appendage can be visualized through the scrotal skin 21; overlying scrotal edema and patient complexion may limit this finding, thus decreasing the sensitivity 22.
When patients with appendiceal torsion present early, focal tenderness at the superior pole of the epididymis, near the torsed appendage, is often appreciated. As local inflammation occurs, the development of local edema may make the diagnosis more challenging. In a series of 119 males with acute scrotum, more than one-half had torsion of a testicular appendage, whereas approximately one-third had testicular torsion 23.
Patients with normal examination results, but with significant tenderness along the epididymis or testicle, may have epididymoorchitis 24. Epididymitis is rare in prepubertal children, except in the presence of abnormal genitourinary anatomy or recent viral infection 25. In older patients, particularly those who are sexually active or who have recently undergone a procedure, bacteria from the bladder or urethra can infect the epididymis or testicle 24. History and physical examination, as well as urinalysis, are helpful in confirming or excluding this diagnosis 24.
Testicular torsion complications
Testicular torsion can cause the following complications:
- Damage to or death of the testicle. When testicular torsion is not treated for several hours, blocked blood flow can cause permanent damage to the testicle. If the testicle is badly damaged, it has to be surgically removed.
- Inability to father children. In some cases, damage or loss of a testicle affects a man’s ability to father children.
Testicular torsion diagnosis
Your doctor will ask you questions to verify whether your signs and symptoms are caused by testicular torsion or something else. Doctors often diagnose testicular torsion with a physical exam of the scrotum, testicles, abdomen and groin.
Your doctor might also test your reflexes by lightly rubbing or pinching the inside of your thigh on the affected side. Normally, this causes the testicle to contract. This reflex might not occur if you have testicular torsion.
Sometimes medical tests are necessary to confirm a diagnosis or to help identify another cause for your symptoms. For example:
- Urine test. This test is used to check for infection.
- Scrotal ultrasound. This type of ultrasound is used to check blood flow. Decreased blood flow to the testicle is a sign of testicular torsion. But ultrasound doesn’t always detect the reduced blood flow, so the test might not rule out testicular torsion.
- Surgery. Surgery might be necessary to determine whether your symptoms are caused by testicular torsion or another condition.
If you’ve had pain for several hours and your physical exam suggests testicular torsion, you might be taken directly to surgery without any additional testing. Delaying surgery might result in loss of the testicle.
Testicular torsion treatment
Manual detorsion should be attempted if surgery is not an immediate option or while preparations for surgical exploration are being made, but should not supersede or delay surgical intervention 26. Manual detorsion should not replace surgical exploration 4. The testes are typically detorsed from the medial to lateral side, turning the physician’s hands as if “opening a book” 27. Analgesic administration, intravenous sedation, or a spermatic cord block may facilitate detorsion by relaxing cremasteric fibers and controlling pain enough to allow manipulation of the testicle for detorsion. The testicle is typically twisted more than 360 degrees, so more than one rotation may be required to completely detorse the testicle 27. The subjective end point is alleviation of pain, although analgesic administration may limit the utility of this measure. Return of blood flow to the testicle on Doppler ultrasonography serves as an objective end point and should always be documented; however, relative hyperemia and altered vascular flow patterns in a newly revascularized testicle may obscure ultrasound results 4.
Testicular torsion surgery
Surgery is required to correct testicular torsion. In some instances, the doctor might be able to untwist the testicle by pushing on the scrotum (manual detorsion). But you’ll still need surgery to prevent torsion from occurring again.
Surgery for testicular torsion is usually done under general anesthesia. A transscrotal surgical approach is typically used to deliver the affected testicle into the operative field 28. Detorsion of the affected spermatic cord is performed until no twists are visible, and testicular viability has been assessed and stitch one or both testicles to the inside of the scrotum.
The sooner the testicle is untwisted, the greater the chance it can be saved. After six hours from the start of pain, the chances of needing testicle removal are greatly increased. If treatment is delayed more than 12 hours from the start of pain, there is at least a 75 percent chance of needing testicle removal.
Orchiectomy is performed if the affected testicle appears grossly necrotic or nonviable. Orchiectomy rates vary widely in the literature, typically ranging from 39% to 71% in most series 29. Age and prolonged time to definitive treatment have been identified as risk factors for orchiectomy 30. The rate of testicular loss can approach 100% in cases where the diagnosis is missed, emphasizing the necessity of maintaining a high index of suspicion for torsion in males presenting with scrotal pain 30. If the affected testicle is deemed viable, orchiopexy with permanent suture should be performed to permanently fix the testicle within the scrotum 31.
Contralateral orchiopexy should be performed regardless of the viability of the affected testicle 32. The bell-clapper deformity that increases testicular mobility and, therefore, the risk of torsion, is bilateral in up to 80% of patients 12. It is assumed to be present contralaterally in all patients with testicular torsion 33.
Testicular torsion in newborns and infants
Testicular torsion can occur in newborns and infants, though it’s rare. The infant’s testicle might be hard, swollen or a darker color. Ultrasound might not detect reduced blood flow to the infant’s scrotum, so surgery might be needed to confirm testicular torsion.
Treatment for testicular torsion in infants is controversial. If a boy is born with signs and symptoms of testicular torsion, it might be too late for emergency surgery to help and there are risks associated with general anesthesia. But emergency surgery can sometimes save all or part of the testicle and can prevent torsion in the other testicle. Treating testicular torsion in infants might prevent future problems with male hormone production and fertility.
References- Zhao LC, Lautz TB, Meeks JJ, Maizels M. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol. 2011;186(5):2009–2013
- Testicular Torsion: Diagnosis, Evaluation, and Management. Am Fam Physician. 2013 Dec 15;88(12):835-840. https://www.aafp.org/afp/2013/1215/p835.html
- Gatti JM, Patrick Murphy J. Current management of the acute scrotum. Semin Pediatr Surg. 2007;16(1):58–63.
- Kapoor S. Testicular torsion: a race against time. Int J Clin Pract. 2008;62(5):821–827.
- Barteczko KJ, Jacob MI. The testicular descent in human. Origin, development and fate of the gubernaculum Hunteri, processus vaginalis peritonei, and gonadal ligaments. Adv Anat Embryol Cell Biol. 2000;156:III–X, 1–98.
- Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol. 2015;56(1):3-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4294852/
- Dogra V, Bhatt S. Acute painful scrotum. Radiol Clin North Am. 2004;42:349–363.
- Marcozzi D, Suner S. The nontraumatic, acute scrotum. Emerg Med Clin North Am. 2001;19:547–568.
- Callewaert PR, Van Kerrebroeck P. New insights into perinatal testicular torsion. Eur J Pediatr. 2010;169(6):705–712.
- Nandi B, Murphy FL. Neonatal testicular torsion: a systematic literature review. Pediatr Surg Int. 2011;27(10):1037–1040.
- Witherington R, Jarrell TS. Torsion of the spermatic cord in adults. J Urol. 1990;143(1):62–63.
- Favorito LA, Cavalcante AG, Costa WS. Anatomic aspects of epididymis and tunica vaginalis in patients with testicular torsion. Int Braz J Urol. 2004;30(5):420–424.
- Nguyen L, Lievano G, Ghosh L, Radhakrishnan J, Fornell L, John E. Effect of unilateral testicular torsion on blood flow and histology of contralateral testes. J Pediatr Surg. 1999;34(5):680–683.
- Davis JE, Silverman M. Scrotal emergencies. Emerg Med Clin North Am. 2011;29(3):469–484.
- Ciftci AO, Senocak ME, Tanyel FC, Büyükpamukçu N. Clinical predictors for differential diagnosis of acute scrotum. Eur J Pediatr Surg. 2004;14(5):333–338.
- Srinivasan A, Cinman N, Feber KM, Gitlin J, Palmer LS. History and physical examination findings predictive of testicular torsion: an attempt to promote clinical diagnosis by house staff. J Pediatr Urol. 2011;7(4):470–474.
- Canning DA, Lambert SM. Evaluation of the pediatric urology patient. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology, 10th ed. Philadelphia, Pa.: Elsevier Saunders; 2012:3067–3084.
- Watkin NA, Reiger NA, Moisey CU. Is the conservative management of the acute scrotum justified on clinical grounds? Br J Urol. 1996;78(4):623–627.
- White WM, Brewer ME, Kim ED. Segmental ischemia of testis secondary to intermittent testicular torsion. Urology. 2006;68(3):670–671.
- Rakha E, Puls F, Saidul I, Furness P. Torsion of the testicular appendix: importance of associated acute inflammation. J Clin Pathol. 2006;59(8):831–834.
- Rabinowitz R, Hulbert WC Jr. Acute scrotal swelling. Urol Clin North Am. 1995;22(1):101–105.
- Davenport M. ABC of general surgery in children. Acute problems of the scrotum. BMJ. 1996;312(7028):435–437.
- Tajchner L, Larkin JO, Bourke MG, Waldron R, Barry K, Eustace PW. Management of the acute scrotum in a district general hospital: 10-year experience. Scientific World Journal. 2009;9:281–286.
- Graumann LA, Dietz HG, Stehr M. Urinalysis in children with epididymitis. Eur J Pediatr Surg. 2010;20(4):247–249.
- Somekh E, Gorenstein A, Serour F. Acute epididymitis in boys: evidence of a post-infectious etiology. J Urol. 2004;171(1):391–394.
- Bomann JS, Moore C. Bedside ultrasound of a painful testicle: before and after manual detorsion by an emergency physician. Acad Emerg Med. 2009;16(4):366.
- Sessions AE, Rabinowitz R, Hulbert WC, Goldstein MM, Mevorach RA. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003;169(2):663–665.
- Corbett HJ, Simpson ET. Management of the acute scrotum in children. ANZ J Surg. 2002;72(3):226–228.
- Yang C Jr, Song B, Liu X, Wei GH, Lin T, He DW. Acute scrotum in children: an 18-year retrospective study. Pediatr Emerg Care. 2011;27(4):270–274.
- Bayne AP, Madden-Fuentes RJ, Jones EA, et al. Factors associated with delayed treatment of acute testicular torsion-do demographics or inter-hospital transfer matter? J Urol. 2010;184(4 suppl):1743–1747.
- Taskinen S, Taskinen M, Rintala R. Testicular torsion: orchiectomy or orchiopexy? J Pediatr Urol. 2008;4(3):210–213.
- Bolin C, Driver CP, Youngson GG. Operative management of testicular torsion: current practice within the UK and Ireland. J Pediatr Urol. 2006;2(3):190–193.
- Ringdahl E, Teague L. Testicular torsion. Am Fam Physician. 2006;74(10):1739–1743.