What is transient lingual papillitis
Transient lingual papillitis is a common painful inflammatory condition affecting one or several fungiform papillae on the top and sides of the tongue 1. Transient lingual papillitis is also known as “lie bumps” or “liar’s bumps” 2 . The term “transient lingual papillitis” was introduced by Whitaker et al. 3 in 1996 to describe the inflammatory hyperplasia of one to several fungiform lingual papillae that has an acute onset, is painful and transient in nature. Similar lesions were, also, reported as “lingual fungiform papillae hypertrophy” 4 and “fungiform papillary glossitis” 5 and “photocopier’s papillitis” 6. “Eruptive lingual papillitis”, “eruptive familial lingual papillitis” and “eruptive lingual papillitis with household transmission” may be included in the spectrum of transient lingual papillitis 7.
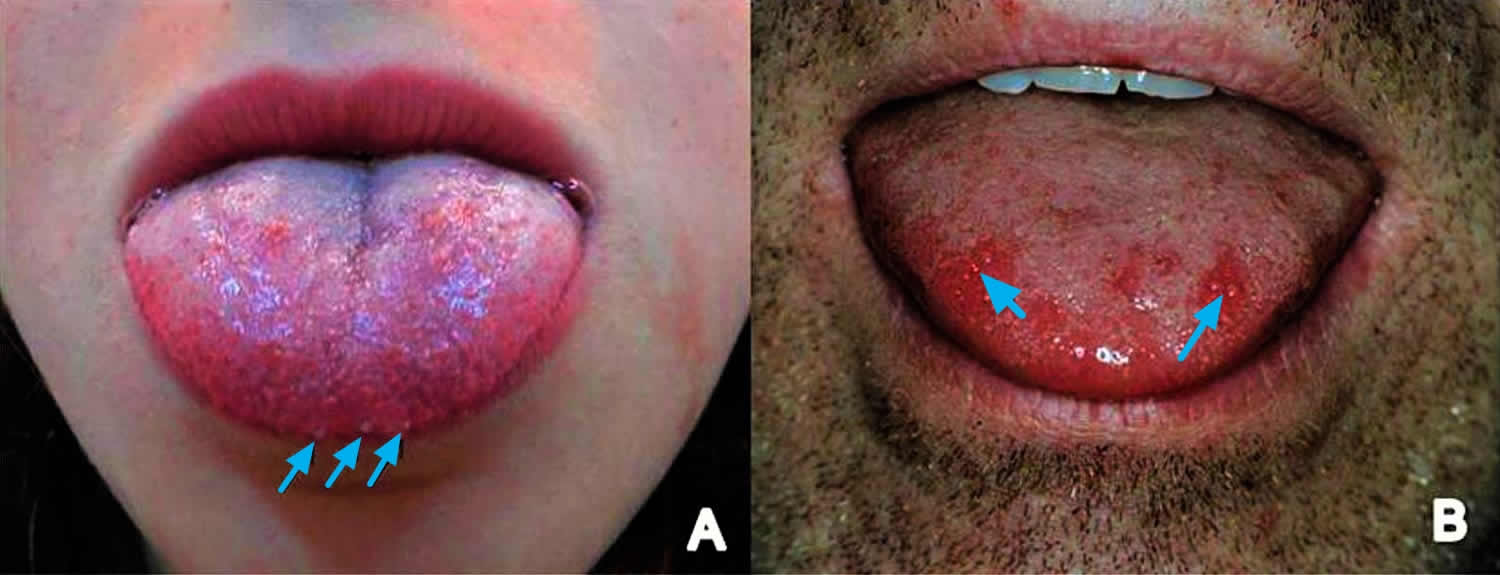
Transient lingual papillitis is considered as a common but under-diagnosed disease 8. Three variants of transient lingual papillitis have been described, based on their clinical features 9. The localized variant presents with swelling of a single to several fungiform papillae of a solitary lingual area, especially of the tip, the lateral borders and the dorsal surface and may occur in patients of every age with a female predilection 8. In the generalized variant a large proportion of the fungiform papillae is involved. During its usual course, a child of a median age of 3.5 years is initially affected and progressively the disease presents in other family members. This form is more consistent with the descriptive terms eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission 10. Both the localized and generalized lie bumps have an acute onset 11 and the enlarged papillae may vary in color from normal, erythematous or whitish to yellow, while they rarely appear brown or black, due to staining from food or smoking 12. Moreover, these two clinical patterns may be accompanied by disproportionate symptoms, including pain, burning, tingling or itchy sensation, difficulty in feeding, sensitivity to hot foods 10 and, in cases with familial transmission, hypersalivation and occasionally fever and lymphadenopathy 10.
Lie bumps symptoms typically resolve after a few hours or 1 to 4 days 11, while the lie bumps may last for 1 to 3 weeks, when diffuse lingual inflammation coexist 8.
Biopsy is not required for the final diagnosis 8, but in cases where it was performed, microscopic examination showed an inflamed fungiform papillae with minimal spongiosis and neutrophils infiltration of the epithelium 9. Taste buds that are normally present in fungiform papillae were not detected 9. The papulokeratotic variant of transient lingual papillitis is characterized by chronic, generalized tongue involvement with painless, whitish or white-yellow in color enlarged fungiform papillae, histologically corresponding to parakeratosis 9.
Figure 1. Lie bumps on tongue
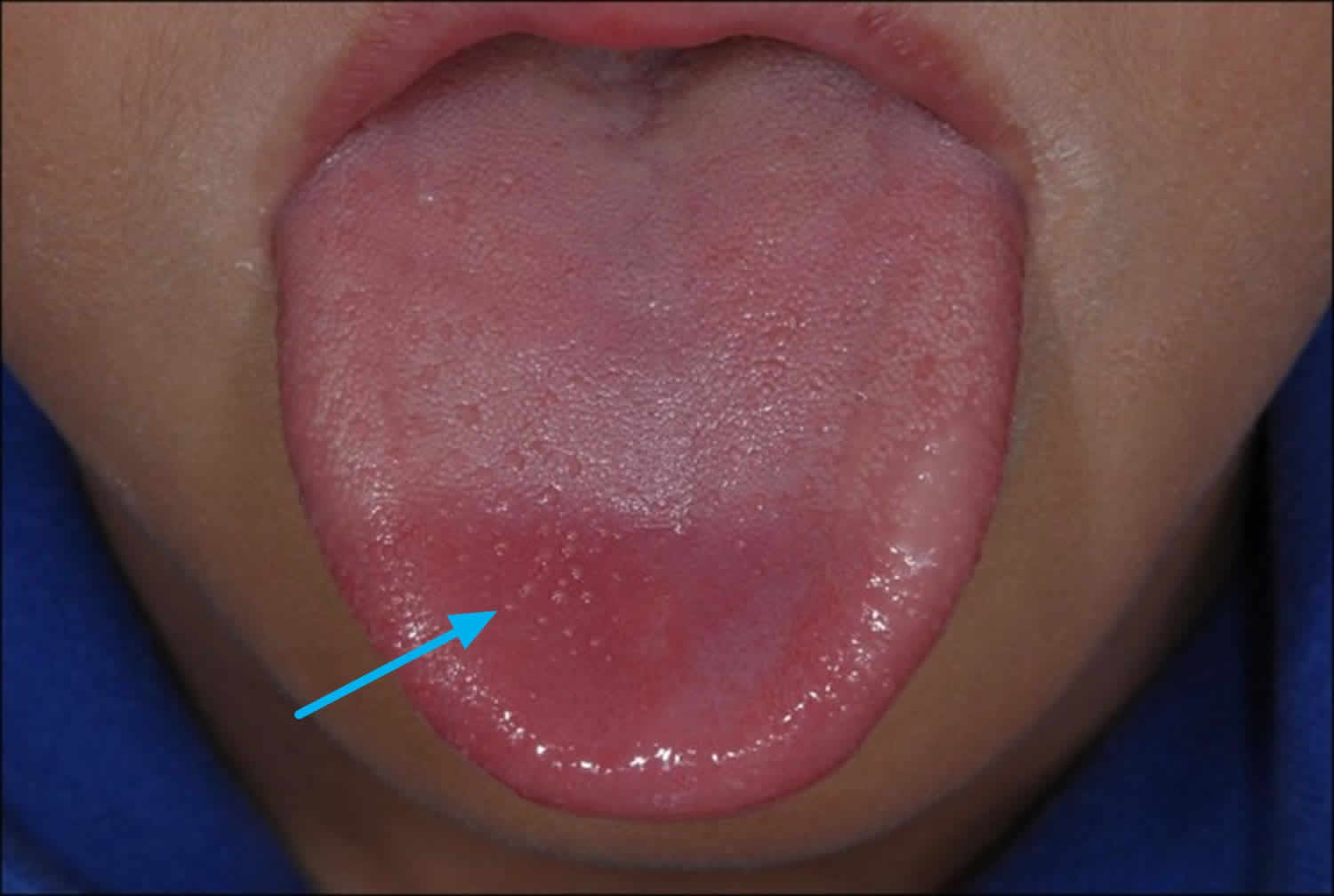
[Source 13]Figure 2. Lie bumps on top the tongue
[Source 14]What are fungiform papillae?
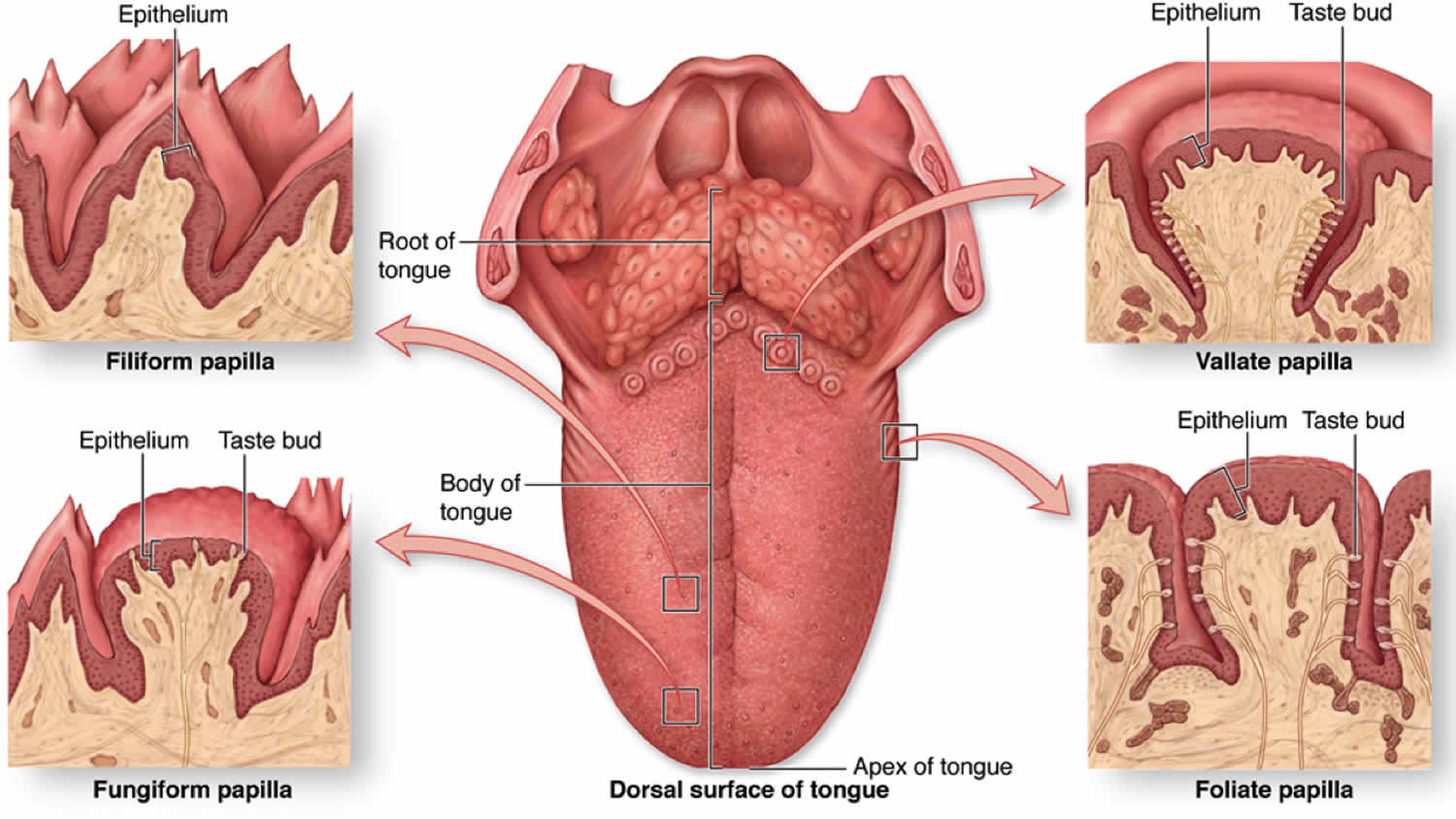
Fungiform papillae are one of the special types of bumps found on the surface of the tongue (see Figure 3). Fungiform papillae contain taste buds (especially for bitter taste), temperature receptors and have a good blood supply.
Fungiform papillae are scattered over the top and sides of the tongue, mainly towards the tip. Usually fungiform papillae are not obvious, being flat and pink.
The number and size of fungiform papillae varies:
- females have more fungiform papillae than males
- they become even more numerous after the menopause
- nerve injury may result in a reduced number of fungiform papillae and reduced taste sensation
Fungiform papillae can become obvious in a number of conditions, the most well recognised of which is the ‘strawberry tongue’ of scarlet fever.
Figure 3. Fungiform papillae
How long do lie bumps last?
Lie bumps symptoms typically resolve after a few hours or 1 to 4 days 11, while the lie bumps may last for 1 to 3 weeks, when diffuse lingual inflammation coexist 8.
Lie bumps (transient lingual papillitis) may relapse 8, most commonly its papulokeratotic variant 9. In recurrences the investigation of the possible trigger factors, especially trauma or allergens, is mandatory 8.
Classic form
The classic form of transient lingual papillitis presents as a single painful raised red or white bump on the tongue, usually towards the tip. It lasts 1-2 days then disappears, often recurring weeks, months or years later. There is no associated illness or lymph gland enlargement. Less commonly the lesions are more numerous, may disappear within hours or last several days, or may be associated with a burning or tingling sensation. Uncommonly the lesion(s) may not cause any symptoms. Some reports suggest an association with geographic tongue or scalloped markings on the side of the tongue.
Papulokeratotic variant
The papulokeratotic variant presents as recurrent multiple white bumps over the tongue that do not cause any symptoms. They may be persistent.
Eruptive lingual papillitis
Eruptive lingual papillitis is a systemic illness often associated with fever and lymph gland enlargement. The onset is sudden. An affected child may be reluctant to eat and produces excessive saliva. The tongue shows enlarged inflamed fungiform papillae on the tip and the sides of the tip but not the top. These may look like pustules. Angular cheilitis may be seen.
The illness lasts on average 1 week (range 2-15 days). Recurrences have been reported 1-2 months later with the same clinical features. Family members, parents and siblings, may develop symptoms on average one week later (range 1-15 days). In adults, the illness presents as a sudden intense burning of the tongue made worse by food. The clinical appearance is the same as in the child.
What causes lie bumps
The cause of lie bumps is unclear but appears to be multifactorial 15. Suggested causes include acute thermal injury (i.e., coffee, tea, soup, tobacco smoke) 16, acute mechanical trauma (sharp-edged teeth or restorations), orthodontic appliances or increased calculus on the anterior teeth 15, chronic mechanical trauma (tongue-thrust habit), hypersensitivity to food or candy or oral hygiene products, contact or airborne toxins (photocopier’s toner) 17, unidentified infections (local), atopic disease, gastrointestinal disorders and hormonal changes during menstruation or menopause (in women) 18. As transient lingual papillitis is more common in patients with history of atopy (allergy), it may also represent a local atopic reaction to heat or irritating foods 19. Fungiform papillary glossitis has been described in patients with a history of eczema, asthma or hayfever. It may be another name for transient lingual papillitis. These authors suggested the condition is due to increased environmental sensitivity of the tongue, similar to the increased sensitivity of the skin, lungs or nose resulting in eczema, asthma or hayfever respectively. Often, though, transient lingual papillitis is considered idiopathic (unknown cause) 20, while it is also regarded as a relapse in adults of eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission that occurred during childhood 21.
Infectious agents, particularly viruses, is implicated in the pathogenesis of both transient lingual papillitis and eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission, but is not documented 21. Immunohistochemical investigation for human papillomavirus types 6 and 11 and herpes simplex virus (HSV) type 1 and 2 20, as well as the histochemical investigation for fungi and parasites in biopsy specimens were all negative in transient lingual papillitis 20. In a recent publication, though, Krakowski et al. 22 described a case of transient lingual papillitis, where the presence of HSV type 1, was confirmed by direct lesional viral culture, in a patient with Kawasaki disease.
Association with benign migratory glossitis has been reported 23. The infective variant seems to follow a viral or “strep-mouth” pattern, may involve filiform papillae as well, is typically pediatric in presentation, is apparently contagious, and is associated with fever and other signs of upper respiratory infection or strep throat 24. A common myth represents transient lingual papillitis (lie bumps), especially the single, exquisitely painful papilla, as resulting from the telling of a lie. This potential cause has not been thoroughly researched but “lie bumps” or “liar’s bumps” are often so painful, albeit transient, that affected persons clip them off with a nail clipper to obtain relief 18.
Lie bumps diagnosis
Transient lingual papillitis and eruptive lingual papillitis are usually diagnosed clinically based on typical presentation.
Mucosal biopsy shows inflammation and swelling of a fungiform papilla, but is not usually necessary. Special stains fail to detect viral, fungal or bacterial infection. In the papulokeratotic variant, biopsy shows severe hyperparakeratosis and mild chronic inflammation.
Lie bumps treatment
Usually no treatment is required for the classic form of transient lingual papillitis as the condition resolves within hours or days.
Management of transient lingual papillitis is symptomatic and aims to relieve symptoms 25. In painful cases local anesthetics, topical corticosteroids, coating agents, saline mouthwashes and combination of antihistamines with aluminum hydroxide or magnesium hydroxide suspension for topical use have been administrated, and eating of cold foods has been recommended. The use of analgesics such as paracetamol or ibuprofen does not affect the duration and intensity of symptoms 10, while there is no consensus on the usefulness of topical antiseptics 10. Patients are also recommended to avoid irritating chewing gums, candies or oral hygiene agents 12.
Treatments reported by some patients to give relief have included:
- salt water mouth rinses
- cold fluids
- soothing foods such as yogurt
- antiseptic or local anaesthetic mouthwashes
- topical steroids
However, the majority of sufferers have found nothing to relieve the symptoms or prevent recurrence.
Transient lingual papillitis may relapse 8, most commonly its papulokeratotic variant 9. In recurrences the investigation of the possible trigger factors, especially trauma or allergens, is mandatory 8.
In eruptive lingual papillitis, paracetamol, ibuprofen and topical antiseptics have not been found to alter the duration or severity of the symptoms in children.
References- Transient lingual papillitis. https://www.dermnetnz.org/topics/transient-lingual-papillitis/
- Bouquot JE, Adibi SS, Sanchez M. Chronic lingual papulosis: new, independent entity or “mature” form of transient lingual papillitis? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:111–7. https://www.ncbi.nlm.nih.gov/pubmed/22669070
- Whitaker SB, Krupa JJ 3rd, Singh BB. Transient lingual papillitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:441–5. https://www.ncbi.nlm.nih.gov/pubmed/8899785
- Silverberg NB, Singh A, Echt AF, Laude TA. Lingual fungiform papillae hypertrophy with cyclosporin A. Lancet. 1996;348:967.
- Broscaru C, Schnopp C, Kardorff B. Fungiform papillary glossitis. J Dtsch Dermatol Ges. 2014;12:356–7. https://www.ncbi.nlm.nih.gov/pubmed/24581085
- Galun E, Rubinow A. Photocopier’s papillitis. Lancet. 1989;2:929.
- Mondal A, Kumar P. Eruptive lingual papillitis. Indian Pediatr. 2014;51:243.
- Flaitz ΚΜ, Chavarria C. Painful tongue lesions associated with a food allergy. Pediatr Dent. 2001;23:506–7.
- Brannon RB, Flaitz CM. Transient lingual papillitis: a papulokeratotic variant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:187–91.
- Roux O, Lacour JP. Eruptive lingual papillitis with household transmission: a prospective clinical study. Br J Dermatol. 2004;150:299–303.
- Bouquot JE, Adibi SS, Sanchez M. Chronic lingual papulosis: new, independent entity or “mature” form of transient lingual papillitis? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:111–7.
- Noonan V, Kemp S, Gallagher G, Kabani S. Transient lingual papillitis. J Mass Dent Soc. 2008;57:39.
- Kalogirou E-M, Tosios KI, Nikitakis NG, Kamperos G, Sklavounou A. Transient lingual papillitis: A retrospective study of 11 cases and review of the literature. Journal of Clinical and Experimental Dentistry. 2017;9(1):e157-e162. doi:10.4317/jced.53283. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5268094
- Song HS, Lee E-S. Transient Filiform Papillitis in a Child. Annals of Dermatology. 2014;26(3):415-416. doi:10.5021/ad.2014.26.3.415. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069663/
- Chronic lingual papulosis: new, independent entity or “mature” form of transient lingual papillitis? Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2012, Volume 113, Issue 1, 111 – 117. https://www.oooojournal.net/article/S1079-2104(11)00616-0/fulltext
- Transient lingual papillitis: a papulokeratotic variant. Brannon RB, Flaitz CM. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 Aug; 96(2):187-91.
- Photocopier’s papillitis. Galun E, Rubinow A. Lancet. 1989 Oct 14; 2(8668):929.
- Chronic lingual papulosis: new, independent entity or “mature” form of transient lingual papillitis? Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, Volume 113, Issue 1, 111 – 117. https://www.oooojournal.net/article/S1079-2104(11)00616-0/fulltext
- Fungiform papillary glossitis: atopic disease in the mouth? Marks R, Scarff CE, Yap LM, Verlinden V, Jolley D, Campbell J. Br J Dermatol. 2005 Oct; 153(4):740-5.
- Transient lingual papillitis. Whitaker SB, Krupa JJ 3rd, Singh BB. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996 Oct; 82(4):441-5.
- Eruptive lingual papillitis with household transmission: a prospective clinical study. Roux O, Lacour JP, Paediatricians of the Region var-Côte d’azur. Br J Dermatol. 2004 Feb; 150(2):299-303.
- Transient lingual papillitis associated with confirmed herpes simplex virus 1 in a patient with kawasaki disease. Krakowski AC, Kim SS, Burns JC. Pediatr Dermatol. 2014 Nov-Dec; 31(6):e124-5.
- Whitaker, S.B., Krupa, J.J. 3rd, and Singh, B.B. Transient lingual papillitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 82: 441–445
- Roux, O. and Lacour, J.P. Paediatricians of the Region var-Côte d’azur (Eruptive lingual papillitis with household transmission: a prospective clinical study) . Br J Dermatol. 2004; 150: 299–303
- Whitaker SB, Krupa JJ 3rd, Singh BB. Transient lingual papillitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:441–5.