Wallenberg syndrome
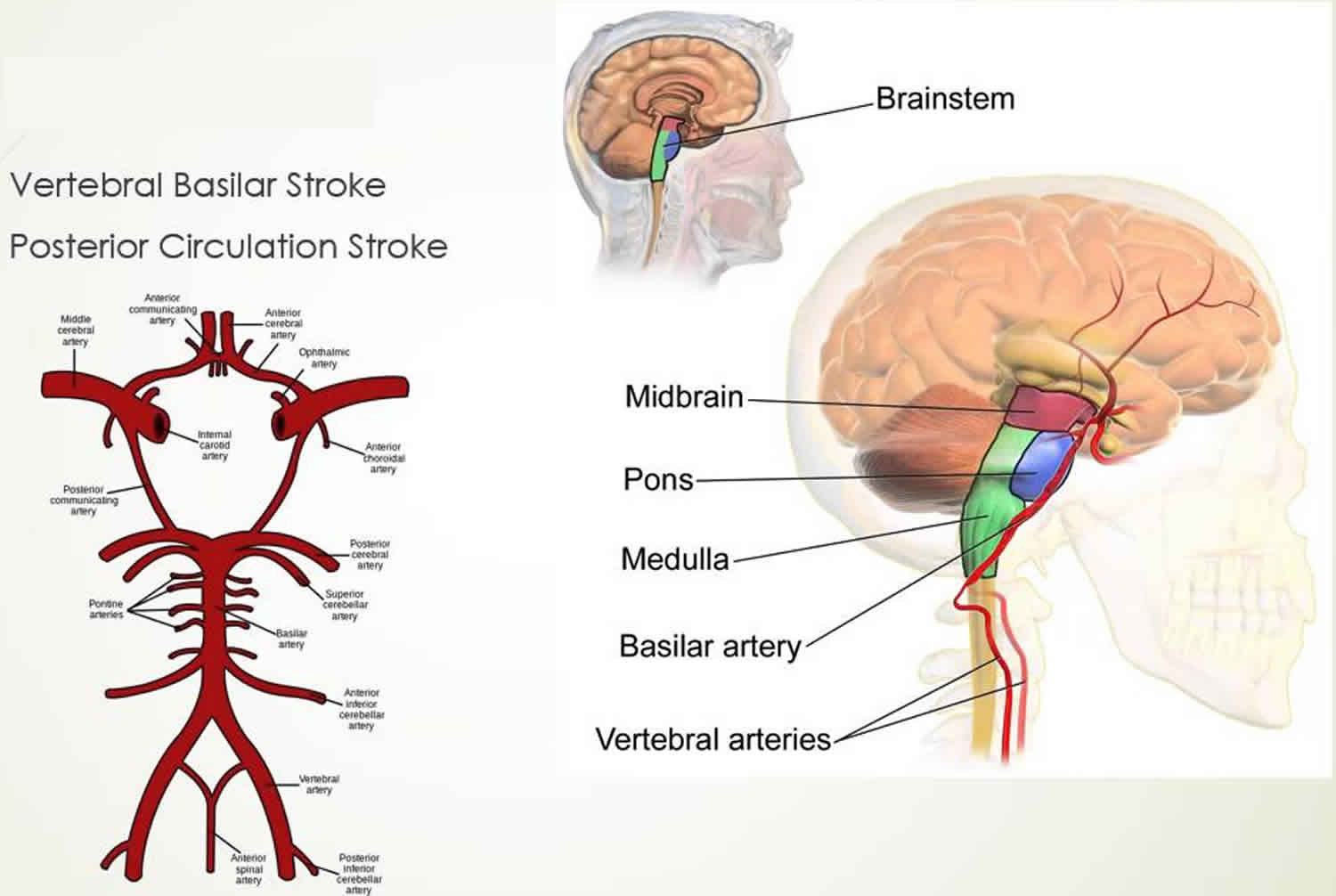
Wallenberg syndrome also known as lateral medullary syndrome or the posterior inferior cerebellar artery syndrome, is a neurological disorder is associated with a variety of symptoms that occur as a result of damage to the lateral segment of the medulla posterior to the inferior olivary nucleus 1. Wallenberg’s syndrome is caused by a stroke in the vertebral or posterior inferior cerebellar artery (PICA) of the brain stem 2. Wallenberg syndrome is the most typical posterior circulation ischemic stroke syndrome in clinical practice 3.
There are nearly 800,000 patients who suffer from an acute stroke each year in the United States. Of these, 83% are ischemic strokes. Twenty percent of the ischemic strokes occur in the posterior circulation 1. If clinicians assume that about half of these suffer from Wallenberg syndrome, it can be estimated that there are more than 60,000 new cases of Wallenberg syndrome each year in the United States. There is a predominance of men in their sixth decade. Large artery atherothrombotic causes account for about 75% of the cases followed by cardioembolism in 17% and vertebral dissection in 8% 1.
Wallenberg syndrome signs and symptoms may include swallowing difficulties, dizziness, hoarseness, nausea and vomiting, rapid involuntary movements of the eyes (nystagmus), and problems with balance and gait coordination. Some people have uncontrollable hiccups, loss of pain and temperature sensation on one side of the face, and/or a pattern of symptoms on opposite sides of the body such as paralysis or numbness in the right side of the face, with weak or numb limbs on the left side. Uncontrollable hiccups may also occur, and some individuals will lose their sense of taste on one side of the tongue, while preserving taste sensations on the other side. Some people with Wallenberg’s syndrome report that the world seems to be tilted in an unsettling way, which makes it difficult to keep their balance when they walk.
Treatment for Wallenberg’s syndrome focuses primarily on relieving symptoms and rehabilitation. Treatment may also depend on the underlying cause and/or how quickly it is identified. A feeding tube may be necessary if swallowing is very difficult. Speech/swallowing therapy may be beneficial. In some cases, medication may be used to reduce or eliminate pain. Some doctors report that the anti-epileptic drug gabapentin appears to be an effective medication for individuals with chronic pain.
While some people’s symptoms may improve within weeks or months, others may have long-term neurological problems 2.
Figure 1. Wallenberg syndrome
Wallenberg syndrome causes
Wallenberg syndrome is caused most commonly by atherothrombotic occlusion of the vertebral artery, followed most frequently by the posterior inferior cerebellar artery (PICA), and least often, the medullary arteries 1. Hypertension is the commonest risk factor followed by smoking and diabetes. Cerebral embolism is a less frequent cause of the infarction. The other important cause to remember is vertebral artery dissection which may have risk factors including neck manipulation or injury, Marfan syndrome, Ehlers Danlos syndrome, and fibromuscular dysplasia. Vertebral artery dissection is the commonest cause of Wallenberg syndrome in younger patients 4.
The primary pathology of Wallenberg syndrome is occlusion of the posterior inferior cerebellar artery (PICA) or one of its branches 5. Wallenberg syndrome can also be due to occlusion of the vertebral artery, or the inferior, middle, or superior medullary vessels. Anatomically the infarcted area in Wallenberg syndrome is supplied by the posterior inferior cerebellar artery (PICA). It turns out occlusion of the posterior inferior cerebellar artery accounts for only a small number of cases. The majority (80%) are caused by occlusion of the vertebral artery which gives rise to the posterior inferior cerebellar artery and the anterior spinal artery before it joins with the opposite vertebral artery to form the basilar artery. The commonest mechanism of occlusion of the vertebral artery or posterior inferior cerebellar artery is atherothrombosis 6.
Several other disorders or conditions reportedly have been associated with Wallenberg syndrome, including 7:
- mechanical trauma to the vertebral artery in the neck
- vertebral arteritis (inflammation of the wall of the artery)
- metastatic cancer
- hematoma
- aneurysm of the vertebral artery
- herpetic brainstem encephalitis (relating to herpes)
- head injury
- arteriovenous malformations (AVMs)
- multiple sclerosis
- varicella infection
- brainstem tuberculoma (a rare form of tuberculosis)
Wallenberg syndrome symptoms
Wallenberg syndrome may cause a variety of symptoms depending on the specific cause and the exact location of the damage to the brain. Symptoms may include 8:
- pain and temperature sensory loss on one side of the face as well as on the opposite side of the body
- rapid involuntary movements of the eyes (nystagmus)
- problems with balance and gait (walking) coordination
- vomiting
- vertigo
- nystagmus
- dysphagia
- hoarseness
- uncontrollable hiccups
- Horner syndrome (decreased pupil size, a drooping eyelid and decreased sweating on the affected side of the face) with visual deficits
A typical patient with Wallenberg syndrome is an elderly patient with vascular risk factors. Like any acute stroke syndrome, the onset is acute. The most common symptoms of onset are dizziness with vertigo, loss of balance with gait instability, hoarseness of voice and difficulty swallowing. The symptoms often progressed over several hours to sometimes a couple of days 6.
Usually, there is no weakness associated with this syndrome and so this condition is often misdiagnosed or missed. A careful neurological examination is key to the diagnosis. A complete Wallenberg syndrome is not common, yet partial syndromes are good enough for the diagnosis most of the time. The important points in clinical diagnosis are a combination of crossed hemiparesis or hemianesthesia to indicate a brainstem lesion and the involvement of structures in the posterolateral medulla to localize where in the brainstem.
Different combinations of the following deficits may all be found in Wallenberg syndrome:
On the side of lesion:
- Vertigo with nystagmus (inferior vestibular nucleus and pathways). The nystagmus is typically central beating to the direction of gaze. Nausea and vomiting, and sometimes hiccup are associated with vertigo. Hiccup can often be intractable.
- Dysphonia, dysarthria, and dysphagia (different nuclei and fibers of the IX and X nerves), often with ipsilateral loss of gag reflex
- Horner syndrome (sympathetic fibers)
- Ipsilateral ataxia with a tendency to fall to the ipsilateral side (inferior cerebellar hemisphere, spinocerebellar fibers, and inferior cerebellar peduncle)
- Pain and numbness with impaired facial sensation on the face (descending trigeminal tract)
- Impaired taste sensation (involvement of nucleus tractus solitarius)
On the contralateral side:
- Impaired pain and temperature sensation in the arms and legs (spinothalamic tract)
- It is important to note that there is no or only minimal weakness of the contralateral side (corticospinal fibers are ventral in location)
It is clinically interesting to note that more rostral lesions tend to be more ventrally located. These patients present with more dysphagia and dysphonia due to the involvement of the nucleus ambiguus. More caudal lesions involve more dorsolateral structures. These patients present with vertigo, ataxia, nausea/vomiting, and Horner syndrome.
Wallenberg syndrome diagnosis
The diagnosis is usually made or suspected from a clinical exam and history of presentation. MRI with diffusion-weighted imaging is the best diagnostic test to confirm the infarct in the inferior cerebellar area or lateral medulla 9. Up to 30% of patients with nondisabling stroke do not have a lesion on diffusion-weighted imaging-MRI brain. These patients are diffusion-weighted imaging-negative stroke patients and secondary prevention should be started to prevent future strokes 10.
A CT angiogram or MR angiogram is very helpful in identifying the site of vascular occlusion and rule out uncommon causes such as vertebral artery dissection 11.
An ECG is helpful in excluding any underlying atrial fibrillation or unexpected acute coronary syndrome.
Checking the serum electrolytes is important.
Patient with dysphagia or dysarthria needs to be assessed by the speech pathologist because any food or medicine can be given orally.
Wallenberg syndrome treatment
Similar to the management of any acute ischemic stroke, remember “TIME IS BRAIN.” Rapid evaluation is essential to an orderly approach(algorithm) developed within each hospital or stroke center. Management in certified stroke centers has shown to improve overall patient outcome. Treatment aims at reducing the size of infarction and preventing any medical complication with the final target of improving patient outcome and prognosis 6.
The management steps include:
- Intravenous (IV) thrombolysis with IV tissue plasminogen activator (tPA) within 3 or 4.5 hours of onset of the ischemic stroke with slightly different exclusion criteria. Overall IV thrombolysis, whether within 3 or 4.5 hours, improve functional stroke outcome by 30%. There have been studies showing that the window for posterior circulation strokes may be longer than 4.5 hours 12.
- Endovascular revascularization: the newer devices have been shown to improve outcome with the number needed to treat to be as low as 3. These are indicated mainly for large vessel intracranial occlusion which carries very poor prognosis without revascularization.
- General medical therapy: Patient is best monitored in the intensive care unit (ICU) for 24 hours after IV thrombolysis. Otherwise, it will be best to manage the patients in dedicated stroke beds or units.
- IV fluid: avoid hypotonic solution to reduce risks of cerebral edema. Normal saline generally is the best.
- Blood pressure management: cerebral autoregulation is impaired in the infarcted areas of the brain. Blood pressure very often comes down gradually without any drug treatment. In general, blood pressure does not need to be lowered unless the patient receives IV thrombolysis or when it is over 220/120.
- Speech therapy assessment: very important to prevent aspiration.
- Deep vein thrombosis prophylaxis: with sequential pressure devices and low dose heparin or low molecular weight heparin.
- Blood sugar: best to keep the patient normoglycemic.
- Fever: the source of fever needs to be identified and treated. A simple antipyretic with acetaminophen is helpful.
- Antithrombotics: numerous more recent clinical trials failed to show any benefit or anticoagulants in acute stroke even in atrial fibrillation. Antithrombotic therapy with aspirin does improve the outcome.
- Early physical therapy and occupational therapy with a good plan for rehabilitation.
Secondary stroke prevention will be decided soon. This will again include a multimodality approach:
- Carotid endarterectomy for significant large vessel extracranial stenosis
- Oral anticoagulation for cardioembolic strokes
- Antiplatelets such as aspirin, clopidogrel, or Aggrenox (ASA/Dipyridamole) for other forms of stroke
- Statin
- Smoking cessation
- Good control of diabetes
- Good blood pressure control
- Healthy diet and lifestyle with regular exercises
This multimodal approach can reduce the risk of subsequent stroke by 80%.
Wallenberg syndrome prognosis
The outlook for someone with Wallenberg’s syndrome depends upon the size and location of the area of the brain stem damaged by the stroke. Some individuals may see a decrease in their symptoms within weeks or months. Others may be left with significant neurological disabilities for years after the initial symptoms appeared.
Overall Wallenberg syndrome has a better functional outcome than most other stroke syndromes. Most patients can return to satisfactory activities of daily living 1. The commonest complication is gait instability.
References- Lui F, Tadi P, Anilkumar AC. Wallenberg Syndrome. [Updated 2019 Dec 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470174
- Wallenberg’s Syndrome Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Wallenbergs-Syndrome-Information-Page
- Ogawa K, Suzuki Y, Oishi M, Kamei S. Clinical study of 46 patients with lateral medullary infarction. J Stroke Cerebrovasc Dis. 2015 May;24(5):1065-74.
- Inamasu J, Nakae S, Kato Y, Hirose Y. Clinical Characteristics of Cerebellar Infarction Due to Arterial Dissection. Asian J Neurosurg. 2018 Oct-Dec;13(4):995-1000.
- Hong YH, Zhou LX, Yao M, Zhu YC, Cui LY, Ni J, Peng B. Lesion Topography and Its Correlation With Etiology in Medullary Infarction: Analysis From a Multi-Center Stroke Study in China. Front Neurol. 2018;9:813.
- Kim JS, Caplan LR. Clinical Stroke Syndromes. Front Neurol Neurosci. 2016;40:72-92.
- Verma R, Sharma P. Lateral medullary syndrome due to brain stem tuberculoma. J Assoc Physicians India. June 2011; 59:382-384. https://www.ncbi.nlm.nih.gov/pubmed/21751596
- Louis DW, Dholakia N, Raymond MJ. Wallenberg Syndrome with Associated Motor Weakness in a Two-Week-Postpartum Female. Case Rep Neurol. September 23, 2015; 7(3):186-190. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4611068
- De Cocker LJ, Lövblad KO, Hendrikse J. MRI of Cerebellar Infarction. Eur. Neurol. 2017;77(3-4):137-146.
- Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Clinically Confirmed Stroke With Negative Diffusion-Weighted Imaging Magnetic Resonance Imaging: Longitudinal Study of Clinical Outcomes, Stroke Recurrence, and Systematic Review. Stroke. 2015 Nov;46(11):3142-8.
- Kumral E, Kisabay A, Ataç C, Calli C, Yunten N. Spectrum of the posterior inferior cerebellar artery territory infarcts. Clinical-diffusion-weighted imaging correlates. Cerebrovasc. Dis. 2005;20(5):370-80.
- Salerno A, Cotter BV, Winters ME. The Use of Tissue Plasminogen Activator in the Treatment of Wallenberg Syndrome Caused by Vertebral Artery Dissection. J Emerg Med. 2017 May;52(5):738-740.