What is eye astigmatism
Astigmatism is an imperfection in the curvature of your cornea — the clear, round dome covering the eye’s iris and pupil — or in the shape of the eye’s lens 1. Normally, the cornea and lens are smooth and curved equally in all directions, helping to focus light rays sharply onto the retina at the back of your eye. However, if your cornea or lens isn’t smooth and evenly curved, light rays aren’t refracted properly. This is called a refractive error. Astigmatism is a common type of refractive error. It is a condition in which the eye does not focus light evenly onto the retina, the light-sensitive tissue at the back of the eye 2.
- When the cornea has an irregular shape, it is called corneal astigmatism. Corneal astigmatism is mainly the result of an aspheric anterior surface of the cornea, which can be measured readily by means of a keratometer; in a small fraction of cases (approximately 1 in 10) the effect is neutralized by the back surface 3. The curvature of the back surface of the cornea is not considered in most studies, because it is more difficult to measure; moreover, in the case of severe corneal astigmatism, there is evidence that both surfaces have the same configuration.
- When the shape of the lens is distorted, you have lenticular astigmatism. Lenticular astigmatism factors are errors in the curvature of the 2 surfaces of the crystalline lens, irregularity in the refractive index of the lens, and an eccentric lens position.
Either type of astigmatism can cause blurred vision. Blurred vision may occur more in one direction, either horizontally, vertically or diagonally.
Astigmatism that is ⩾1 Diopter is a common refractive error, with a frequency of ∼20% in the Caucasian population.
What does the cornea do ?
The cornea is responsible for 65-75 percent of the eye’s total focusing power 4.
The cornea and lens of the eye are built to focus light on the retina, which is the light-sensitive tissue at the back of the eye. When light strikes the cornea, it bends—or refracts—the incoming light onto the lens. The lens refocuses that light onto the retina, which starts the translation of light into vision. The retina converts light into electrical impulses that travel through the optic nerve to the brain, which interprets them as images.
The refractive process the eye uses is similar to the way a camera takes a picture. The cornea and lens in the eye act as the camera lens. The retina is like the film (in older cameras), or the image sensor (in digital cameras). If the image is not focused properly, the retina makes a blurry image.
The cornea also serves as a filter that screens out damaging ultraviolet (UV) light from the sun. Without this protection, the lens and the retina would be exposed to injury from UV rays.
What is refraction ?
Refraction is the bending of light as it passes through one object to another. Vision occurs when light rays are bent (refracted) as they pass through the cornea and the lens. The light is then focused on the retina. The retina converts the light-rays into messages that are sent through the optic nerve to the brain. The brain interprets these messages into the images we see 2.
How does astigmatism occur ?
Astigmatism occurs when light is bent differently depending on where it strikes the cornea and passes through the eyeball. The cornea of a normal eye is curved like a basketball, with the same degree of roundness in all areas. An eye with astigmatism has a cornea that is curved more like a football, with some areas that are steeper or more rounded than others. This can cause images to appear blurry and stretched out.
As a result of either type of astigmatism, your vision for both near and far objects appears blurry or distorted. It’s almost like looking into a fun house mirror in which you appear too tall, too wide or too thin.
Who is at risk for astigmatism ?
Astigmatism can affect both children and adults. People can be born (present at birth) with astigmatism and may occur in combination with nearsightedness (myopia) or farsightedness (hyperopia) 1. In fact, most people probably are born with some degree of astigmatism and they may have it along with other refractive errors: nearsightedness (you can see near things more clearly than distant ones) or farsightedness (you can see distant objects clearly, but objects nearby may be blurry). The incidence of astigmatism was five times greater in myopes than in nonmyopes. Some patients with slight astigmatism will not notice much change in their vision. It is important to have eye examinations at regular intervals in order to detect any astigmatism early on for children.
In a study involving risk factor for astigmatism in preschool children 5 preschool children with myopia (≤−1.0 diopters) were 4.6 times as likely to have astigmatism than those without refractive error, whereas participants with hyperopia (≥+2.00 diopters) were 1.6 times as likely. Children 6 to <12 months of age were approximately 3 times as likely to have astigmatism than children 5 to 6 years of age. Both Hispanic and African-American children were as likely to have astigmatism than non-Hispanic white children. Furthermore, children whose mothers smoked during pregnancy were 1.46 times as likely to have astigmatism than children whose mothers did not smoke 5.
Children who have astigmatism symptoms may not be aware they have this condition and are unlikely to complain about blurred or distorted vision 1. But uncorrected astigmatism can seriously impact a child’s ability to achieve in school and sports. And some forms of astigmatism can be a sign of keratoconus, a cone-like bulge of the cornea, which can distort vision. That’s why it is crucial that children have regular eye exams to detect astigmatism or other vision problems as early as possible.
Can you have astigmatism and not know it ?
It is possible to have mild astigmatism and not know about it. This is especially true for children, who are not aware of their vision being other than normal. Some adults may also have mild astigmatism without any symptoms. It’s important to have comprehensive dilated eye exams to make sure you are seeing your best.
Is there a cure for astigmatism ?
No. However, there are plenty of treatment options to correct the astigmatism, such as eyeglasses, contact lenses and corrective surgery like LASIK. See treatment below for more details.
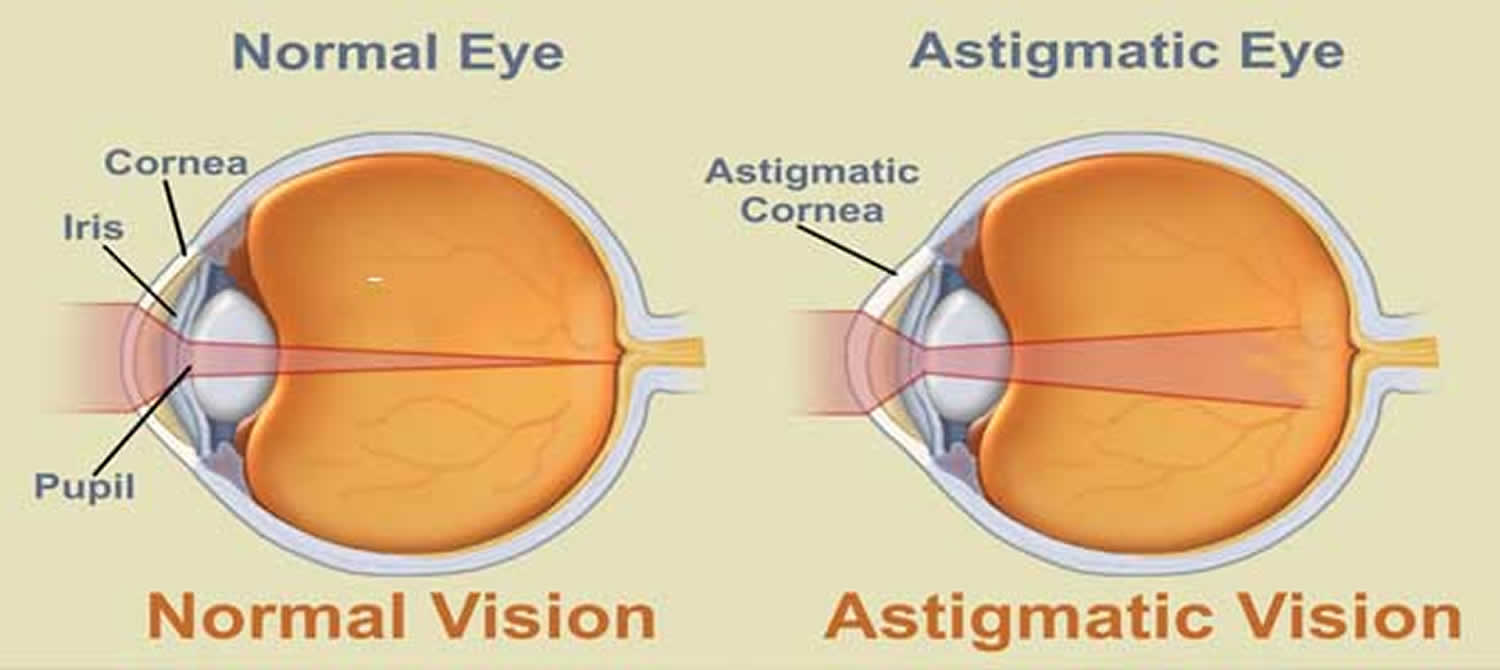
Figure 1. Eye anatomy
Figure 2. Eye with Lenticular Astigmatism (Irregular Lens)
Figure 3. Eye with Corneal Astigmatism (Irregular Cornea)
Figure 4. Normal eye refraction (perfect image on the Macula’s Fovea)
Figure 5. In astigmatism, images focus in front of and beyond the retina, causing both close and distant objects to appear blurry.
Astigmatism in children
Children may not realize their vision is blurry, so they need to be screened for eye disease and have their vision tested by a pediatrician, an ophthalmologist, an optometrist or another trained screener at the following ages and intervals.
- During the newborn period
- At well-child visits until school age
- During school years, every one to two years at well-child visits, at the eye doctor, or through school or public screenings.
Can astigmatism get worse
As with other organs, the eye’s growth is regulated by homeostatic control mechanisms. Unlike other organs, the eye relies on vision as a principal input to guide growth 6. A mechanism exists to regulate eye growth so as to minimise refractive errors 7. For many years this process was largely hypothetical, but in recent years a number of longitudinal studies have provided direct evidence for such a mechanism in human infants 8, 9, 10. The astigmatism rates of change (diopters/year), were highly dependent on their respective initial powers 8. Animal studies have provided clear evidence of the mechanisms that might drive this process. It has now been demonstrated, in a wide range of species, that the retina is able to detect and use hyperopic and myopic defocus to control eye growth 6. The progression rate of astigmatism was affected by the ethnicity, presence of myopia, axis, and subtype of astigmatism 11. A study of astigmatism from infancy to late childhood showed that the mean cylindrical power remained stable between 7 and 9 years of age. Gwiazda et al. 12 reported that cylinder power may increase slightly after 10 years of age, although this trend was not statistically significant. More studies should be performed in older children to determine whether astigmatism progresses beyond certain age group. The association of computer use with progression of astigmatism remained even after adjustment for myopia and had not been reported in previous studies on astigmatism. Playing video games and computer use may be associated with astigmatism severity, although the presence of astigmatism (> 1 D) was not associated with any nearwork factors. A family history of myopia was associated with oblique astigmatism severity 13. The exact explanation for this association was unclear and could be explored in further studies. In short, astigmatism may change with time, requiring new glasses or contact lenses. Laser vision correction can usually eliminate, or greatly reduce, astigmatism.
Control of Eye Growth by Visual Signals
Eye length must match the focal length of its optics for images of distant objects to fall on the retina (emmetropia) rather than in front of or behind it. Although this might happen by a perfectly shaped eye in the embryo growing proportionally in all dimensions, this is not what occurs. In all species studied, the eyes at birth or hatching are ill matched to the focal lengths of their optics – the eyes are either too short and thus are hyperopic or the eyes are too long and thus myopic 14. It was presumed that this homeostatic growth control has two components: active regulation using nonvisual signals that convey size (e.g. genes), as is used in the developmental control of other organs, and, specific to the eye, visually guided control of growth. Because normal vision eyes that are initially of normal size and shape compensate for lenses, thereby becoming abnormal in size and shape, vision must be more powerful than other inputs to the postnatal homeostatic controller. Therefore, vision guides the growth of the eye: if spectacle lenses cause images to fall either behind or in front of the retina (hyperopia or myopia, respectively), eye growth compensates for the optical effects of the lenses.
Spectacle Lens Compensation. The homeostatic control of eye growth functions to keep images sharply focused on the retina. Therefore, if the eye length increases more slowly than does the focal length, the focal plane will be behind the retina, creating hyperopic defocus on the retina. The same occurs if one puts a negative lens over the eye (Figure 6A – Red Concave lens). To regain sharp focus, the retina needs to be displaced backward to where the image is. This is done in two ways: the eye is lengthened by increasing the rate of growth or of remodeling of the sclera at the posterior pole of the eye 15, 16 and the retina is pulled back within the eye by the thinning of the choroid, the vascular layer between the retina and sclera 17; once distant images are again focused on the retina (emmetropia), both the rate of ocular elongation and the choroid thickness return to normal.
Conversely, if the eye length increases more quickly than the focal length does, the image will be formed in front of the retina, creating myopic defocus. The same occurs if one puts a positive lens over the eye (Figure 6A – Blue Convex lens). The eye compensates first by expanding the choroid, which pushes the retina forward toward the image plane, and then by slowing ocular elongation, which causes the continuously increasing focal length of the eye to move the image plane back to the retina (Figure 6B) 18, 17.
In addition to these changes in eye length and choroid thickness that occur over days or weeks, the eye can change the focal length of its optics in a fraction of second (ocular accommodation). These three processes all act to put the image onto the retina.
One of the most striking aspects of the effects of both lenses and diffusers on the eye is that they act locally within the eye. If diffusers or negative lenses cover only half of the retina, only that half of the eye becomes enlarged and myopic 19 and if positive lenses cover half the retina, only that half shows inhibited eye growth.
Figure 6. Control of eye growth by visual signals
Note: (A) A positive lens (blue, convex) causes the image to form in front of the retina (myopic defocus), whereas a negative lens (red, concave) pushes the image plane behind the retina (hyperopic defocus). With no lens (black rays), the image of a distant object is focused on the retina.
(B) The eye compensates for positive lenses by slowing its rate of elongation and by thickening the choroid, pushing the retina forward toward the image plane. It compensates for negative lenses by increasing the rate of elongation and thinning the choroid, pulling the retina back toward the image plane. The emmetropic eye is intermediate in length and in choroid thickness.
Several studies have addressed changes in astigmatism during life; the general consensus is that astigmatism present during the 1st year of life decreases as the infant grows, but that there are few small changes after the age of 2 years and that a stable value is reached at age ⩾3 years 21, 22, 23.
What causes astigmatism
Astigmatism is caused by an irregular curvature of the eye’s cornea or lens 24. If your cornea or lens isn’t smooth and evenly curved, light rays aren’t refracted properly. This is called a refractive error. Astigmatism is one type of refractive error, with blurred or distorted vision at near and far distances.
Astigmatism is very common. In most cases, people with astigmatism are born with this condition. The reason why corneal shape differs from person to person is unknown, but the likelihood of developing astigmatism is inherited.
Sometimes, astigmatism can develop after an eye disease, eye injury or surgery. It is a myth that astigmatism can develop or worsen from reading in low light or sitting very close to the television 24.
Astigmatism symptoms
Signs and symptoms of astigmatism may include 25:
- Blurred or distorted vision
- Eyestrain or discomfort
- Headaches
- Difficulty with night vision
- Squinting
Having these symptoms may not necessarily mean that you have astigmatism, but they do indicate the need for a visit to your ophthalmologist for a complete eye exam 24.
Other refractive errors
Astigmatism may occur in combination with other refractive errors, which include:
- Nearsightedness (myopia). This occurs when your cornea is curved too much for the length of the eyeball or your eye is longer than normal or a lens that is too thick 26. Instead of being focused precisely on your retina, light is focused in front of your retina, making distant objects seem blurry. In a myopic eye, the eyeball is usually too long from front to back 26. This causes light rays to focus at a point in front of the retina, rather than directly on its surface. This makes distant objects blurry. Myopia can also be the result of a cornea that is too curved for the length of the eyeball or a lens that is too thick 26. For some people, their myopia may be caused by a combination of problems in the cornea, lens, and length of the eyeball 26.
- Farsightedness (hyperopia). This occurs when your cornea is curved too little or your eyeball is shorter than normal or it may also be caused by an abnormal shape of the cornea or lens. 27. The effect is the opposite of nearsightedness. When your eye is in a relaxed state, light never comes to a focus on the back of your eye, making nearby objects seem blurry.
Figure 7. Nearsightedness (Myopia)
[Source 28]Figure 8. Farsightedness (Hyperopia)
[Source 29]How is astigmatism diagnosed ?
Astigmatism is usually found during a comprehensive dilated eye exam 30. Being aware of any changes in your vision is important. It can help in detecting any common vision problems. If you notice any changes in your vision, visit your eye care professional for a comprehensive dilated eye examination.
Your visual acuity will be measured, where you will be asked to read letters on a distance chart to determine the clarity of your vision at a certain distances. You will also have the focusing power of your eyes tested with a series of lenses placed in front of your eyes. The curvature of your cornea will be measured with a keratometer, and corneal topography may be used to provide additional information about the shape of the surface of the cornea.With these tests, your eye doctor can diagnose astigmatism and will be able to determine the power of glasses or contact lenses you require for clear vision. He or she will also discuss other options for treatment, such as astigmatism surgery.
Your eye doctor may use several machines to measure you for astigmatism:
- An auto refractor shines light into the eye and then measures how it changes as it bounces off the back of the eye.
- A topography machine (also called a keratometer) focuses a circle of light on the cornea and measures its reflection. This determines the curvature of the cornea and helps the doctor properly fit your contact lenses.
- A phoropter measures how a lens must be shaped and curved to correct your vision to a normal state. The doctor has you look through a series of lenses in front of your eyes, and asks which ones make your vision better. Based on your answers, the doctor determines the lenses that provide the clearest vision.
What Do Astigmatism Measurements Mean ?
When you have an eye exam, your eye doctor will test you for astigmatism, a condition that may lead to blurred or double vision.
Astigmatism is measured in diopters. A perfect eye with no astigmatism has O diopters. Most people have between 0.5 to 0.75 diopters of astigmatism. People with a measurement of 1.5 or more typically need contacts or eyeglasses to correct their astigmatism in order to maintain clear vision 31.
Glasses or contacts correct astigmatism by counteracting uneven curvatures of your cornea and lens. Treatment such as LASIK can treat astigmatism as well.
A person with the eye condition known as kerataconus, in which the cornea becomes thin and develops a cone-like bulge, can have astigmatism of up to 20 diopters. In such extreme conditions, a corneal transplant may be necessary to restore the spherical shape of the cornea. Ophthalmologists and optometrists sometimes use different measurements for astigmatism. Optical shops — who actually make the glasses or contacts to correct vision — have no problem understanding the prescription, no matter who is providing it.
Of the three numbers on your contacts or glasses prescription, the last two refer to astigmatism:
- “Spherical” indicates whether you are nearsighted or farsighted. A plus sign indicates you are farsighted, a minus sign indicates you are nearsighted. The higher the number, the stronger your prescription.
- “Cylinder” measures what degree of astigmatism you have, or how flat or irregular your cornea is shaped.
- “Axis” is measured in degrees, and refers to where on the cornea the astigmatism is located. Axis numbers go from 0 to 180.
Figure 9. Keratoconus

Astigmatism Treatment
Usually, mild to moderate astigmatism can be corrected with eyeglasses or contact lenses 32.
- Eyeglasses. Eyeglasses are made with lenses that help compensate for the uneven shape of your eye. The lenses make the light bend into your eye properly. Eyeglasses can also correct for other refractive errors, such as nearsightedness or farsightedness.
- Contact lenses. Like eyeglasses, contact lenses can correct most astigmatism. They are available in a variety of types and styles, including disposable soft; extended wear; rigid, gas permeable; and bifocal.
While it used to be the case that contact lenses for astigmatism could only be rigid contact lenses (RGPs, also called GP lenses), this is no longer true. Now, soft lenses called toric contact lenses can correct astigmatism. But while soft toric lenses may be appropriate for some, if you have severe astigmatism, rigid contacts or glasses may be a better option. Your eye doctor will discuss your lens options with you.
Contact lenses are also used in a procedure called orthokeratology. In orthokeratology, you wear rigid contact lenses for several hours a day until the curvature of your eye evens out. Then you wear the lenses less frequently to maintain the new shape. If you discontinue this treatment, your eyes return to their former shape.
Wearing contact lenses for extended periods of time increases the risk of infection in the eye.
Ask your eye doctor about the pros and cons and risks of contact lenses and what might be best for you.
- Refractive Surgery aims to change the shape of the cornea permanently. This change in eye shape restores the focusing power of the eye by allowing the light rays to focus precisely on the retina for improved vision. There are many types of refractive surgeries. Your eye care professional can help you decide if surgery is an option for you.
Types of refractive surgery for astigmatism include:
- Laser-assisted in-situ keratomileusis (LASIK). With this procedure, your eye surgeon makes a thin, hinged flap in your cornea. He or she uses an excimer laser to sculpt the shape of the cornea and then repositions the flap.
- Laser-assisted subepithelial keratectomy (LASEK). Instead of creating a flap in the cornea, the surgeon loosens the cornea’s thin protective cover (epithelium) with a special alcohol. He or she uses an excimer laser to change the curvature of the cornea and then repositions the loosened epithelium.
- Photorefractive keratectomy (PRK). This procedure is similar to LASEK, except the surgeon removes the epithelium. It will grow back naturally, conforming to your cornea’s new shape. You may need to wear a bandage contact lens for a few days after surgery.
- Epi-LASIK. This is a variation of LASEK. Your doctor uses a special mechanized blunt blade — instead of the alcohol — to separate a very thin sheet of epithelium. He or she then uses an excimer laser to reshape the cornea and repositions the epithelium.
Other newer refractive surgeries include clear lens extraction and implantable contact lenses. There is no one best method for refractive surgery, and the decision should only be made after a complete evaluation and thorough discussion with your surgeon.
Some of the possible complications that can occur after refractive surgery include:
- Undercorrection or overcorrection of your initial problem
- Visual side effects, such as a halo or starburst appearing around lights
- Dry eye
- Infection
- Corneal scarring
- Rarely, vision loss
Discuss the potential risks and benefits of these procedures with your eye doctor.
How long does it take to heal after laser eye surgery ?
One of the benefits of correcting refractive errors with laser surgery is that, in most cases, recovery is relatively quick 33.
Immediately after LASIK, LASEK, or other similar procedures that create a replaceable flap in your cornea, your eye begins to heal. The day after your surgery, your eye surgeon or other eye doctor will test your vision and check to see that your eyes are healing as they should. In most cases, you can return to work, as well as drive, the day after the procedure.
If you have had PRK, healing may take a little longer. This is because a thin, outer layer of corneal cells is removed (rather than replaced as a flap like with LASIK or LASEK). The cells grow back, but it takes a few days after surgery to do so. This will delay the amount of time it takes to comfortably and safely get back to working and driving.
For several weeks or even months after laser eye surgery, it is normal to have some blurry vision or notice your vision changing. You may also have dry eyes, or see glare or halos around lights.
For six months or longer after laser surgery, you will probably be scheduled for regular follow-up visits with your eye doctor to check how your eyes are doing. In most cases, vision is stable and clear at about six months after surgery. If you had dry eyes or other visual disturbances after surgery, you should find most of these symptoms have disappeared or are much less obvious.
Past the six-month point after laser eye surgery, if you still have vision issues, your ophthalmologist may recommend another laser surgery procedure—called an enhancement—to fine tune your eyesight.
LASIK for astigmatism
LASIK (laser-assisted in situ keratomileusis) is an outpatient refractive surgery procedure used to treat nearsightedness, farsightedness and astigmatism 34. A laser is used to reshape the cornea — the clear, round dome at the front of the eye — to improve the way the eye focuses light rays onto the retina at the back of the eye.
With LASIK, an ophthalmologist creates a thin flap in the cornea using either a blade or a laser. The surgeon folds back the flap and precisely removes a very specific amount of corneal tissue under the flap using an excimer laser. The flap is then laid back into its original position where it heals in place.
For people who are nearsighted, LASIK is used to flatten a cornea that is too steep. Farsighted people will have LASIK to achieve a steeper cornea. LASIK can also correct astigmatism by shaping an irregular cornea into a more normal shape.
It is important that anyone considering LASIK have realistic expectations. LASIK allows people to perform most of their everyday tasks without corrective lenses. However, people looking for perfect vision without glasses or contacts run the risk of being disappointed. More than 90 percent of people who have LASIK achieve somewhere between 20/20 and 20/40 vision without glasses or contact lenses. If sharp, detailed 20/20 vision is essential for your job or leisure activities, consider whether 20/40 vision would be good enough for you.
You should be comfortable with the possibility that you may need a second surgery (called a retreatment or enhancement) or that you might need to wear glasses for certain activities, such as reading or driving at night. Also, you should be aware that LASIK cannot correct presbyopia, the age-related loss of close-up focusing power.
How the LASIK procedure works
LASIK is performed while the patient reclines under a surgical device called an excimer laser in an outpatient surgical suite.
First, the eye is numbed with a few drops of topical anesthetic. An eyelid holder is placed between the eyelids to keep them open and prevent the patient from blinking. A suction ring placed on the eye lifts and flattens the cornea and helps keep the eye from moving. The patient may feel pressure from the eyelid holder and suction ring, similar to a finger pressed firmly on the eyelid.
From the time the suction ring is put on the eye until it is removed, vision appears dim or goes black. Once the cornea is flattened, a hinged flap of corneal tissue is created using an automated microsurgical device, either a laser or blade. This corneal flap is lifted and folded back. Then the excimer laser preprogrammed with the patient’s unique eye measurements is centered above the eye.
The surgeon checks that the laser is positioned correctly. The patient looks at a special pinpoint light, called a fixation or target light, while the excimer laser sculpts the corneal tissue. Then the surgeon places the flap back into position and smoothes the edges. The corneal flap sticks to the underlying corneal tissue within two to five minutes, and stitches are not needed.
The patient should plan to have someone drive him or her home after the procedure and then take a nap or just relax. To help protect the cornea as it heals, the surgeon may place a transparent shield over the eye(s) to protect against accidental bumps and to remind the patient not to rub the eye(s). The patient may need to wear the shield only when sleeping. The surgeon will provide eyedrops to help the eye heal and relieve dryness.
It may take three to six months after LASIK surgery for the improvements in a person’s vision to fully stabilize and any side effects to go away.
LASIK risks and side effects
LASIK, like any surgery, has potential risks and complications that should be carefully considered. Since it was approved by the FDA in 1998, LASIK is has become a popular treatment in the United States and the overall complication rate is low. Infection and inflammation are possibilities, as with any surgical procedure, and usually can be cleared up with medications.
Problems with the corneal flap after surgery sometimes make further treatment necessary. There is a chance, though small, that vision will not be as good after the surgery as before, even with glasses or contacts 34.
Some people experience side effects after LASIK that usually disappear over time. These side effects may include hazy or blurry vision; difficulty with night vision and/or driving at night; scratchiness, dryness and other symptoms of the condition called “dry eye”; glare, halos or starbursts around lights; light sensitivity; discomfort or pain; or small pink or red patches on the white of the eye. In a small minority of patients, some of these effects may be permanent 34.
Sometimes a second surgery, called a retreatment or enhancement, may be needed to achieve the desired vision correction. This is more likely for people who were more nearsighted, farsighted, or had higher astigmatism before LASIK — those whose vision originally needed more intensive correction. Approximately 10.5 percent of LASIK patients in the United States require a retreatment.
Considering LASIK ?
Before choosing to have LASIK, it’s important to do your homework to ensure you are a good candidate, understand the potential risks and benefits, and have realistic expectations about what your vision will be like after surgery and for years to come. To ensure the best possible outcome, be a well-prepared and informed patient by reviewing the resources below before you have LASIK. If these materials raise any questions for you, be sure to discuss these questions with your ophthalmologist.
Questions to ask before LASIK surgery
Here are recommended questions to help you and your ophthalmologist decide whether you have a reasonable chance of success and satisfaction with LASIK and if you are willing to accept the unknowns that are part of any medical procedure.
- Is my refractive error within the approved range? LASIK is approved by the FDA to treat certain degrees of nearsightedness, farsightedness and certain types and degrees of astigmatism, alone or in combination with near- or farsightedness. In general, severe refractive error reduces the chance of success and increases the chance that retreatment may be needed.
- Is this the optimal age and life-stage for me to have LASIK? Eyes and visual acuity fluctuate up to about age 25, during pregnancy, breastfeeding or menopause, and after age 40-45 (when presbyopia and other aging eye changes may begin).
- Have my eyes been relatively stable for the last year or so, as confirmed by my contact lens or glasses prescription?
- Are my current (and near future) lifestyle choices, including work, family life and sports/recreation, compatible with LASIK?
- What results can I reasonably expect? What might be the best and worst case scenarios?
- Please describe “LASIK 20/20 and 20/40 vision” and how these might compare with my current corrected vision correction (glasses or contact lenses.)
- If LASIK results do not meet our goals, what might be involved in retreatment?
- About how long does it take for eyes to recover and adjust after LASIK? What kinds of adjustments at work or home might I need to make during this time?
- If I experience any undesirable side effects, about how long might it be before these resolve, and how might they be treated?
- Would any of the medications I’m taking, either prescription or over-the-counter, rule out LASIK or affect the results?
- Do I have other general health or eye conditions that might rule out LASIK or need to be treated and resolved before the procedure? (Health conditions include: diabetes, autoimmune diseases, immunodeficiency states; eye conditions include: dry eye, uveitis and other eye inflammations, eye injuries or previous surgeries, keratoconus, corneal scarring, cataract, glaucoma, retinal disease, ocular herpes.)
- What are the costs of LASIK and of potential related treatments (such as minor side effects or retreatment)?
EpiLasik
A special microkeratome, the Epi-keratome, is used to precisely separate a very thin sheet of epithelial tissue from the cornea. This thin sheet is lifted to the side and the cornea is treated as with PRK. Then the thin sheet may be moved back into place to re-adhere to the cornea or removed. A “bandage” soft contact lens is applied and used for about four days to help the epithelial layer heal.
Wavefront-Guided LASIK
Before surgery, the excimer laser is programmed with each patient’s wavefront data to prepare it to perform a very precise “sculpting” of each unique cornea. In conventional LASIK, this programming is based on the patient’s vision correction prescription (the same as used for the patient’s glasses or contacts.)
In wavefront-guided LASIK, computer imaging technology creates a very detailed three-dimensional “map” of the patient’s cornea that looks a bit like a miniature mountain range 35. This “map” is used to program the excimer laser for surgery. Wavefront technology can measure very subtle abnormalities in the surface of the cornea, enabling wavefront-guided LASIK to achieve vision correction beyond what is possible with glasses or conventional LASIK.
Also, wavefront LASIK has been shown in several studies to reduce side effects, such as problems with night vision and contrast sensitivity (the ability to clearly see objects against a background, such as black letters on a white page), and also to increase the percentage of patients who achieve 20/20 vision. Wavefront technology may also be used in Photorefractive Keratectomy (PRK Surgery) procedures, for similar reasons and with similar results 35.
Photorefractive Keratectomy (PRK Surgery)
Photorefractive keratectomy (PRK) uses the excimer laser in the same way as LASIK, and patients’ vision correction results are similar. The main difference between PRK and LASIK is that in PRK there is no flap — only the very top (epithelial) layer of the cornea is removed (or moved aside) before the excimer laser sculpts the cornea 35.
Many photorefractive keratectomy (PRK) surgeons use a blunt, gently vibrating microkeratome to remove the epithelial layer. LASEK and Epi-LASIK, described below, are other PRK techniques. New approaches, such as advanced surface ablation in which the cornea is cooled either before or after surgery, help reduce the discomfort that may occur after PRK. The patient may also be given topical antibiotics and anti-inflammatory medications and oral pain medications to reduce discomfort and speed healing after surgery. A “bandage” soft contact lens is used to promote epithelial healing, which takes about four days.
While LASIK patients often report clear, improved vision by the day after surgery, it may be a few days before vision stabilizes for PRK patients. The cornea’s epithelial layer re-grows during this time. The thicker corneal flap created in LASIK is not made in PRK, so if there is a concern about potential flap complications, the surgeon may recommend PRK. If the patient’s corneas are too thin to meet LASIK standards, if he or she had LASIK previously, or if other eye health factors are involved, the surgeon and patient may decide that PRK would be a better choice.
Wavefront-guided PRK offers additional vision correction, similar to wavefront-guided LASIK 35. Though thousands of wavefront-guided PRK procedures have been safely and effectively performed in the United States, the FDA approval process has not yet taken place, so wavefront-guided PRK is considered an “off-label” use of the technology 35. Professional medical standards permit Eye M.D.s to use this and other “off-label” procedures and medications.
LASEK surgery
LASEK (laser epithelial keratomileusis) is a laser refractive procedure to correct nearsightedness, farsightedness and astigmatism. LASEK is sometimes referred to as “Epi-LASEK.” During this procedure, the surgeon:
- Removes the top layer of the cornea as a flap-like (or epithelial) sheet before re-sculpting the cornea with the excimer laser.
- Replaces the flap-like sheet on the surface of the eye.
- Inserts a soft contact lens for a few days following the surgery.
What Is the Difference Between LASIK and LASEK ?
In the LASIK procedure, the surgeon uses an instrument called a microkeratome to create a protective flap of tissue. LASEK also involves the creation of a protective epithelial flap, but without the microkeratome. Instead, the surgeon loosens the tissue with a microsurgical instrument called a trephine to create a flap of epithelial corneal tissue, and an alcohol solution is used to loosen the epithelial cells. Once the epithelial flap is created and moved aside, the procedure is the same as PRK. After corneal sculpting, the epithelial flap is repositioned and smoothed with a small spatula, then secured with a “bandage” soft contact lens to promote epithelial healing, which takes about four days 35.
Why Have LASEK Over LASIK ?
LASEK is a great option for patients previously turned down for LASIK because of thin or unusually shaped corneas. It is also an option for patients who are uncomfortable with the microkeratome or flap in general.
Conductive Keratoplasty (CK)
Conductive Keratoplasty (CK) is a noninvasive, thermal refractive surgery procedure used to correct mild to moderate farsightedness (hyperopia) in people over age 40 35. With Conductive Keratoplasty (CK), your Eye M.D. uses a tiny probe that releases controlled amounts of radio frequency energy, instead of a laser, to apply heat to the peripheral portion of the cornea. The heat then causes the peripheral cornea to shrink and tighten like a belt. This increases the curvature (steepness) of the central cornea, improving the optical power of the central cornea. This refocuses light rays on the retina and enhances vision.
Conductive Keratoplasty (CK) can be used to achieve “monovision” (blended vision). With monovision, Conductive Keratoplasty (CK) can be used to improve close-up vision in a presbyopic eye with good vision but poor near focus. To maintain good distance vision, usually only one eye is set to near focus (the non-dominant eye), while the other is left or set at good distance vision. Conductive Keratoplasty (CK) does not offer permanent correction; for some people, farsightedness may return over time.
Phakic Intraocular Lenses (IOLs)
Phakic Intraocular Lenses (IOLs) are designed for people with high degrees of refractive errors that cannot be safely corrected with corneal-based refractive surgery. The phakic IOL, sometimes referred to as an implantable contact lens, or ICL, is surgically implanted inside the eye in front of the eye’s natural lens. The eye’s natural lens is not removed, so patients can retain their pre-existing ability to focus 35.
During the phakic IOL procedure, your Eye M.D. places the phakic IOL either in front of or behind the iris of the eye. Once the IOL is properly positioned inside the eye, it provides the necessary correction to redirect light rays precisely onto the retina.
Refractive Lens Exchange (Clear Lens Extraction)
With refractive lens exchange (RLE) — also called Clear Lens Extraction or CLE — an artificial lens is used to replace your eye’s natural lens in order to improve vision. The procedure is performed much like cataract surgery 35.
As is an option in cataract surgery, RLE may employ multifocal or accommodative intraocular lenses (IOLs). These lenses allow the ability to focus at all distances.
Some people who have early stage cataracts may choose to have RLE instead of waiting for their cataracts to progress to the point where they should be removed. This is because the lens implants generally provide them with better uncorrected vision at that point, particularly if they currently need vision correction.
RLE may also be an option for people with severe hyperopia (farsightedness), for whom LASIK is not recommended.
RLE is not FDA-approved, however, ophthalmologists legally may choose to perform this procedure in what is called an “off-label” use.
References- American Academy of Ophthalmology. What Is Astigmatism ? https://www.aao.org/eye-health/diseases/what-is-astigmatism
- The National Eye Institute, the National Institutes of Health. Facts About Astigmatism. https://www.nei.nih.gov/health/errors/astigmatism
- Online Mendelian Inheritance in Man (OMIM). ASTIGMATISM. http://www.omim.org/entry/603047?search=astigmatism&highlight=astigmatism
- The National Eye Institute, the National Institutes of Health. Facts About the Cornea and Corneal Disease. https://nei.nih.gov/health/cornealdisease/
- McKean-Cowdin, Roberta et al. Risk Factors for Astigmatism in Preschool Children. Ophthalmology , Volume 118 , Issue 10 , 1974 – 1981. http://www.aaojournal.org/article/S0161-6420(11)00610-5/fulltext
- Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447–468. http://www.cell.com/neuron/fulltext/S0896-6273(04)00493-3
- Straub M. Über die Aetiologie der Brechungsanomalien des Auges und den Ursprung der Emmetropie. Graefes Arch Ophthalmol. 1909;70:130–199.
- Ehrlich DL, Braddick OJ, Atkinson J, Anker S, Weeks F, Hartley T, et al. Infant emmetropization: longitudinal changes in refraction components from nine to twenty months of age. Optom Vis Sci. 1997;74:822–843. https://www.ncbi.nlm.nih.gov/pubmed/9383797
- Mohindra I, Held R. Refraction in humans from birth to five years. Doc Ophthalmol Proc Series. 1981;28:19–27.
- Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, et al. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005;46:3074–3080. https://www.ncbi.nlm.nih.gov/pubmed/16123404
- Incidence and Progression of Astigmatism in Singaporean Children. Investigative Ophthalmology & Visual Science November 2004, Vol.45, 3914-3918. doi:10.1167/iovs.04-0492 http://iovs.arvojournals.org/article.aspx?articleid=2124328
- wiazda J, Grice K, Held R, McLellan J, Thorn F. Astigmatism and the development of myopia in children. Vision Res. 2000;40:1019–1026. https://www.ncbi.nlm.nih.gov/pubmed/10720671
- Tong L, Saw SM, Carkeet A, et al. Prevalence rates and epidemiological risk factors for astigmatism in Singapore school children. Optom Vis Sci. 2002;79:606–613. https://www.ncbi.nlm.nih.gov/pubmed/12322931
- Curtin, B.J. The Myopias. Harper and Row, Philadelphia; 1985
- Gentle A, McBrien NA. Modulation of scleral DNA synthesis in development of and recovery from induced axial myopia in the tree shrew. Exp Eye Res. 1999 Feb;68(2):155-63. https://www.ncbi.nlm.nih.gov/pubmed/10068481
- Nickla DLCompensation for spectacle lenses involves changes in proteoglycan synthesis in both the sclera and choroid., Wildsoet C, Wallman J. Curr Eye Res. 1997 Apr;16(4):320-6. https://www.ncbi.nlm.nih.gov/pubmed/9134320
- Wildsoet C, Wallman J. Choroidal and scleral mechanisms of compensation for spectacle lenses in chicks. Vision Res. 1995 May;35(9):1175-94. https://www.ncbi.nlm.nih.gov/pubmed/7610579
- Hung LF, Wallman J, Smith EL 3rd. Vision-dependent changes in the choroidal thickness of macaque monkeys. Invest Ophthalmol Vis Sci. 2000 May;41(6):1259-69. https://www.ncbi.nlm.nih.gov/pubmed/10798639
- Diether S, Schaeffel F. Local changes in eye growth induced by imposed local refractive error despite active accommodation. Vision Res. 1997 Mar;37(6):659-68. https://www.ncbi.nlm.nih.gov/pubmed/9156210
- Wallman, Josh et al. Homeostasis of Eye Growth and the Question of Myopia. Neuron , Volume 43 , Issue 4 , 447 – 468. http://www.cell.com/neuron/fulltext/S0896-6273(04)00493-3
- Clementi, Maurizio et al.Inheritance of Astigmatism: Evidence for a Major Autosomal Dominant Locus. The American Journal of Human Genetics , Volume 63 , Issue 3 , 825 – 830. http://www.cell.com/ajhg/fulltext/S0002-9297(07)61385-8
- Howland, HC and Sayle, N. Photokeratometric and photorefractive measurements of astigmatism in infants and young children. Vis Res. 1985; 25: 73–81. https://www.ncbi.nlm.nih.gov/pubmed/3984220
- Saunders, KJ. Early refractive development in humans. Surv Ophthalmol. 1995; 40: 207–216. http://www.surveyophthalmol.com/article/S0039-6257(95)80027-1/pdf
- American Academy of Ophthalmology. What Causes Astigmatism ? https://www.aao.org/eye-health/diseases/astigmatism-causes
- Mayo Foundation for Medical Education and Research. Symptoms and causes of astigmatism. http://www.mayoclinic.org/diseases-conditions/astigmatism/symptoms-causes/dxc-20253075
- The National Eye Institute, the National Institutes of Health. Facts About Myopia. https://nei.nih.gov/health/errors/myopia
- The National Eye Institute, the National Institutes of Health. Hyperopia. Facts About Hyperopia. https://nei.nih.gov/health/errors/hyperopia
- The National Eye Institute, the National Institutes of Health. Myopia. https://nei.nih.gov/health/myopia
- The National Eye Institute, the National Institutes of Health. Hyperopia. https://nei.nih.gov/health/hyperopia
- The National Eye Institute, National Institutes of Health. Facts About Astigmatism. https://www.nei.nih.gov/health/errors/astigmatism
- American Academy of Ophthalmology. What Do Astigmatism Measurements Mean ? https://www.aao.org/eye-health/diseases/what-do-astigmatism-measurements-mean
- American Academy of Ophthalmology. Astigmatism Treatment. https://www.aao.org/eye-health/diseases/astigmatism-treatment
- American Academy of Ophthalmology. Laser Surgery Recovery. https://www.aao.org/eye-health/treatments/laser-surgery-recovery
- American Academy of Ophthalmology. LASIK — Laser Eye Surgery. https://www.aao.org/eye-health/treatments/lasik
- American Academy of Ophthalmology. Alternative Refractive Surgery Procedures. https://www.aao.org/eye-health/treatments/refractive-surgery-alternative-procedures