Acne necrotica
Acne necrotica miliaris also known as scalp folliculitis or proprionibacterium folliculitis, is an inflammatory disorder of the hair follicles in the scalp. Acne necrotica also known as “acne necrotica varioliformis” or “acne frontalis”, is a more severe form of scalp folliculitis. In acne necrotica, larger follicular spots (papules) become inflamed then develop blackened crusts, finally leaving permanent pox-like scars. Acne necrotica may affect the face, scalp or other areas. Acne necrotica miliaris is an inflammatory reaction to Cutibacterium acnes (formerly Propionibacterium acnes) and in severe cases to Staphylococcus aureus 1. Acne necrotica miliaris or scalp folliculitis is characterized by small, very itchy pustules on the scalp, often most troublesome on the frontal hairline. There may be only a small number of lesions, or they may be very numerous. They are hard to leave alone because of the itch. They often become sore and crusted.
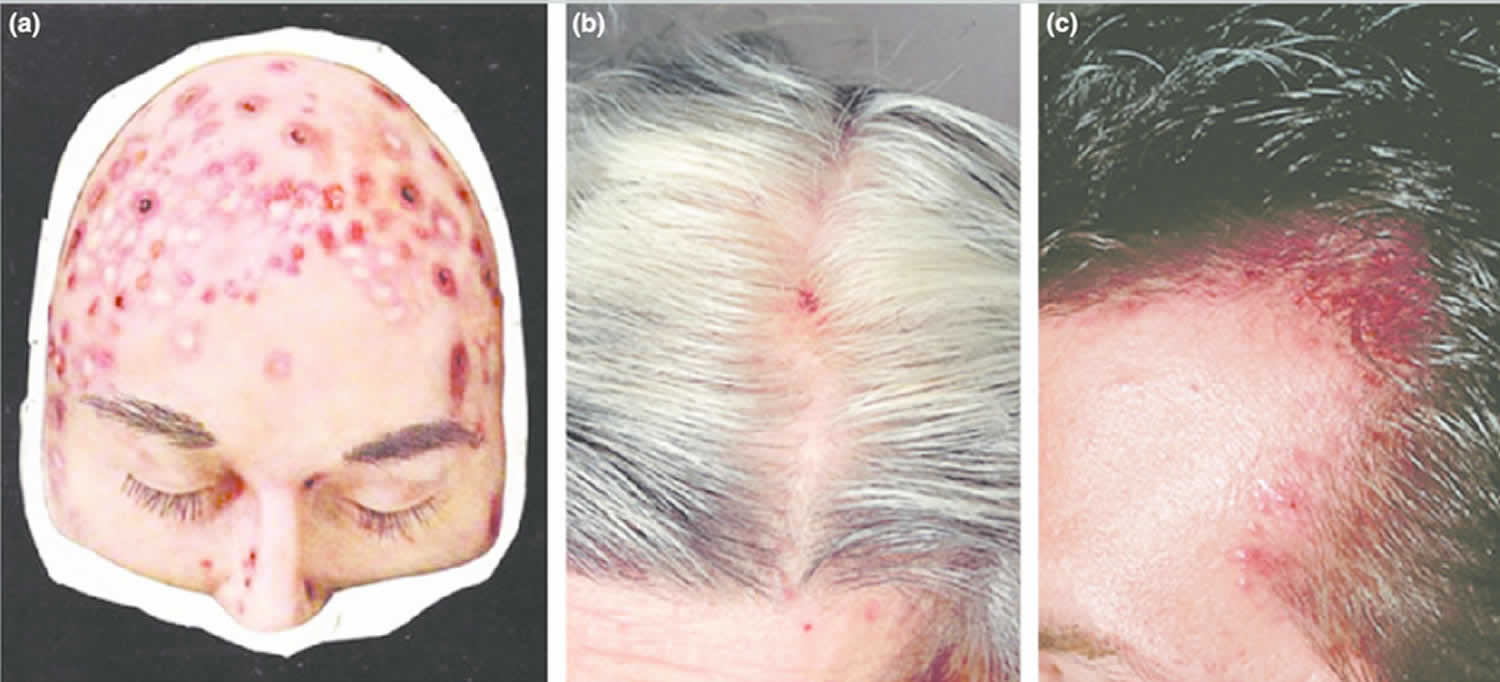
Figure 1. Acne necrotica (acne necrotica varioliformis)
Footnote: (a) Moulage of acne necrotica varioliformis. (b, c) Typical lesions of acne necrotica varioliformis.
[Source 2 ]Acne necrotica causes
The cause of acne necrotica miliaris or scalp folliculitis is not well understood. Acne necrotica miliaris is generally considered to be an inflammatory reaction to components of the hair follicle, particularly the micro-organisms. These include:
- Bacteria (especially Cutibacterium acnes, but in severe cases, also Staphylococcus aureus) 1
- Yeasts (Malassezia species)
- Mites (Demodex folliculorum).
Acne necrotica signs and symptoms
Acne necrotica varioliformis is characterized by crops of follicular lesions, usually involving the parietal scalp and frontal hair line, which heal with scarring. Other areas affected may include the face, eyebrows, neck and chest. The lesions typically comprise edematous, umbilicated papulopustules that undergo central necrosis, crust over and then slowly heal, leaving varioliform scars 2. Most lesions are excoriated and maybe painful or itchy 3.
Acne necrotica diagnosis
Folliculitis is fairly easy to diagnose in most cases. Your physician may wish to perform a bacterial culture in order to determine the cause of the scalp folliculitis. The procedure involves:
- Penetrating the pus-filled lesion with a needle, scalpel, or lancet.
- Rubbing a sterile cotton-tipped applicator across the skin to collect the pus.
- Sending the specimen away to a laboratory.
Typically, the laboratory will have preliminary results within 48–72 hours if there are many bacteria present. However, the culture may take a full week or more to produce final results. In addition to identifying the strain of bacteria that is causing the scalp folliculitis, the laboratory usually performs antibiotic sensitivity testing in order to determine the medications that will be most effective in killing off the bacteria.
Acne necrotica treatment
The scalp affected by folliculitis should be washed with a mild normal shampoo as often as desired. Antidandruff shampoos containing antifungal agents such as ketoconazole or ciclopirox are sometimes helpful. Conditioner can be used if desired.
The following medications may be helpful for acne necrotica scalp:
- Topical antibiotics (eg, fusidic acid gel), clindamycin solution, erythromycin solution
- Mild topical steroid lotions or creams
- Oral antihistamines
- Oral antibiotics, particularly long-term tetracycline
- Oral isotretinoin – long-term low dose treatment may be required.
Depending on bacterial culture results, your physician may recommend the following treatments:
- Prescription-strength antibacterial wash, such as chlorhexidine gluconate
- Topical antibiotic lotion or gel, such as erythromycin or clindamycin
- Oral antibiotic pills, such as cephalexin, erythromycin, or doxycycline
Occasionally, the bacteria causing the infection are resistant to treatment with the usual antibiotics (particularly, methicillin-resistant Staphylococcus aureus or MRSA). This can sometimes cause a more severe form of folliculitis. Depending on the circumstances, your doctor may consider more aggressive treatment that includes prescribing:
- A combination of two different oral antibiotics, including trimethoprim-sulfamethoxazole, clindamycin, amoxicillin, linezolid, or a tetracycline
- A topical medication, mupirocin ointment, to apply to the nostrils
- If your doctor prescribes antibiotics, be sure to take the full course of treatment to avoid allowing the bacteria to develop resistance to the antibiotic prescribed.
- Hay RJ, Adriaans BM. Bacterial Infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s Textbook of Dermatology. 8th ed. Sussex: Wiley Blackwell; 2010. pp. 30.26–65.
- Filbrandt, Rebecca & Rufaut, Nicholas & Jones, Leslie & Sinclair, Rodney. (2013). Primary cicatricial alopecia: Diagnosis and treatment. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 185. 10.1503/cmaj.111570
- Hadshiew IM, Foitzik K, Arck PC et al. Burden of hair loss: stress and the underestimated psychosocial impact of telogen effluvium and androgenetic alopecia. J Invest Dermatol 2004;123:455–7.