Ectopic pacemaker
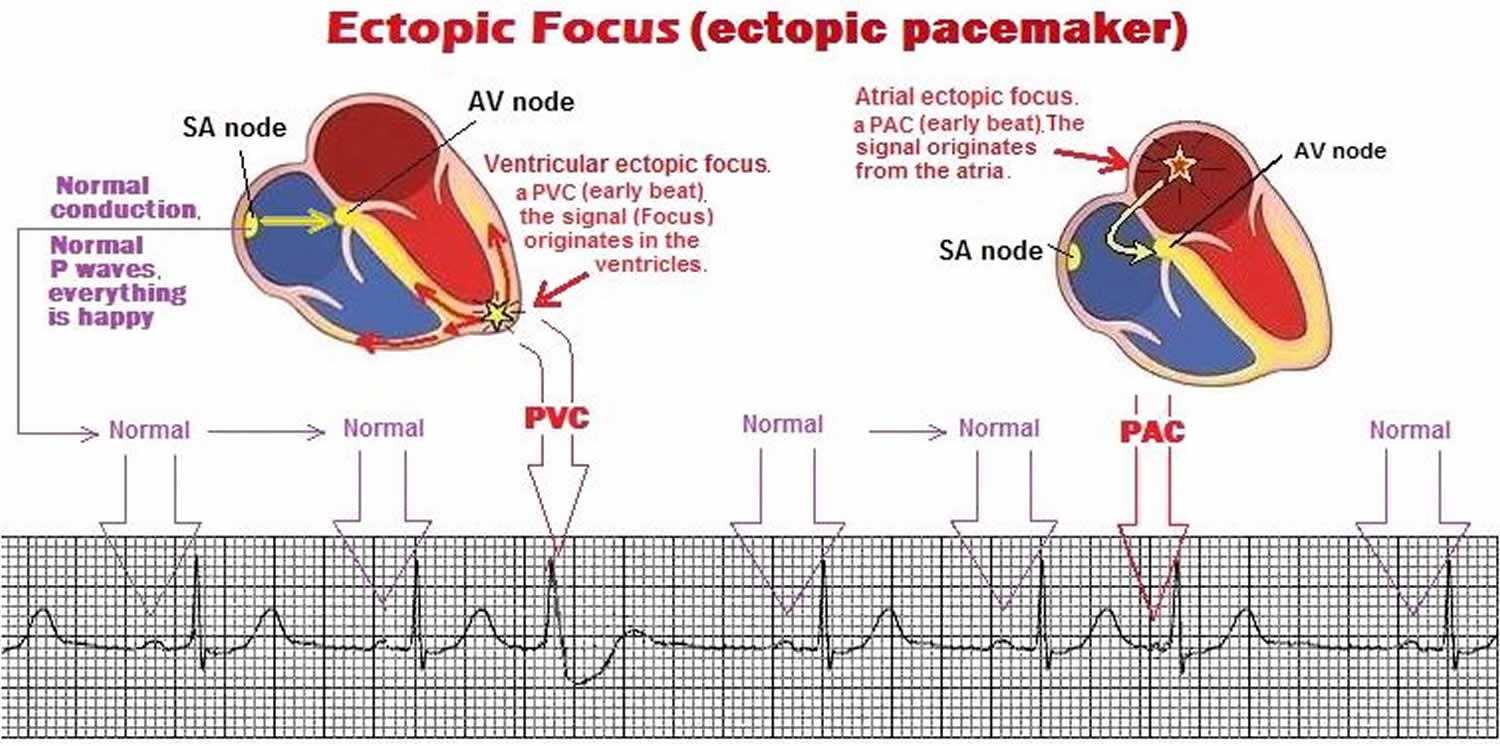
Ectopic pacemaker also known as ectopic focus, are abnormal pacemaker (excitable group of cells) sites within the heart outside of the normally functioning sinoatrial (SA) node that display automaticity and causes a premature heartbeat. Ectopic pacemaker can occur within the atria, junction (the AV nodal area) or from the ventricles. When an electrical signal is generated from this group of cells, it is called ectopic. The term ectopic focus means: ectopic, the electrical signal originates from a different location other than the SA node, and focus, the site where the electrical signal originates from. This ectopic pacemaker can self-generate an electrical signal that can either cause an early beat or can continually pace the heart. Normally the SA node is located at the junction of the crista terminalis in the upper wall of the right atrium and the opening of the superior vena cava 1. Ectopic pacemaker activity, however, is normally suppressed (overdrive suppression) by the higher rate of the SA node. When a ectopic pacemaker drives the rhythm of the heart, the spread of depolarization generally does not follow the normal, fast conducting pathways within the heart. Because of this, the depolarization wave takes longer to spread throughout the myocardium. This typically causes a shape change in QRS complex and prolongs its duration (>0.10 sec) because more time is required for the entire ventricle to become depolarized.
Ectopic pacemaker can cause additional heart beats which is observed as premature beats or take over the normal pacemaker activity of the SA node. These ectopic pacemakers can lead to either tachycardia or bradycardia depending upon their location and surrounding electrical conditions. Typically, an ectopic pacemaker will simply cause an early contraction such as premature atrial contractions (PACs), premature ventricular contractions (PVCs) or premature junctional complexes (PJCs). If ectopic pacemaker paces the heart from the junctional area or ventricles, it is called an escape rhythm, i.e. junctional escape or ventricular escape. If ectopic pacemaker paces from within the atria, it will generate a rhythm such as atrial fibrillation, atrial flutter, wondering atrial pacemaker (WAP) or multifocal atrial tachycardia (MAT). Many times doctors use the term ectopic pacemaker to describe a rhythm having premature atrial contractions (PACs), premature ventricular contractions (PVCs) or premature junctional complexes (PJCs), because they all have an ectopic focal point (ectopic focus). For example, an ectopic foci in the ventricle when coupled with a reentry pathway can precipitate ventricular tachycardia. In third degree AV nodal block, a ventricular rhythm still occurs because of the expression of normally latent ectopic pacemaker sites within the ventricle. These ectopic ventricular pacemakers generally produce a rhythm (30-40 beats/minutes); this resting rate is much slower than that generally produced by the SA node (60-100 beats/min).
Ectopic heartbeats are rare in children without heart disease that was present at birth (congenital). Most extra heartbeats in children are premature atrial contractions (PACs). These are often benign.
In adults, ectopic heartbeats are common. They are most often due to premature atrial contractions (PACs) or premature ventricular contractions (PVCs). Your health care provider should look into the cause when they are frequent. Treatment is directed at symptoms and the underlying cause.
Often, arrhythmias caused by an ectopic pacemaker are innocuous, such as in single atrial or ventricular premature beats (extra systoles) and no therapy is necessary. If ectopic pacemaker give rise to sustained arrhythmias, mapping of the spread of activation during the arrhythmias may detect the abnormal focus and radiofrequency ablation may be the proper cure.
The main function of the SA node is to act as the normal pacemaker of the heart. Any dysfunction of the sinus node can affect the heart’s rate and rhythm 1.
The SA (sinus) node represents a crescent-like shaped cluster of myocytes with pacemaker activity. Under normal circumstances, it generates electrical impulses that set the rhythm and rate of the heart. The sinoatrial (SA) node initiates an action potential that results in an electrical impulse traveling through the heart’s electrical conduction system to cause myocardial contraction. Unlike atrial and ventricular cells, pacemaker cells in the sinus node do not have a resting phase. Instead, these cells have pacemaker potential, in which they begin to depolarize automatically after an action potential ends 2. The mass of the sinus node is too small to create a substantial electrical signal that can be detected on the electrocardiogram (ECG). Instead, SA nodal pacemaker activity must be inferred indirectly from P waves generated by the atrial activity.
Spontaneous beating of the SA node is initiated, sustained, and regulated by a complex system that integrates ion channels and transporters located on the cell membrane surface (often referred to as “membrane clock”) with subcellular calcium handling machinery (by parity of reasoning referred to as an intracellular “Ca-Clock”) 3. Stable, rhythmic beating of the SA node is ensured by a rigorous synchronization between these two clocks highlighted in the coupled-clock system concept of SA node timekeeping 4.
See your doctor if:
- You keep feeling the sensation of your heart pounding or racing (palpitations).
- You have palpitations with chest pain or other symptoms.
- You have this condition and your symptoms get worse or do not improve with treatment.
Is ectopic pacemaker dangerous?
In most cases these extra beats are not life threatening. They do sometimes make people feel anxious, especially during quiet times, when they can be felt more frequently. The symptoms of ectopic beats and anxiety can interfere with work, education and holidays. Rarely, ectopic beats are more serious. Their presence may be a sign that there is a problem with the heart. Additionally, the ectopic beats can cause the heart function to worsen. If this is the case, your doctor will discuss this with you.
What is catheter ablation for ectopic pacemaker and what does it involve?
Catheter ablation is a term that describes the process of modifying the heart muscle so that it no longer transmits electrical signals. The procedure involves passing long fine wires (called catheters) into the heart via the blood vessels. Strong sedatives and local anesthetic are used to make it comfortable and virtually painless. The procedure is performed as a keyhole operation through small punctures in the skin.
The punctures are made in the groin. Once in the heart, the catheter ends are placed in contact with the heart muscle.
The wires are used to seek out the abnormal heart muscle that may be responsible for causing the ectopic beats. The ablation energy (heat or freezing) is applied through the tip of one of the wires onto the abnormal connection for about 30 seconds. Sometimes the connection can be a little resistant to a single application so several energy deliveries may be necessary. Finding the abnormality and then delivering the energy can take anything from 1–4 hours.
How successful is catheter ablation for ectopic pacemaker?
Catheter ablation for ectopic heartbeats is very effective at stopping the extra heartbeats. A successful ablation for ectopic beats depends on the ectopic beats being present at the time of the procedure. If the ectopic beats are very uncommon then it becomes difficult to seek them out with the wires. If the ectopic beats are very infrequent or absent at the time of the procedure then the procedure may be abandoned.
What if I have ectopic beats after my ectopic pacemaker ablation procedure?
You may experience what may feel like the start of palpitations within the first 6 weeks after the ectopic pacemaker ablation procedure. This is normal and does not mean the procedure has not worked. Over the following months this sensation will disappear. The chance of the palpitations returning is low, about 1 in 20 (5%). The ectopic beats return because the abnormal area that has been ablated has healed or because a part was overlooked at the time of the procedure. The ablation procedure can be repeated if the ectopic beats return. The repeat procedure is usually shorter as the doctor will already have a clear knowledge of where the problem is. If your ectopic beats return then you can inform your doctor or your local cardiologist and they will refer you back to us. It would be helpful but not essential to get an ECG whilst you are having symptoms of ectopic beats and to bring it along to the consultation. In the meantime, the medication that you were taking before the procedure to control the ectopic beats can be restarted while you are waiting for the consultation.
Who benefits from having catheter ablation for ectopic pacemaker?
- Individuals who have palpitations caused by ectopic beats.
- Individuals who experience palpitations in those situations where drug therapy has either failed to control the ectopic beats, or where the side effects of those drugs have become undesirable. Catheter ablation can often offer a complete cure for this.
- Individuals who are not keen to take medicines for long periods of time. Catheter ablation can often offer a complete cure for this.
- Individuals who have worsened heart function as a result of the ectopic beats. Often the heart function will improve after catheter ablation.
Ectopic pacemaker causes
Ectopic pacemakers can occur within healthy hearts in response to various stimulating events, such as:
- Elevated sympathetic nervous system input. An important factor tending to exacerbate ectopic pacemakers is the release of norepinephrine from sympathetic nerves. Norepinephrine acts on beta-adrenoceptors in the heart to increase its rate, which strongly increases the tendency for ectopic pacemakers to develop. Beta-adrenoceptor-blocking drugs (e.g., propranolol), commonly known as beta-blockers, are widely used to control these types of arrhythmia because they slow the actions of the heart.
- Overstimulation from drugs such as caffeine 5.
- Changes in the blood, such as a low potassium level (hypokalemia)
- Decrease in blood supply to the heart
- When the heart is enlarged or structurally abnormal
Ectopic beats may be caused or made worse by smoking, alcohol use, caffeine, stimulant medicines, and some street drugs.
Atrial ectopic tachycardia is a rare arrhythmia; however, it is the most common form of incessant supraventricular tachycardia (SVT) in children 6. Atrial ectopic tachycardia is believed to be secondary to increased automaticity of a nonsinus atrial focus or foci. This arrhythmia, which is also known as ectopic atrial tachycardia or automatic atrial tachycardia, has a high association with tachycardia-induced cardiomyopathy. Atrial ectopic tachycardia is often refractory to medical therapy and is not usually responsive to direct current (DC) cardioversion.
Atrial ectopic tachycardia is usually idiopathic. Occasionally, mycoplasmal or viral infections, such as respiratory syncytial virus, may trigger this arrhythmia, although more complex atrial tachycardias, such as chaotic atrial tachycardia, are more frequently found in this scenario. Atrial tumors have been reported to be associated with atrial ectopic tachycardia. Reports of familial cases with an autosomal dominant inheritance are present in the literature 7. This arrhythmia is also observed in patients who have congenital heart disease and have undergone surgical treatment of this congenital heart disease.
The adult form of atrial ectopic tachycardia may have a different cause and natural history than the pediatric form.
Cardiac causes of premature ventricular contractions (PVCs) include the following:
- Acute myocardial infarction or myocardial ischemia
- Myocarditis
- Cardiomyopathy, dilated or hypertrophic 8 – Two consistent predictors of of PVC-induced cardiomyopathy are PVC burden and PVC QRS duration 9
- Myocardial contusion
- Mitral valve prolapse
Other causes of premature ventricular contractions (PVCs) include the following:
- Hypoxia and/or hypercapnia
- Medications (eg, digoxin, sympathomimetics, tricyclic antidepressants, aminophylline, caffeine)
- Illicit substances (eg, cocaine, amphetamines, alcohol, tobacco)
- Hypomagnesemia, hypokalemia, hypercalcemia
Ectopic pacemaker symptoms
Ectopic pacemaker symptoms may include:
- There may be no symptoms
- Feeling your heartbeat (palpitations)
- Feeling like your heart stopped or skipped a beat
- Feeling of occasional, forceful beats
Ectopic pacemaker diagnosis
A physical exam may show an occasional uneven pulse. If the ectopic heartbeats DO NOT occur very often, your doctor may not find them during a physical exam.
Blood pressure is most often normal.
An ECG will be done. Often, no further testing is needed when your ECG is normal and the symptoms are not severe or worrisome.
If your doctor wants to know more about your heart rhythm, they may order:
- A monitor that you wear that records and stores your heart rhythm for 24 to 48 hours (Holter monitor)
- Rhythm monitoring with a loop recorder or device. A recording device that you wear, and records your heart rhythm whenever you feel a skipped beat
- An echocardiogram may be ordered if your doctor suspects problems with the size or structure of your heart are the cause. An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a standard x-ray image. An echocardiogram does not expose you to radiation.
- Intracardiac electrophysiology study (EPS). Intracardiac electrophysiology study (EPS) is a test to look at how well your heart’s electrical signals are working. Wire electrodes are placed in your heart to do this test. These electrodes measure electrical activity in your heart. The procedure is done in a hospital laboratory. The staff will include a cardiologist, technicians, and nurses. To have intracardiac electrophysiology study (EPS):
- Your groin and/or neck area will be cleaned and numbing medicine (anesthetic) will be applied to the skin.
- The cardiologist will then place several IVs (called sheaths) into the groin or neck area. Once these IVs are in place, wires or electrodes can be passed through the sheaths into your body.
- The doctor uses moving x-ray images to guide the catheter into the heart and place the electrodes in the right places.
- The electrodes pick up the heart’s electrical signals.
- Electrical signals from the electrodes may be used to make the heart skip beats or produce an abnormal heart rhythm. This can help the doctor understand more about what is causing the abnormal heart rhythm or where in the heart it is starting.
- You may also be given medicines that may also be used for the same purpose.
- Other procedures that may also be done during the test:
- Placement of a heart pacemaker
- Procedure to destroy small areas in your heart that may be causing your heart rhythm problems (called catheter ablation)
You may also have blood chemistries and other tests.
Ectopic pacemaker treatment
The following may help reduce ectopic heartbeats for some people:
- Limiting caffeine, alcohol, and tobacco
- Regular exercise for people who are inactive
Many ectopic heartbeats are not life threatening although the symptoms can feel intense and interfere with everyday activities and do not need to be treated. In rare cases the ectopic beats can be dangerous. If your ectopic beats are dangerous your cardiologist will advise you of this. It is up to you to decide what treatment you want. Your cardiologist will have discussed the following alternative treatments with you:
- Taking prescribed drugs continually to prevent the extra beats. These may have side effects, may not work and may need to be taken life-long.
- If ectopic pacemaker give rise to sustained arrhythmias, mapping of the spread of activation during the arrhythmias may detect the abnormal focus and radiofrequency ablation may be the proper cure.
- Dealing with the symptoms as and when they appear by trying to ignore them or seeking psychological help, such as behavior therapy, to learn to cope with the symptoms
- Using alternative therapies, for example aromatherapy, acupuncture or homeopathy. Your cardiologist will not be able to talk to you in detail about these methods and this kind of therapy will not prevent ectopic beats from occurring
Ectopic pacemaker prognosis
In some cases, ectopic heartbeats may mean you are at greater risk for serious abnormal heart rhythms, such as ventricular tachycardia.
Ventricular tachycardia (VT) is a rapid heartbeat that starts in the lower chambers of the heart (ventricles). Ventricular tachycardia is a pulse rate of more than 100 beats per minute, with at least 3 irregular heartbeats in a row.
You may have symptoms if the heart rate during a ventricular tachycardia (VT) episode is very fast or lasts longer than a few seconds. Symptoms may include:
- Chest discomfort (angina)
- Fainting (syncope)
- Lightheadedness or dizziness
- Sensation of feeling the heart beat (palpitations)
- Shortness of breath
Symptoms may start and stop suddenly. In some cases, there are no symptoms.
Ventricular tachycardia (VT) treatment depends on the symptoms, and the type of heart disorder.
If someone with VT is in distress, they may require:
- CPR
- Cardioversion (electric shock)
- Medicines (such as lidocaine, procainamide, sotalol, or amiodarone) given through a vein
After an episode of VT, steps are taken to further episodes.
- Medicines taken by mouth may be needed for long-term treatment. However, these drugs may have severe side effects. They are being used less often as other treatments are developed.
- A procedure to destroy the heart tissue that is causing the abnormal heartbeat (called ablation) may be done.
- An implantable cardioverter defibrillator (ICD) may be recommended. It is an implanted device that detects any life-threatening, rapid heartbeat. This abnormal heartbeat is called an arrhythmia. If it occurs, the ICD quickly sends an electrical shock to the heart to change the rhythm back to normal. This is called defibrillation.
- Kashou AH, Basit H, Chhabra L. Physiology, Sinoatrial Node (SA Node) [Updated 2020 Aug 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459238
- Vetulli HM, Elizari MV, Naccarelli GV, Gonzalez MD. Cardiac automaticity: basic concepts and clinical observations. J Interv Card Electrophysiol. 2018 Aug;52(3):263-270.
- Lakatta E. G., Maltsev V. A., Vinogradova T. M. (2010). A coupled SYSTEM of intracellular Ca2+ clocks and surface membrane voltage clocks controls the timekeeping mechanism of the heart’s pacemaker. Circ. Res. 106 659–673. 10.1161/CIRCRESAHA.109.206078
- Lang D, Glukhov AV. Functional Microdomains in Heart’s Pacemaker: A Step Beyond Classical Electrophysiology and Remodeling. Front Physiol. 2018;9:1686. Published 2018 Nov 27. doi:10.3389/fphys.2018.01686 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6277479
- Carol, Mattson, Port. Pathophysiology: Concepts of Altered Health States 7th Ed, Pg 588. Lippincott Williams & Wilkins, 2005. ISBN 0-7817-4988-3
- Pediatric Atrial Ectopic Tachycardia. https://emedicine.medscape.com/article/898784-overview
- Dagres N, Gutersohn A, Wieneke H, Sack S, Erbel R. A new hereditary form of ectopic atrial tachycardia with autosomal dominant inheritance. Int J Cardiol. 2004 Feb. 93(2-3):311-3.
- Cha YM, Lee GK, Klarich KW, Grogan M. Premature ventricular contraction-induced cardiomyopathy: a treatable condition. Circ Arrhythm Electrophysiol. 2012 Feb 1. 5(1):229-36.
- Lee AK, Deyell MW. Premature ventricular contraction-induced cardiomyopathy. Curr Opin Cardiol. 2016 Jan. 31 (1):1-10.