What is analgesic
Analgesic refers to the classes of drugs that includes most “painkillers” or “pain relievers” — that reduce or relieve headaches, sore muscles, arthritis, or other aches and pains. The word analgesic is derived from ancient Greek and means to reduce or stop pain. There are many different analgesics, and each one has advantages and risks. Some types of pain respond better to certain pain medicines than others. Each person may also have a slightly different response to a pain reliever. Analgesic includes classes of non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen as well as acetaminophen (paracetamol) and opioids. Nonprescription or over-the-counter analgesic drugs (e.g. aspirin, ibuprofen, acetaminophen) are generally used for mild to moderate pain. Prescription analgesic medications such as opioid pain relievers, sold through a pharmacy under the direction of a physician, are used for moderate to severe pain.
Over-the-counter (OTC) analgesics are good for many types of pain. There are two main types of over-the-counter (OTC) pain medicines: acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs). Aspirin, naproxen (Aleve), and ibuprofen (Advil, Motrin) are examples of over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs).
Over-the-counter (OTC) analgesics can be helpful in treating many types of pain. These can include headaches, arthritis pain, earaches, back pain, and pain after surgery. They can also treat pain from the flu or a cold, sinusitis, or a sore throat. In some cases, a specific type of pain reliever does a better job helping a specific kind of pain.
For most people, over-the-counter (OTC) analgesics are all they need to relieve pain or reduce fever. If an over-the-counter (OTC) analgesic doesn’t help your pain or fever, it may be a sign you have a more serious problem. You could need a prescription medicine.
If over-the-counter medicines don’t relieve your pain, your doctor may prescribe something stronger. Many nonsteroidal anti-inflammatory drugs (NSAIDs) are also available at higher prescription doses. The most powerful analgesics are opioids (narcotics). Opioids are very effective, but they can sometimes have serious side effects. There is also a risk of addiction. Because of the risks, you must use them only under a doctor’s supervision.
There are many things you can do to help ease pain. Pain relievers are just one part of a pain treatment plan.
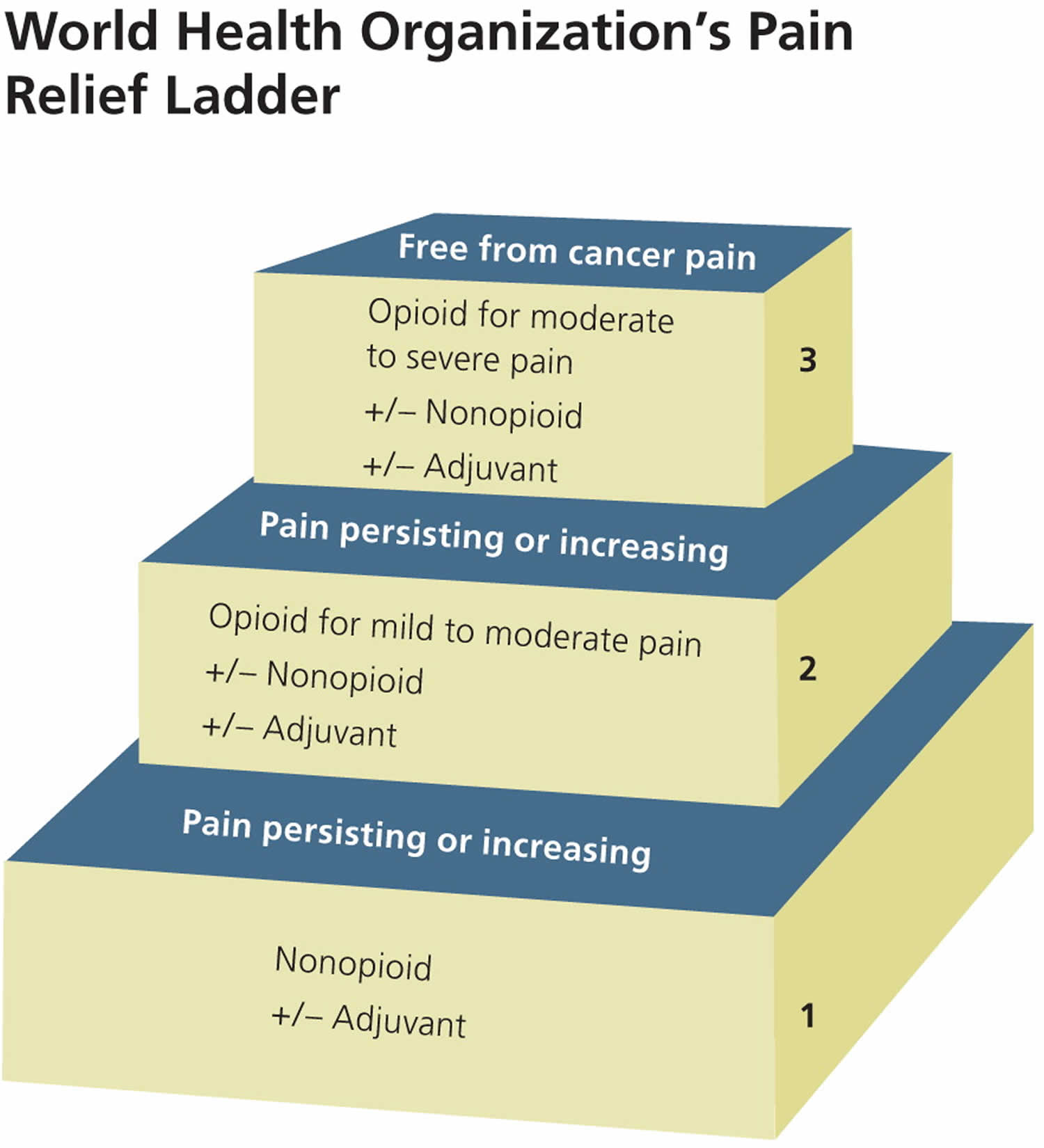
The World Health Organization’s (WHO’s) pain relief ladder (Figure 1) provides a stepped approach to the management of cancer pain and can also be used for patients with acute and chronic nonmalignant pain.5 Adjuvant medications can be initiated as needed at any step of the ladder 1. These medications include antidepressants (e.g., tricyclics for acute neuropathic pain), anticonvulsants (e.g., gabapentin [Neurontin]), and glucocorticoids (e.g., dexamethasone to reduce postoperative pain, nausea, and vomiting). The analgesic effectiveness increases with each step up on the ladder, as does the potential for medication abuse or addiction. Table 1 summarizes medications used to treat acute pain in adults 2.
Figure 1. Stepped approach to pain management
[Source 3 ]Table 1. STEPS for Medications to Treat Acute Pain in Adults
| Medication class | Safety | Tolerability | Effectiveness* | Price of generic (brand) | Simplicity | Comments | |
|---|---|---|---|---|---|---|---|
Acetaminophen |
|
| + |
|
|
| |
Aspirin |
|
| ++ |
|
|
| |
Nonselective NSAIDs (e.g., ibuprofen) |
|
| ++ |
|
|
| |
Cyclooxygenase-2 selective NSAIDs (e.g., celecoxib [Celebrex]) |
|
| ++ |
|
|
| |
Opioid combinations (e.g., hydrocodone/acetaminophen) |
|
| +++ |
|
|
| |
Opioid (e.g., morphine) |
|
| +++ |
|
|
| |
Dual-action opioids (e.g., tapentadol [Nucynta]) |
|
| +++ |
|
|
| |
FDA = U.S. Food and Drug Administration; GI = gastrointestinal; NA = not available; NSAID = nonsteroidal anti-inflammatory drug.
*—Based on information from Cochrane reviews regarding number needed to treat to produce 50% pain reduction at 4 to 6 hours (when available)
Types of analgesics
Over-the-counter (OTC) Medications
These relieve the minor aches and pains associated with conditions such as headaches, fever, colds, flu, arthritis, toothaches, and menstrual cramps.
There are basically two types of over-the-counter (OTC) pain relievers: acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs).
Acetaminophen is an active ingredient found in more than 600 OTC and prescription medicines, including pain relievers, cough suppressants, and cold medications.
Non-steroidal anti-inflammatory drugs (NSAIDs) are common medications used to relieve fever and minor aches and pains. They include aspirin, naproxen, and ibuprofen, as well as many medicines taken for colds, sinus pressure, and allergies. They act by inhibiting an enzyme that helps make a specific chemical.
Prescription Medications
Typical prescription pain relief medicines include opioids and non-opioid medications.
Derived from opium, opioid drugs are very powerful products. They act by attaching to a specific “receptor” in the brain, spinal cord, and gastrointestinal tract. Opioids can change the way a person experiences pain.
Types of prescription opioid medications include:
- morphine, which is often used before and after surgical procedures to alleviate severe pain
- oxycodone, which is also often prescribed for moderate to severe pain
- codeine, which comes in combination with acetaminophen or other non-opioid pain relief medications and is often prescribed for mild to moderate pain
- hydrocodone, which comes in combination with acetaminophen or other non-opioid pain relief medications and is prescribed for moderate to moderately severe pain
FDA has recently notified makers of certain opioid drugs that these products will need to have a Risk Evaluation and Mitigation Strategy (REMS) to ensure that the benefits continue to outweigh the risks.
Affected opioid drugs, which include brand name and generic products, are formulated with the active ingredients fentanyl, hydromorphone, methadone, morphine, oxycodone, and oxymorphone.
What is pain?
The International Association for the Study of Pain 4 defines it as: “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” The International Association for the Study of Pain 4 definition means that pain is a subjective experience; one that cannot be objectively measured and depends on the person’s self-report. There can be a wide variability in how a person experiences pain to a given stimulus or injury.
Pain can be classified as acute or chronic, and the two kinds differ greatly:
- Acute pain, for the most part, results from disease, inflammation, or injury to tissues. This type of pain generally comes on suddenly, for example, after trauma or surgery, and may be accompanied by anxiety or emotional distress. The cause of acute pain can usually be diagnosed and treated. The pain is self-limiting, which means it is confined to a given period of time and severity. It can become chronic.
- Chronic pain is now believed to be a chronic disease condition in the same manner as diabetes and asthma. Chronic pain can be made worse by environmental and psychological factors. By its nature, chronic pain persists over a long period of time and is resistant to many medical treatments. It can—and often does—cause severe problems. People with chronic pain often suffer from more than one painful condition. It is thought that there are common mechanisms that put some people at higher risk to develop multiple pain disorders. It is not known whether these disorders share a common cause.
You may experience pain as a prick, tingle, sting, burn, or ache. Normally, acute pain is a protective response to tissue damage resulting from injury, disease, overuse, or environmental stressors. To sense pain, specialized receptors (called nociceptors) which are found throughout the body, trigger a series of events in response to a noxious (painful) stimulus. The events begin with conversion of the stimulus to an electrical impulse that travels through nerves from the site of injury or disease process to the spinal cord. These signals are transmitted to a specialized part of the spinal cord called the dorsal horn, where they can be dampened or amplified before being relayed to the brain.
Pain disorders
Hundreds of pain syndromes or disorders make up the spectrum of pain. There are the most benign, fleeting sensations of pain, such as a pin prick. There is the pain of childbirth, the pain of a heart attack, and the pain that sometimes follows amputation of a limb. There is also pain accompanying cancer and the pain that follows severe trauma, such as that associated with head and spinal cord injuries. A sampling of common pain syndromes follows, listed alphabetically.
Arachnoiditis
- Arachnoiditis is a condition in which one of the three membranes covering the brain and spinal cord, called the arachnoid membrane, becomes inflamed. A number of causes, including infection, chemical irritation, or trauma, can result in inflammation of this membrane. Arachnoiditis can produce disabling, progressive, and even permanent pain.
Arthritis
- Millions of Americans suffer from arthritic conditions such as osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and gout. These disorders are characterized by joint pain in the extremities. Many other inflammatory diseases affect the body’s soft tissues, including tendonitis and bursitis.
Back pain
- Back pain has become the high price paid by our modern lifestyle and is a startlingly common cause of disability for many Americans, including both active and inactive people. Back pain that spreads to the leg is called sciatica and is a very common condition (see below). Another common type of back pain is associated with the discs of the spine, the soft, spongy padding between the vertebrae (bones) that form the spine. Discs protect the spine by absorbing shock, but they tend to degenerate over time and may sometimes rupture. Of note, as people age, discs tend to normally lose elasticity and degenerate. This process, by itself, is not necessarily associated with pain. Spondylolisthesis occurs when one vertebra extends over another and may result in pressure on nerve roots and therefore pain. It also may cause damage to nerve roots so called radiculopathy, which can be extremely painful and can be associated with weakness or numbness due to nerve compression. Treatment for a damaged disc includes drugs such as painkillers, muscle relaxants, and steroids (administered orally or via epidural); exercise or rest, depending on the patient’s condition; adequate support, such as a brace or better mattress; and physical therapy. In some cases, surgery may be required to remove the damaged portion of the disc, especially when it is pressing a nerve root. However, surgery cannot return the disc to its original condition, it can only relieve the pressure on the nerve root. Surgical procedures include discectomy, laminectomy, or spinal fusion.
Burn pain
- Burn pain (pain that is caused by burns) can be profound and poses an extreme challenge to the medical community. Depending on the injury, pain accompanying burns can be excruciating, and even after the wound has healed people may have chronic pain at the burn site.
Cancer pain
- Cancer pain can accompany the growth of a tumor, the treatment of cancer, or chronic problems related to cancer’s permanent effects on the body. Fortunately, most cancer pain can be treated to help reduce discomfort and stress.
Central pain syndrome
- Some individuals who have had an injury to the spinal cord experience intense pain ranging from tingling to burning and, commonly, both. Such persons are sensitive to hot and cold temperatures and touch. For these individuals, a touch can be perceived as intense burning, indicating abnormal signals relayed to and from the brain. This condition is called central pain syndrome or, if the damage is in the thalamus (the brain’s center for processing bodily sensations), thalamic pain syndrome. Central pain syndromes affect as many as 100,000 Americans with disorders such as multiple sclerosis, Parkinson’s disease, amputated limbs, spinal cord injuries, and stroke. Their pain may be severe and is extremely difficult to treat effectively. A variety of medications, including analgesics, antidepressants, anticonvulsants, and electrical stimulation, are options available to people with central pain.
Complex regional pain syndrome
- Complex regional pain syndrome is accompanied by burning pain and hypersensitivity to temperature. Often triggered by trauma or nerve damage, complex regional pain syndrome causes the skin of the affected area to become characteristically shiny and the limb swollen. In the past, complex regional pain syndrome was often called reflex sympathetic dystrophy syndrome or causalgia.
Fibromyalgia
- Fibromyalgia affects millions of Americans, more often women than men. It is a disorder characterized by fatigue, sleep disturbances, stiffness, tender points, joint tenderness, and widespread muscle pain.
Headaches
Headaches affect millions of Americans. The three most common types of chronic headache are migraines, cluster headaches, and tension headaches. Each comes with its own telltale brand of pain.
- Migraines are characterized by throbbing head pain, sensitivity to light and sound, and sometimes by other symptoms, such as nausea, dizziness, and visual disturbances that begine before the headache. Migraines are more frequent in women than men. Stress can trigger a migraine headache, and migraines only very rarely put the sufferer at risk for stroke.
- Cluster headaches are characterized by excruciating, piercing pain on one side of the head and eye; they occur more frequently in men than women.
- Tension headaches are often described as a tight band around the head.
Head and facial pain
- Head and facial pain can be agonizing, whether it results from dental problems or from disorders such as cranial neuralgia, in which one of the nerves in the face, head, or neck is inflamed. Another condition, trigeminal neuralgia (also called tic douloureux), affects the largest of the cranial nerves and is characterized by a stabbing, shooting pain.
Muscle pain
- Muscle pain can range from an aching muscle, spasm, or strain, to the severe spasticity that accompanies paralysis. Polymyositis, dermatomyositis, and inclusion body myositis are painful disorders characterized by muscle inflammation. They may be caused by infection or autoimmune dysfunction and are sometimes associated with connective tissue disorders, such as lupus and rheumatoid arthritis.
Myofascial pain syndromes
- Myofascial pain syndromes affect sensitive areas known as trigger points, located within the body’s muscles.
Neuropathic pain
- Neuropathic pain is a type of pain that can result from injury to nerves, either in the peripheral or central nervous system (see The Nervous Systems in the Appendix). Neuropathic pain can occur in any part of the body and is frequently described as a hot, burning sensation, which can be devastating to the affected individual. It can result from diseases that affect nerves (such as diabetes) or from trauma, or, because chemotherapy drugs can affect nerves, it can be a consequence of cancer treatment. Among the many neuropathic pain conditions are diabetic neuropathy (which results from nerve damage secondary to vascular problems that occur with diabetes); complex regional pain syndrome, which can follow injury; phantom limb and post-amputation pain (see Phantom Pain in the Appendix), which can result from the surgical removal of a limb; postherpetic neuralgia, which can occur after an outbreak of shingles; and central pain syndrome, which can result from trauma, stroke or injury to the brain or spinal cord.
Repetitive stress injuries
Repetitive stress injuries are muscular conditions that result from repeated motions performed in the course of normal work or other daily activities. They include:
- writer’s cramp, which affects musicians and writers and others,
- compression or entrapment neuropathies, including carpal tunnel syndrome, and
- tendonitis or tenosynovitis, affecting one or more tendons.
Sciatica
- Sciatica is a generic term representing pain in the buttocks that continues down into the thighs, legs, ankles, and feet . Sciatica can be caused by a number of factors including an injury or irritation to the nerve roots exiting the spinal cord that make up the sciatic nerve (e.g. herniated disc), or to the sciatic nerve directly.
Shingles and other painful disorders
Shingles and other painful disorders affect the skin and nerves. Pain is a common symptom of many skin disorders, even the most common rashes. One of the most distressing neurological disorders is shingles or herpes zoster, an infection that often causes agonizing pain resistant to treatment. Prompt treatment with antiviral agents is important to stop the infection and prevent an associated condition known as postherpetic neuralgia. Since postherpetic neuralgia is more common in the elderly, a vaccine is often recommended for persons over age 60 as part of one’s proactive health care. Other painful disorders affecting the skin include:
- vasculitis, or inflammation of blood vessels;
- other infections, including herpes simplex;
- skin tumors and cysts, and
- tumors associated with neurofibromatosis, a neurogenetic disorder.
Sports injuries
- Sports injuries are common. Sprains, strains, bruises, dislocations, and fractures are all well-known words in the language of sports. Pain is another. In extreme cases, sports injuries can take the form of costly and painful spinal cord and head injuries, which cause severe suffering and disability.
Spinal stenosis
- Spinal stenosis refers to a narrowing of the canal surrounding the spinal cord. The condition occurs naturally with aging. Spinal stenosis causes weakness in the legs and leg pain usually felt while the person is standing up and often relieved by sitting down.
Surgical pain
- Surgical pain may require regional or general anesthesia during the procedure and medications to control discomfort following the operation. Control of pain associated with surgery includes presurgical preparation and careful monitoring during and after the procedure.
Temporomandibular joint disorders
- Temporomandibular joint disorders are conditions in which the temporomandibular joint (the jaw) is damaged and/or the muscles used for chewing and talking become stressed, causing pain. The condition may result from a number of factors, such as an injury to the jaw or joint misalignment. It may give rise to a variety of symptoms, most commonly pain in the jaw, face, and/or neck muscles. Physicians reach a diagnosis by listening to the individual’s description of the symptoms and by performing a simple examination of the facial muscles and the temporomandibular joint.
Trauma
- Trauma can occur after injuries in the home, at the workplace, during sports activities, or on the road. Any of these injuries can result in severe disability and pain.
Vascular disease or injury
- Vascular disease or injury—such as vasculitis or inflammation of blood vessels, coronary artery disease, and circulatory problems—all have the potential to cause pain. Vascular pain affects millions of Americans and occurs when communication between blood vessels and nerves is interrupted. Ruptures, spasms, constriction, or obstruction of blood vessels, as well as a condition called ischemia in which blood supply to organs, tissues, or limbs is cut off, can also result in pain.
Anatomy of pain
Pain signals from the head and face directly enter the brain stem where they join the pain pathways that travel from the spinal cord to the brain. One central place these signals travel to is the thalamus. The thalamus is a relay station that distributes sensory signals to many other brain regions—including the anterior cingulate cortex, somatosensory cortex, insular cortex, and prefrontal cortex. These cortical brain regions process the nociceptive (pain causing or reacting to pain) information from the body and generate the complex experience of pain. This pain experience has multiple components that include the: 1) sensory-discriminative aspect which helps us localize where on our body the injury occurs, 2) affective-motivational aspect which conveys just how unpleasant the experience is and the 3) cognitive-evaluative which involves thoughtful planning on what to do to get away from the pain. Many of these characteristics of pain have been associated with specific brain systems, although much remains to be learned. Additionally, researchers have found that many of the brain systems involved with the experience of pain overlap with the experience of basic emotions. Consequently, when people experience negative emotions (e.g. fear, anxiety, anger), the same brain systems responsible for these emotions also amplify the experience of pain.
Fortunately, there are systems in the brain that help to dampen or decrease pain. Descending signals from the brain are sent back to the spinal cord and can inhibit the intensity of incoming nociceptive signals, thereby reducing the pain experience.
Neurochemistry of pain
This complicated process by which we perceive pain involves intricate connections among multifaceted brain regions. The nervous system uses a set of chemicals, called neurotransmitters, to communicate between neurons within and across these stations in the pain pathway. These chemicals are released by neurons in tiny packets (vesicles) into the space between two cells. When they reach their target cell, they bind to special proteins on the surface of the cells calledreceptors. The transmitter then activates the receptor, which functions much like a gate. The gate will either close to block (inhibitory receptor) the signal or open to send (excitatory receptor) the signal along to the next station.
There are many different neurotransmitters in the human body and they play a role in normal function as well as in disease. In the case of nociception and pain, they act in various combinations at all levels of the nervous system to transmit and modify signals generated by noxious stimuli.
One excitatory neurotransmitter of special interest to pain researchers is glutamate, which plays a major role in nervous system function and in pain pathophysiology. The modulation of glutamate neurotransmission is complex, but it plays a key role in heightening the sensitivity to pain through increased responsiveness of excitatory receptors in the spinal cord dorsal horn and in the brain. This is part of a process called central sensitization (see below) and contributes to making pain persist. A great deal of attention has been given to developing molecules/drugs that block certain receptors for glutamate for their potential in reducing pain.
Unlike glutamate, GABA (or gamma-aminobutyric acid) is predominately an inhibitory neurotransmitter in that it generally decreases or blocks the activity of neurons. Most of what we know of its role in pain is related to its function in inhibiting spinal cord neurons from transmitting pain signals and therefore dampening pain. Chemicals that are similar to GABA have been explored as possible analgesics, but because GABA is so widespread in the nervous system it is difficult to make a GABA-like drug without affecting other nervous system functions. As we learn more about the specific roles of GABA receptors, drug development may be accelerated.
Norepinephrine and serotonin are neurotransmitters used by the descending pain pathways from the brain stem to dampen the incoming signals from painful stimuli from the site of the injury or inflammation. Drugs that modulate the activity of these transmitters, such as some antidepressants, are effective in treating some chronic pain conditions, likely by enhancing the availability of the transmitters through a recycling and reuse process. Serotonin receptors also are present on the nerves that supply the surface of the brain involved in migraines, and their modulation by a class of drugs called “triptans” is effective in acutely treating migraine.
The opioids are another important class of neurotransmitters that are involved in pain control, as well as pleasure and addiction. Their receptors are found throughout the body and can be activated by endogenous (produced by our bodies) opioid peptides that are released by neurons in the brain. The enkephalins, dynorphins, and endorphins are some of the body’s own natural pain killers. They may be more familiar for the role of endorphins in the feeling of well-being during exercise—the runner’s high. Opioid receptors also can be activated by morphine, which mimics the effect of our endogenous opioids. Morphine is a natural product and like similar synthetic opioids, is a very potent, but potentially addictive pain killer that is used broadly for severe acute and chronic pain management. Together the opioids provide effective pain relief for many people with pain. Other peptides also transmit neuronal signals and play a role in pain responses. Scientists have shown that mice bred experimentally to lack a gene for two peptides, called tachykinins-neurokinin A and substance P, have a reduced response to severe pain. When exposed to mild pain, these mice react in the same way as mice that carry the missing gene. But when exposed to more severe pain, the mice exhibit a reduced pain response. This suggests that the two peptides are involved in the perception of pain sensations, especially moderate-to-severe pain.
Genetics of pain
Differences in our genes highlight how different we are in respect to pain. Scientists believe that genetic variations can determine our risk for developing chronic pain, how sensitive we are to painful stimuli, whether or not certain therapies will ease our pain, and how we respond to acute or chronic pain. Many genes contribute to pain perception, and mutations in one or more pain-related genes account for some of the variability of each individual’s pain experiences. Some people born genetically insensate to pain—meaning they cannot feel pain—have a mutation in part of a gene that plays a role in electrical activity of nerve cells. A different mutation in that same gene can cause a severe and disabling pain condition. Scientists have identified many genes involved in pain by screening large numbers of people with pain conditions for shared gene mutations. While genes play a role in determining our sensitivity to pain, they only account for a portion of this variability. Ultimately, our individual sensitivity to pain is governed by a complex interaction of genes, cognitions, mood, our environment and early life experiences.
Inflammation and pain
The link between the nervous and immune systems also is important. Cytokines, a group of proteins found in the nervous system, are also part of the immune system—the body’s shield for fighting off disease and responding to tissue injury. Cytokines can trigger pain by promoting inflammation, even in the absence of injury or damage. After trauma, cytokine levels rise in the brain and spinal cord and at the site where the injury occurred. Improvements in our understanding of the precise role of cytokines in producing pain may lead to new classes of drugs that can block the action of these substances to produce analgesia.
Neural circuits and chronic pain
The pain that we perceive when we have an injury or infection alerts us to the potential for tissue damage. Sometimes this protective pain persists after the healing occurs or may even appear when there was no apparent cause. This persistent pain is linked to changes in our nervous system, which responds to internal and external change by reorganizing and adapting throughout life. This phenomenon is known as neuronal plasticity, a process that allows us to learn, remember, and recover from brain injury. Following an injury or disease process, sometimes the nervous system undergoes a structural and functional reorganization that is not a healthy form of plasticity. Long-term, maladaptive changes in both the peripheral and central nervous system can make us hypersensitive to pain and can make pain persist after injuries have healed. For example, sensory neurons in the peripheral nervous system, which normally detect noxious/painful stimuli, may alter the electrical or molecular signals that they send to the spinal cord. This in turn triggers genes to alter production of receptors and chemical transmitters in spinal cord neurons setting up a chronic pain state. Scientists have methods to identify which genes’ activities change with injury and chronic pain. Knowledge of the proteins that ultimately are synthesized by these genes are providing new targets for therapy development. Increased physiological excitation of neurons in the spinal cord, in turn enhance pain signaling pathways to the brain stem and in the brain. This hypersensitivity of the central nervous system is called central sensitization. It is difficult to reverse and makes pain persist beyond its protective role.
How is pain diagnosed?
There is no way to tell accurately how much pain a person has. Tools to measure pain intensity, to show pain through imaging technology, to locate pain precisely, and to assess the effect of pain on someone’s life, offer some insight into how much pain a person has. They do not, however, provide objective measures of pain. Sometimes, as in the case of headaches, physicians find that the best aid to diagnosis is the person’s own description of the type, duration, and location of pain. Defining pain as sharp or dull, constant or intermittent, burning or aching may give the best clues to the cause of pain. These descriptions are part of what is called the pain history, taken by the physician during the preliminary examination of a person with pain. Developing a test for assessing pain would be a very useful tool in diagnosing and treating pain.
Doctors, however, do have a number of approaches and technologies they use to find the cause of pain. Primarily these include:
- A musculoskeletal and neurological examination in which the physician tests movement, reflexes, sensation, balance, and coordination.
- Laboratory tests (e.g. blood, urine, cerebrospinal fluid) can help the physician diagnose infection, cancer, nutritional problems, endocrine abnormalities and other conditions that may cause pain.
- Electrodiagnostic procedures include electromyography (EMG), nerve conduction studies, evoked potential studies, and quantitative sensory testing. These procedures measure the electrical activity of muscles and nerves. They help physicians evaluate muscle symptoms that may result from a disease or an injury to the body’s nerves or muscles. Electromyography (EMG) tests muscle activity. It can help physicians tell which muscles or nerves are affected by weakness or pain. Nerve conduction studies are usually performed along with electromyography (EMG). These studies record how nerves are functioning. evoked potential studies measure electrical activity in the brain in response to sight, sound, or touch stimulation. Quantitative sensory testing can establish thresholds for sensory perception in individuals which can then be compared to normal values. These tests are used to detect abnormalities in sensory function and nerve disorders.
- Imaging, especially magnetic resonance imaging or MRI, provides physicians with pictures of the body’s structures and tissues, such as the brain and spinal cord. MRI uses magnetic fields and radio waves to differentiate between healthy and diseased tissue. X-rays produce pictures of the body’s structures, such as bones and joints.
How is pain treated?
The goal of pain management is to improve function, enabling individuals to work, attend school, and participate in day-to-day activities. People with pain and their physicians have a number of options for treatment; some are more effective than others. Sometimes, relaxation and the use of imagery as a distraction provide relief. These methods may be powerful and effective, according to those who advocate their use. Whatever the treatment regime, it is important to remember that, while not all pain is curable, all pain is treatable. The following treatments are among the most common.
Treatment varies depending on the duration and type of pain. For the most part, the medications listed below have been shown in clinical trials to relieve or prevent pain associated with a specific condition(s), but none have been proven fully effective in relieving all types of pain. A health care professional should be consulted to determine which medication is effective for a given pain condition and what to expect for pain relief and side effects. Evidence for the procedures listed below is variable in its quality. In some cases, evidence suggesting that some treatments are effective is anecdotal—or based on personal experience—and in other cases it is collected from well-designed clinical trials.
Acupuncture
- Acupuncture involves the application of needles to precise points on the body. It is part of a general category of healing called traditional Chinese medicine. The mechanism by which acupuncture provides pain relief remains controversial but is quite popular and may one day prove to be useful for a variety of conditions as it continues to be explored. Evidence of the effectiveness of acupuncture for pain relief is conflicting and clinical studies to investigate its benefits are ongoing.
Anticonvulsants
Anticonvulsants are used to treat seizure disorders because they dampen abnormally fast electrical impulses. They also sometimes are prescribed to treat pain. Carbamazepine in particular is used to treat a number of painful conditions, including trigeminal neuralgia. Other antiepileptic drugs, including gabapentin and pregabalin, are also used to treat some forms of pain, including neuropathic pain. Some, such as valproic acid and topiramate, are helpful in preventing migraine headaches.
Your doctor may want you to try an anticonvulsant medicine. It may help reduce some types of chronic pain, such as low back pain. Examples of anticonvulsants are:
- gabapentin (Neurontin)
- carbamazepine (Tegretol)
- phenytoin (Dilantin)
- pregabalin (Lyrica)
- topiramate (Topamax).
Like antidepressants (see below), your doctor may start you on a low dose of anticonvulsants. This helps prevent or reduce side effects. The doctor may increase the amount over time. Contact your doctor right away if you have suicidal thoughts. Minor side effects may include:
- drowsiness
- nausea or vomiting
- restlessness
- dizziness
- loss of appetite
- weight gain
- itching or swelling.
Antidepressants
- Antidepressants are sometimes used to treat chronic pain and along with neuroleptics and lithium, belong to a category of drugs called psychotropic drugs. For example, antidepressants can improve function and provide pain relief.
- Antidepressants may be used to treat nerve damage, arthritis, and fibromyalgia. They also may help with headaches, facial pain, low back pain, and pelvic pain. It can take several weeks for the medicines to start working.
- Types of antidepressants your doctor may prescribe include:
- Tricyclic antidepressants (TCAs), such as amitriptyline (Elavil), imipramine (Tofranil), nortriptyline (Pamelor), and doxepin.
- Selective serotonin/norepinephrine reuptake inhibitors (SNRIs), such as duloxetine (Cymbalta).
- Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac), paroxetine (Paxil), and sertraline (Zoloft).
- Possible side effects of antidepressants include:
- nausea
- drowsiness
- insomnia (trouble sleeping)
- dry mouth
- dizziness
- constipation
- weight gain
- heart problems.
Tricyclic antidepressants (TCAs) tend to have more side effects than selective serotonin/norepinephrine reuptake inhibitors (SNRIs) or selective serotonin reuptake inhibitors (SSRIs), but they usually are mild. Your doctor may start you on a low dose of medicine. This helps prevent side effects and allows your body to adjust. The doctor may increase the amount over time. If at any point while taking medicine you become depressed or have suicidal thoughts, call your doctor right away.
Anxiolytics
- Anxiolytics include medications in the class of benzodiazepines (which are used to decrease central nervous system activity). These drugs also act as muscle relaxants and are sometimes used for acute pain situations. Physicians usually try to treat the condition with analgesics before prescribing these drugs.
Beta-blockers
- Beta-blockers are medications which inhibit one arm of the sympathetic nervous system and adrenal “fight or flight” hormones. Propranolol and timolol are used to prevent migraine headaches.
Biofeedback
- Biofeedback is used to treat many common pain problems, most notably headache and back pain. Using a special electronic machine, individuals are trained to become aware of, to follow, and to gain control over certain bodily functions, including muscle tension, heart rate, and skin temperature. The individual can then learn to change his or her responses to pain, for example, by using relaxation techniques. Eventually, these changes can be maintained without using the machine. Biofeedback is often used in combination with other treatment methods, generally without side effects. Similarly, the use of relaxation techniques to treat pain can increase a person’s feeling of well-being.
Capsaicin
- Capsaicin is a chemical found in chili peppers that is also a primary ingredient in prescription or over-the-counter pain-relieving creams available as a treatment for a number of pain conditions, such as shingles. This topical cream may be particularly good for deep pain. It works by reducing the amount of substance P found in nerve endings and interferes with the transmission of pain signals to the brain. Individuals can become desensitized to the compound, however, perhaps because of long-term capsaicin-induced damage to nerve tissue. Some individuals find the burning sensation they experience when using capsaicin cream to be intolerable, especially when they are already suffering from a painful condition, such as postherpetic neuralgia, which occurs in some people after a bout of shingles. Soon, however, better treatments that relieve pain by blocking vanilloid receptors (also called capsaicin receptors) may arrive in drugstores.
Chiropractic care
- Chiropractic care may ease back pain, neck pain, headaches, and musculoskeletal conditions. It involves “hands-on” therapy designed to adjust the relationship between the body’s structure (mainly the spine) and its functioning. Chiropractic spinal manipulation includes the adjustment and manipulation of the joints and adjacent tissues. Such care may also involve therapeutic and rehabilitative exercises. Numerous clinical trials have been done to assess the effectiveness of spinal manipulations. A review of these trials concludes that evidence of their benefit for acute and sub-acute low back pain is of low quality. For chronic back pain however, there is evidence for small to moderate treatment relief.
Cognitive-behavioral therapy
- Cognitive-behavioral therapy (CBT) is a well-established treatment for pain that involves helping the person improve coping skills, address negative thoughts and emotions that can amplify pain, and learn relaxation methods to help prepare for and cope with pain. It is used for chronic pain, postoperative pain, cancer pain, and the pain of childbirth. Many clinical studies provide evidence for the effectiveness of this form of treatment in pain management.
Counseling
- Counseling can give an individual suffering from pain much needed support, whether it comes from family, group, or individual counseling. Support groups can provide an important supplement to drug or surgical treatment. Psychological treatment can also help people learn about the physiological changes produced by pain.
Electrical stimulation
Electrical stimulation, including transcutaneous electrical stimulation (TENS), implanted electric nerve stimulation, and deep brain or spinal cord stimulation, is the modern-day extension of age-old practices in which the nerves or muscles are subjected to a variety of stimuli, including heat or massage. The following techniques each require specialized equipment and personnel trained in the specific procedure being used:
- TENS (transcutaneous electrical stimulation) uses tiny electrical pulses, delivered through the skin to nerve fibers, to cause changes in muscles, such as numbness or contractions. This in turn produces temporary pain relief. There is also evidence that TENS (transcutaneous electrical stimulation) can activate subsets of peripheral nerve fibers that can block pain transmission at the spinal cord level, in much the same way that shaking your hand can reduce pain.
- Peripheral nerve stimulation uses electrodes placed surgically or percutaneously (through the skin using a needle) on a peripheral nerve. The individual is then able to deliver an electrical current as needed to the affected nerve, using a controllable electrical generator.
- Spinal cord stimulation uses electrodes surgically or percutaneously inserted within the epidural space of the spinal cord. The individual is able to deliver a pulse of electricity to the spinal cord using an implanted electrical pulse generator that resembles a cardiac pacemaker.
- Deep brain stimulation (DBS) is considered a more extreme treatment and involves surgical stimulation of the brain, usually the thalamus or motor cortex. It is used to treat chronic pain in cases that do not respond to less invasive or conservative treatments.
Exercise
- Exercise also may be part of the pain treatment regime for some people with pain. Because there is a known link between many types of chronic pain and tense, weak muscles, exercise—even light to moderate exercise such as walking or swimming—can contribute to an overall sense of well-being by improving blood and oxygen flow to muscles. Just as we know that stress contributes to pain, we also know that exercise, sleep, and relaxation can all help reduce stress, thereby helping to alleviate pain. Exercise has been proven to help many people with low back pain. It is important, however, to work with a physician or physical therapist to create an appropriate routine.
Hypnosis
- Hypnosis was first approved for medical use by the American Medical Association in 1958. In general, hypnosis is used to control physical function or response, that is, the amount of pain an individual can withstand. How hypnosis works is not fully understood. Some believe that hypnosis delivers the person into a trance-like state, while others feel that the individual is simply better able to concentrate and relax or is more responsive to suggestion. Hypnosis may result in relief of pain by acting on chemicals in the nervous system, slowing impulses. Whether and how hypnosis works involves greater insight—and research—into the mechanisms underlying human consciousness.
Low-power lasers
- Low-power lasers have been used occasionally by some physical therapists as a treatment for pain, but like many other treatments, this method is not without controversy.
Magnets
- Magnets are increasingly popular with athletes who are convinced of their effectiveness for the control of sports-related pain and other painful conditions. Usually worn as a collar or wristwatch, the use of magnets as a treatment dates back to the ancient Egyptians and Greeks. While it is often dismissed as quackery and pseudoscience by skeptics, proponents offer the theory that magnets may effect changes in cells or body chemistry, thus producing pain relief.
Marijuana
- Marijuana or cannabis, continues to remain highly controversial as a pain killer. In the eyes of many individuals campaigning on its behalf, marijuana rightfully belongs with other pain remedies. Scientific studies are underway to test the safety and usefulness of cannabis for treating certain medical conditions. Currently, smoking marijuana is not recommended for the treatment of any disease or condition. In fact, federal law prohibits the use of cannabis. However, a number of states and the District of Columbia permit its use for certain medical problems.
Nerve blocks
Nerve blocks employ the use of drugs, chemical agents, or surgical techniques to interrupt the relay of pain messages between specific areas of the body and the brain. There are many different names for the procedure, depending on the technique or agent used. Types of surgical nerve blocks include neurectomy; spinal dorsal, cranial, and trigeminal rhizotomy; and sympathectomy, also called sympathetic blockade.
Nerve blocks may involve local anesthesia, regional anesthesia or analgesia, or surgery; dentists routinely use them for traditional dental procedures. Nerve blocks can also be used to prevent or even diagnose pain and may involve injection of local anesthetics to numb the nerve and/or steroids to reduce inflammation.
In the case of a local nerve block, any one of a number of local anesthetics may be used, such as lidocaine or bupivicaine. Peripheral nerve blocks involve targeting a nerve or group of nerves that innervate a part of the body. Nerve blocks may also take the form of what is commonly called an epidural, in which a drug is administered into the space between the spine’s protective covering (the dura) and the spinal column. This procedure is most well known for its use during childbirth. However it is also used to treat acute or chronic leg or arm pain due to an irritated spinal nerve root.
- Sympathectomy, also called sympathetic blockade, typically involves injecting local anesthetic through a needle next to the sympathetic nervous system. The procedure is often performed to treat neuropathic pain of a limb (e.g. complex regional pain syndrome) as well as vascular disease pain, and other conditions. In some cases, a drug called guanethidine is administered intravenously in order to accomplish the block.
- Neurolytic blocks employ injection of chemical agents such as alcohol, phenol, or glycerol – or the use of radiofrequency energy – to kill nerves responsible for the transmission of nociceptive signals. Neurolytic blocks are most often used to treat cancer pain or to block pain in the cranial nerves.
- Surgical blocks are performed on cranial, peripheral, or sympathetic nerves. They are most often done to relieve the pain of cancer and extreme facial pain, such as that experienced with trigeminal neuralgia. There are several different types of surgical nerve blocks and they are not without problems and complications. Nerve blocks can cause muscle paralysis and, in many cases, result in at least partial numbness. For that reason, the procedure should be reserved for a select group of patients and should only be performed by skilled surgeons. Types of surgical nerve blocks include:
- Spinal dorsal rhizotomy, in which the surgeon cuts the root or rootlets of one or more of the nerves radiating from the spinal cord. Other rhizotomy procedures include cranial rhizotomy and trigeminal rhizotomy, performed as a treatment for extreme facial pain or for the pain of cancer.
Physical therapy and rehabilitation
Physical therapy and rehabilitation date back to the ancient practice of using physical techniques and methods, such as heat, cold, exercise, massage, and manipulation, in the treatment of certain conditions. These may be applied to increase function, control pain, and gain full recovery.
Placebo
- Placebo is not a treatment for pain but is an effect generally used in clinical studies as a control factor to help determine the effectiveness of an active treatment. Placebos are inactive substances, such as sugar pills, or harmless procedures, such as saline injections or sham surgeries. Placebos offer some individuals pain relief although how they have an effect is mysterious and somewhat controversial. Although placebos have no direct effect on the underlying causes of pain, evidence from clinical studies suggests that many pain conditions such as migraine headache, back pain, post-surgical pain, rheumatoid arthritis, angina, and depression sometimes respond well to them. This positive response is known as the placebo response, which is defined as the observable or measurable change that can occur in people after administration of a placebo. One large component responsible for the effect of placebo is the degree to which people expect the treatment to work. Placebos work, in part, by stimulating the brain’s own analgesics.
Rest, Ice, Compression, and Elevation
R.I.C.E.—Rest, Ice, Compression, and Elevation—are four components prescribed by many orthopedists, coaches, trainers, nurses, and other professionals for temporary muscle or joint injuries, such as sprains or strains. Ice is used to reduce the inflammation associated with painful and acute injuries. Ice or heat may be recommended to relieve subacute and chronic pain, allowing for reduced inflammation and increased mobility. While many common orthopedic problems can be controlled with these four simple steps, especially when combined with over-the-counter pain relievers, more serious conditions may require surgery or physical therapy, including exercise, joint movement or manipulation, and stimulation of muscles.
Serotonergic agonists
- Serotonergic agonists—the triptans (including sumatriptan, naratriptan, and zolmitriptan)—are used specifically for acute migraine headaches. They can have serious side effects in some people and therefore, as with all prescription medicines, should be used only under a doctor’s care.
Surgery
Surgery, although not always an option, may be required to relieve pain, especially pain caused by back problems or serious musculoskeletal injuries. Surgery may take the form of a nerve block (see Nerve Blocks in the Appendix) or it may involve an operation to relieve pain from a ruptured disc. Surgical procedures for pain due to a vertebral disc pressing on a nerve root or spinal cord include discectomy or, when microsurgical techniques are used, microdiscectomy, in which the part of or the entire disc is removed; laminectomy, a procedure in which a surgeon opens up the arched portion of a vertebra thereby allowing the nerve root to exit more freely; and spinal fusion, a procedure where two or more vertebral segments are fused together. Although the operation can cause the spine to stiffen, resulting in lost flexibility, the procedure serves one critical purpose: protection of the spinal cord. Other operations for pain includerhizotomy, in which a nerve close to the spinal cord are burned or cut, and cordotomy, where bundles of nerves within the spinal cord are severed. Cordotomy is generally used only for the pain of terminal cancer that does not respond to other therapies. Another operation for pain is the dorsal root entry zone operation (DREZ), in which spinal neurons corresponding to the individual’s pain are destroyed surgically. Microvascular decompression, in which tiny blood vessels are surgically separated from surrounding nerves, is helpful for some individuals suffering from trigeminal neuralgia who are not responsive to drug treatment. Because surgery can result in scar tissue formation that may cause additional problems, people are well advised to seek a second opinion before proceeding.
Surgical procedures are not always successful. The related risks associated and other treatment options should be explored and considered. There is little measurable evidence to show which procedures work best for their particular indications.
Analgesic medications
Acetaminophen
- Acetaminophen (paracetamol) is the basic ingredient found in Tylenol® and its many generic equivalents. It is sold over the counter, in a prescription-strength preparation, and in combination with codeine (also by prescription).
- Acetaminophen seems to work on the parts of the brain that receive pain messages. It also works with the part that controls body temperature.
- Acetaminophen does not reduce inflammation the way other pain medicines do. But it has fewer side effects, such as stomach problems. This makes it safer for long-term use and for children.
- Use acetaminophen to:
- relieve headaches
- ease common aches and pains
- treat arthritis and other chronic painful conditions.
Acetaminophen side effects
- Acetaminophen (paracetamol) can cause liver damage in some cases. This usually happens if you take too much, or if you take it while drinking alcohol. Adults should not take more than 3 grams (3,000 mg) of acetaminophen (6 extra-strength 500 mg tablets) a day.
- Do not take acetaminophen if you:
- have severe kidney or liver disease
- have 3 or more drinks that contain alcohol every day
- are already taking another product containing acetaminophen.
Nonsteroidal anti-inflammatory drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) (including aspirin, ibuprofen and naproxen) are widely prescribed and sometimes called non-narcotic or non-opioid analgesics. Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce the level of hormone-like substances (called prostaglandins) that your body makes. These substances irritate your nerve endings and cause the feeling of pain. They also are part of the system that helps your body control its temperature. Many of these drugs irritate the stomach and for that reason are usually taken with food. Nonsteroidal anti-inflammatory drugs (NSAIDs) can also adversely effect the kidneys and heart and should be taken with caution by people with kidney dysfunction, heart disease, or hypertension.
- Aspirin may be the most widely used pain-relief agent and has been sold over-the-counter since 1905 as a treatment for fever, headache, and muscle soreness.
- COX-2 inhibitors may be effective for individuals with arthritis. COX-2 inhibitors are a type of nonsteroidal anti-inflammatory drug (NSAID). NSAIDs work by blocking two enzymes, cyclooxygenase-1 and cyclooxygenase-2, both of which promote production of hormones called prostaglandins, which in turn cause inflammation, fever, and pain. COX-2 inhibitors primarily block cyclooxygenase-2 and are less likely to have the gastrointestinal side effects sometimes produced by NSAIDs. Due to possible increased cardiovascular risk and gastrointestinal bleeding, the American Geriatic Association recommended in 2009 that NSAIDs and COX-2s be considered rarely for older people, and with extreme caution,. Individuals taking any of the COX-2 inhibitors should review their drug treatment with their doctors.
- Ibuprofen is sold over the counter and also comes in prescription-strength preparations.
Nonsteroidal anti-inflammatory drugs (NSAIDs) may cause upset stomach. They can also cause increased bruising or risk of bleeding in the stomach. When taken for a long time, they may cause kidney damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) can interact with blood pressure medicines. If you take one of these medicines and an NSAID, your medicine may not work as well as it should.
Nonsteroidal anti-inflammatory drugs side effects
Always take nonsteroidal anti-inflammatory drugs (NSAIDs) with food or milk because the most common side effects are related to the stomach. Other side effects include:
- increased bruising.
- risk of bleeding in the stomach.
- kidney damage (when taken for long periods of time).
- high blood pressure.
- interference with blood pressure medicines.
If you take other pain medicines, do not take NSAIDs without talking to your doctor first.
Talk with your doctor before you take an nonsteroidal anti-inflammatory drug (NSAID), especially aspirin, if you:
- are allergic to aspirin or other pain relievers
- have 3 or more drinks that contain alcohol every day
- have bleeding in the stomach or intestines, or have peptic (stomach) ulcers
- have liver or kidney disease
- have heart disease
- take blood-thinning medicine or have a bleeding disorder
Children and teenagers younger than 18 years of age should not take aspirin. It increases the risk of Reye’s Syndrome, a serious illness that can lead to death.
Opioids
Opioids also known as narcotic analgesics, opiates, opioid analgesics, or narcotics, are derived from the poppy plant and are among the oldest drugs known to humankind. Opioids (narcotic analgesics) are a class of medicines that are used to provide relief from moderate-to-severe acute or chronic pain 5. Opioids include codeine and perhaps the most well-known opioid of all, morphine. Morphine can be administered in a variety of forms, including a pump for self-administration. Opioids are extremely effective in treating acute pain. Opioids have a narcotic effect, that is, they induce sedation as well as pain relief. In addition to drowsiness, other common side effects include constipation, nausea, and vomiting. Opioids are addictive, with severely unpleasant and potentially dangerous withdrawal symptoms occurring when drugs are stopped. Chronic opioid use is a major health problem, stimulating research to develop a less addictive alternative for severe pain. For these reasons, people given opioids should be monitored carefully. Research is still needed to determine which patients will most benefit from opioids and which patients are most vulnerable to their addicting properties.
- Doctors rarely prescribe narcotics or opioids to treat chronic pain. This is because they are highly addictive. Currently, there is an opioid crisis in the United States with more than two million people in the U.S. alone having a substance misuse disorder involving prescription narcotic analgesics; this was second only to marijuana 6. People who become addicted can develop severe symptoms, such as increased pain, depression, or suicidal thoughts. They may begin to abuse other substances or their behaviors could become harmful or violent. Addicts are at risk of misusing or overdosing on narcotics, which can cause death. Talk to your doctor about all risks of narcotics before starting a new medicine.
- Among individuals who reported the nonmedical use of a prescription analgesic, 55% obtained the drug from a friend or relative, 79% of whom obtained the prescription from a physician, and another 17% obtained the prescription directly from a physician 6. Among patients hospitalized for opioid dependence, 51% first started using the drug to treat pain (e.g., after a surgery, dental procedure, or injury) 7. Patients should be counseled to safely dispose of any unused medication 8.
If your doctor does prescribe a narcotic, be sure to follow their directions. Do not drive or operate heavy machinery when taking narcotics. Do not use alcohol as well. Tell your doctor if you have side effects from narcotics. These may include nausea, constipation, and trouble focusing or thinking clearly. Your doctor can prescribe an anti-nausea drug or laxative to help with side effects.
USE OPIOIDS SAFELY: 3 KEY STEPS
- Keep your doctor informed. Inform your health care professional about any past history of substance abuse. All patients treated with opioids for pain require careful monitoring by their health care professional for signs of abuse and addiction, and to determine when these analgesics are no longer needed.
- Follow directions carefully. Opioids are associated with significant side effects, including drowsiness, constipation, and depressed breathing depending on the amount taken. Taking too much could cause severe respiratory depression or death. Do not crush or break pills. This can alter the rate at which the medication is absorbed and lead to overdose and death.
- Reduce the risk of drug interactions. Don’t mix opioids with alcohol, antihistamines, barbiturates, or benzodiazepines. All of these substances slow breathing and their combined effects could lead to life-threatening respiratory depression.
When you’re taking narcotics, it’s important to remember the difference between “physical dependence” and “psychological addiction.” Physical dependence means that your body adjusts to a medicine and needs it in order to function. When you function has improved, your doctor will help you slowly and safely decrease the amount of medicine. Doing this helps prevent or reduce symptoms of withdrawal. It is critical to tell your doctor about these symptoms and work through the process together.
Psychological addiction is the desire to use a drug whether or not it’s needed to improve function and relieve pain. Using a narcotic this way is harmful to your health. Talk to your doctor if you think you are addicted to narcotics. They may give you other medicines to help your addiction. They could lower the dose, change to another drug, or stop the medicine. They may recommend counseling or rehab as well.
Table 2. Common narcotic analgesics available in the U.S.
| Name | Route | Onset of effect | Duration of effect |
|---|---|---|---|
| Alfentanil | Intravenous (IV) | 90 seconds | 45-60 mins |
| Codeine | Oral | 15-60 mins | 3-4 hours |
| Fentanyl | IV | Immediate | 0.5-1h |
| Intramuscular (IM) | 7-8 mins | 1-2 hours | |
| Buccal (through the gums) Sublingual (SL) | 5-15mins | 4-6 hours | |
| Transdermal patch (via the skin) | 6h | 72-96 hours | |
| Hydrocodone | Oral | 10-20 minutes | 4-8 hours |
| Hydromorphone | Oral | 15-30 mins | 3-4 hours |
| IV | 5 mins | 3-4 hours | |
| Methadone | Subcutaneous (SC) (under the skin) | 15 mins | 3-4 hours |
| Morphine | Oral | 30-60 mins | 3-6 hours (immediate-release) 8-24 hours (extended-release) |
| IV/SC | 5-10 mins | 4 hours | |
| Oxycodone | Oral | 10-15 mins | 3-6 hours |
| Oxymorphone | Oral | 30-60 mins (immediate-release) 1-2 hours (extended-release) | 4-6 hours (immediate-release) 12 hours (extended-release) |
| IM/IV/SC | 5-10 mins | 3-6 hours | |
| Tramadol | Oral | 30-60 mins (immediate-release) 1-2 hours (extended-release) | 4-6 hours (immediate-release) 24 hours (extended-release) |
What are the differences between opioids?
Narcotic analgesics differ in their structure, potency, and the way they are absorbed, distributed, metabolized and excreted within the body.
Some, like morphine and codeine were originally derived from plants. Others, such as heroin, hydrocodone, hydromorphone, oxycodone and oxymorphone were made by modifying morphine and are called semi-synthetic. There are three main classes of opioids – those that are structurally like morphine (the phenanthrenes), those that resemble fentanyl (the phenylpiperidines), and those that resemble methadone (the phenylheptylamines).
Different narcotic analgesics have different potencies, based on how strongly they bind to the opioid receptor (for example, fentanyl is 80 to 100 times stronger than morphine). This means that dosages for one narcotic may be significantly different from another. Although conversion charts exist (these tell you what dose of a narcotic compares to the equivalent analgesic dose of morphine), these are only at best a guide because other variables, such as an individual’s genetics, also play a part in how a person responds to a narcotic.
If a narcotic analgesic is deemed appropriate, codeine or tramadol should be tried first if the pain is mild-to-moderate. If the pain is unresponsive to these analgesics, or for more severe pain, then hydromorphone, morphine, or oxycodone should be considered. Fentanyl and methadone should only be used for severe pain that is unresponsive to other narcotic analgesics.
What are opioids used for?
In the past, narcotic analgesics have been used for all types of pain, which may explain why there are so many people addicted to them today.
The most appropriate use of narcotic analgesics is for the relief of short-term, intense pain, such as that occurring immediately after surgery or due to a medical condition.
Narcotic analgesics are also appropriate for the relief of pain due to cancer, or for palliative care or end-of life care. However, they should only be considered to treat other types of chronic pain under strict conditions and with close monitoring.
Opioids side effects
Narcotic analgesics (opioids) have many side effects, although people with cancer or terminal illness taking narcotics for long periods of time may become tolerant to some of these side effects.
Drowsiness, sleepiness, or dizziness is common with most narcotic analgesics. This can affect driving or a person’s ability to operate machinery and perform other hazardous tasks. Alcohol may potentiate these effects.
Other commonly reported opioids side effects include:
- Constipation
- Breathing difficulty
- Itching or a skin rash
- Loss of appetite
- Low blood pressure
- Miosis (constriction of the pupil of the eye)
- Nausea and vomiting
- Problems with urination
- Shakiness or a tremor
- Slow heartbeat.
Withdrawal symptoms may occur when people who have been taking narcotic analgesics abruptly stop taking them. Symptoms are like having the flu, and may include body aches, chills, depression, diarrhea, goose-bumps, headaches, high blood pressure, insomnia, irritability, a runny nose and sweats. Withdrawal symptoms usually last about a week.
Are opioids safe?
There are serious risks associated with narcotic analgesics including respiratory depression (unusually slow and shallow breathing), opioid-use disorder, and potentially fatal overdose.
Opioid-use disorder is defined as the repeated occurrence of at least two out of 11 specific opioid-associated problems, including using opioids in increased amounts or for longer than intended; continued use despite interference with daily activities; or still using while in hazardous situations. Severe opioid-use disorder is defined as a cluster of 6 or more problems and it can affect people from all educational and socioeconomic backgrounds.
Narcotic analgesics are potentially addictive and the risk of becoming emotionally and physically dependent on them increases the more you take and the longer you take them for. When prescribed by a doctor and used for short periods of time, such as for less than five days for pain relief after surgery, the risk of becoming addicted to narcotic analgesics is relatively low.
The number of fatal overdoses from opioids continues to rise and this has resulted in government officials introducing new legislation to further restrict the prescribing of opioids. More than 42,000 people died in 2016 because of an opioid overdose; 40% of these deaths involved a prescription narcotic analgesic.
When taken exactly as prescribed by a doctor, for short periods of time, for the relief of severe pain, and under strict monitoring, opioids (narcotic analgesics) are considered acceptable to use. However, they may still be associated with some severe side effects, despite proper use.
Combination analgesics
Many analgesic products contain combinations of different drugs. There are at least 40 different combination analgesic preparations available. Most of these are combinations of acetaminophen (paracetamol) 500 mg with codeine (an opioid) in doses ranging from 8 mg to 30 mg. Some products contain both acetaminophen and aspirin (2 brand names: Excedrin, Vanquish). These typically contain caffeine as well. They are good for treating headaches. A number of other preparations also contain doxylamine, a sedating antihistamine with anticholinergic effects 9. There are also other preparations available which contain acetaminophen (paracetamol) and dextropropoxyphene, aspirin and codeine, aspirin and dihydrocodeine, and ibuprofen and codeine. Internationally, preparations containing acetaminophen (paracetamol) with other opioids such as oxycodone and tramadol are available.
Which analgesic to start first?
The World Health Organization (WHO) pain relief ladder (see Figure 1 above) recommends a nonopioid such as acetaminophen (paracetamol) or a nonsteroidal anti-inflammatory drug (NSAID) for the initial management of pain. Acute pain characteristics and patient risk factors should be considered when choosing between acetaminophen and an NSAID (e.g., aspirin, other nonselective NSAIDs, cyclooxygenase-2 [COX-2] selective NSAIDs).
Acetaminophen
Acetaminophen, called paracetamol outside of the United States, is the first-line treatment for most mild to moderate acute pain 10. The effectiveness of acetaminophen is similar to that of nonsteroidal anti-inflammatory drugs (NSAIDs) such as celecoxib (Celebrex), 200 mg; aspirin, 600 to 650 mg; and naproxen (Naprosyn), 200 to 220 mg 10. Acetaminophen is generally well-tolerated, has few drug-drug interactions, is not associated with increased blood pressure (as with NSAIDs), can be used during pregnancy (U.S. Food and Drug Administration [FDA] pregnancy category B), and is the analgesic of choice for episodic use in patients with impaired renal function 11. Although acetaminophen is less effective for acute low back pain than some NSAIDs, it is a reasonable first-line option because of its favorable safety and cost profiles 12.
U.S. Food and Drug Administration [FDA] pregnancy category B: Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in pregnant women.
Aspirin
Aspirin effectively relieves mild to moderate acute pain. Aspirin is similar to the same dose of acetaminophen and is comparable to celecoxib, 200 mg 2. Over a dose range of 500 to 1,200 mg, aspirin exhibits a dose-response relationship (i.e., a 1,200-mg dose of aspirin provides better pain relief than 600- to 650-mg doses) 2. Like nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin can cause gastrointestinal bleeding and ulcer 13. Patients with chronic urticaria and asthma have a greater likelihood of salicylate hypersensitivity, which can manifest as bronchospasm (20% and 4%, respectively, compared with 1% in the general population) 3.
Aspirin, 900 to 1,000 mg, is as effective for acute migraine pain as oral sumatriptan (Imitrex), 50 mg.10 Adverse events with aspirin use are generally mild and less common than with the use of sumatriptan, 100 mg 2.
Other Nonselective NSAIDs
Nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit both COX-1 and COX-2, whereas COX-2 selective nonsteroidal anti-inflammatory drugs (NSAIDs) have greater COX-2 selectivity. Inhibition of COX-2 is thought to mediate the analgesic properties of NSAIDs, whereas inhibition of COX-1 appears to be associated with gastrointestinal adverse effects. Nonsteroidal anti-inflammatory drugs (NSAIDs) possess anti-inflammatory effects that are lacking with acetaminophen, and they can be especially useful for the treatment of acute pain associated with prostaglandin-mediated activity, such as dysmenorrhea or osteoarthritis 14.
Because most NSAIDs have nearly identical analgesic effects, the choice is based on cost, dosing schedule, and the frequency or severity of adverse effects. Some NSAIDs (e.g., indomethacin [Indocin], mefenamic acid [Ponstel]) are now rarely used because of adverse effects. Ibuprofen and naproxen are among the most commonly used NSAIDs in the United States because of their effectiveness, adverse effect profile, cost, and over-the-counter availability 14.
There is a ceiling to the analgesic effects of NSAIDs but not to their anti-inflammatory effects, although adverse effects may limit upward dosing titration. NSAIDs are more effective than placebo or acetaminophen for primary dysmenorrhea, but they are associated with a higher incidence of adverse effects such as headache, drowsiness, nausea, and indigestion 14. In general, there are no differences among NSAIDs in terms of effectiveness or adverse effects.
For osteoarthritis, NSAIDs provide significantly better pain relief than acetaminophen, but with more gastrointestinal adverse events 15. Some evidence suggests that NSAIDs and acetaminophen may be comparable for mild osteoarthritis pain, whereas NSAIDs may be better for moderate to severe osteoarthritis pain 15.
Acetaminophen and NSAIDs are equally effective for acute low back pain, although NSAIDs are associated with a higher incidence of adverse effects 16. There is no difference in effectiveness among NSAIDs, narcotic analgesics, and muscle relaxants for acute low back pain 17. Adding a muscle relaxant to an NSAID regimen does not provide further relief for acute low back pain and is associated with more adverse effects 17.
Topical NSAIDs are more effective than placebo for treating acute pain (e.g., from strains, sprains, contusions, or overuse injuries) in superficial locations, and the incidence of local and systemic adverse events is similar to placebo 18. Based on the number needed to treat, topical indomethacin is not as effective as topical diclofenac (Solaraze), ibuprofen, ketoprofen, or piroxicam (not available in the United States), which are similarly effective 18.
COX-2 Selective NSAIDs
Celecoxib is the only COX-2 selective NSAID still available in the United States, where it is approved for bone or dental pain, dysmenorrhea, headache, osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis. Meloxicam (Mobic) is sometimes referred to as a COX-2 selective NSAID but is classified as a nonselective NSAID. COX-2 selective NSAIDs are considered second-line medications for mild to moderate pain because they have similar effectiveness to nonselective NSAIDs but with a greater cost.13 COX-2 selective NSAIDs and traditional NSAIDs are similarly effective for acute low back pain, but COX-2 selective NSAIDs have fewer adverse effects 17.
NSAID side effects
NSAIDs should be used cautiously in several patient populations. Risk factors for gastrointestinal bleeding and peptic ulcer disease associated with NSAID use include a history of gastrointestinal bleeding, peptic ulcer, older age, smoking or alcohol use, and longer duration of NSAID use. Indomethacin and ketorolac should not be used in older adults because of the increased risk of these gastrointestinal adverse effects 19. Concomitant use of NSAIDs and low-dose aspirin is associated with an increased risk of upper gastrointestinal bleeding 20.
Studies of patients with rheumatoid arthritis or osteoarthritis, who were not taking low-dose aspirin and who did not have risk factors for gastrointestinal bleeding or peptic ulcers, have shown that celecoxib, NSAIDs, and acetaminophen have similar analgesic effects 21. Although celecoxib was associated with fewer gastrointestinal effects, the researchers concluded that this relatively small reduction does not justify the extra cost of celecoxib 22. Celecoxib alone and an NSAID plus a proton pump inhibitor (e.g., diclofenac plus omeprazole [Prilosec], naproxen plus lansoprazole [Prevacid]) have the same probability of causing recurrent ulcer bleeding or recurrent gastric or duodenal ulcer complications in those at high risk of these complications 23. However, a cost analysis suggests that in patients 75 years or older with a history of gastrointestinal bleeding or peptic ulcers, celecoxib treatment is less expensive than treatment with an NSAID plus misoprostol (Cytotec) or a proton pump inhibitor 22.
In recent years, the concern about COX-2 selective NSAIDs and, to a lesser extent, nonselective NSAIDs has centered on their cardiovascular adverse effects (i.e., stroke, myocardial infarction, and thrombus formation) 17 and these drugs include an FDA boxed warning regarding these risks. An analysis of six randomized, placebo-controlled trials evaluating the cardiovascular risk associated with celecoxib use showed that the risk increases with dose and that patients with higher baseline cardiovascular risk are more likely to experience a cardiovascular event while taking celecoxib 24. The cardiovascular risk is also thought to be greater with greater COX-2 selectivity (celecoxib > diclofenac > ibuprofen > naproxen) 25.
Renal insufficiency associated with NSAID use is related to inhibition of renal prostaglandin synthesis, which can present as azotemia and hyperkalemia. Use of NSAIDs in patients with impaired renal function, decreased creatinine clearance, or azotemia can result in acute renal failure.
Opiod Combinations
If nonopioid medications such as acetaminophen or NSAIDs do not adequately control pain, the next step of the WHO pain relief ladder includes considering an opioid, with or without a nonopioid 26. Opioids such as hydrocodone and oxycodone are typically combined with acetaminophen or an NSAID. In 2010, hydrocodone/acetaminophen was the most commonly dispensed medication in the United States 27. Opioid combinations are more effective than any one opioid for postoperative pain 16. In a meta-analysis of double-blind randomized controlled trials, patients who received an opioid, such as morphine, with an NSAID had significantly lower pain scores and needed significantly less of the opioid for pain control 28. Adding codeine, 60 mg, to acetaminophen, 600 to 1,000 mg, resulted in only 10% to 15% more patients achieving at least 50% pain relief compared with the same dose of acetaminophen alone 29.
The FDA has been concerned about the potential for acetaminophen-induced hepatic injury 30, and in 2011 requested that manufacturers of prescription products limit the amount of acetaminophen in each dosage unit to no more than 325 mg and to include a boxed warning about the risk of severe hepatic injury 31. This does not affect over-the-counter products, although patients should not exceed 4,000 mg per day and should be cautioned about using prescription and over-the-counter products containing acetaminophen.
Full opioid agonists
Full opioid agonists, such as morphine, are potent analgesics that may be used if opioids combined with acetaminophen or NSAIDs are insufficient to control moderate to severe pain 32. There is a lack of good evidence to suggest any one opioid is more effective or has a better adverse effect profile than morphine 33. The exception is codeine. There is good evidence that codeine is less effective than morphine and other opioid agonists because of its low affinity for opioid receptors 34. Some opioids commonly used in the past are now unavailable (e.g., propoxyphene [Darvon]) or no longer widely used (e.g., meperidine [Demerol], pentazocine [Talwin]).
Adverse effects of opioids include nausea, vomiting, constipation, sedation, pruritus, urinary retention, and respiratory depression. Opioid-induced emesis is mediated by histamine release and can be treated with antihistamines or selective serotonin antagonists (e.g., ondansetron [Zofran]), if needed. Opioids rarely cause gastroparesis, which can present as persistent vomiting. If the opioid cannot be discontinued, opioid-induced gastroparesis can be treated with a gastric motility agent, such as metoclopramide (Reglan). However, caution should be used because metoclopramide can cause extrapyramidal adverse effects. There is no good evidence that adverse effects vary among the different opioids given at equianalgesic doses 35. If the initial opioid does not provide adequate pain relief or the patient experiences intolerable adverse effects, trying an alternative opioid may be reasonable. However, this has not been well studied in acute noncancer pain 36.
Recent clinical guidelines recommend that the duration of opioid agonist therapy be limited if used to relieve low back pain 12. Reassessment, other treatment options, or specialist referral should be considered if the patient’s pain does not improve 12.
Dual-Action Analgesics
Tapentadol (Nucynta), a Schedule 2 controlled substance, is a muopioid receptor agonist and norepinephrine reuptake inhibitor that can be used orally for relief of moderate to severe acute pain. It has similar effectiveness as oxycodone for acute pain, with a significantly lower incidence of nausea, vomiting, and constipation 37. Tapentadol should be used cautiously with serotonergic medications because of the risk of serotonin syndrome.
Tramadol (Ultram) is not federally controlled but is a Schedule IV controlled substance in some states; its designation is currently being reviewed. It is a weak muopioid receptor agonist and a weak inhibitor of norepinephrine and serotonin reuptake in the central nervous system. It is effective for acute pain (e.g., osteoarthritis) in clinical trials, but the benefits are small and it is considered a second-tier medication 38. Among patients presenting to the emergency department with acute musculoskeletal pain, hydrocodone/acetaminophen, 5 mg/500 mg, provided statistically and clinically significant reductions in pain at all time points compared with tramadol, 100 mg 38. Tramadol should be used cautiously, if at all, in patients at risk of seizures.
How do I safely take over-the-counter analgesics?
Read the directions on the label before taking any medicine. Learn how much to take and how often you should take it. If you have any questions about how much medicine to take, call your family doctor or pharmacist. Keep track of which over-the-counter (OTC) medicines you are using and when you take them. If you need to go to the doctor, take this list with you.
Follow these tips to make sure you are taking the right amount of medicine:
- Take only the amount recommended on the medicine’s label. Don’t assume that more medicine will work better or quicker. Taking more than the recommended amount can be dangerous.
- If you are taking a prescription medicine, ask your doctor if it’s okay to also take an OTC analgesic.
- Don’t use more than 1 OTC analgesic at a time unless your doctor says it’s okay. They may have similar active ingredients. These could add up to be too much medicine.
- Check whether other OTC medicines you are taking contain acetaminophen. For example, many combination medicines for cold symptoms contain this active ingredient. Taking too much acetaminophen can cause health problems.
Topical analgesic
Only few topical analgesic formulations have become available for clinical use, and among these, analgesic creams are still rare. Such formulations are said to be effective, without troublesome local or systemic side effects, and various formulations such as patches, creams, and gels have become available for the prescribing physician. Most of these formulations deliver drugs systemically to act as transdermal delivery systems, whereas lidocaine patches and capsaicin cream and patches mainly act locally without causing any direct systemic effect.
Lidocaine
Lidocaine is a local anesthetic (numbing medication). Lidocaine works by blocking nerve signals in your body. Lidocaine topical (for use on the skin) is used to reduce pain or discomfort caused by skin irritations such as sunburn, insect bites, poison ivy, poison oak, poison sumac, and minor cuts, scratches, or burns. Lidocaine topical is also used to treat rectal discomfort caused by hemorrhoids. Lidocaine applied to the skin is not likely to cause an overdose unless you apply more than the recommended dose. An overdose of numbing medicine can cause fatal side effects if too much of the medicine is absorbed through your skin and into your blood. Overdose symptoms may include uneven heartbeats, seizure (convulsions), slowed breathing, coma, or respiratory failure (breathing stops).
Lidocaine topical comes in many different forms (gel, spray, cream, lotion, ointment, liquid, skin patch). Improper use of lidocaine topical may result in death.
Lidocaine topical side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have:
- severe burning, stinging, or irritation where the medicine was applied;
- swelling or redness;
- sudden dizziness or drowsiness after medicine is applied;
- confusion, blurred vision, ringing in your ears; or
- unusual sensations of temperature.
Common side effects include:
- mild irritation where the medication is applied; or
- numbness in places where the medicine is accidentally applied.
Capsaicin
Capsaicin cream or patches is a topical analgesic derived from chili peppers that makes them hot that is also a primary ingredient in prescription or over-the-counter pain-relieving creams available as a treatment for a number of pain conditions. Capsaicin topical is used for temporary relief of muscle or joint pain caused by strains, sprains, arthritis, bruising, or backaches. Capsaicin topical is also used to treat nerve pain (neuralgia) in people who have had herpes zoster, or “shingles.” Capsaicin topical cream may be particularly good for deep pain. It works by reducing the amount of substance P found in nerve endings and interferes with the transmission of pain signals to the brain. Individuals can become desensitized to the capsaicin compound, however, perhaps because of long-term capsaicin-induced damage to nerve tissue.
Some individuals find the burning sensation they experience when using capsaicin cream to be intolerable, especially when they are already suffering from a painful condition, such as postherpetic neuralgia, which occurs in some people after a bout of shingles. Soon, however, better treatments that relieve pain by blocking vanilloid receptors (also called capsaicin receptors) may arrive in drugstores. Capsaicin cream has been found to be superior to placebo in treating osteoarthritis pain. Capsaicin cream or patches is widely available, is relatively inexpensive, and can be used as an adjunct to standard osteoarthritis treatments 39.
Do not use capsaicin topical if you are allergic to chili peppers, or if you have ever had an allergic reaction to capsaicin topical.
It is not known whether capsaicin topical will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant while using this medication.
It is not known whether capsaicin topical passes into breast milk or if it could harm a nursing baby. Do not apply capsaicin topical to your breast area if you are breast-feeding a baby.
Do not use capsaicin topical on anyone younger than 18 years old without the advice of a doctor.
How should I use capsaicin topical?
Use exactly as directed on the label, or as prescribed by your doctor. Do not use in larger or smaller amounts or for longer than recommended.
Do not take by mouth. Topical medicine is for use only on the skin.
Do not use capsaicin topical on open wounds or on sunburned, windburned, dry, chapped, or irritated skin. If this medicine gets in your eyes, nose, mouth, rectum, or vagina, rinse with water.
Make sure your skin is clean and dry before you apply capsaicin topical.
When using the cream or lotion, apply a thin layer to the affected area and rub in gently until completely absorbed.
To use the liquid or stick, uncap the applicator and press it firmly on your skin to apply the medication. Massage gently onto the affected are until completely absorbed.
Capsaicin topical may be used up to 4 times daily or as directed on the medicine label.
To apply a capsaicin topical skin patch, remove the liner and apply the patch to your skin over the area of pain. Press the edges firmly into place. Remove the patch and apply a new patch 1 or 2 times daily if needed.
Wash your hands with soap and water immediately after applying capsaicin topical or handling the skin patch. If you have applied the medicine to your hands or fingers to treat pain in those areas, wait at least 30 minutes before washing your hands.
To keep the medication from getting on your fingers when you apply it, you may use a rubber glove, finger cot, cotton ball, or clean tissue to apply the medicine.
Capsaicin can cause a burning sensation wherever it is applied. This sensation is usually mild and should gradually lessen over time with continued regular use of the medicine.
If the burning sensation is painful or causes significant discomfort, wash the treated skin area with soap and cool water. Get medical attention right away if you have severe burning, pain, swelling, or blistering.
Do not cover treated skin with a bandage or heating pad, which can increase the burning sensation. You may cover the skin with clothing.
Avoid taking a bath or shower within 1 hour before or after you apply capsaicin to your skin. Also avoid swimming or vigorous exercise. Warm water or perspiration can increase the burning sensation caused by capsaicin.
Avoid getting capsaicin topical in your eyes or near your nose where you might inhale it. If it does get into any of these areas, rinse thoroughly with water.
Also avoid getting this medication on contact lenses, dentures, and other items that come into contact with sensitive areas of your body.
It may take up to 2 weeks of using this medicine regularly before your symptoms improve. For best results, keep using the medication as directed. Pain relief should occur gradually as the substance P in your body is decreased in the nerve cells.
Call your doctor if your pain does not improve after using this medication for 7 days, or if your symptoms get worse or get better and then come back in a few days.
Store capsaicin topical at room temperature away from moisture and heat, in a place where children and pets cannot get to it.
Capsaicin topical liquid is flammable. Do not use or store near fire or open flame.
Capsaicin topical side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Wash the skin and get medical attention right away if you have severe burning, pain, swelling, or blistering of the skin where you applied this medication.
Stop using capsaicin topical and call your doctor at once if you have:
- skin redness where the medicine was applied; or
- trouble breathing or swallowing (after accidental inhalation of capsaicin odor or dried residue).
Less serious side effects may include a mild burning sensation that can last for several hours or days, especially after your first use of capsaicin topical.
This is not a complete list of side effects and others may occur.
Topical nonselective nonsteroidal anti-inflammatory drugs (NSAIDs)
Topical nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) are more effective than placebo for treating acute pain (e.g., from strains, sprains, contusions, or overuse injuries) in superficial locations, and the incidence of local and systemic adverse events is similar to placebo 18. Based on the number needed to treat, topical indomethacin is not as effective as topical diclofenac (Solaraze), ibuprofen, ketoprofen, or piroxicam (not available in the United States), which are similarly effective 18.
References- Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Acute pain management. 3rd ed. 2010. http://www.anzca.edu.au/fpm/resources/books-and-publications/publications-1/Acute Pain – final version.pdf. Accessed March 15, 2013.
- Derry S, Moore RA. Single dose oral aspirin for acute postoperative pain in adults. Cochrane Database Syst Rev. 2012;(4):CD002067.
- Pharmacologic Therapy for Acute Pain. Am Fam Physician. 2013 Jun 1;87(11):766-772. https://www.aafp.org/afp/2013/0601/p766.html
- IASP Terminology. http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698
- Hudson TJ, Edlund MJ, Steffick DE, Tripathi SP, Sullivan MD. Epidemiology of regular prescribed opioid use: results from a national, population-based survey. J Pain Symptom Manage. 2008;36(3):280-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4741098/
- U.S. Department of Health and Human Services. Results from the 2010 National Survey on Drug Use and Health: summary of national findings. September 2011.
- Canfield MC, Keller CE, Frydrych LM, Ashrafioun L, Purdy CH, Blondell RD. Prescription opioid use among patients seeking treatment for opioid dependence [published correction appears in J Addict Med. 2011;5(1):86]. J Addict Med. 2010;4(2):108–113.
- Where and How to Dispose of Unused Medicines. https://www.fda.gov/forconsumers/consumerupdates/ucm101653.htm
- Sweetman SC, editor. Martindale: The complete drug reference. 36th ed. London: Pharmaceutical Press; 2009.
- Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database Syst Rev. 2008;(4):CD004602.
- Henrich WL, Agodoa LE, Barrett B, et al. Analgesics and the kidney: summary and recommendations to the Scientific Advisory Board of the National Kidney Foundation from an Ad Hoc Committee of the National Kidney Foundation. Am J Kidney Dis. 1996;27(1):162–165.
- Chou R, Qaseem A, Snow V, et al.; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society [published correction appears in Ann Intern Med. 2008;148(3):247–248]. Ann Intern Med. 2007;147(7):478–491.
- Carvajal A, Prieto JR, Alvarez Requejo A, Martin Arias LH. Aspirin or acetaminophen? A comparison from data collected by the Spanish Drug Monitoring System. J Clin Epidemiol. 1996;49(2):255–261.
- Marjoribanks J, Proctor M, Farquhar C, Derks RS. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2010;(1):CD001751
- Towheed TE, Maxwell L, Judd MG, Catton M, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. 2006;(1):CD004257
- Gaskell H, Derry S, Moore RA, McQuay HJ. Single dose oral oxycodone and oxycodone plus paracetamol (acetaminophen) for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;(3):CD002763
- Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tulder MW. Nonsteroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2008;(1):CD000396
- Massey T, Derry S, Moore RA, McQuay HJ. Topical NSAIDs for acute pain in adults. Cochrane Database Syst Rev. 2010;(6):CD007402
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–631.
- Sørensen HT, Mellemkjaer L, Blot WJ, et al. Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin. Am J Gastroenterol. 2000;95(9):2218–2224.
- Deeks JJ, Smith LA, Bradley MD. Efficacy, tolerability, and upper gastrointestinal safety of celecoxib for treatment of osteoarthritis and rheumatoid arthritis: systematic review of randomised controlled trials. BMJ. 2002;325(7365):619.
- Simon LS, Weaver AL, Graham DY, et al. Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA. 1999;282(20):1921–1928.
- Lai KC, Chu KM, Hui WM, et al. Celecoxib compared with lansoprazole and naproxen to prevent gastrointestinal ulcer complications. Am J Med. 2005;118(11):1271–1278.
- Solomon SD, Wittes J, Finn PV, et al.; Cross Trial Safety Assessment Group. Cardiovascular risk of celecoxib in 6 randomized placebo-controlled trials: the cross trial safety analysis. Circulation. 2008;117(16):2104–2113
- Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115(12):1634–1642.
- WHO’s cancer pain ladder for adults. http://www.who.int/cancer/palliative/painladder/en/
- Bartholow M. Pharmacy Times. Top 200 drugs of 2010. May 16, 2011.
- Jirarattanaphochai K, Jung S. Nonsteroidal antiinflammatory drugs for postoperative pain management after lumbar spine surgery: a meta-analysis of randomized controlled trials. J Neurosurg Spine. 2008;9(1):22–31
- Toms L, Derry S, Moore RA, McQuay HJ. Single dose oral paracetamol (acetaminophen) with codeine for postoperative pain in adults. Cochrane Database Syst Rev. 2009;(1):CD001547
- U.S. Food and Drug Administration. June 29–30, 2009: joint meeting of the Drug Safety and Risk Management Advisory Committee with the Anesthetic and Life Support Drugs Advisory Committee and the Nonprescription Drugs Advisory Committee: meeting announcement.
- U.S. Food and Drug Administration. FDA drug safety communication: prescription acetaminophen products to be limited to 325 mg per dosage unit; boxed warning will highlight potential for severe liver failure.
- Toms L, Derry S, Moore RA, McQuay HJ. Single dose oral paracetamol (acetaminophen) with codeine for postoperative pain in adults. Cochrane Database Syst Rev. 2009;(1):CD001547.
- Quigley C. Clinical Evidence. Opioids in people with cancer-related pain. July 31, 2008. http://www.clinicalevidence.bmj.com/x/systematic-review/2408/archive/07/2008.html
- Reisine T, Pasternak G. Opioid analgesics and antagonists. In: Goodman LS, Gilman AG, Hardman JG, Limbird LE, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: McGraw-Hill; 1996.
- McQuay H, Moore A, Justins D. Treating acute pain in hospital. BMJ. 1997;314(7093):1531–1535.
- Quigley C. Opioid switching to improve pain relief and drug tolerability. Cochrane Database Syst Rev. 2004;(3):CD004847.
- Hartrick CT, Rozek RJ. Tapentadol in pain management: a μ-opioid receptor agonist and noradrenaline reuptake inhibitor. CNS Drugs. 2011;25(5):359–370.
- Turturro MA, Paris PM, Larkin GL. Tramadol versus hydrocodone-acetaminophen in acute musculoskeletal pain: a randomized, double-blind clinical trial. Ann Emerg Med. 1998;32(2):139–143.
- Ernst E. Complementary treatments in rheumatic diseases. Rheum Dis Clin North Am. 2008;34(2):455–467.