Angina bullosa haemorrhagica
Angina bullosa haemorrhagica also called angina bullosa hemorrhagica or angina bullosa haemorrhage, is the term used to describe benign subepithelial, often painful, tense blood-filled blister or blisters that develop in the mouth that are not attributable to a systemic disorder or hemostatic defect (blood dyscrasia) 1. Angina means painful, bullosa is a blister and haemorrhagica means blood-filled. Angina bullosa haemorrhagica is a very rare condition. Lesions of angina bullosa haemorrhagica occur mainly on the soft palate. Elderly patients are usually affected and lesions heal spontaneously without scarring. The pathogenesis is unknown, although it may be a multifactorial phenomenon. Trauma seems to be the major provoking factor and long-term use of steroid inhalers has also been implicated in the disease. The diagnosis of the lesion is very important as a rapidly expanding blood-filled bulla in the oropharynx can cause upper airway obstruction.
The management of a patient presenting with oral blood-filled bullae should start with a detailed medical history and careful examination to differentiate angina bullosa haemorrhagica from other more serious diseases 1. The lesion should be biopsied to perform histology and direct immunofluorescence in order to exclude more serious diseases. A complete blood count and baseline coagulation tests should always be performed to exclude blood disorders. The patient should be reassured of the benign nature of the blisters. A large palatal or pharyngeal blister causing a choking sensation should be surgically treated if still intact. Management of angina bullosa haemorrhagica should be symptomatic. Long-term follow-up is recommended to positively exclude other conditions which may present with oral blood containing bullae.
Angina bullosa haemorrhagica causes
Angina bullosa haemorrhagica pathogenesis is unknown, although it may be a multifactorial phenomenon 2. Angina bullosa haemorrhage possible causative factors include trauma caused by eating, hot drinks, dental procedures or shouting, long-term use of topical or inhaled steroids, diabetes and hereditary predilection.
Other conditions which may need consideration include mucous membrane pemphigoid, bullous pemphigoid, lichen planus, epidermolysis bullosa, dermatitis herpetiformis, linear IgA disease and oral amyloidosis.
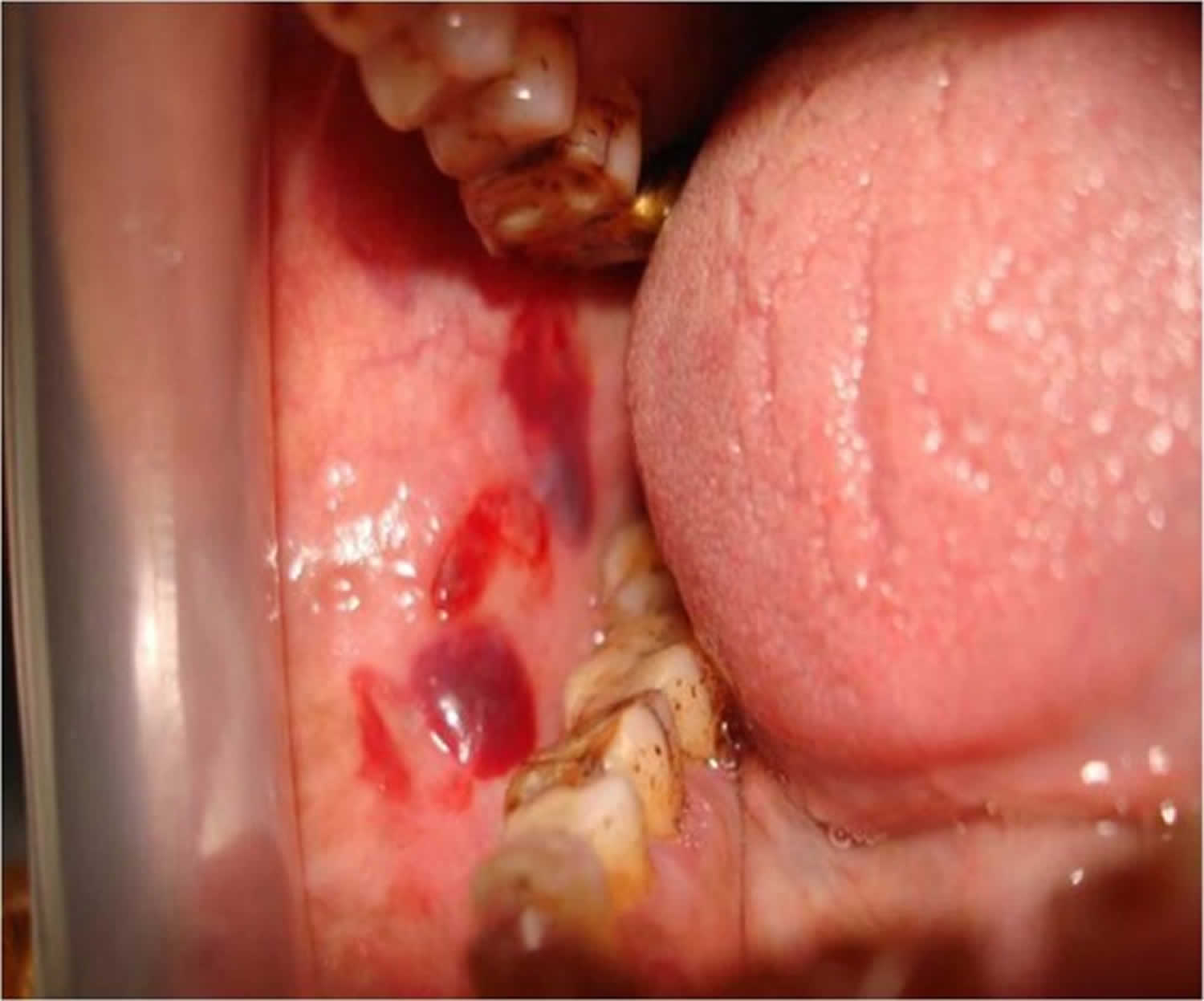
In the largest published series of 30 patients, no precipitating factor was found in 47% 3. Pahl and colleagues 4 reported a case of postoperative angina bullosa haemorrhagica caused by intubation and extubation, describing a patient with a single blister at the junction of the soft and hard palate, which did not compromise the patient’s airway. Lesions predominantly occur on the soft palate. The intact bulla is red to purple in color. Blisters usually reach 2–3 cm in diameter and burst spontaneously, leaving ragged ulcers that heal without scarring. Clinically, the lesions may recur.
Angina bullosa haemorrhagica symptoms
The soft palate is the most common site of angina bullosa haemorrhage. Other sites inside the mouth may be involved. There is usually a solitary lesion. Multiple blisters may develop. The blisters usually rupture spontaneously and the sites heal uneventfully.
Angina bullosa haemorrhagica diagnosis
The diagnosis of angina bullosa haemorrhagica is largely clinical, and includes the elimination of other disease processes at histology. No investigations are usually needed unless the other medical conditions (e.g., bleeding disorders, liver disease, diabetes) need to be excluded. Lesions of angina bullosa haemorrhagica can be easily confused with those occurring in many dermatological and systemic disorders. Even if there is a typical history of rapid blistering, the absence of any dermatological, haematological or systemic sign and normal healing of the ulcers generally lead to a diagnosis of angina bullosa haemorrhagica. Patients with bleeding disorders (thrombocytopenia and von Willebrand’s disease) can present with intraoral blood-filled lesions but a haemostatic function test will distinguish between these conditions 5.
The absence of desquamative gingivitis and nasal or conjunctival mucosal involvement will differentiate it from benign mucous membrane pemphigoid 6. Linear IgA disease and dermatitis herpetiformis usually can be differentiated by the presence of a pruritic rash. In oral bullous lichen, planus bullae are often associated with a striated pattern. The target-like lesion of the skin in erythema multiforme helps to distinguish it 7. The haemorrhagic bullae found in amylodosis are usually persistent and other clinical features include macroglossia and petechiae 8. Epidermolysis bullosa can be differentiated by the presence of bullous skin lesions.
Skin antibodies may be measured. If a biopsy is taken in angina bullosa haemorrhagica, a blister will be found under the mucosa (lining of the mouth). This contains red blood cells and sparse inflammatory cells.
The histopathological features of angina bullosa haemorrhagica include the parakeratotic epithelium with a subepithelial separation from the underlying lamina propria. Superficially located vesicles filled with erythrocytes and fibrin are seen. The inflammatory cell infiltrate, when present, consists primarily of lymphocytes. Neutrophils and eosinophils seen in other blistering disorders are not present. Immunofluorescence demonstrates no evidence of IgG, IgM, IgA or C3 antibodies within the epithelium or the basement membrane zone 9.
Angina bullosa haemorrhagica treatment
No treatment is usually necessary other than a mild analgesic and/or a simple mouth wash. Long-term follow-up is recommended to positively exclude other conditions which may present with oral blood containing bullae.
References- Singh D, Misra N, Agrawal S, Misra P. Angina bullosa haemorrhagica. BMJ Case Rep. 2013;2013:bcr2012008505. Published 2013 Feb 8. doi:10.1136/bcr-2012-008505 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3604492
- Giuliani M, Favia GF, Miani CM. Angina bullosa haemorrhagica: presentation of eight new cases and a review of the literature. Oral Dis 2002;8:54–8
- Stephenson P, Lamey P-J, Scully C, et al. Angina bullosa haemorrhagica: a report of three cases and review of the litreture. Clin Exp Dermatol 1990;15:422–4
- Pahl C, Yarrow S, Steventon N, et al. Angina bullosa haemorrhagica presenting as acute upper airway obstruction. Br J Anaesth 2004;92:283–6
- Korman N. Bullous pemphigoid. J Am Acad Dermatol 1987;16:907–24
- Neville BW, Damm DD, Allen CM, et al. Oral & maxillofacial pathology. 2nd edn St. Louis, MO: Saunders Elsiever, 2008
- Gonçalves LM, Bezerra Júnior JR, Cruz MC. Clinical evaluation of oral lesions associated with dermatologic diseases. An Bras Dermatol 2010;85:150–6
- Schwartz HC, Olson DJ. Amyloidosis: a rational approach to diagnosis by intraoral biopsy. Oral Surg Oral Med Oral Pathol 1975;39:837–43
- Curran AE, Rives RW. Angina bullosa haemorrhagica: an unusual problem following periodontal yherapy. J Periodontol 2000;71:1770–3