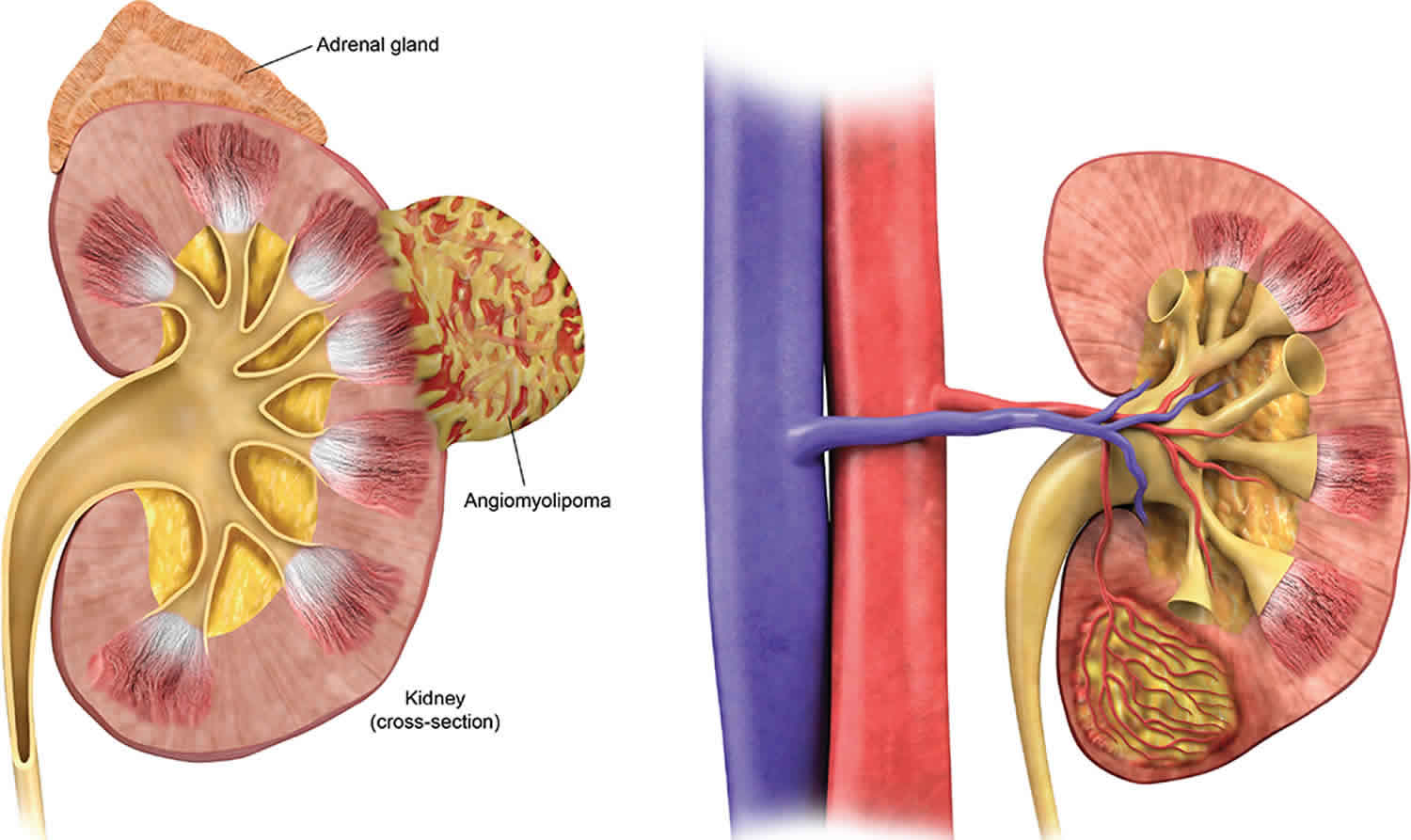
What is angiomyolipoma
Angiomyolipoma also called renal angiomyolipoma is the most common benign solid renal lesion and also the most common fat-containing lesion of the kidneys 1. Renal angiomyolipomas are considered one of a number of tumors with perivascular epitheloid cellular differentiation (PEComas) and are composed of vascular, smooth muscle and fat elements. There are two types of renal angiomyolipoma: isolated angiomyolipoma and angiomyolipoma that is associated with tuberous sclerosis. Isolated angiomyolipoma occurs sporadically. It is often solitary and accounts for 80% of the angiomyolipomas 2. The incidence of isolated angiomyolipoma in the general population is estimated to be 0.13%, and it is about 4 times more common in women than in men 3. The mean age at presentation of patients with isolated angiomyolipoma is 43 years 4. Interestingly, 80% of the cases involve the right kidney 2. Risk of life threatening hemorrhage is the main clinical concern. Due to the fat content, angiomyolipomas are generally readily identifiable on computerized tomography and magnetic resonance imaging 5. However, fat poor angiomyolipoma can present a diagnostic challenge. Novel research suggests that various strategies using magnetic resonance imaging (MRI), including chemical shift magnetic resonance imaging, have the potential to differentiate fat poor angiomyolipoma from renal cell carcinoma. Active surveillance is the accepted management for small asymptomatic masses. Generally, symptomatic masses and masses greater than 4 cm should be treated. However, other relative indications may apply.
Two histological renal angiomyolipoma types have been described:
- typical (triphasic)
- atypical (monophasic or epithelioid)
A special variant called an epithelioid angiomyolipoma is composed of more plump, epithelial-looking cells, often with nuclear atypia, that have a described risk of malignant behavior. This variant, unlike conventional angiomyolipomas, may mimic renal cell carcinoma 6. Metastases have also been described 7.
Renal angiomyolipoma that is associated with tuberous sclerosis complex accounts for 20% of angiomyolipomas, although they have also been described in the setting of von Hippel-Lindau syndrome (vHL) and neurofibromatosis type 1 (NF1) 8. The lesions are typically larger than isolated angiomyolipomas, and they are often bilateral and multiple 9 and is associated with potentially life-threatening complications 10. Tuberous sclerosis complex is an autosomal dominant genetic disease characterized by growth of benign tumors (hamartomas) in multiple organs, especially the kidneys, brain, heart, lungs, and skin 11. Tuberous sclerosis complex is usually caused by a mutation in either the tuberous sclerosis complex 1 (9q34) or tuberous sclerosis complex 2 (16p13) gene, resulting in constitutive activation of mammalian target of rapamycin signaling. The majority of patients with tuberous sclerosis complex (80%) can develop angiomyolipoma.
The estimated prevalence of angiomyolipoma with tuberous sclerosis complex varied between studies and ranged from 55% to 80%. Some studies showed a higher proportion of renal angiomyolipoma in females 12, whereas others have shown no gender disparity 13. Patients with tuberous sclerosis complex-2 (TSC 2) mutations have been reported to exhibit a higher incidence and severity of angiomyolipoma compared with patients with tuberous sclerosis complex-1 (TSC 2) mutations 12. Patients with tuberous sclerosis complex-associated renal angiomyolipoma are susceptible to spontaneous life-threatening bleeding 14. Large angiomyolipomas (>3–4 cm in diameter) may develop a vascular aneurysm and life-threatening hemorrhage or compress normal kidney tissue, potentially leading to kidney failure. These complications are especially common when the renal lesions are rapidly growing 11.
Currently, mammalian target of rapamycin inhibitors (mTOR) are recommended in adult patients with tuberous sclerosis complex for the treatment of asymptomatic, growing renal angiomyolipoma that are >3 cm in diameter and pediatric or adult patients with brain lesions (subependymal giant cell astrocytoma) that either are growing or are not amenable to surgical resection 11. Clinical evidence suggests that systemic administration of a mammalian target of rapamycin inhibitor may provide concurrent improvements in multiple lesions and symptoms of tuberous sclerosis complex 11.
Most patients with a solitary renal angiomyolipomas do not have tuberous sclerosis complex. Treatment of these idiopathic angiomyolipomas with mTOR inhibition in this setting is neither suggested nor US Food and Drug Administration (FDA) approved. Furthermore, not every patient with tuberous sclerosis complex and renal angiomyolipomas will need to be started on mTOR inhibitor therapy at diagnosis. Rather, clinical follow-up and monitoring for lesion growth, hypertension, proteinuria, or the development of renal disease are the cornerstones of nephrology care 15. As these lesions grow, initiation of treatment is indicated. Many patients may be treated successfully with an mTOR inhibitor if side effects are managed appropriately.
Clinical monitoring of patients on active therapy consists of regular office visits with routine laboratory checks. Although frequent follow-up is warranted on initiation of therapy to assess side effects and assure safe provision of therapy, after lesions have shrunk and patients remain on a maintenance phase of treatment, follow-up visits can be spaced out. Timing of imaging should be individualized, although annual imaging with magnetic resonance imaging is likely sufficient for most patients on maintenance therapy 15.
Although most of the lesion shrinkage occurs within the first year of therapy initiation, continued small reductions in lesion size are possible beyond the first year. Lesions do not generally disappear altogether on imaging but instead, shrink and then stabilize. Unlike oncology care, where the goal of treatment is to rid the patient of every last vestige of tumor cells, in angiomyolipoma, small stable lesions are not a problem for long-term survival or symptom relief. Although there is evidence that halting treatment with an mTOR inhibitor will likely lead to regrowth of the angiomyolipomas 16, whether reduction in the dose of an mTOR inhibitor is possible after lesions have reached a small stable size is unclear.
Angiomyolipoma symptoms
Most renal angiomyolipoma patients are usually asymptomatic and the diagnosis of kidney angiomyolipoma is often found incidentally when the kidneys are imaged for other reasons or as part of screening in patients with tuberous sclerosis. Symptomatic presentation is most frequently with spontaneous retroperitoneal hemorrhage. The classical triad of symptoms characterized by flank pain, palpable mass, and hematuria appeared in less than half of the individuals 17. The main complication of renal angiomyolipoma is retroperitoneal hemorrhage caused by tumor rupture, which can be severe and life threatening. Acute bleeding of angiomyolipoma manifest as Lenk’s triad, including acute flank pain, abdominal tenderness, and signs of internal bleeding such as hematuria; this urological emergency is also called Wünderlich syndrome 18. Currently, the risk of angiomyolipoma rupture is usually determined by tumor size and surgical approach is necessary for tumor size >4 to 8 cm 19.
Some patients may present with numerous other symptoms and signs 20, e.g. palpable mass, flank pain, urinary tract infections, hematuria, renal failure, or hypertension 21.
Angiomyolipoma diagnosis
The cornerstone of diagnosis of kidney angiomyolipoma on all modalities is the demonstration of macroscopic fat, however in the setting of hemorrhage, or when the renal angiomyolipoma happen to contain little fat, it may be difficult to distinguish an angiomyolipoma from a renal cell carcinoma.
Ultrasound
- tend to appear as hyperechoic lesions on ultrasound, located in the cortex and with posterior acoustic shadowing
- in the setting of tuberous sclerosis, they may be so numerous that the entire kidney is affected, appearing echogenic with the loss of normal corticomedullary differentiation 22
- contrast-enhanced ultrasound 23
- tend to enhance peripherally
- decreased central enhancement, compared with normal cortex
Figure 1. Angiomyolipoma ultrasound
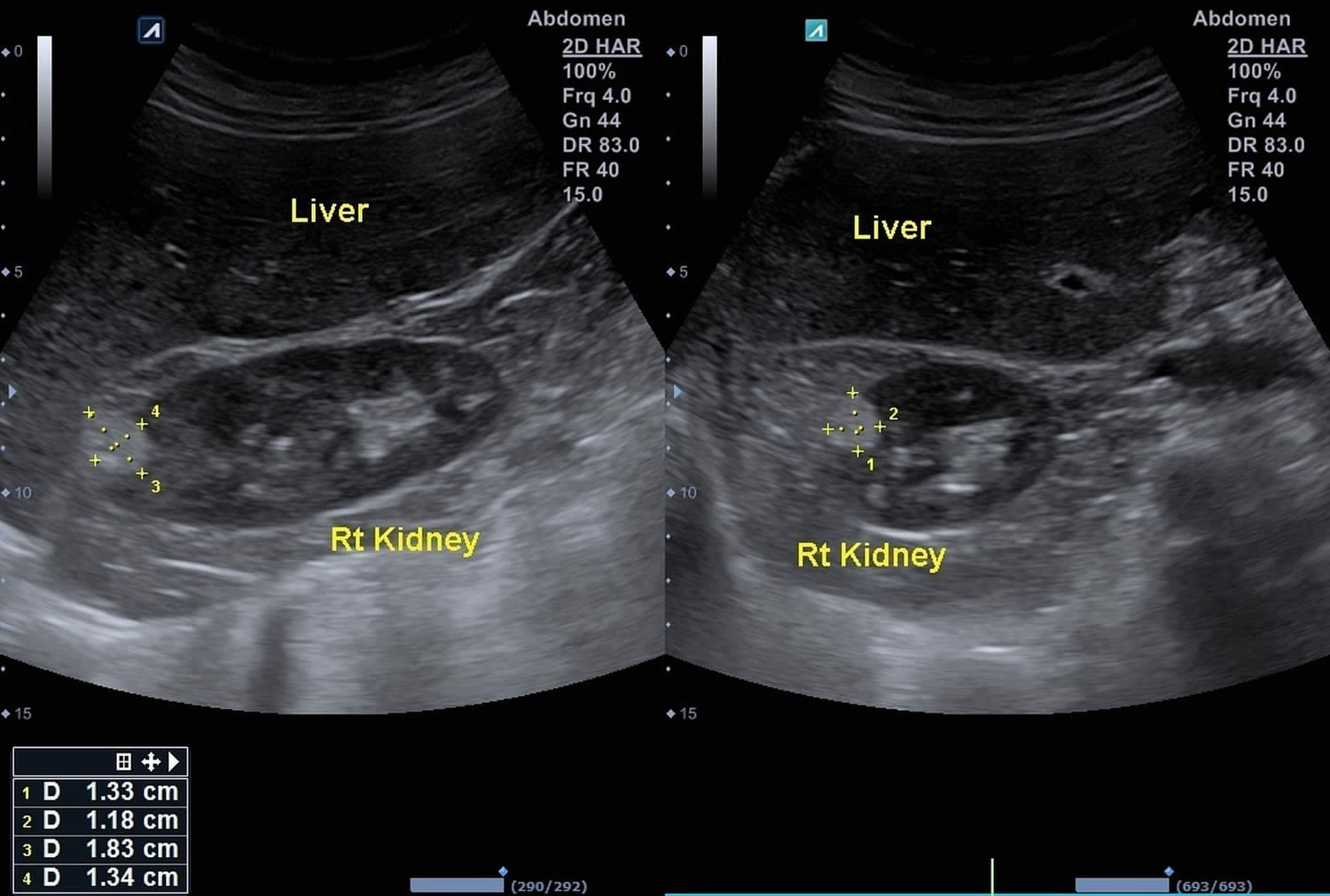
Footnote: Female presented with abdominal discomfort. Renal ultrasound showed hyperechoic, cortical renal masses in both kidneys.
[Source 24 ]CT
Most lesions involve the cortex and demonstrate macroscopic fat (less than -20 HU). When small, volume averaging may make differentiation from a small cyst difficult.
It is important to realize that ~5% of angiomyolipomas are fat-poor 25. This is especially the case in the setting of tuberous sclerosis, where up to a third do not demonstrate macroscopic fat on CT 26. Calcification is rare.
MRI
MRI is excellent at evaluating fat-containing lesions, and two main set of sequences are employed. Firstly, and traditionally if you will, fat saturated techniques demonstrate high signal intensity on non-fat-saturated sequences and loss of signal following fat saturation.
The second method is to use in-phase and out-of-phase imaging which generates India ink artifact at the interface between fat and non-fat components. This can occur either at the interface between the angiomyolipoma and surrounding kidney or between fat and non-fat components of the mass 8. Chemical shift signal intensity loss, along with other features, may suggest a fat-poor angiomyolipoma 25.
It is essential to remember that rarely renal cell carcinomas may have macroscopic fat components and as such the presence of fat is strongly indicative of an angiomyolipoma, but not pathognomonic. Since macroscopic fat in renal cell carcinoma almost always occurs in the presence of ossification/calcification, absence of ossification/calcification on imaging is in favor of angiomyolipoma.
DSA – angiography
Angiomyolipomas are hypervascular lesions demonstrating often characteristic features:
- arterial phase: a sharply marginated hypervascular mass with a dense early arterial network, and tortuous vessels giving the “sunburst” appearance
- venous phase: whorled “onion peel” appearance of peripheral vessels
- micro- or macro-aneurysms 20
- absent arteriovenous shunting
Angiomyolipoma treatment
Angiomyolipomas found incidentally usually require no therapy (when small), although follow-up is recommended to assess for growth. Small solitary angiomyolipomas (<20 mm) probably do not require follow-up due to their slow growth 27.
Larger angiomyolipomas, or those that have been symptomatic, can be electively embolized and/or resected with a partial nephrectomy.
The traditional convention is that intervention is considered when an angiomyolipoma reaches 40 mm in size 28.
Lesions that present with retroperitoneal hemorrhage often requires emergency embolization as a life-saving measure.
mTOR inhibitors (e.g. everolimus) have been shown to significantly decrease angiomyolipoma size and may help to preserve renal function in tuberous sclerosis patients.
Current guidelines recommend periodic clinical and radiographic assessments of the kidney in patients with tuberous sclerosis complex 15. Abdominal imaging should be performed at diagnosis and every 1–3 years throughout a patient’s lifetime. Magnetic resonance imaging (MRI) is the preferred modality to follow renal lesions. In addition, blood pressure should be measured and followed closely, because the risk of hypertension increases with increasing burden of kidney lesions. Although angiotensin-converting enzyme inhibitors are often used in the management of hypertension, caution must be used in patients taking mTOR inhibitors, because the combination may lead to increased risk of angioedema 15. Control of blood pressure is important to slow progression of chronic kidney disease and avoid cardiovascular complications.
Additionally, patients with tuberous sclerosis complex-associated kidney lesions should have renal function monitored at least yearly, including eGFR and urinalysis to assess for the development of proteinuria, another common finding among those with kidney lesions 15. The most common method of estimating GFR includes measurement of serum creatinine levels, although cystatin C may be appropriate in certain situations. The presence of proteinuria and hypertension, both markers and causes of progression in renal damage, can help clinicians determine the frequency with which laboratory monitoring and imaging are indicated.
In the new guidelines, there has been a major paradigm shift toward screening at diagnosis to ascertain the extent of the disease and organ involvement, with ongoing monitoring for disease progression and emergence of new manifestations 15. For patients with kidney disease, subsequent close and regular monitoring of kidney function by a nephrologist is particularly important, because unlike some other manifestations of tuberous sclerosis complex, angiomyolipoma and other renal lesions may appear later in life and accumulate with time, necessitating lifelong follow-up of patients 15. With this management approach, it is important that every patient with tuberous sclerosis complex is seen and monitored by a nephrologist.
After intervention is required, treatment with an mTOR inhibitor or embolization should be considered. Medical therapy with an mTOR inhibitor has only recently become an option. Before the 2012 approval of everolimus, surgical resection or intravascular embolization was the standard of care for most hamartomas that needed medical intervention 29. Because hamartomas treated with surgery may recur in remaining kidney tissue if total resection is not achieved 30, total or partial nephrectomy should be avoided for angiomyolipomas in patients with tuberous sclerosis complex 15. Surgery may lead to loss of healthy tissue and compromise kidney function, and growth of new angiomyolipomas is likely in the remaining kidney 31. The 2012 consensus guidelines specifically state that “nephrectomy is to be avoided because of the high incidence of complication and increased risk of future renal insufficiency, end-stage renal failure, and the poor prognosis that results from chronic kidney disease” 29. Given these many risks of nephrectomy in this population, embolization of the lesion’s vascular supply became a standard of care; however, embolization does not address the underlying cause of tuberous sclerosis complex, and continued growth is likely to occur. The consensus guidelines from 2012 now recommend mTOR inhibitors as first-line treatment for asymptomatic angiomyolipoma ≥3 cm in diameter, with embolization and partial resection reserved as second-line options 29.
The mTOR inhibitor everolimus has been approved by the US Food and Drug Administration (FDA) for use in patients in the United States with tuberous sclerosis complex, specifically treatment of adults with renal angiomyolipomas that do not require immediate surgery. Sirolimus, the other mTOR inhibitor, has been assessed in treating tuberous sclerosis complex-associated angiomyolipomas and SEGAs but is not FDA approved for this use 32. In an open label trial of patients with angiomyolipoma, 12 months of treatment with sirolimus resulted in most patients having reduction in angiomyolipoma size; however, lesions began to regrow after treatment discontinuation 16. The importance of sustained treatment in maintaining reductions in angiomyolipoma volumes was emphasized in a longer 2-year trial of sirolimus, in which angiomyolipoma response was maintained by continuing therapy, with little further shrinkage during the second year of treatment 32. Reductions in angiomyolipomas and regression of SEGAs were also observed in a separate open label sirolimus study in 36 adults with tuberous sclerosis complex or angiomyolipoma with at least one angiomyolipoma ≥2 cm in diameter who received daily sirolimus for up to 1 year. The overall angiomyolipoma response rate was 44% (all partial responses), and among 13 patients with measureable SEGA at baseline, tumor regression was observed in seven patients 33.
There are some commonly reported adverse events associated with mTOR inhibitor therapy that should be noted. These include stomatitis/mucositis, respiratory infection, diarrhea, hypertriglyceridemia, hypercholesterolemia, bone marrow suppression (anemia, mild neutropenia, and leukopenia), proteinuria, and joint pain 33. Monitoring of patients on active therapy includes early follow-up to assess for bothersome side effects, most notably mouth sores. By preparing patients for their occurrence, addressing side effects quickly, and managing expectations, most patients can be successfully continued on active therapy, despite occasional discomfort. Because many of these side effects seem linked to mTOR drug level, monitoring of drug levels when therapy is initiated or after dose alteration may reduce their likelihood or severity. Dose interruptions and subsequent adjustments of the mTOR inhibitor may also help reduce systemic side effects. Additionally, because hyperlipidemia is a common side effect of these treatments, prescribing clinicians should be comfortable with the use of statins or should be prepared to refer patients for this management. Because wound healing may be delayed, treatment should be interrupted in the perioperative period of any surgery.
As a result of the initial promising studies, the mTOR inhibitor everolimus was evaluated in tuberous sclerosis complex-associated renal angiomyolipoma in the double-blind, placebo-controlled, phase 3, EXIST-2 (Everolimus for angiomyolipoma associated with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis) Trial 34. A total of 118 patients with either tuberous sclerosis complex or sporadic angiomyolipoma received everolimus at 10 mg once daily or placebo. After a median treatment duration of 38 weeks, 42% of patients treated with everolimus (n=79) experienced a reduction of ≥50% in angiomyolipoma volume compared with none of the patients receiving placebo (n=39; between-treatment difference, 42%). Everolimus was generally well tolerated, and the most common adverse effects (≥20%) included stomatitis, nasopharyngitis, headache, acne, cough, and hypercholesterolemia 34. These data resulted in the FDA approval of everolimus in treating tuberous sclerosis complex-associated angiomyolipoma. Long-term results from this study showed sustained responses to everolimus; the proportion of patients with a ≥50% reduction in renal angiomyolipoma increased over time from 55% at week 24 to 69% at week 192. Over a median treatment duration of 47 months (approximately 4 years), 58% of patients treated with everolimus (n=112) experienced a ≥50% reduction in angiomyolipoma volume. Side effects remained consistent with previous reports, and the incidence of emergent side effects decreased over time. In addition, no renal hemorrhages were observed over the approximately 4-year time period.
Although rare, acute intervention is occasionally required to address massive hemorrhage, usually from aneurisms that form in the vessels of rapidly growing angiomyolipoma lesions that are larger than 4 cm in diameter. Often painful and presenting as gross hematuria and possibly, hypotension and hypovolemic shock, aneurism rupture may be treated with urgent embolization if available. The use of beads is preferred to coils, because the former can lodge into more distal collateral vessels, whereas the coils occlude more proximal vessels and thus, often preclude subsequent radiology intervention. If embolization is unavailable, nephrectomy may be emergently required as a lifesaving method to control bleeding. These interventions often are outside of nephrology expertise and require cooperation with interventional radiology or surgery colleagues.
References- Wang C, Li X, Peng L, Gou X, Fan J. An update on recent developments in rupture of renal angiomyolipoma. Medicine (Baltimore). 2018;97(16):e0497. doi:10.1097/MD.0000000000010497 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5916643
- Rakowski SK, Winterkorn EB, Paul E, Steele DJ, Halpern EF, Thiele EA. Renal manifestations of tuberous sclerosis complex: Incidence, prognosis, and predictive factors. Kidney Int. 2006 Nov. 70(10):1777-82
- Update on the Diagnosis and Management of Renal Angiomyolipoma. Flum AS, Hamoui N, Said MA, Yang XJ, Casalino DD, McGuire BB, Perry KT, Nadler RB. J Urol. 2016 Apr; 195(4 Pt 1):834-46.
- Jinzaki M, Silverman SG, Akita H, Nagashima Y, Mikami S, Oya M. Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management. Abdom Imaging. 2014 Jun. 39 (3):588-604
- Update on the Diagnosis and Management of Renal Angiomyolipoma. J Urol. 2016 Apr;195(4 Pt 1):834-46. doi: 10.1016/j.juro.2015.07.126. Epub 2015 Nov 21. https://www.ncbi.nlm.nih.gov/pubmed/26612197
- Cui L, Zhang JG, Hu XY et-al. CT imaging and histopathological features of renal epithelioid angiomyolipomas. Clin Radiol. 2012;67 (12): e77-82. doi:10.1016/j.crad.2012.08.006
- Lai HY, Chen CK, Lee YH et-al. Multicentric aggressive angiomyolipomas: a rare form of PEComas. AJR Am J Roentgenol. 2006;186 (3): 837-40. doi:10.2214/AJR.04.1639
- Harriet J. Paltiel Sonography of Pediatric Renal Tumors January 2007 volume 2 issue 1 Pages 89-104 DOI: 10.1016/j.cult.2007.01.004
- Renal Angiomyolipoma Imaging. https://emedicine.medscape.com/article/376848-overview
- Kingswood JC, Belousova E, Benedik MP, et al. Renal angiomyolipoma in patients with tuberous sclerosis complex: findings from the TuberOus SClerosis registry to increase disease Awareness. Nephrol Dial Transplant. 2018;34(3):502–508. doi:10.1093/ndt/gfy063 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6399480
- Samuels JA. Treatment of Renal Angiomyolipoma and Other Hamartomas in Patients with Tuberous Sclerosis Complex. Clin J Am Soc Nephrol. 2017;12(7):1196–1202. doi:10.2215/CJN.08150816 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5498351
- Rakowski SK, Winterkorn EB, Paul E. et al. Renal manifestations of tuberous sclerosis complex: incidence, prognosis, and predictive factors. Kidney Int 2006; 70: 1777–1782
- Ewalt DH, Sheffield E, Sparagana SP. et al. Renal lesion growth in children with tuberous sclerosis complex. J Urol 1998; 160: 141–145
- Dixon BP, Hulbert JC, Bissler JJ. Tuberous sclerosis complex renal disease. Nephron Exp Nephrol 2011; 118: e15–e20
- Krueger DA, Northrup H.; International Tuberous Sclerosis Complex Consensus Group: Tuberous sclerosis complex surveillance and management: Recommendations of the 2012 international tuberous sclerosis complex consensus conference. Pediatr Neurol 49: 255–265, 2013
- Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, Laor T, Brody AS, Bean J, Salisbury S, Franz DN.: Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med 358: 140–151, 2008
- Nelson CP, Sanda MG. Contemporary diagnosis and management of renal angiomyolipoma. J Urol 2002;168:1315–25
- Sotosek S, Markic D, Spanjol J, et al. Bilateral Wünderlich syndrome caused by spontaneous rupture of renal angiomyolipomas. Case Rep Urol 2015;2015:316956
- Champagnac J, Melodelima C, Martinelli T, et al. Microaneurysms in renal angiomyolipomas: can clinical and computed tomography features predict their presence and size? Diagn Interv Imaging 2016;97:321–6
- Logue LG, Acker RE, Sienko AE. Best cases from the AFIP: angiomyolipomas in tuberous sclerosis. Radiographics. 23 (1): 241-6. doi:10.1148/rg.231025109
- Umeoka S, Koyama T, Miki Y et-al. Pictorial review of tuberous sclerosis in various organs. Radiographics. 28 (7): e32. doi:10.1148/rg.e32
- Harriet J. Paltiel Sonography of Pediatric Renal Tumors January 2007, volume 2 issue 1 Pages 89-104 DOI: 10.1016/j.cult.2007.01.004
- Malhi H, Grant EG, Duddalwar V. Contrast-Enhanced Ultrasound of the Liver and Kidney. Radiol. Clin. North Am. 2014;52 (6): 1177-1190. doi:10.1016/j.rcl.2014.07.005
- Renal angiomyolipoma. https://radiopaedia.org/cases/renal-angiomyolipoma-25
- Shetty AS, Sipe AL, Zulfiqar M, Tsai R, Raptis DA, Raptis CA, Bhalla S. In-Phase and Opposed-Phase Imaging: Applications of Chemical Shift and Magnetic Susceptibility in the Chest and Abdomen. (2019) Radiographics : a review publication of the Radiological Society of North America, Inc. 39 (1): 115-135. doi:10.1148/rg.2019180043
- Choyke PL. Imaging of hereditary renal cancer. Radiol. Clin. North Am. 2003;41 (5): 1037-51
- Maclean DF, Sultana R, Radwan R et-al. Is the follow-up of small renal angiomyolipomas a necessary precaution?. Clin Radiol. 2014;69 (8): 822-6. doi:10.1016/j.crad.2014.03.016
- Dawson C. Guidelines for the active surveillance of angiomyolipoma. Urology Clinical Governance Lead (2017). http://www.pchurology.co.uk/governance/AML%202017.pdf
- Krueger DA, Care MM, Holland K, Agricola K, Tudor C, Mangeshkar P, Wilson KA, Byars A, Sahmoud T, Franz DN.: Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. N Engl J Med 363: 1801–1811, 2010
- Franz DN, Bissler JJ, McCormack FX.: Tuberous sclerosis complex: Neurological, renal and pulmonary manifestations. Neuropediatrics 41: 199–208, 2010
- Budde K, Gaedeke J.: Tuberous sclerosis complex-associated angiomyolipomas: Focus on mTOR inhibition. Am J Kidney Dis 59: 276–283, 2012
- Davies DM, de Vries PJ, Johnson SR, McCartney DL, Cox JA, Serra AL, Watson PC, Howe CJ, Doyle T, Pointon K, Cross JJ, Tattersfield AE, Kingswood JC, Sampson JR.: Sirolimus therapy for angiomyolipoma in tuberous sclerosis and sporadic lymphangioleiomyomatosis: A phase 2 trial. Clin Cancer Res 17: 4071–4081, 2011
- Dabora SL, Franz DN, Ashwal S, Sagalowsky A, DiMario FJ Jr., Miles D, Cutler D, Krueger D, Uppot RN, Rabenou R, Camposano S, Paolini J, Fennessy F, Lee N, Woodrum C, Manola J, Garber J, Thiele EA.: Multicenter phase 2 trial of sirolimus for tuberous sclerosis: Kidney angiomyolipomas and other tumors regress and VEGF- D levels decrease. PLoS One 6: e23379, 2011
- Bissler JJ, Kingswood JC, Radzikowska E, Zonnenberg BA, Frost M, Belousova E, Sauter M, Nonomura N, Brakemeier S, de Vries PJ, Whittemore VH, Chen D, Sahmoud T, Shah G, Lincy J, Lebwohl D, Budde K.: Everolimus for angiomyolipoma associated with tuberous sclerosis complex or sporadic lymphangioleiomyomatosis (EXIST-2): A multicentre, randomised, double-blind, placebo-controlled trial. Lancet 381: 817–824, 2013