What is anisocoria
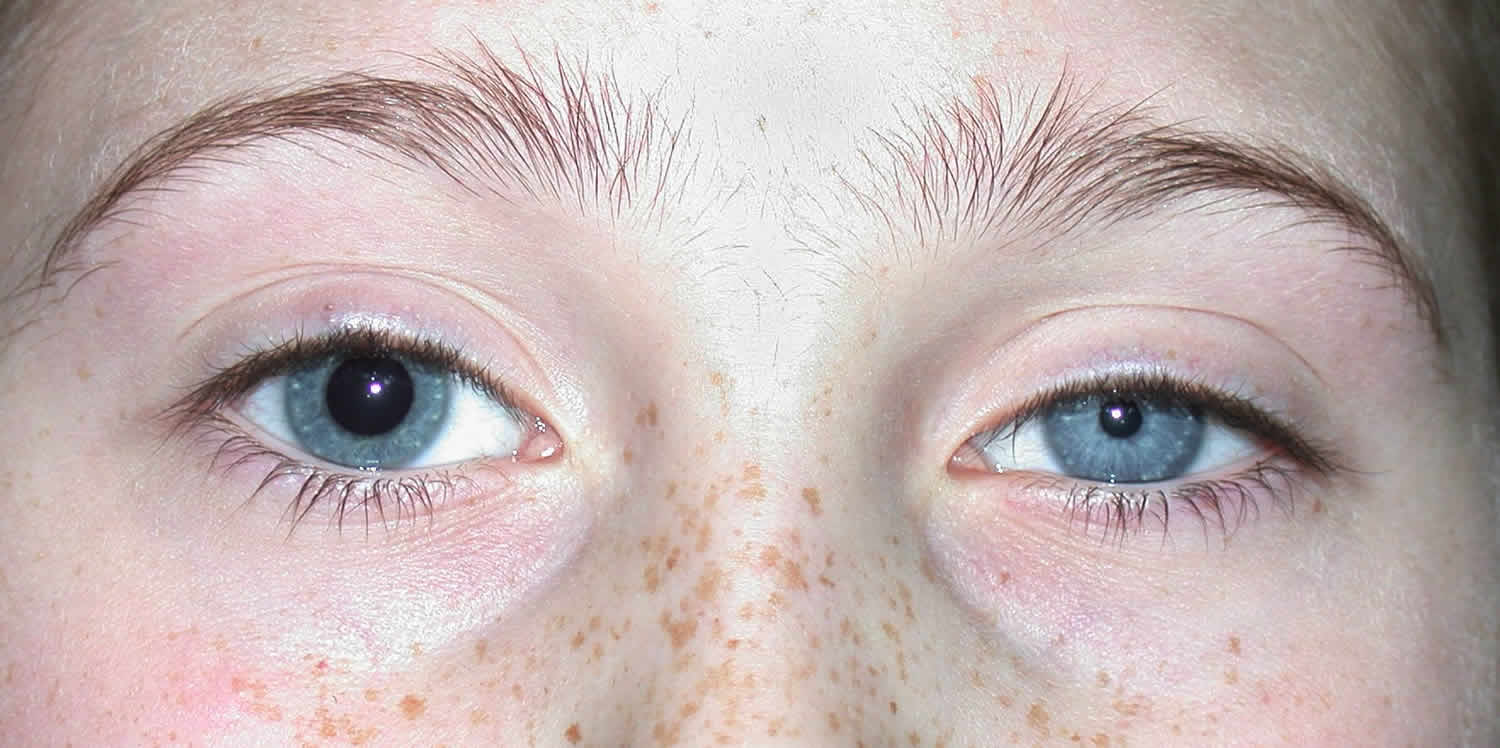
Anisocoria is a condition characterized by unequal pupil sizes 1. The pupil is the black part in the center of the eye. It gets larger in dim light and smaller in bright light. Anisocoria is a relatively common condition, and causes vary from benign physiologic anisocoria to potentially life-threatening emergencies. Therefore thorough clinical evaluation is important for the appropriate diagnosis and management of the underlying cause.
Physiologic anisocoria: slight differences in pupil sizes are found in up to 1 in 5 healthy people. Most often, the diameter difference is less than 0.5 mm, but it can be up to 1 mm (0.05 inch). The difference between pupil sizes in physiologic anisocoria is typically ≤ about 1 mm.
Babies born with anisocoria (different sized pupils) may not have any underlying disorder. If other family members also have similar pupils, then the pupil size difference could be genetic and is nothing to worry about.
Also, for unknown reasons, pupils may temporarily differ in size. If there are no other symptoms and if the pupils return to normal, then it is nothing to worry about.
Unequal pupil sizes of more than 1 mm that develop later in life and do NOT return to equal size may be a sign of an eye, brain, blood vessel, or nerve disease. Many disorders are accompanied by anisocoria due to iris or neurologic dysfunction but usually manifest with other, more bothersome symptoms (e.g., uveitis, stroke, subarachnoid hemorrhage, acute angle-closure glaucoma).
Examining the pupils in light and dark and inspecting an old photograph or the driver’s license of the patient provide a great deal of diagnostic information.
Serious disorders should be considered in patients with Horner syndrome or 3rd cranial nerve palsy.
Red flags – The following findings are of particular concern:
- Ptosis
- Anhidrosis (reduced sweating on the face of the affected side)
- Pupils that respond more to accommodation than light
- Impaired extraocular movements
Treatment depends on the cause of the unequal pupil size. You should see a health care provider if you have sudden changes that result in unequal pupil size.
Contact a doctor if you have persistent, unexplained, or sudden changes in pupil size. The new development of different-sized pupils may be a sign of a very serious condition.
- If you have differing pupil size after an eye or head injury, get medical help immediately.
Always seek immediate medical attention if differing pupil size occurs along with:
- Blurred vision
- Double vision
- Eye sensitivity to light
- Fever
- Headache
- Loss of vision
- Nausea or vomiting
- Eye pain
- Stiff neck
Figure 1. Human eye
 Pupil Anatomy
Pupil Anatomy
Physiologic control of pupillary function is dictated by sympathetic and parasympathetic innervation to the pupillary dilator and the pupillary sphincter muscles, respectively. Pupillary function is autonomic, largely occurring in response to light stimulation and adrenergic tone.
The sympathetic pathway is a three-order neuron pathway that mediates pupillary dilation. The first-order neuron originates from the posterolateral hypothalamus and travels caudally down the brainstem to the ciliospinal center of Budge (C8-T2). The second-order neuron continues over the lung apex and synapses at the superior cervical ganglion located at the carotid bifurcation. The third-order neuron ascends along the carotid artery into the cavernous sinus to ultimately synapse at the pupillary dilator muscle, the Muller muscle of the upper eyelid, and the smooth muscle of the lower eyelid. Sudomotor fibers course with the external carotid artery to innervate sweat glands of the face.
The parasympathetic pathway is a four-order neuron pathway that controls pupillary constriction and accommodation. Afferent light stimulus is received by retinal ganglion cells whose axons traverse as the optic nerve, optic chiasm and optic tract that eventually synapses at the pretectal nuclei of the dorsal midbrain at the level of the superior colliculi. The second-order neuron connects each pretectal nucleus to bilateral Edinger-Westphal nuclei in the midbrain and allows for the consensual light reflex. The Edinger-Westphal nucleus then supplies parasympathetic fibers to the third cranial nerve which traverses the cavernous sinus and enters the orbit via the superior orbital fissure to synapse at the ipsilateral ciliary ganglion. Postganglionic fibers of the short ciliary nerve reach the pupillary sphincter and ciliary muscles.
Anisocoria causes
Generally, anisocoria is caused by impaired dilation (a sympathetic response) or impaired constriction (a parasympathetic response) of pupils. An injury or lesion in either pathway may result in changes in pupil size.
The use of eye drops is a common cause of a harmless change in pupil size. Other medicines that get in the eyes, including medicine from asthma inhalers, can change pupil size.
Other causes of anisocoria (unequal pupil sizes) may include:
- Aneurysm in the brain
- Bleeding inside the skull caused by head injury
- Brain tumor or abscess (such as, pontine lesions)
- Excess pressure in one eye caused by glaucoma
- Increased intracranial pressure, because of brain swelling, intracranial hemorrhage, acute stroke, or intracranial tumor
- Infection of membranes around the brain (meningitis or encephalitis)
- Migraine headache
- Seizure (pupil size difference may remain long after seizure is over)
- Tumor, mass, or lymph node in the upper chest or lymph node causing pressure on a nerve may cause decreased sweating, a small pupil, or drooping eyelid all on the affected side (Horner syndrome)
- Diabetic occulomotor nerve palsy
- Prior eye surgery for cataracts
Table 1. Common causes of anisocoria
| Cause | Suggestive Findings |
| Adie tonic pupil (idiopathic impaired constriction) | Pupils that respond more to accommodation than to light; delayed dilation after constriction |
| Argyll Robertson pupil (due to syphilis) | Pupils that respond more to accommodation than to light; possibly findings suggesting syphilis |
| Congenital iris defects | Associated ocular abnormalities, chromosomal disorder, nonocular congenital defects, chronicity |
| Drugs (eg, scopolamine patch; cocaine, pilocarpine, animal flea collars or sprays, organophosphates, or aerosolized ipratropium if they contact the eye; cycloplegic, mydriatic, clonidine, or apraclonidine eye drops) | History of use or exposure |
| Horner’s syndrome (eg, congenital, traumatic, postsurgical, due to migraine or lung tumors) | Ptosis, anhidrosis, delayed dilation after constriction, features of causative disorder |
| Iris or other ocular dysfunction after surgery | History |
| Physiologic anisocoria | Chronicity, absence of symptoms or associated findings, difference of < 1 mm (usually < 0.4 mm) between pupil sizes, normal pupillary light responses |
| Third cranial nerve palsy (eg, due to aneurysm or tumor) | Impaired extraocular movements, ptosis |
| Traumatic mydriasis | History or evidence of trauma |
Physiologic (also known as simple or essential) anisocoria is the most common cause of unequal pupil sizes, affecting up to 20% of the population 2. Physiologic anisocoria is a benign condition with a difference in pupil size of less than or equal to 1 mm 3. The exact cause is unknown, but it is thought to be due to transient asymmetric supranuclear inhibition of the Edinger-Westphal nucleus that controls the pupillary sphincter 4. Light and near response is intact, and the degree of anisocoria is typically equal in light and dark. Physiologic anisocoria may be intermittent and even self-resolving. However, many cases are persistent.
Congenital anisocoria in the structure of the iris may contribute to abnormal pupillary sizes and shapes that present in childhood. Examples include aniridia, coloboma and ectopic pupil 1.
Mechanical anisocoria is an acquired defect that results from damage to the iris or its supporting structures. Causes include physical injury from ocular trauma or surgery, inflammatory conditions such as iritis or uveitis, angle closure glaucoma leading to iris occlusion of the trabecular meshwork, or intraocular tumors causing physical distortion of the iris.
Pharmacologic anisocoria can present as mydriasis or miosis following administration of agents that act on the pupillary dilator or sphincter muscles. Anticholinergics such as atropine, homatropine, tropicamide, scopolamine and cyclopentolate lead to mydriasis and cycloplegia by inhibiting parasympathetic M3 receptors of the pupillary sphincter and ciliary muscles. The use of pilocarpine, a non-selective muscarinic receptor agonist in the parasympathetic nervous system, may result in a small and poorly reactive pupil. Sympathomimetics such as adrenaline, and phenylephrine cause mydriasis through their actions at ɑ-1 receptors of the pupillary dilator muscle.
Horner’s syndrome (oculosympathetic palsy) is classically described by the triad of ptosis, miosis and anhydrosis, although clinical presentation may vary. Anisocoria is greater in the dark due to a defect in the pupillary dilator response secondary to lesions along the sympathetic trunk. Central or first-order lesions are often caused by stroke, lateral medullary syndrome, neck trauma or demyelinating disease. Preganglionic or second-order neuron lesions may be caused by a Pancoast tumor, mediastinal or thyroid mass, cervical rib, and neck trauma or surgery. Postganglionic or third-order neuron lesions include carotid artery dissection, cavernous sinus lesion, otitis media, and head or neck trauma. Further pharmacologic workup (see diagnostic procedures) is useful in confirming Horner’s and distinguishing the order of the lesion.
Adie’s tonic pupil results from damage to the parasympathetic ciliary ganglion or short ciliary nerves that innervate the sphincter pupillae and ciliary muscle. Aberrant reinnervation and upregulation of post-synaptic receptors lead to the clinical presentation of a tonically dilated pupil with near stimulation that is poorly reactivity to light. Ninety percent of cases occur in women between the ages of 20-40 years, 80% of cases are unilateral, and 70% of cases are associated with decreased deep tendon reflexes (Adie’s syndrome) 3.
Oculomotor (third) nerve palsy varies in presentation and cause. The oculomotor nerve innervates 4 out of the 6 extraocular muscles (superior rectus, medial rectus, inferior rectus and inferior oblique), the sphincter pupillae muscle, the ciliary muscle and the levator palpebrae muscle. Third nerve palsies rarely present as an isolated mydriasis; associated findings include ptosis, an ipsilateral “down and out” gaze, and loss of accommodation. Compressive lesions from head trauma, intracranial aneurysms, uncal herniation and tumors typically involve the pupil as they affect the superficial parasympathetic fibers that innervate the pupil. Ischemic or diabetic oculomotor nerve palsies typically spare the pupil 5.
Anisocoria symptoms
Isolated anisocoria is often asymptomatic, though mydriasis may cause glare, photosensitivity, and impaired accommodation. Complaints of pain, headaches, ptosis, diplopia, blurred vision, numbness, weakness or ataxia may warrant further evaluation for more life-threatening conditions including traumatic injury, intracranial mass, aneurysm or carotid dissection.
Anisocoria diagnosis
Medical history
A careful history to elucidate the onset and chronicity of anisocoria may be useful for determining the cause of anisocoria. Old photographs may provide information since symptoms may not exist or may go unnoticed. Chronic anisocoria without associated symptoms may point to a benign process such as physiologic anisocoria, whereas sudden-onset anisocoria in the setting of other symptoms may be more worrisome. For example, anisocoria with headaches, confusion, altered mental status and other focal neurologic deficits suggest an underlying mass effect and may require further neurologic work-up and intervention.
Complete ophthalmic history is important as coexisting ocular conditions, previous surgeries or trauma to the head or orbit may also contribute to anisocoria. A thorough review of medications, especially topical eye drops, may provide explanations for pharmacologic anisocoria. A discussion about exposures to certain narcotics, insecticides (organophosphates) or plants (Brugmansia Angel’s trumpet or Datura Devil’s trumpet), should also be considered.
Physical examination
External eye structures should be examined for associated ocular manifestations. Ptosis and gaze deviation may suggest an oculomotor nerve palsy, whereas proptosis may indicate and underlying space-occupying lesion within the orbit.
A thorough pupillary exam is crucial, and it is best done in dim light with the patient’s eyes fixed on a distant object to eliminate the near reaction. Pupils should be compared for size in light and in dark (normal size difference is less than 0.4 mm), shape, position, symmetry and reactivity. The pupils should be evaluated for direct and consensual responses that are normally equal in speed and magnitude. Accommodation to near stimuli should also be examined as light-near dissociation, or impaired light reaction in the setting of a normal near reaction, may suggest Adie’s tonic pupil or Argyll Robertson pupil of syphilis.
The slit-lamp examination can provide additional information for associated or coexisting ocular conditions. Congenital, traumatic and surgical causes of anisocoria will often be associated with other structural defects. The anterior chamber can be examined for signs of iritis or uveitis. Abnormal gonioscopy and tonometry findings may suggest angle closure glaucoma. The clinical picture of Adie’s tonic pupil under slit-lamp examination shows iris sector palsy and vermiform iris movement 6.
A detailed neurologic exam is important to localize lesions, look for accompanying signs of cranial nerve involvement, and assess for focal neurologic deficits in the sensory, motor and deep tendon reflex pathways.
Laboratory tests
If the history and physical examination leads to clinical suspicion for Argyll Robertson pupil, venereal disease research laboratory test (VDRL) and fluorescent treponemal antibody absorption (FTA-ABS) tests for screening and confirmation of syphilis can be done. Lumbar punctures for VDRL, FTA-ABS, total protein and cell count may be indicated in the evaluation of neurosyphlis.
Additional tests that may be done include:
- Blood studies such as CBC and blood differential
- Cerebrospinal fluid studies (lumbar puncture)
- CT scan of the head
- EEG
- Head MRI scan
- Tonometry (if glaucoma is suspected)
- X-rays of the neck
Diagnostic procedures
In the diagnostic work-up for anisocoria, it is useful to distinguish between anisocoria that is greater in the dark versus anisocoria that is greater in the light. This is followed by a series of pharmacologic tests to further determine the exact cause 7.
Anisocoria that is greater in the dark suggests a lesion in the sympathetic pathway, which results in an abnormal pupil that is smaller or unable to dilate in response to removal of a light stimulus. Causes include Horner’s syndrome, Argyll Robertson pupil, iritis, mechanical anisocoria, and pharmacologic anisocoria from miotics, narcotics and insecticides.
In this setting, one to two drops of cocaine 4-10% is administered to both eyes and evaluated after 30 to 45 minutes. Cocaine prevents the reuptake of norepinephrine at the post-synaptic third-order neuron thereby allowing dilation of the normal pupil. There is an increased pupillary asymmetry in Horner’s syndrome because the sympathetic pathway to the affected pupil is low in norepinephrine to begin with. Apraclonidine, a strong α-2 and weak α-1 agonist, is a more readily available alternative to cocaine. While apraclonidine 0.5% causes constriction of the normal pupil due to its strong α-2 adrenergic activity, it causes reversal of anisocoria in Horner’s by moderately dilating the affected pupil that has undergone denervation supersensitivity (when supersensitivity is present, apraclonidine’s weak α-1 agonist activity predominates) 8.
The use of hydroxyamphetamine 1% (Paredrine) can provide localization to the defect in Horner’s syndrome. Hydroxyamphetamine requires an intact third-order sympathetic neuron to stimulate norepinephrine release. Therefore, an asymmetric dilation suggests a third-order or postganglionic lesion whereas equal pupillary dilation indicates a central or preganglionic lesion 9.
On the other hand, anisocoria that is greater in the light suggests a parasympathetic defect, resulting in an abnormal pupil that is larger or unable to constrict in response to a light stimulus. Causes include Adie’s tonic pupil, oculomotor nerve palsy, traumatic injury to the iris, or pharmacologic dilation from mydriatics/cycloplegics (atropine, tropicamide, cyclopentolate) or cocaine.
The use of pilocarpine can be diagnostic in this setting. Low doses of pilocarpine 0.1% or methacholine 2.5% do not constrict a normal pupil but result in the constriction of Adie’s tonic pupil due to hypersensitivity from the upregulation of cholinergic receptors. If no constriction is observed, a higher dose of pilocarpine 1% is used. Pupillary constriction indicates an oculomotor nerve palsy, whereas no response indicates a pharmacologic cause to the anisocoria.
When pharmacologic and laboratory tests are unequivocal, or when clinical suspicion persists for an underlying aneurysm, hemorrhage or tumor, imaging of the head, neck, and chest can help identify causes of Horner’s or oculomotor nerve palsies.
Anisocoria treatment
Treatment of anisocoria varies depending on the cause. Physiologic anisocoria is often asymptomatic and does not require intervention. Mechanical anisocoria secondary to trauma may require surgery to correct the structural defect. Mechanical anisocoria secondary to other ophthalmic conditions such as uveitis or acute angle glaucoma can be medically managed as indicated. Pharmacologic anisocoria typically resolves with cessation of the offending agent. Adie’s tonic pupil can be managed with the help of glasses to improve vision and pilocarpine to constrict the pupil. Benign causes of Horner’s syndrome and ocolomotor nerve palsies can be observed with expectant partial or full resolution of symptoms. However, life-threatening causes such as stroke, aneurysm, hemorrhage, dissection, and tumor must be ruled-out and managed appropriately via surgical or medical intervention.
References- Anisocoria. http://eyewiki.org/Anisocoria
- Lam BL , Thompson HS, Corbett JJ. The prevalence of simple anisocoria. Am J Ophthalmol.1987;104(1):69–73.
- Kaiser PK. Friedman NJ. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 4th Edition. 2014. Pp 647.
- Loewenfeld IE. “Simple, central” anisocoria. A common condition seldom recognized. Trans. Am. Acad Ophthalmol Otolaryngol. 1977; 83: 832–839.
- Goldstein JE. Diabetic opthalmopegia with special reference to the pupil. Arch Opthalmol 1960. 64: 592.
- Thompson HS. Segmental palsy of the iris sphincter in Adie’s syndrome. Arch Opthalmol. 1978;96(9):1615-1620.
- Thompson HS, Pilley SFJ. Unequal pupils. A flow chart for sorting out the anisocorias. Survey of ophthalmology 1976; 21(1):45-48.
- Koc F, Kavuncu S, Kansu T. The sensitivity and specificity of 0.5% apraclonidine in the diagnosis of oculosympathetic paresis, Br J Ophthalmol 2005; 89(11):1442-1444.
- Cremer SA, Thompson HS, Digre KB, Kardon RH. Hydroxyamphetamine mydriasis in Horner’s syndrome. Am J Ophthalmol 1990; 110(1):71-6.