Ankle impingement syndrome
Ankle impingement syndrome is a syndrome that encompasses a wide range of anterior (anterolateral and anteromedial) and posterior (posteromedial) ankle joint pathology causing painful mechanical limitation of full ankle range of motion secondary to both osseous and soft tissue abnormalities 1. Location of pain is referenced from the tibiotalar (talocrural) joint 2. With anterior impingement producing symptoms with terminal dorsiflexion and posterior impingement is exacerbated by activities involving hyper-plantar flexion 1. History, physical examination, imaging studies, and diagnostic injections all contribute to the accurate diagnosis of ankle impingement syndrome. Many patients will respond favorably to non-operative treatment modalities, but both open and arthroscopic techniques have evolved to address chronic problems with successful and predictable outcomes.
Soft-tissue impingement lesions of the ankle usually occur as a result of synovial or capsular irritation secondary to traumatic injuries, infection, or rheumatologic or degenerative disease states. Ankle impingement syndromes may also be congenital in origin. The leading causes of impingement lesions are posttraumatic injuries, usually ankle sprains, leading to chronic pain. Involved areas may include the anterolateral gutter, syndesmosis, and posterior ankle regions.
In 1950, Glassman et al 3 reported on 9 patients who presented with chronic persistent pain and swelling around the anterolateral aspect of the ankle following an inversion ankle sprain. At the time of surgery, a massive hyalinized connective-tissue band that extended from the anteroinferior region of the talofibular ligament (talofibular ligament) into the ankle joint was found. The authors referred to this pathologic entity as a meniscoid lesion because of its resemblance to a torn meniscus of the knee 3. It was believed that repetitive tension on this tissue led to increasing hypertrophy and fibrosis, resulting in impingement on the talar cartilage and causing pain and swelling. Resolution of symptoms occurred in all cases with excision of the pathologic tissue.
In 1982, Waller 4 described a pain syndrome along the anteroinferior border of the fibula and anterolateral talus following repetitive inversion injuries. Examination of his patients revealed foot pronation and heel valgus. Waller believed this pathology to be synovial compression or chondromalacia of the lateral talar dome and called it the anterolateral corner compression syndrome 4.
Bassett et al 5 found and described a separate pathologic fascicle of the anterior talofibular ligament in syndesmotic impingement. Following a tear of the Atalofibular ligament, the anterolateral talar dome extrudes anteriorly with dorsiflexion, resulting in impingement.
Hamilton 6 described a labrum or pseudomeniscus of the posterior lip of the tibia, which can become torn or hypertrophied with ankle sprains and lead to posterior impingement.
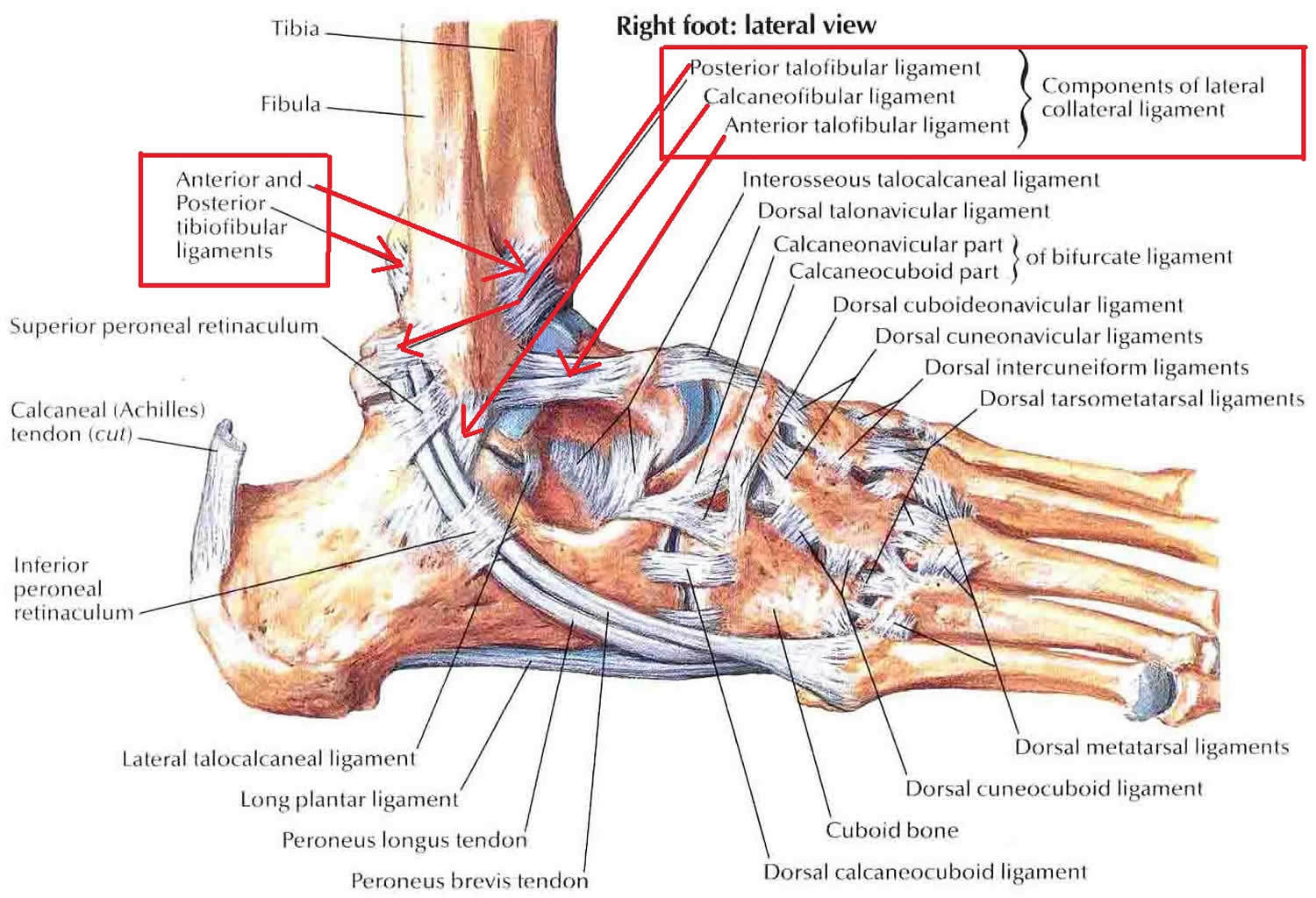
Figure 1. Ankle ligaments
Anterior ankle impingement syndrome
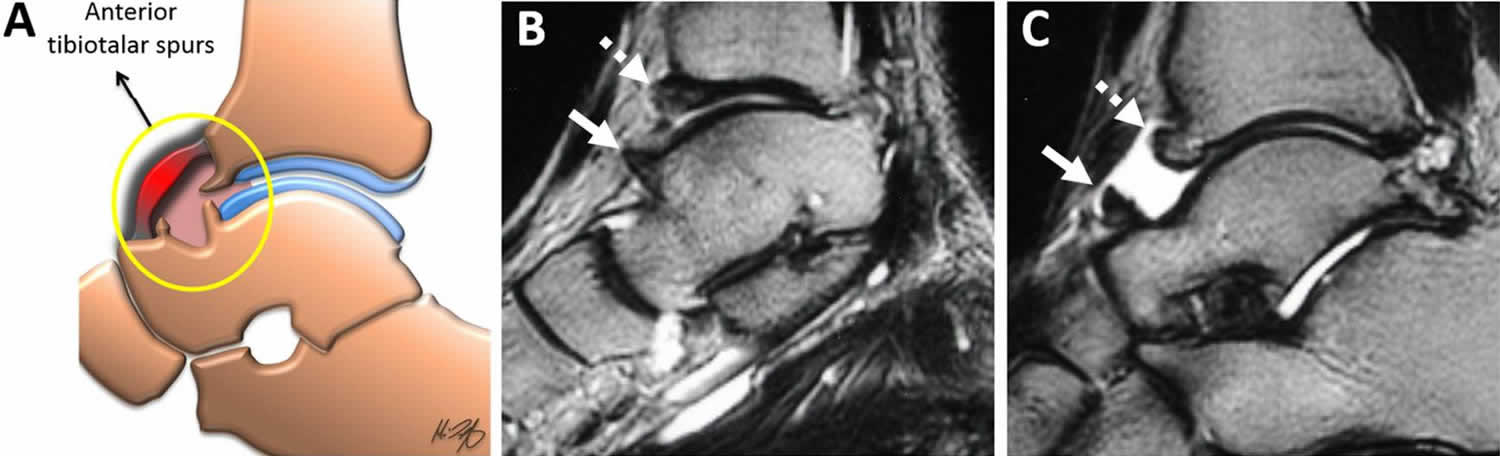
Anatomically, the anterior aspect of the ankle is defined as the central portion of the ankle recess between the anterior tibial plafond and talar dome (Figure 2). Anterior impingement syndrome was first described in soccer players in 1943 by Morris 7 and later by McMurray 8 and named “athlete’s ankle” and “footballers’ ankle”. The prototypical patient who presents with anterior ankle impingement is a ballet dancer or soccer player who has anterior joint pain and limited dorsiflexion.
Anterior impingement syndrome typically presents as anterior ankle pain during terminal dorsiflexion. Exacerbating activities commonly include climbing stairs, running or walking up hills, ascending ladders, and deep squatting. The classic association with competitive soccer players has long been recognized, but the reason that this subset of athletes is commonly affected is unclear 9. In the later stages, dorsiflexion may be limited secondary to mechanical block or pain, creating a cycle of progressive joint stiffness and loss of function. In isolated soft tissue lesions, the patient may report a subjective popping or snapping sensation.
Initially, it was thought that the anterior ankle impingement was caused by plantar flexion of the tibiotalar joint with repetitive traction to the anterior joint capsule forming anterior tibiotalar osteophytes (traction spurs) 10. However, cadaveric and arthroscopic evaluations suggest direct microtrauma to the talus and tibia as the cause 10. The natural course of this repetitive microtrauma is to form osseous spurs (Figure 2) 10. These spurs can cause impingement through a Cam-type mechanism 11. However, it should also be noted that osteophyte formation is common in asymptomatic ballet dancers and soccer players 12.
Much like the anterolateral impingement syndrome, this reactive process can cause irritation of the capsule and lead to a synovial inflammatory response, which in itself can cause pain and can also lead to the formation of fibrous bands 9. These bands can further limit dorsiflexion. A differential diagnosis may include tendon sheath rupture, tenosynovitis, synovial cyst rupture or a ganglion cyst.
Figure 2. Anterior ankle impingement
Footnote: (a) An illustration in the mid-sagittal plane is demonstrating the involved anterior joint capsule (circle) with associated osteophytes from the anterior tibial plafond and anterior talar neck. (b, c) Sagittal fluid-sensitive MR images are showing a superior talar neck (arrows) and anterior tibial osteophytes (dashed arrows) in a male with anterior ankle impingement symptoms.
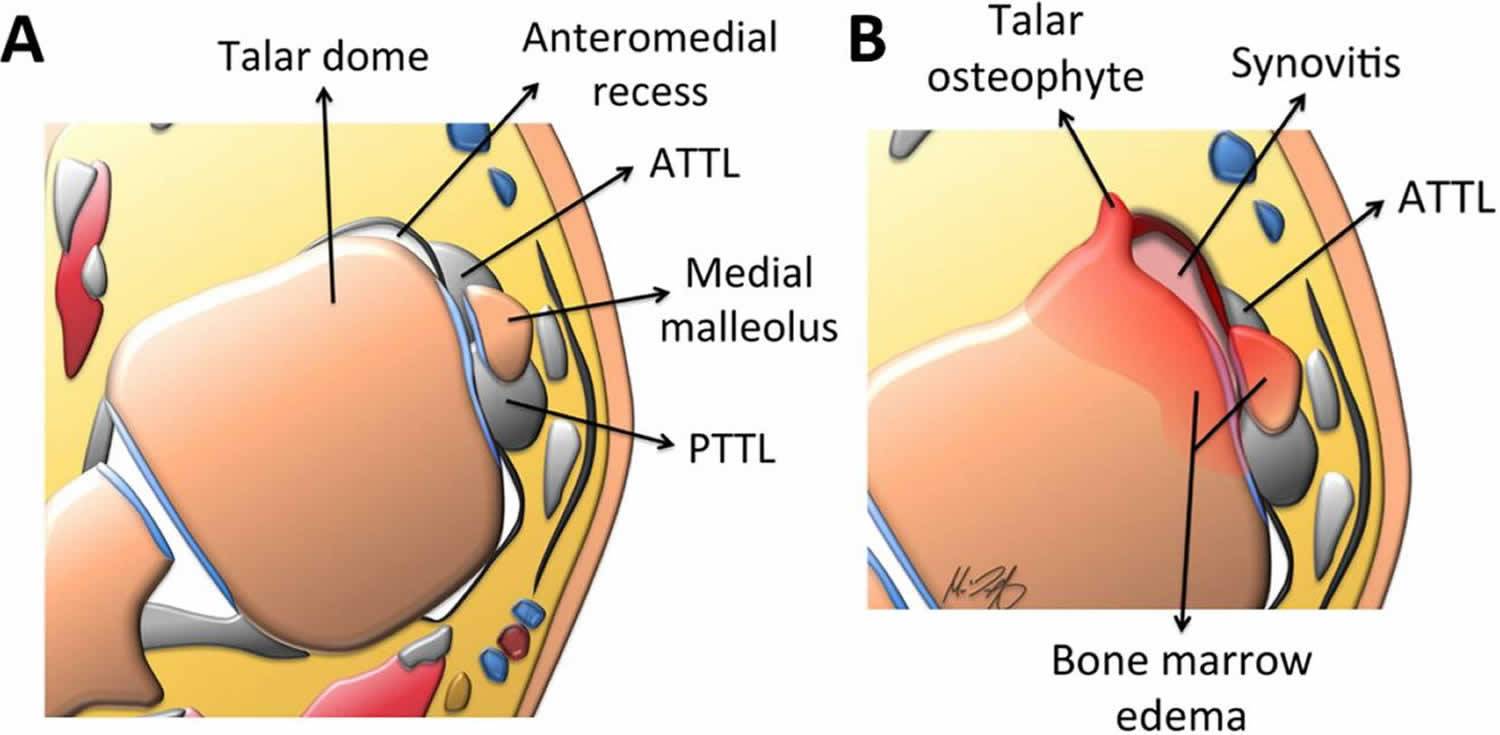
[Source 13 ]Anteromedial impingement syndrome
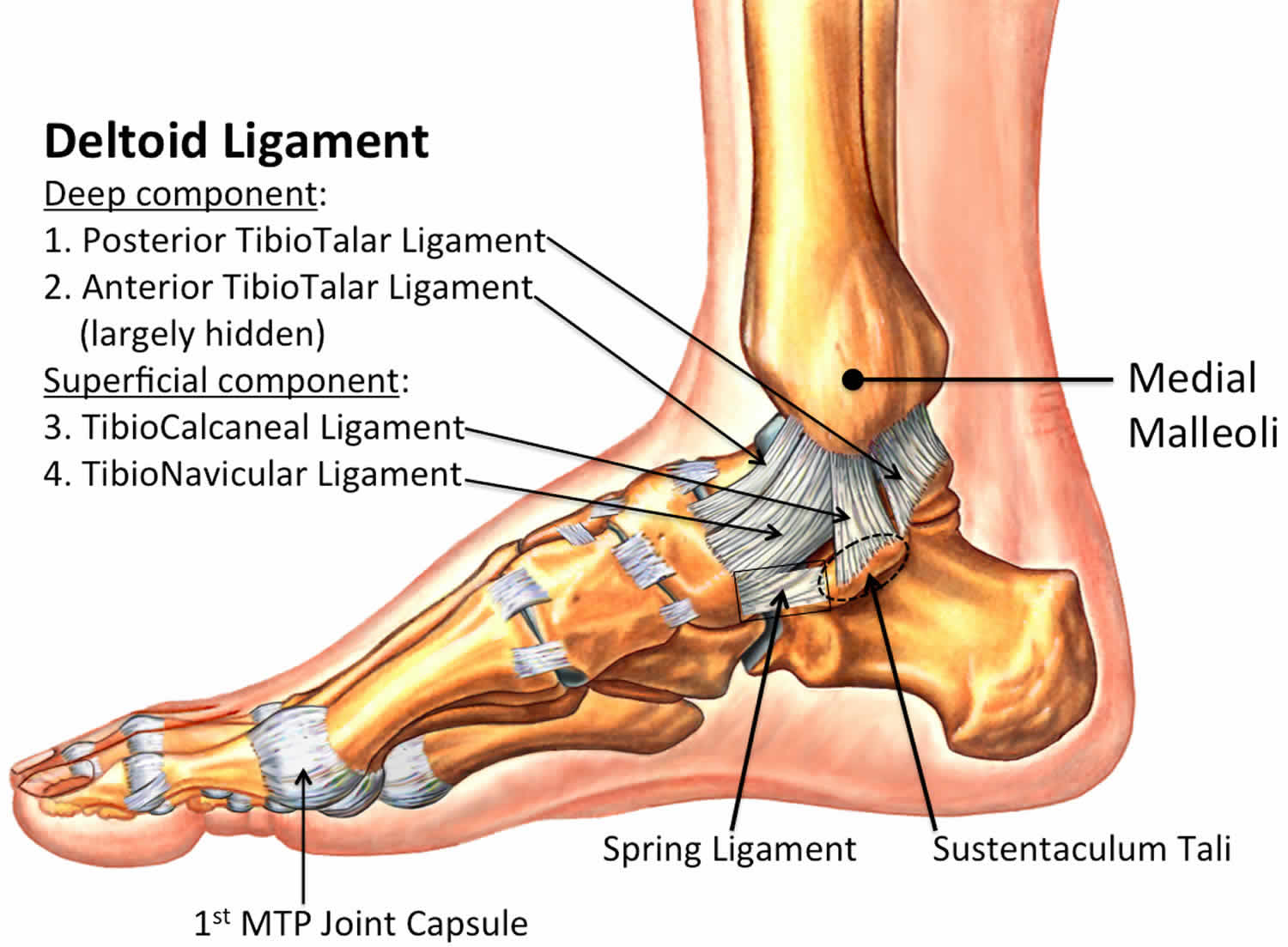
The anteromedial gutter or recess is formed superficially by the anteromedial joint capsule, laterally by the talar dome, body and neck, medially by the medial malleolus and inferiorly by the anterior tibiotalar fascicle of the deltoid ligament (anterior tibiotalar ligament or ATTL) (Figure 3).
Clinically, the anteromedial ankle impingement syndrome presents with pain associated with dorsiflexion and inversion and can be seen in soccer players, dancers and cross-country runners.40 This can result as the sequela of a prior plantar flexion/inversion injury 14. Anteromedial ankle impingement syndrome was first described by Egol and Parisien in 1997 in a case report and subsequently by Mosier-La Clair et al in 2000 with a case series of 11 patients 15.
During the acute injury, there is damage to the anterior tibiotalar ligament, which subsequently thickens 15. In addition to ligament thickening, osteophytes, synovitis and fractures have been described as other possible causative factors 15. Lastly, recurrent microtrauma over time can form bony spurs along the talar neck, anterior margin of the medial malleolus or anteromedial tibial plafond, which can impair the range of motion, similar to anterior ankle impingement 16.
Figure 3. Anteromedial impingement syndrome
Footnote: Axial illustrations through the level of the talus: (a) the normal appearance of the anteromedial ankle recess is shown, which is formed by the talus, anteromedial joint capsule, medial malleolus and the anterior tibiotalar ligament (ATTL). Also shown is the posterior tibiotalar ligament (PTTL), which forms the posterior border. (b) Possible aetiologies of anteromedial impingement syndrome are shown, including but not limited to: a talar osteophyte from chronic repetitive microtrauma, thickening of the anterior tibiotalar ligament (ATTL), synovial inflammatory response and associated bone marrow oedema.
[Source 13 ]Posterior ankle impingement syndrome
Posterior impingement syndrome generally presents as a less specific pain deep to the Achilles tendon and may often be confused with Achilles or peroneal tendon pathology. Symptoms may be worsened by activities involving plantar flexion and repetitive push-off maneuvers, including downhill running and walking, descending stairs, and high-heeled shoe wear. Posterior impingement classically presents in dancers, specifically those participating in classic ballet, presumably due to repetitive weight bearing in the plantar-flexed “en-pointe” and “demi-pointe” positions 17. In a recent systematic review, dancers represented 61 % of patients undergoing surgery for posterior impingement 18. It has also been reported to affect fast-bowlers in cricket 19.
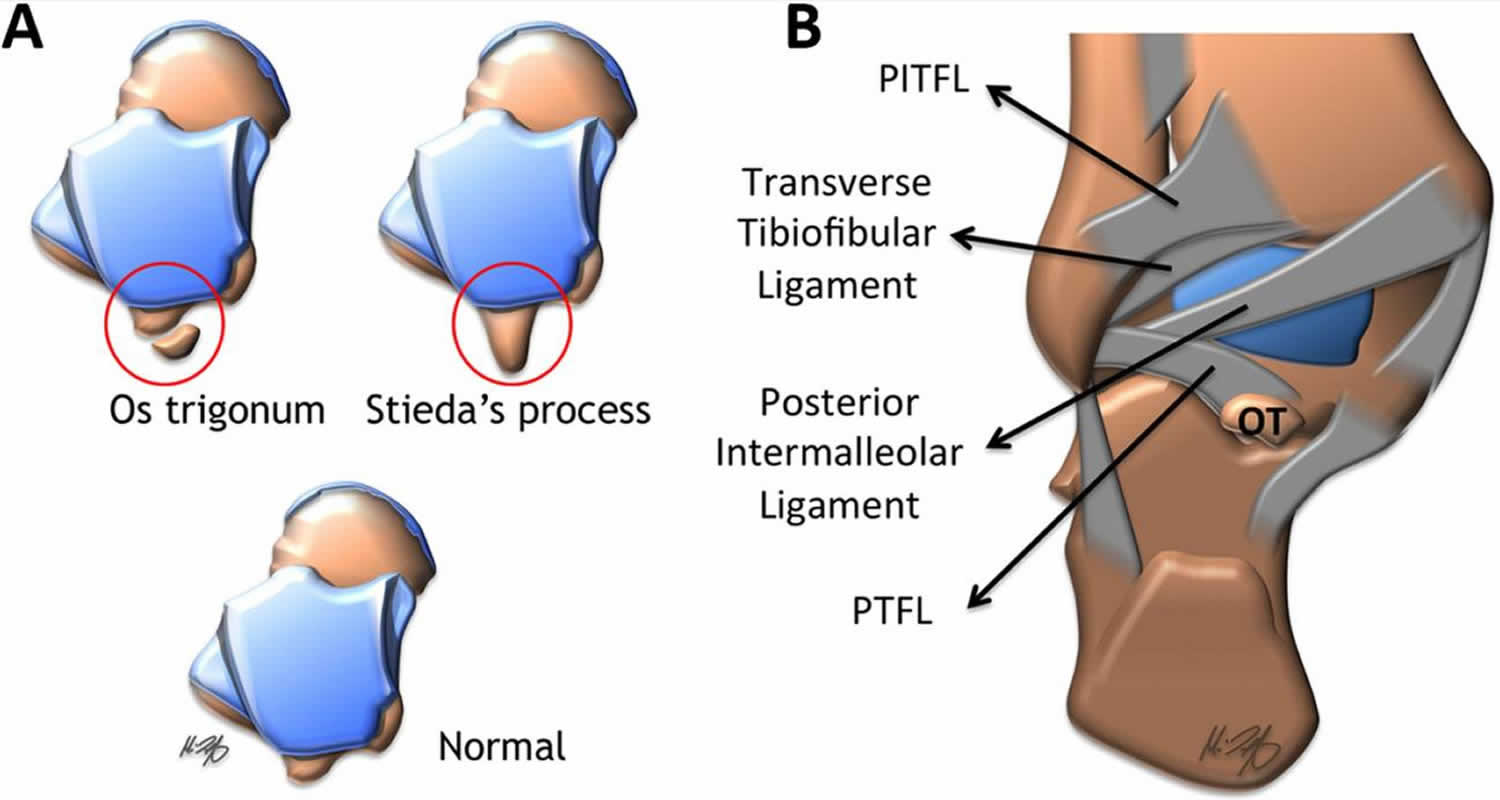
The majority of the posterior impingement syndromes are related to the posterior talus. The secondary ossification center of the posterolateral talus forms around 8–13 years of age and then subsequently fuses within 1 year of that 20. Occasionally (approximately 7%), there may be non-fusion with a resultant os trigonum 21. In addition, this ossification centre may remain prominent with the so-called “Stieda’s process” (Figure 4) 22.
In addition to the osseous posterolateral talus, the ligamentous anatomy includes (from superior to inferior): (1) the posteroinferior talofibular ligament, which extends from the lateral malleolus to the posterolateral tibia; (2) the transverse tibiofibular ligament extending from the fibula to the posterior tibia and medial malleolus; (3) the tibial slip, also called the posterior intermalleolar ligament, originating from the posterior tibia and inserts at the posterior talofibular ligament; and (4) the posterior talofibular ligament extending from the lateral malleolus to the posterolateral talus (Figure 4).
Clinically, the posterior impingement syndrome presents with chronic pain and swelling within the posterior ankle. Classically, this is seen with activities that cause extreme plantar flexion, such as ballet, soccer, football and downhill running 20.
Figure 4. Posterior impingement syndrome
Footnote: (a) Illustrations as seen from a superior view demonstrating the normal posterior process of the talus, os trigonum (OT) and Stieda’s process variants; (b) an illustration as seen from a posterior view of the ankle demonstrating the ligamentous anatomy of the posterolateral ankle.
Abbreviations: PITFL = posteroinferior tibiofibular ligament; PTFL = posterior talofibular ligament.
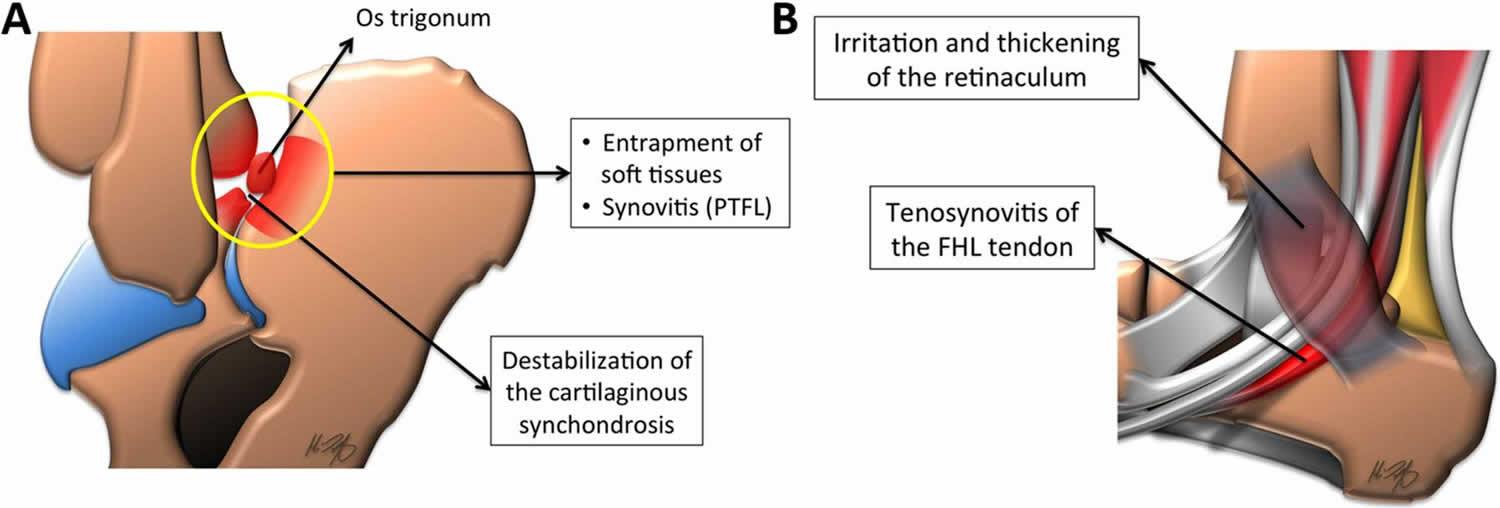
[Source 13 ]Figure 5. Posterior ankle impingement
Footnote: Sagittal illustrations as seen from a lateral view in posterior ankle impingement: (a) in the plantar flexed ankle with an associated os trigonum, there is an entrapment of the posterior soft tissues, including the posterior talofibular ligament (PTFL) and associated synovitis. (b) An irritated and thickened flexor retinaculum can cause flexor hallucis longus (FHL) tendon irritation and tenosynovitis owing to their intimate relationship.
[Source 13 ]Posteromedial impingement syndrome
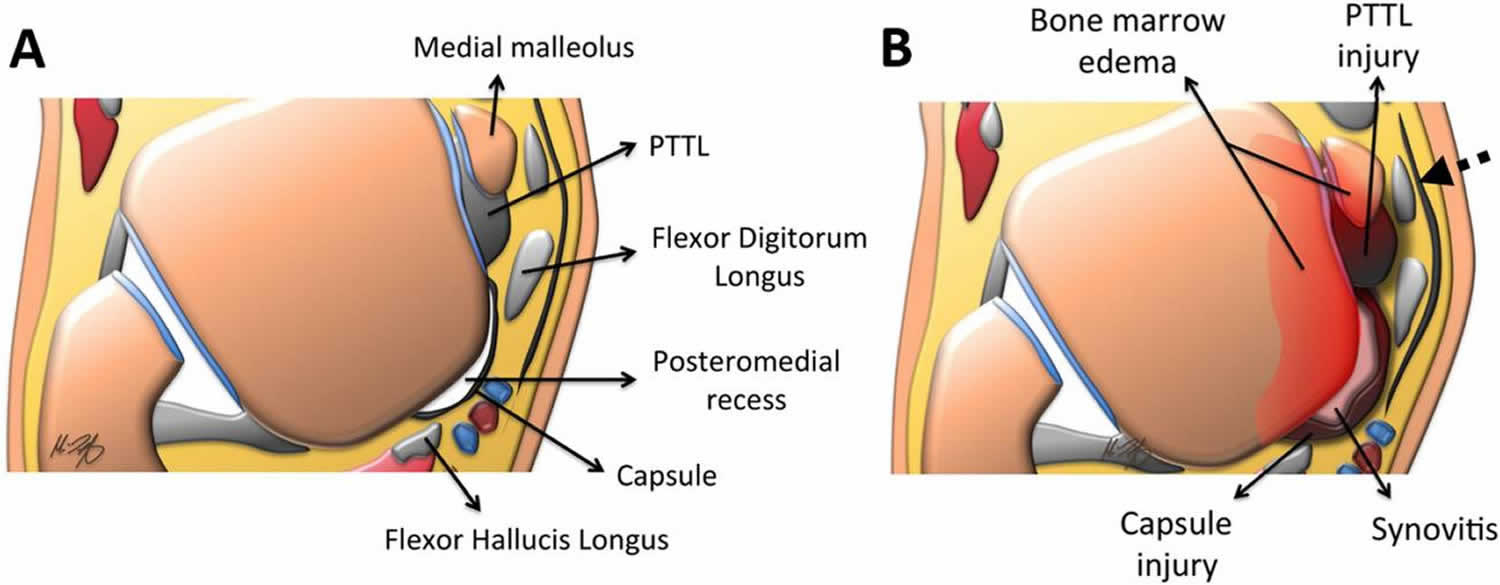
The anterior boundaries of the posteromedial recess are the medial malleolus and posterior tibiotalar ligament (PTTL). The lateral side is formed by the talar dome and posterior process of the talus. Peripherally, the recess is demarcated by the posteromedial joint capsule, neurovascular bundle and flexor hallucis longus tendon (Figure 6).
The common precipitating injury for posteromedial ankle impingement is a plantar flexion, inversion and internal rotation trauma. This can lead to damage to the posterior tibiotalar ligament (PTTL) and associated synovitis, which can partially encase the posterior tibialis tendon (PTT) (40% of cases), the flexor hallucis longus tendon (16% of cases) or the flexor digitorum longus tendon (8% of cases) 23.
It was first described by Liu and Mirzayan 24 in 1993 and remains one of the least common ankle impingement syndromes 25. Commonly, the patient presents with pain over the posteromedial aspect of the ankle with both passive and active movement 26. Owing to the strong nature of the deltoid ligament, injury occurs in 15% of ligamentous traumas of the ankle and leads to an impingement syndrome only in a fraction of those cases 27. Also, given the high-energy nature of an injury that could lead to deltoid ligament rupture, a high percentage of patients will have concomitant osteochondral injuries or other ligamentous injury 28.
Figure 6. Posteromedial impingement syndrome
Footnote: Axial illustrations through the level of the talus: (a) the boundaries of the posteromedial recess are the medial malleolus and posterior tibiotalar ligament (PTTL) anteriorly, the talar dome and posterior process of the talus laterally and the posteromedial joint capsule, neurovascular bundle and flexor hallucis longus tendon peripherally. (b) In posteromedial impingement, a constellation of findings can be seen including an injured and thickened posterior tibiotalar ligament (PTTL), associated synovitis, posteromedial joint capsule injury and bone marrow oedema. The close proximity of the enlarged posteromedial recess to the flexor tendons, especially the tibialis posterior (dashed arrow), which is affected in approximately 40% of cases, can be noted.
[Source 13 ]Ankle impingement syndrome causes
After an ankle sprain, 20-40% of patients have chronic ankle pain; of these patients, approximately one third has pain that is related to ankle impingement.
The most common mechanism of an acute ankle impingement injury is plantar flexion/inversion injury that results in acute ankle sprain (eg, basketball player landing on opponent’s shoe, cross-country runner stepping in a hole).
Anterior ankle impingement
Seen in activities that cause forced ankle dosiflexion. Seen in soccer players while kicking sometimes termed “footballer’s ankle” and ballet dancers especially with pliés, which are lunging maneuvers. Chronic damage or microtrauma leads to subsequent bone spur formation (anterior tibiotalar spurs), which cause subsequent limitation of movement and pain.
Anterior ankle impingement generally refers to entrapment of structures along the anterior margin of the tibiotalar joint in terminal dorsiflexion. Multiple osseous and soft tissue anatomic abnormalities have been recognized as causative factors.
Characteristic spurs or “exostoses” at the anterior distal tibia and dorsal talar neck have long been observed in athletes with anterior ankle pain and limited motion. Isolated talofibular lesions have also been described 29. The morphology of anterior tibiotalar exostoses has been well-studied, and cadaveric dissections have found these lesions to be intra-articular, well within the distal tibial and dorsal talar capsular attachments 30.
Although they are often referred to as “kissing osteophytes”, these tibial and talar spurs surprisingly often do not actually overlap and abut. Evaluation of preoperative CT scans has shown that talar spurs generally lie medial to the midline of the talar dome and tibial spurs are generally located laterally 31. A distinct trough in the articular talar dome often “accepts” the tibial osteophyte during dorsiflexion. Kim, et al. 32 referred to this as a “tram-track lesion”, while Raikin, et al. 33 termed it a “divot sign”. Subsequent studies have confirmed a high rate of corresponding talar cartilage lesions (80.7 %) and loose bodies in patients with distal tibial lesions 34.
Anterior intra-articular soft tissues may contribute to impingement in isolation or in conjunction with bony lesions. A triangular soft tissue mass composed primarily of adipose and synovial tissues exists in the anterior joint space. These tissues are compressed after 15° of dorsiflexion in asymptomatic individuals 35. Anterior osteophytes may limit the space available for this soft tissue and exacerbate its entrapment, resulting in chronic inflammation, synovitis, and capsuloligamentous hypertrophy. Post-traumatic fibrous bands 36, thickened anterior tibiofibular ligaments 37 and synovial plica 38, have also been identified as causative factors.
While the impinging anatomic lesions have been well described, their exact cause is less well understood. Early reports hypothesized spurs to be enthesophytes caused by traction to the anterior capsule during repetitive plantar flexion 39. However, anatomic studies have demonstrated the chondral margins and lesions to be deep to the joint capsule rather than at its attachment, resulting in the traction, disproving the traction theory 30. More recent observations of athletic populations commonly affected by anterior impingement have led to hypotheses that pathology occurs due to repetitive impaction injury to the anterior chondral margin from hyper-dorsiflexion or direct impact from an external object such as a soccer ball 9.
Chronic lateral ankle instability has also been hypothesized to contribute to the development of both bony and soft tissue lesions associated with anterior impingement due to abnormal repetitive micromotion 40. Multiple studies have examined the prevalence of associated anterior impingement lesions at the time of arthroscopy in patients undergoing stabilization procedures for lateral ankle instability. Soft tissue lesions, such as synovitis in the anterior compartment or anterior lateral gutter, have been observed with high frequency (63–100 %), while anterior tibial osteophytes have often been found consistently (12–26.4 %) 41. In one study 42, patients undergoing a Brostrom procedure had 3.37 times the incidence of bone spurs than matched asymptomatic controls.
Posterior ankle impingement
Posterior ankle impingement results from compression of structures posterior to the tibiotalar and talocalcaneal articulations during terminal plantar flexion. Similarly, this can be caused by multiple osseous and soft tissue causes in isolation or in combination. Clinically, the posterior impingement syndrome presents with chronic pain and swelling within the posterior ankle. Classically, this is seen with activities that cause extreme plantar flexion, such as ballet, soccer, football and downhill running 20.
The two main proposed mechanisms of posterior impingement are 43:
- An acute plantar hyperflexion injury and
- Chronic repetitive microtrauma.
The similarity between the two mechanisms revolves around the posterior soft tissues, which may become secondarily hypertrophied and compressed between the posterior talus and the calcaneus. The presence of an osseous body (os trigonum or prominent Stieda’s process) can further narrow this space, which has led to its other name of “os trigonum syndrome” (Figure 5) 20. This increased compression leads to damage to the regional tendons and ligaments. Flexor hallucis longus tenosynovitis is commonly involved (Figure 5) 44. Important differentials include Achilles tendinosis/tear, arthrosis, acute posterior talar process fractures, flexor hallucis longus tenosynovitis, Haglund’s syndrome, osteochondral lesions and retrocalcaneal bursitis 45.
Hypertrophy or tear of the posterior inferior talofibular ligament, transverse talofibular ligament, tibial slip, or pathologic labrum on the posterior ankle joint can lead to posterior ankle impingement, which may pinch on the os trigonum or posterior talus of calcaneus. Posterior ankle impingement syndrome can also result from pathology of the os trigonum-talar process, ankle osteochondritis, flexor hallucis longus tenosynovitis, subtalar joint disease, and fracture. Pain is caused by forced plantar flexion and push-off maneuvers, as seen in dancing, kicking, gymnastics, or downhill-running types of activities 46. In ballet dancers, forcing turnout of the foot can predispose to this condition 47.
Pathology associated with the lateral (trigonal) process of the posterior talus is the most common cause of posterior impingement. Anatomic variants of this structure have been well described. A Stieda process refers to an elongated tubercle. An os trigonum may represent failure of fusion of a secondary ossification center to the talar body, although this structure has been heavily debated in the orthopedic and radiologic literature. Impingement related to the trigonal process can result from acute fracture, chronic injury due to repetitive microtrauma, or mechanical irritation of the surrounding soft tissues 48.
Less commonly, posterior symptoms may result from tibiotalar or subtalar degenerative joint disease due to osteophyte impingement or associated reactive hypertrophic capsule and synovium. Post-traumatic sequelae from fracture malunion of the posterior malleolus, talus, or calcaneus may also occur 49. A case of talar osteonecrosis resulting in posterior impingement has also been reported 50.
Various soft tissue structures may cause posterior impingement symptoms as well. Posterior capsuloligamentous injury due to repetitive or acute hyperflexion can lead to inflammation, scarring and thickening of the capsule, posterior inferior tibiofibular ligament, and posterior fibers of the deltoid ligament 51. The flexor hallucis longus tendon, running between the medial and lateral posterior processes of the talus, is commonly affected by tenosynovitis and tendinosis. The tendinopathy may result from overuse or secondary to irritation from surrounding abnormal bony anatomy. Anatomic soft tissue variants, such as the posterior intermalleolar ligament and several anomalous muscles, have been described as other sources of impingement 52.
Anterolateral ankle impingement
Common causes are inversion ankle injuries and sprains sustained while playing basketball (45%), volleyball (25%), or soccer (31%). Injury to the ligament or joint capsule may lead to synovitis, scar tissue, hypertrophied soft tissue, and, ultimately, impingement.
Posteromedial impingement syndrome
The common precipitating injury for posteromedial ankle impingement is a plantar flexion, inversion and internal rotation trauma. This can lead to damage to the posterior tibiotalar ligament (PTTL) and associated synovitis, which can partially encase the posterior tibialis tendon (PTT) (40% of cases), the flexor hallucis longus tendon (16% of cases) or the flexor digitorum longus tendon (8% of cases) 23.
It was first described by Liu and Mirzayan 24 in 1993 and remains one of the least common ankle impingement syndromes 25. Commonly, the patient presents with pain over the posteromedial aspect of the ankle with both passive and active movement 26. Owing to the strong nature of the deltoid ligament, injury occurs in 15% of ligamentous traumas of the ankle and leads to an impingement syndrome only in a fraction of those cases 27. Also, given the high-energy nature of an injury that could lead to deltoid ligament rupture, a high percentage of patients will have concomitant osteochondral injuries or other ligamentous injury 28.
Syndesmosis impingement
Tearing of the syndesmosis or the anterior talofibular ligament results in chronic instability and extrusion of the anterolateral talus, leading to syndesmotic impingement. Ice hockey, football, and soccer players often sustain this type of injury.
Ankle impingement syndrome symptoms
- Anterior ankle impingement: Chronic ankle pain occurs, usually presenting as persistent anterior ankle pain or disability after an ankle sprain. Anterior ankle pain is present with a subjective feeling of stiffness or “blocking” on dorsiflexion. The pain is usually most severe with dorsiflexion, and dorsiflexion may be limited on examination. It is possible to do the anterior impingement test, in which the patient lunges forward maximally with the heel on the floor. If this test reproduces the pain, the test is positive and suggestive of anterior impingement. Swelling over the anterior aspect of the ankle may be present.
- Anterolateral ankle impingement: Chronic vague pain over the anterolateral ankle occurs, usually associated with cutting and pivoting movements. Tenderness is noted along the lateral gutter and anterior talofibular ligament. Proprioception may be poor in these patients.
- Syndesmosis impingement: Syndesmotic or a “high” ankle sprain occurs in up to 10% of all ankle injuries. Extreme tenderness along the syndesmosis and interosseous membrane is noted, along with pain on bimalleolar compression of the syndesmosis and on passive external rotation stress of the ankle.
- Posterior impingement: Posterior impingement syndrome is usually located posteriorly or posterolaterally following an ankle sprain. The diagnosis of posterior ankle impingement is often difficult, requiring a high index of clinical suspicion. Posterior impingement often causes lingering pain, swelling, and catching of a synovial nodule, and it may be worse with forced plantar flexion. If further confirmation is necessary, local anesthetic can be injected around the posterior talus, and then the impingement test (reproduction of pain with passive plantarflexion of the ankle) can be performed without pain.
Ankle impingement syndrome diagnosis
Physical examination
A comprehensive physical examination of the foot and ankle should be performed when assessing for impingement syndromes. The ankle and foot are inspected for abnormal alignment, joint effusion, or soft tissue edema. The bone and soft tissue structures are systematically palpated to assess for localized tenderness. While anterior or anterolateral tenderness is characteristic in anterior impingement, posterior impingement signs can be more difficult to elicit and localize, as structures are deeper. Posteromedial ankle tenderness with resisted plantar flexion of the first metatarsophalangeal joint is more consistent with flexor hallucis longus pathology, while posterolateral tenderness with forced ankle plantar flexion is more likely to involve pathology associated with the trigonal process.
Passive and active ranges of motion of the joints bilaterally are measured, including dorsiflexion, plantar flexion, subtalar, and midfoot motions. Laterally, the peroneal tendon is assessed for tenderness, deformity, or subluxation. The sural nerve is evaluated for sensitivity. Posteriorly, the Achilles tendon is assessed for fusiform enlargement or retrocalcaneal bursitis. Medially, the tibial nerve is evaluated for tarsal tunnel syndrome, and the posterior tibial tendon’s function is assessed. The anterior drawer and talar tilt tests of the tibiotalar joint are performed to exclude ankle instability. Finally, a straight leg raise test in the seated or supine position may be done to exclude an L5 or S1 radiculopathy.
Imaging studies
Imaging of an ankle suspected of impingement should begin with a plain x-ray series, as the diagnosis is often confirmed with simple radiographs. Initial views should include weight-bearing AP, lateral, and mortise projections. Careful attention is given to the lateral view, assessing for exostoses on distal anterior tibia and dorsal talar neck and posterior bony abnormalities, including a Stieda process or os trigonum.
Alternative oblique views have been described for both anterior and posterior impingement lesions to better assess for bony abnormalities, as standard views can miss some lesions. To detect anteromedial lesions, the beam is aimed 45° craniocaudad with the leg externally rotated 30° 53. The utility of the oblique anteromedial impingement view has been confirmed to have a higher sensitivity in detecting both tibial (85 vs. 40 %) and talar (73 vs. 32 %) osteophytes when added to a standard lateral radiograph 54. Lesions associated with the trigonal process are best viewed on a 25° external rotation-lateral view 55. Dynamic hyper-plantar-flexed or dorsiflexed laterals can be considered to demonstrate abnormal bony contact.
Advanced imaging, such as magnetic resonance imaging (MRI), may also be considered when the diagnosis remains inconclusive because of its advantage in identifying osseous and soft-tissue abnormalities. Images should be evaluated for bone edema, effusion, synovitis, tenosynovitis, and concomitant chondral injury. In anterior soft tissue impingement, the anterolateral gutter may contain hypertrophic synovium or fibrosis. Increased marrow signal intensity at the trigonal process or os trigonum is suggestive of an acute injury or chronic stress fracture 56. The efficacy of MRI in evaluating soft tissue impingement lesions is variable, with reported sensitivities 42–89 % and specificities 75–100 % 57. Computed tomography has been used in defining the morphology of bony lesions for planning surgical resections 58. Recently, ultrasound has also gained popularity as a reliable and inexpensive modality in evaluating impingement lesions and administering therapeutic injections 59.
Ankle impingement syndrome treatment
Nonsurgical treatment
Nonsurgical treatment remains the initial approach to the management of both anterior and posterior impingement syndromes, despite limited evidence of its efficacy. For acute symptoms, a period of rest and an avoidance of provocative activities are recommended. This approach can be supplemented with ice, non-steroidal antiinflammatory drugs (NSAIDs) or cast immobilization in more severe cases. In chronic cases, shoe modifications, including heel lift orthoses to prevent dorsiflexion, have been utilized. Physical therapy protocols focus on improving ankle stability and optimizing proprioception. Authors have reported successful symptom relief with ultrasound-guided corticosteroid injections, which may also have diagnostic uses 60. Intra-articular anesthetic (lidocaine) ankle injection can be used as a differential tool to distinguish between ankle pain and subtalar pain.
Electrotherapeutic modalities may also be helpful.
In ballet dancers, technique assessment is helpful and essential to prevent further pain and injury.
Surgical treatment
Surgical intervention is generally indicated for persistent symptoms which have not responded to non-operative treatment, affected normal activities of daily living or athletic performance, and correlated with physical exam and imaging findings. The surgical approach and technique vary by the anatomic region and pathology involved.
Anterior ankle impingement
Surgical goals for the treatment of anterior impingement involve removing the offending pathologic lesion contributing to the symptoms. This may involve resection or debridement of bony lesions, soft tissue lesions, or both. Early studies described the use of open anterior or lateral arthrotomy 39. A lateral arthrotomy is often still utilized if a lateral ligamentous procedure is being performed concurrently. However, open approaches have largely been replaced by arthroscopic techniques 61.
Hawkins is credited with reporting the first arthroscopic approach for the treatment of bony anterior ankle impingement in 1988, citing improved visualization with a less invasive approach 62. Standard anterolateral and anteromedial portals are typically utilized and may be extended with conversion to open arthrotomy if necessary. An arthroscopic burr is used to reshape the anterior tibia and dorsal talus to their native contours. A combination of a shaver and electrothermal device is used to debride hypertrophic or inflamed synovium and fibrotic tissue. Intraoperative fluoroscopy may be used to confirm adequate resection of spurs.
Zwiers et al. 63 conducted a recent systematic review examining the results of the arthroscopic treatment of anterior impingement. The review included 19 studies and 905 patients, with an average age of 32.7 years. At a combined mean follow-up 35.3 months, 74–100 % of patients were satisfied with the results of their procedure. American Orthopaedic Foot and Ankle Society (AOFAS) scores improved consistently, ranging from 34–75 preoperatively and increasing to 83.5–92 postoperatively. There was a 5.1 % overall complication rate, with 1.2 % considered major complications. This is consistent with a 4 % complication rate in a previous review by Simonson et al. 64.
Posterior ankle impingement
Similarly, the surgical goal of treating posterior impingement involves resection of the causative anatomy. Most commonly, symptom relief is achieved by excision of a painful trigonal process or os trigonum, with debridement of surrounding inflammatory or hypertrophic soft tissues.
Posterior pathology can be targeted through an open lateral, open medial, or endoscopic approach. A lateral approach allows for more direct access to the trigonal process with less risk to the medial neurovascular bundle. A medial approach allows for concomitant flexor hallucis longus pathology to be addressed more easily. Since 2000, posterior endoscopic approaches have gained popularity, with the potential for faster return to sport and lower complication rates 65. With the patient positioned prone, posteromedial and posterolateral hindfoot portals adjacent to the Achilles tendon typically provide excellent access to extra-articular posterior structures.
Ribbans et al. 18 reviewed 47 papers consisting of 905 patients treated surgically with both open and endoscopic approaches for posterior impingement. Eighty-one percent of symptoms were attributed to osseous pathology. In the included series, 67–100 % of patients experienced good or excellent outcomes. Zwiers et al. 66 conducted a similar systematic review including 16 studies. Significantly lower complication rates (7.2 vs. 15.9 %) and earlier return to full activity (11.3 vs. 16 weeks) were found with endoscopic surgery.
Rehabilitation program
Postoperatively, advise posterior splinting for 1 week, as well as a supportive brace and elastic compression stocking. Physical therapy is initiated at 2-3 weeks for strengthening, range of motion, proprioception, and sport-specific rehabilitation.
References- Lavery, K.P., McHale, K.J., Rossy, W.H. et al. Ankle impingement. J Orthop Surg Res 11, 97 (2016). https://doi.org/10.1186/s13018-016-0430-x
- Vaseenon, T., Amendola, A. Update on anterior ankle impingement. Curr Rev Musculoskelet Med 5, 145–150 (2012). https://doi.org/10.1007/s12178-012-9117-z
- Wolin I, Glassman F, Sideman S, Levinthal DH. Internal derangement of the talofibular component of the ankle. Surg Gynecol Obstet. 1950 Aug. 91(2):193-200.
- Waller JF. Hindfoot and midfoot problems. Symposium on the foot and leg. Mack RP, ed. Running Sports. St. Louis, Mo: Mosby; 1982. pp 64-71.
- Bassett FH 3rd, Gates HS 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990 Jan. 72(1):55-9.
- Hamilton WG. Tendonitis about the ankle joint in classical ballet dancers. Am J Sports Med. 1977 Mar-Apr. 5(2):84-8.
- Morris LH. Athlete’s ankle. J Bone Joint Surg Am 1943; 25: 220.
- McMurray TP. Footballer’s ankle. J Bone Joint Surg Am 1950; 32: 68–9.
- Tol JL, et al. The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med. 2002;30(1):45–50.
- Tol JL, van Dijk CN. Etiology of the anterior ankle impingement syndrome: a descriptive anatomical study. Foot Ankle Int 2004; 25: 382–6.
- Amendola N, Drew N, Vaseenon T, Femino J, Tochigi Y, Phisitkul P. CAM-type impingement in the ankle. Iowa Orthop J 2012; 32: 1–8.
- Massada JL. Ankle overuse injuries in soccer players. Morphological adaptation of the talus in the anterior impingement. J Sports Med Phys Fitness 1991; 31: 447–51.
- Berman Z, Tafur M, Ahmed SS, Huang BK, Chang EY. Ankle impingement syndromes: an imaging review. Br J Radiol. 2017;90(1070):20160735. doi:10.1259/bjr.20160735 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5685116
- Bassett FH, 3rd, Gates HS, 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am 1990; 72: 55–9. doi: https://doi.org/10.2106/00004623-199072010-00009
- Mosier-La Clair SM, Monroe MT, Manoli A. Medial impingement syndrome of the anterior tibiotalar fascicle of the deltoid ligament on the talus. Foot Ankle Int 2000; 21: 385–91.
- Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med 2010; 38: 2017–24. doi: https://doi.org/10.1177/0363546510369335
- Russell JA, et al. Pathoanatomy of anterior ankle impingement in dancers. J Dance Med Sci. 2012;16(3):101–8.
- Ribbans WJ, et al. The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg. 2015;21(1):1–10.
- Mansingh A. Posterior ankle impingement in fast bowlers in cricket. West Indian Med J. 2011;60(1):77–81.
- Karasick D, Schweitzer ME. The os trigonum syndrome: imaging features. AJR Am J Roentgenol 1996; 166: 125–9. doi: https://doi.org/10.2214/ajr.166.1.8571860
- O’Rahilly R. A survey of carpal and tarsal anomalies. J Bone Joint Surg Am 1953; 35: 626–42.
- Stieda L. Ueber secundäre fusswurzelknochen. Arch Phys Wiss Med 1869: 108–11.
- Giannini S, Buda R, Mosca M, Parma A, Di Caprio F. Posterior ankle impingement. Foot Ankle Int 2013; 34: 459–65. doi: https://doi.org/10.1177/1071100713477609
- Liu SH, Mirzayan R. Posteromedial ankle impingement. Arthroscopy 1993; 9: 709–11. doi: https://doi.org/10.1016/s0749-8063(05)80514-6
- Cerezal L, Abascal F, Canga A, Pereda T, Garcia-Valtuille R, Perez-Carro L, et al. . MR imaging of ankle impingement syndromes. AJR Am J Roentgenol 2003; 181: 551–9. doi: https://doi.org/10.2214/ajr.181.2.1810551
- Paterson RS, Brown JN. The posteromedial impingement lesion of the ankle. A series of six cases. Am J Sports Med 2001; 29: 550–7.
- Cetti R. Conservative treatment of injury to the fibular ligaments of the ankle. Br J Sports Med 1982; 16: 47–52. doi: https://doi.org/10.1136/bjsm.16.1.47
- van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br 1996; 78: 562–7.
- Ahn JY, Choi HJ, Lee WC. Talofibular bony impingement in the ankle. Foot Ankle Int. 2015;36(10):1150–5.
- Hayeri MR, Trudell DJ, Resnick D. Anterior ankle impingement and talar bony outgrowths: osteophyte or enthesophyte? Paleopathologic and cadaveric study with imaging correlation. AJR Am J Roentgenol. 2009;193(4):W334–8.
- Berberian WS, et al. Morphology of tibiotalar osteophytes in anterior ankle impingement. Foot Ankle Int. 2001;22(4):313–7.
- Kim SH, Ha KI, Ahn JH. Tram track lesion of the talar dome. Arthroscopy. 1999;15(2):203–6.
- Raikin SM, Cooke PH. Divot sign: a new observation in anterior impingement of the ankle. Foot Ankle Int. 1999;20(8):532–3.
- Moon JS, et al. Cartilage lesions in anterior bony impingement of the ankle. Arthroscopy. 2010;26(7):984–9.
- Tol JL, van Dijk CN. Etiology of the anterior ankle impingement syndrome: a descriptive anatomical study. Foot Ankle Int. 2004;25(6):382–6.
- Valkering KP, et al. “Web impingement” of the ankle: a case report. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1289–92.
- Akseki D, et al. The distal fascicle of the anterior inferior tibio-fibular ligament as a cause of anterolateral ankle impingement: results of arthroscopic resection. Acta Orthop Scand. 1999;70(5):478–82.
- Rosenbaum AJ, et al. Ankle impingement caused by an intra-articular plica: a report of 2 cases. Foot Ankle Spec. 2016;9(1):79–82.
- O’Donoghue DH. Impingement exostoses of the talus and tibia. J Bone Joint Surg Am. 1957;39-A(4):835–52. discussion, 852; passim.
- Cannon LB, Hackney RG. Anterior tibiotalar impingement associated with chronic ankle instability. J Foot Ankle Surg. 2000;39(6):383–6.
- Odak S, et al. Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int. 2015;36(9):1045–9.
- Scranton Jr PE, McDermott JE, Rogers JV. The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot Ankle Int. 2000;21(8):657–64.
- Hayashi D, Roemer FW, D’Hooghe P, Guermazi A. Posterior ankle impingement in athletes: pathogenesis, imaging features and differential diagnoses. Eur J Radiol 2015; 84: 2231–41. doi: https://doi.org/10.1016/j.ejrad.2015.07.017
- Hedrick MR, McBryde AM. Posterior ankle impingement. Foot Ankle Int 1994; 15: 2–8. doi: https://doi.org/10.1177/107110079401500102
- Jordan LK, 3rd, Helms CA, Cooperman AE, Speer KP. Magnetic resonance imaging findings in anterolateral impingement of the ankle. Skeletal Radiol 2000; 29: 34–9.
- Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005 Oct. 13(6):365-71.
- Alfredson H, Cook J, eds. Pain in the Achilles region. Brukner P, Khan K. Clinical Sports Medicine. 2nd ed. New York: McGraw-Hill; 2000.
- Mouhsine E, et al. Post-traumatic overload or acute syndrome of the os trigonum: a possible cause of posterior ankle impingement. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):250–3.
- Lui TH. Posterior ankle impingement syndrome caused by malunion of joint depressed type calcaneal fracture. Knee Surg Sports Traumatol Arthrosc. 2008;16(7):687–9.
- Cortes ZE, Harris AM, Baumhauer JF. Posterior ankle pain diagnosed by positional MRI of the ankle: a unique case of posterior ankle impingement and osteonecrosis of the talus. Foot Ankle Int. 2006;27(4):293–5.
- Peace KA, et al. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59(11):1025–33.
- Seipel R, et al. The peroneocalcaneus internus muscle: an unusual cause of posterior ankle impingement. Foot Ankle Int. 2005;26(10):890–3.
- van Dijk CN, et al. Oblique radiograph for the detection of bone spurs in anterior ankle impingement. Skelet Radiol. 2002;31(4):214–21.
- Tol JL, et al. The anterior ankle impingement syndrome: diagnostic value of oblique radiographs. Foot Ankle Int. 2004;25(2):63–8.
- Wiegerinck JI, et al. The posterior impingement view: an alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30(10):1311–6.
- Bureau NJ, et al. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215(2):497–503.
- Ferkel RD, et al. MRI evaluation of anterolateral soft tissue impingement of the ankle. Foot Ankle Int. 2010;31(8):655–61.
- Takao M, et al. Arthroscopic treatment for anterior impingement exostosis of the ankle: application of three-dimensional computed tomography. Foot Ankle Int. 2004;25(2):59–62.
- Pesquer L, et al. US in ankle impingement syndrome. J Ultrasound. 2014;17(2):89–97.
- Jose J, et al. Sonographically guided therapeutic injections in the meniscoid lesion in patients with anteromedial ankle impingement syndrome. Foot Ankle Spec. 2014;7(5):409–13.
- Buda R, et al. Arthroscopic treatment and prognostic classification of anterior soft tissue impingement of the ankle. Foot Ankle Int. 2016;37(1):33–9.
- Hawkins RB. Arthroscopic treatment of sports-related anterior osteophytes in the ankle. Foot Ankle. 1988;9(2):87–90.
- Zwiers R, et al. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy. 2015;31(8):1585–96.
- Simonson DC, Roukis TS. Safety of ankle arthroscopy for the treatment of anterolateral soft-tissue impingement. Arthroscopy. 2014;30(2):256–9.
- Carreira DS, et al. Outcome of arthroscopic treatment of posterior impingement of the ankle. Foot Ankle Int. 2016;37(4):394–400.
- Zwiers R, et al. Surgical treatment for posterior ankle impingement. Arthroscopy. 2013;29(7):1263–70.