Medial gastrocnemius strain
Medial gastrocnemius strain commonly called “tennis leg”, results from an acute, forceful push-off with the foot that occurs commonly in sports activities such as hill running, jumping, basketball, football, skiing or tennis, but it can occur in any activity 1. A medial gastrocnemius strain is often seen in the intermittently active athlete, often referred to as the “weekend warrior” 2. One mechanism that occurs is on the back leg during a lunging shot, in which the knee is extended while the foot is dorsiflexed. This action puts maximal tension on the gastrocnemius muscle as the lengthened muscle is contracted at the “push off,” resulting in a medial calf injury. The classic presentation is of a middle-aged male tennis player who suddenly extends the knee with the foot in dorsiflexion, resulting in immediate pain, disability, and swelling. Pain and disability can last months to years depending on the severity and effectiveness of initial treatment 3.
Medial calf injuries are most commonly seen acutely, but up to 20% of affected patients report a prodrome of calf tightness several days before the injury, thus suggesting a potential chronic predisposition.
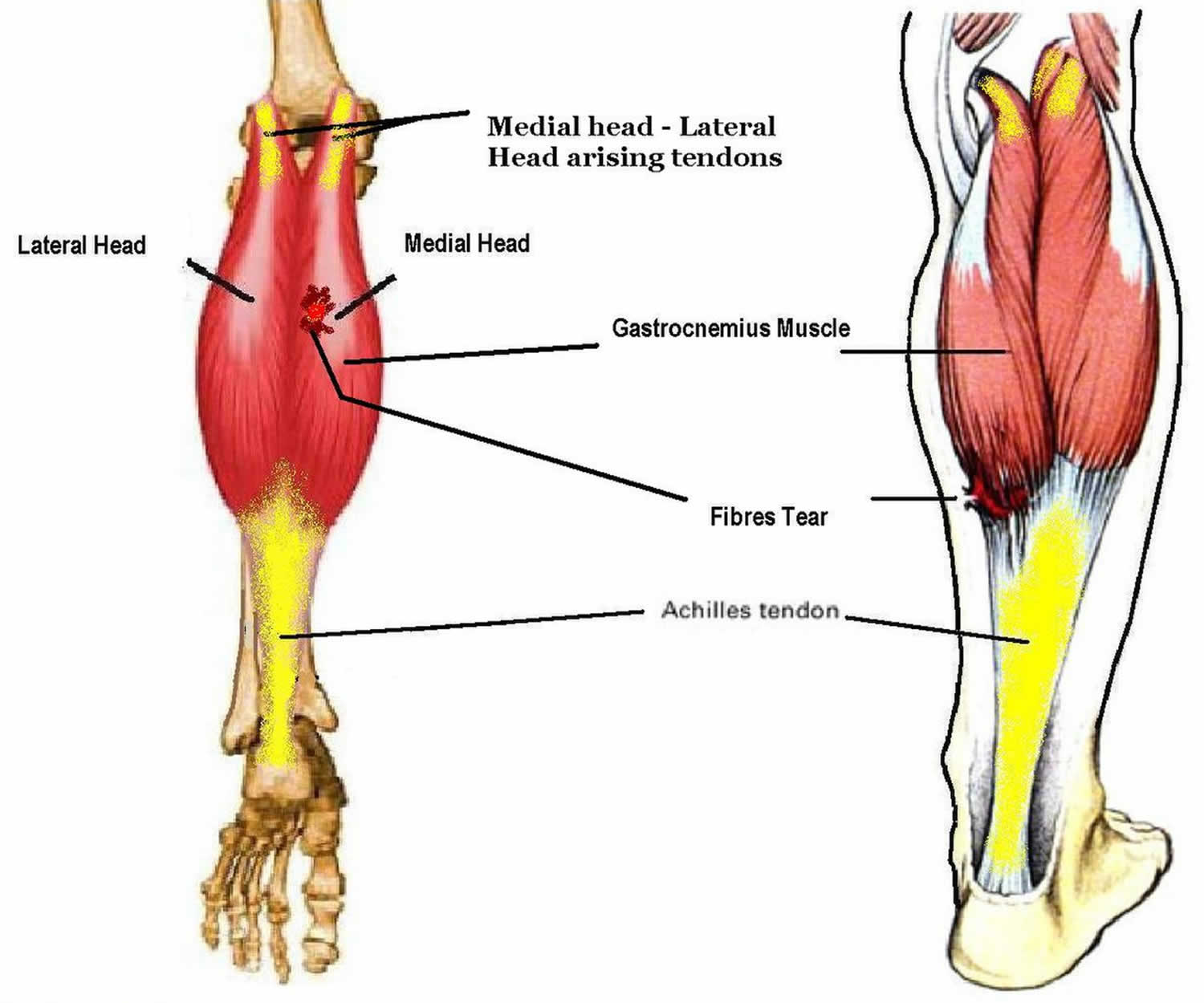
Medial gastrocnemius injuries occur more commonly in men than in women, and these injuries usually afflict athletes and others in the fourth to sixth decade of life. Gastrocnemius strain may also occur in younger athletes as named “tennis leg” 4. The term is derived from the posture to serve tennis, which involves maximal knee extension and ankle dorsiflexion. The medial head of the gastrocnemius muscle is injured more commonly than the lateral head as some studies have shown the muscular activity to be more active at the medial head than the lateral head 5.
An unusual presentation of a medial gastrocnemius injury during namaz praying 6. The namaz praying requires the participant to kneel with the head touching the group. The calf muscle is eccentrically stretched when the participant attempts to stand up. Yilmaz et al 7, who performed a retrospective study of the sonographic and magnetic resonance image (MRI) findings of patients referred over 7 years with leg pain and swelling. Of 543 patients, 14 had a final diagnosis of medial gastrocnemius rupture that occurred during namaz praying. Nine of 14 (64.2%) patients had incomplete tears at the musculotendinous junction, and 5 of 14 (35.8%) patients had partial tears 7.
The diagnosis in 4 of 14 (28.6%) patients was misattributed to deep vein thrombosis due to clinical findings and presentation, associated fluid collection between the gastrocnemius and soleus muscles was found in 11 of 14 (78.5%) patients, and isolated fluid collection between the gastrocnemius and soleus muscles was seen in 1 patient 7. The investigators suggested ultrasonography and MRI can be used to correctly diagnose patients with medial gastrocnemius injuries.
The gastrocnemius muscle is considered at high risk for strains because it crosses two joints (the knee and ankle) and has a high density of type two fast twitch muscle fibers 8. The combination of biarthrodial architecture leading to excessive stretch and rapid forceful contraction of type two muscle fibers results in strain. This mechanism of injury conjures up the image of a cracking whip. Consequently, strains of the gastrocnemius have historically been called coup de fouet or snap of the whip 1.
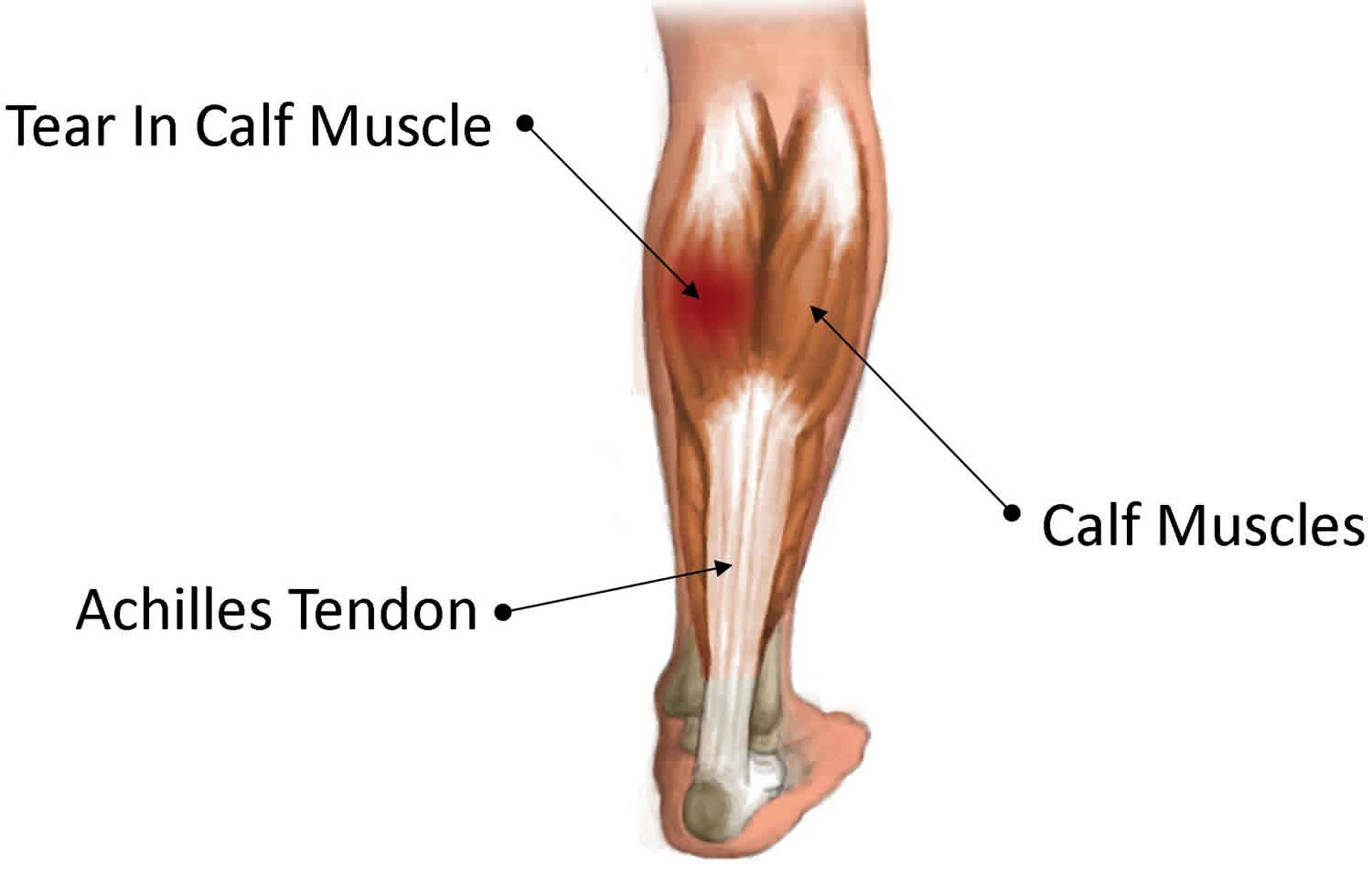
Figure 1. Gastrocnemius muscle
Gastrocnemius muscle functional anatomy
The medial head of the gastrocnemius muscle originates from the posterior aspect of the medial femoral condyle, and as it courses distally, the medial head merges with the lateral head of the gastrocnemius (see Figure 1 above). Further distally, the joined heads of the gastrocnemius merge with the soleus muscle-tendon complex to form the Achilles tendon. The main function of the gastrocnemius muscle is to plantar flex the ankle, but it also provides some knee flexion, as well as contributes to the posterior stability of the knee and partially to the motion of the menisci with flexion/extension of the knee. Throughout the belly of the muscle, the medial gastrocnemius has several origins of tendinous formation. Most strains occur at this musculotendinous junction.
Using shear wave elastography, Yoshida et al found that the elastic moduli of the medial gastrocnemius vary significantly at different points on the aponeurosis, specifically, the point at the center of the musculotendinous junction and those 10 mm proximal and 10 mm distal to it, with the highest modulus found at the distal point (4.83 m/s) and the lowest at the proximal (2.82 m/s). Moreover, the distal modulus, as well as the elastic modulus at a point on the muscle belly, was found to be significantly higher in males than in females, while the muscle-belly modulus was higher in younger persons than in those in middle age 9.
Medial gastrocnemius strain staging
Grade 1 Injury (Mild)
The patients may feel a sharp pain at the time of injury or pain with activity. They are usually able to continue the activity. There may be no or minimal loss of strength and range of motion. One MRI study exposes bright signals on fluid-sensitive sequences with less than 5% feathery appearance of muscle fiber involved. Pathologically, grade 1 injury indicates less than 10% of muscle fibers disrupted.
Grade 2 Injury (Moderate)
The patient cannot walk at the moment of injury. The patient may complain of weakness during ankle dorsiflexion and plantar flexion. One MRI study concedes the change in myotendinous junction as edema or hemorrhage. Grade 2 injury implies 10% to 50% disruption of muscle fibers.
Grade 3 Injury (Severe)
There may be a palpable defect on the affected calf. The MRI findings include complete disruption of continuity of muscle, wavy tendon morphology and retraction and extensive hemorrhage or edema. Dixon et al. suggested that grade 3 injury indicates 50% to 100% disruption of muscle fibers 10.
Medial gastrocnemius strain causes
The medial gastrocnemius injury usually occurs when an eccentric force is applied to the gastrocnemius muscle, which usually happens when the knee is extended, the ankle is dorsiflexed, and the gastrocnemius attempts to contract in the already lengthened state 11. This is the common position of the back leg in a tennis stroke, and it results in the greatest force to the muscle unit; but medial calf injuries can also occur during a typical contraction of ankle plantar flexion, especially if the athlete is pushing or lifting a large weight or force.
Muscle fatigue and impaired coordination are common factors contributing to gastrocnemius muscle strain. Some research revealed that impaired vascular supply to the gastrocnemius muscle might result in weakness of the musculotendinous unit. Failure of muscle relaxation also plays a role in causing muscle strain. Due to the inability to fully relax, muscle fibers are more vulnerable to stretching injury 4.
Medial gastrocnemius strain symptoms
Typically, the patient feels something stricken on the calf. Accompanying this feeling is an audible pop or snap, sounding like breaking a twig, when the injury to the medial calf occurred is usually reported, and the patient complains of feeling like a stick struck his/her calf. At the moment of injury, there may be no pain. After the victim takes a few steps, the pain develops on the posteromedial part of the calf. Intense pain may make patients unable to walk 4.
The patient complains of pain in the area of the calf, which also radiates to the knee or the ankle. In addition, the patient complains of pain with range of motion (ROM) of the ankle.
The patient complains of a swollen leg that extends down to the foot or ankle, as well as the associated color changes of bruising.
Prodromal symptoms play an interesting role in gastrocnemius muscle injury. Patients may recall similar prodromic discomfort. There might be dull pain first noted on the affected calf 4. One report states that 20% of patients experience prodromic symptoms 12.
Medial gastrocnemius strain complications
The most common complication of a medial gastrocnemius injury is scar-tissue formation, which results in chronic pain or dysfunction that is caused by a functional shortening of the muscle-tendon unit. This scar tissue can then predispose to frequent reinjury. Another complication is the formation of a deep vein thrombosis (DVT) as a result of patient inactivity and trauma.
Medial gastrocnemius strain diagnosis
Physical examination
The physical finding includes bruising (ecchymosis) and tenderness over muscle tear site. A subcutaneous gap may be palpated if there is a frank retraction across the injury site. The patient may have severe pain during passive stretching the calf or resistive plantar flexion 6.
Inspection
- Asymmetric calf swelling and discoloration, potentially spreading to the ankle and foot, is noted on physical examination.
- If the stage of swelling has resolved, a visible defect in the medial gastrocnemius muscle may be evident.
Palpation
- Tenderness is noted upon palpation in the entire medial gastrocnemius muscle, but this tenderness is observed to be exquisitely more painful at the medial musculotendinous junction.
- Depending on the degree of swelling, a palpable defect may be evident at the medial musculotendinous junction; however, with extreme swelling, this finding may not be appreciable.
- Palpation of the Achilles tendon should demonstrate an intact tendon.
- The peripheral pulses should be present and symmetric.
Provocative maneuvers: Moderate to severe pain is demonstrated with passive ankle dorsiflexion (due to stretching of the torn muscle fibers), as well as with active resistance to ankle plantar flexion (due to the firing of the torn muscle fibers).
Imaging studies
Imaging studies can assist in differentiating partial and complete ruptures. The utility of plain films and computed tomography scans in soft tissue injury is limited. Ultrasound offers the advantage of nonionizing radiation and is relatively inexpensive. The examiner should be aware of sonographic findings such as the disruption of the normal fiber arrangement at the myotendinous junction, hematoma, and fluid collection between the gastrocnemius and soleus muscles. Ultrasonography can also differentiate partial from complete tears of the muscle, determine the size of the hematoma. A bigger hematoma usually indicates complete gastrocnemius muscle tear rather than partial tear. Ultrasound can also determine the size of a complete rupture and is helpful in guiding percutaneous aspiration of the hematoma. Deep vein thrombosis can also be scrutinized by using ultrasound, which is sometimes concomitant with gastrocnemius strain 13.
One study 14 of 141 patients with clinically diagnosed tennis leg showed that 67% had a partial tear of medial gastrocnemius, 1.4% had associated plantaris tendon rupture, and 21% had intermuscular fluid collection without medial gastrocnemius muscle tear. Ten percent had deep vein thrombosis without visible gastrocnemius pathology.
Sonography is useful to follow up the healing course. Signs of recovery on sonography include a progressive decrease in the hematoma size, reparative tissue signified by a peripheral hypoechoic area that extends toward the center, and rearrangement of muscle fibers 10.
Magnetic resonance imaging (MRI) is indispensable in certain conditions as it offers outstanding soft tissue imaging. Findings include rupture or discontinuity of muscle fibers and retraction of the torn muscle fibers. MRI also allows differentiation between gastrocnemius and Achilles tendon injury, which can help to improve direct treatment. MRI can also provide an assessment of surrounding connective tissues in some muscle injury cases. Three MRI studies reported that connective tissue injury plays an important role to evaluate the return to sports after muscle injury 15.
Medial gastrocnemius strain treatment
Initial treatment of a medial gastrocnemius injury includes relative rest, ice, compression, elevation (RICE), and early weight bearing, as tolerated. The initial treatment should continue for 24-72 hours. Ice therapy is best instituted over a damp elastic wrap, which also provides compression. Preventing the limb from hanging dependently prevents further swelling. The use of crutches with a feathering gait and bilateral heel lifts is indicated if normal gait is compromised. Active foot and ankle range of motion (ROM) can be carried out if there is pain-free ROM.
Initially, gentle stretching can help lengthen the intramuscular scar of the injured muscle. Later, strengthening, heel raising and proprioceptive exercise should be added as well as core muscles strengthening and general reconditioning. The patient is allowed to ambulate as tolerated and to increase the activity level gradually after the pain subsides. In patients suffering from severe injury, weight bearing of the affected lower extremity should be limited, and a cast or orthosis may be needed for ambulation. Weight-bearing exercise or dorsiflexion stretching should be delayed until the pain subsides.
Pain management should include analgesics as indicated. The simplest, yet least powerful of the recommended analgesics is acetaminophen. Typical doses of 1000-1300 mg, 3-4 times daily can be used as needed. This agent does not affect platelet function but may not greatly control pain. Caution should be used with nonsteroidal anti-inflammatory drugs (NSAIDs) during the acute injury phase, as these agents can predispose the patient to increased bleeding and hematoma formation in the initial days after an injury. Theoretically, cyclooxygenase-2 (COX-2) inhibitors may provide pain control without the risk of bleeding in acute injuries, which is a concern with traditional NSAIDs.
Strengthening and stretching of the injured area should continue for several months to overcome the increased risk for reinjury due to the deposition of scar tissue that is involved in the healing process.
A 2014 randomized trial 16 reported that the use of shock-absorbing insoles during 3 weeks of training on artificial turf resulted in a significant increase in the pain threshold for the medial head of the gastrocnemius muscle.
Other treatment
Ankle/foot bracing should be used to keep the ankle in a position of maximal tolerable dorsiflexion. Studies have shown an increased rate of healing with this intervention.
As with any large muscle strain, hematoma formation can be complicated by heterotopic ossification resulting in myositis ossificans. Studies do support the use of nonsteroidal anti-inflammatory medication, which may help prevent this.
Most patients recover well under non-operative treatment. Surgical repairing of the muscle tear may be needed in certain cases. But the procedure is technically challenging due to the difficulty of performing a suture through muscle tissue. Fibrosis and contracture at the incision site appear to be another concern. The absolute surgical indication is still unclear 17.
Return to play
When an athlete will be able to return to play is predicated on the patient being pain free and recovering full ROM. This period can last 1-12 weeks, depending on the degree of tissue damage that was sustained. Strength testing should reveal that more than 90% of the uninjured side accounts for the patient’s dominance preference.
Medial gastrocnemius strain prognosis
If the above treatments are followed, the prognosis for recovery and return to sports after a medial gastrocnemius injury is excellent. Most studies indicate that gastrocnemius strains mostly have a good prognosis. Most patients can have a marked decrease in pain and return to exercise after adequate management.
References- Fu FH, Stone DA, editors. Sports injuries: mechanisms, prevention, treatment. 2. Philadelphia: Lippincott Williams & Wilkins; 2001.
- Medial Gastrocnemius Strain. https://emedicine.medscape.com/article/91687-overview
- Coughlin MJ, Mann RA, Saltzman CL. Surgery of the foot and ankle. 8. Philadelphia: Mosby; 2006.
- Froimson AI. Tennis leg. JAMA. 1969 Jul 21;209(3):415-6.
- Cibulka M, Wenthe A, Boyle Z, et al. VARIATION IN MEDIAL AND LATERAL GASTROCNEMIUS MUSCLE ACTIVITY WITH FOOT POSITION. Int J Sports Phys Ther. 2017;12(2):233-241.
- Campbell JT. Posterior calf injury. Foot Ankle Clin. 2009 Dec;14(4):761-71.
- Yilmaz C, Orgenc Y, Ergenc R, Erkan N. Rupture of the medial gastrocnemius muscle during namaz praying: an unusual cause of tennis leg. Comput Med Imaging Graph. 2008 Dec. 32(8):728-31.
- Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803–842. doi: 10.1016/j.csm.2006.06.011
- Yoshida K, Itoigawa Y, Maruyama Y, et al. Application of shear wave elastography for the gastrocnemius medial head to tennis leg. Clin Anat. 2016 Sep 4.
- Lee JC, Mitchell AW, Healy JC. Imaging of muscle injury in the elite athlete. Br J Radiol. 2012 Aug;85(1016):1173-85.
- Glazer JL, Hosey RG. Soft-tissue injuries of the lower extremity. Prim Care. 2004 Dec. 31(4):1005-24.
- Shields CL, Redix L, Brewster CE. Acute tears of the medial head of the gastrocnemius. Foot Ankle. 1985 Jan-Feb;5(4):186-90.
- Chang KV, Wu WT, Özçakar L. Ultrasound Imaging for Posterior Knee Pain: Tibial Nerve Schwannoma Not Popliteus Muscle Strain. Med Ultrason. 2017 Apr 22;19(2):237-238.
- Delgado GJ, Chung CB, Lektrakul N, Azocar P, Botte MJ, Coria D, Bosch E, Resnick D. Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002 Jul;224(1):112-9.
- Prakash A, Entwisle T, Schneider M, Brukner P, Connell D. Connective tissue injury in calf muscle tears and return to play: MRI correlation. Br J Sports Med. 2018 Jul;52(14):929-933.
- Madeleine P, Hoej BP, Fernández-de-Las-Peñas C, Rathleff MS, Kaalund S. Pressure pain sensitivity changes after use of shock-absorbing insoles among young soccer players training on artificial turf: a randomized controlled trial. J Orthop Sports Phys Ther. 2014 Aug. 44(8):587-94.
- Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Curr Rev Musculoskelet Med. 2009 Jun;2(2):74-7.