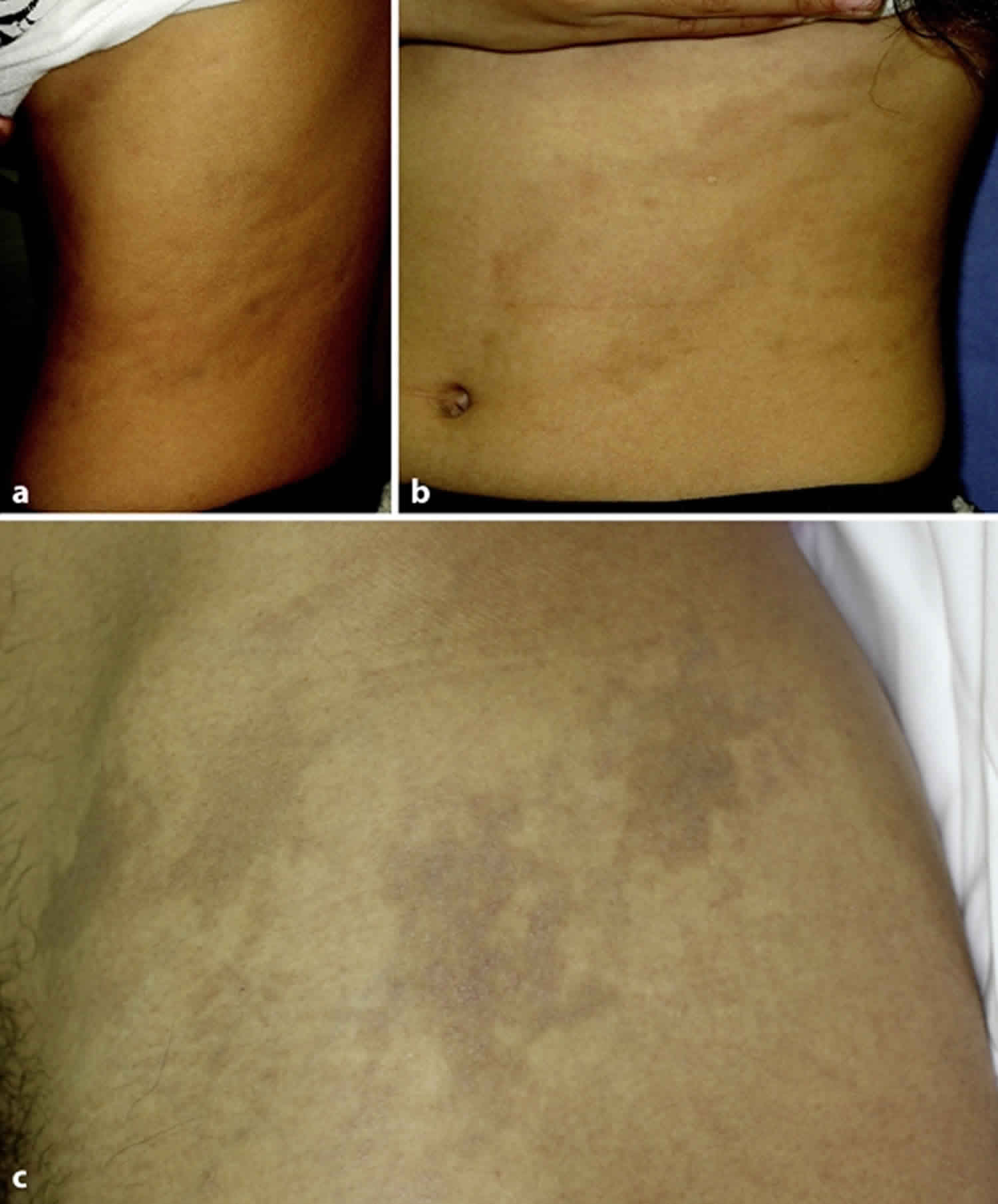
Ashy dermatosis
Ashy dermatosis also called erythema dyschromicum perstans, dermatosis cinecienta or erythema chronicum figuratum melanodermicum, is a form of acquired dermal macular hyperpigmentation characterized by well-circumscribed round to oval or irregular patches on the face, neck and trunk that are grey in color 1. Ashy dermatosis is a typically asymptomatic disease of unknown origin that causes gray spots to appear on the skin 2. Ashy dermatosis is an acquired, typically asymptomatic, disfiguring skin disease that occurs most commonly in Latin American (particularly Mexican) and Asian populations 3.
Patients with erythema dyschromicum perstans or ashy dermatosis have been called los cenicientos (the ash ones) due to the eruptions of oval, irregular or polycyclic, gray macules with erythematous, indurated, inflammatory borders 1. With progression, the eruption develops a gray-blue color and loses the erythematous border, which is sometimes replaced with a hypopigmented periphery. Ashy dermatosis affects the trunk and extremities, and typically occurs symmetrically 3.
Erythema dyschromicum perstans most often affects darker-skinned patients, most frequently Latin Americans and Indians. It has also been reported in people of lighter skin color and various ethnicities.
Erythema dyschromicum perstans may occur at any age but it appears to be more frequent in young adults with the majority of patients are under 30 years old 3. Women are affected more often than men.
Histologic examination of the active stage of ashy dermatosis is reported to demonstrate lichenoid dermatitis with vacuolization of the basal cell layer, occasionally colloid bodies, and increased epidermal melanin 1. The dermal changes are reported to be edema of the papillary dermis, a moderate or mild lymphohistiocytic infiltrate, and dermal melanophages. In the inactive stage of ashy dermatosis, there is no vacuolization of the basal cell layer, and a diminished dermal infiltrate 1. In addition, it was reported that patients of ashy dermatosis show idiopathic eruptive hyperpigmented macules, irrespective of the presence or absence of interface dermatitis histologically at the time of examination 4.
Figure 1. Ashy dermatosis
Ashy dermatosis causes
The exact cause for ashy dermatosis or erythema dyschromicum perstans remains unidentified. It is often classified as a variant of lichen planus pigmentosus because of its histopathological features. Melanin complexes in the dermis and epidermis are responsible for the ashen-gray color that occurs in sun-exposed and sun-protected areas 5. Over the years, theories have included:
- Genetic susceptibility
- Contact allergy to cosmetics and hair dye
- Toxic effects of chemicals such as ammonium nitrate or barium sulphate
- Whipworm infestation
- Viral infections
- An adverse effect of drugs and medications.
Ashy dermatosis symptoms
Ashy dermatosis is a chronic skin condition characterized by asymptomatic, slate-gray or violaceous hyperpigmented macules distributed most commonly over the trunk and proximal extremities, and less frequently over the face and neck. Lesions, which occur in otherwise healthy persons, may initially present as erythematous macules that slowly progress to a blue-gray hue. The macules of erythema dyschromicum perstans vary in size and may occasionally demonstrate an erythematous raised border 6.
Ashy dermatosis clinical features 7:
- The pigmented patches may be symmetrical in distribution or unilateral.
- Early lesions may be reddish in color, often with a more pronounced border, and they may be somewhat elevated. This phase is not always observed.
- The patient is otherwise well with no associated disease or blood test abnormality.
Ashy dermatosis diagnosis
It is important to obtain a thorough general health and medication history, perform an oral and genital examination, and obtain a punch biopsy at the border of the lesion to rule out other possible causes of hyperpigmentation. Several authors speculate that erythema dyschromicum perstans may be a variant of lichen planus, and the sequela of resolving lichen planus may cause hyperpigmented lesions. Thus, the patient should be examined for the characteristic lacy white patterned and erosive lesions of the oral and genital mucosa to rule out lichen planus. Review of medications may indicate a drug hypersensitivity reaction, particularly a fixed drug eruption, as a cause of hyperpigmented macules. Certain drugs, such as chlorpromazine, amiodarone, thiazides, and tetracyclines are the most common culprits. A general health history can help distinguish diffuse hyperpigmentation caused by internal disease entities, such as Addison’s disease and hemochromatosis. A punch biopsy at the border of the lesion is necessary to rule out melanosis secondary to malignant melanoma that manifests as a generalized blue-gray skin discoloration. Finally, melasma, which presents in sun-exposed areas, particularly the face, and postinflammatory hyperpigmentation, which occurs after inflammatory dermatoses, are other benign causes of hyperpigmented lesions 8.
In some cases, the clinical picture of ashy dermatosis or erythema dyschromicum perstans may be classical enough to diagnose the condition. A skin biopsy may reveal minor vacuolar degeneration of the basal layer in early lesions, and pigmentary incontinence with dermal melanophages in more established patches.
Ashy dermatosis differential diagnosis
Several other skin conditions may appear similar to erythema dyschromicum perstans because they also result in discolored skin patches.
- Acquired dermal macular hyperpigmentation
- Lichen planus pigmentosus
- Multiple lesions of fixed drug eruption
- Drug-induced skin pigmentation
- Postinflammatory hyperpigmentation
- Urticaria pigmentosa
- Incontinentia pigmenti
- Pinta
- Leprosy
Ashy dermatosis treatment
Erythema dyschromicum perstans or ashy dermatosis is rather resistant to currently available treatments. It may persist unchanged for years although some cases eventually clear up by themselves.
Treatments that may help improve the appearance of erythema dyschromicum perstans include:
- Topical steroids
- Exposure to ultraviolet radiation
- Pigment lasers, such as Q-switched ruby laser
- Chemical peels.
The most successful systemic treatment has been clofazimine (an antileprosy drug). Clofazimine, an antileprosy drug, has recently been studied in six patients who demonstrated marked improvement with treatment 9. Dapsone, griseofulvin, hydroxychloroquine, isoniazid and corticosteroids have been used successfully in a few cases.
References- Lapeere H, Boone B, Schepper SD, Verhaeghe E, Ongenae K, Geel NV, Lambert J, Brochez L, Naeyaert JM. Erythema dyschromicum perstans. In: Wolff K, Goldsmith L, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. vol 1. New York: McGraw-Hill; 2008. p. 640.
- Imanishi H, Tsuruta D, Kobayashi H, Ishii M, Nakagawa K. Two cases of unilateral ashy dermatosis. Case Rep Dermatol. 2011;3(1):1–4. doi:10.1159/000323663 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3155693
- Mckee PH, Calonje E, Granter SR. Erythema dyschromicum perstans. In: Mckee PH, Calonje E, Granter SR, editors. Pathology of the Skin with Clinical Correlations. vol 1. London: Elsevier Mosby; 2005. pp. 234–236.
- Zaynoun S, Rubeiz N, Kibbi AG. Ashy dermatoses – a critical review of the literature and a proposed simplified clinical classification. Int J Dermatol. 2008;47:542–544.
- Mosher TB, Fitzpatrick TB. Hypomelanoses and hypermelanoses. In: Freedberg IM, ed. Fitzpatrick’s Dermatology in general medicine. 5th ed. New York: McGraw-Hill, 1999:996–1009.
- Pandya AG, Guevara IL. Disorders of hyperpigmentation Dermatol Clin. 2000;18:91–8
- Erythema dyschromicum perstans. https://www.dermnetnz.org/topics/erythema-dyschromicum-perstans
- Ashy Dermatosis. Am Fam Physician. 2003 Aug 1;68(3):529-530. https://www.aafp.org/afp/2003/0801/p529.html
- Baranda L, Torres-Alvarez B, Cortes-Franco R, Moncada B, Portales-Perez DP, Gonzalez-Amaro R. Involvement of cell adhesion and activation molecules in the pathogenesis of erythema dyschromicum perstans (ashy dermatitis). The effect of clofazimine therapy Arch Dermatol. 1997;133:325–9