Balsalazide
Balsalazide disodium 750 mg is used to treat ulcerative colitis (a condition which causes swelling and sores in the lining of the colon [large intestine] and rectum). Balsalazide is an anti-inflammatory medication that belongs to the drug class 5-aminosalicylates. Balsalazide is converted in your body to mesalamine (5-aminosalicylic acid; 5-ASA) and works by reducing bowel inflammation, diarrhea, rectal bleeding, and stomach pain. Balsalazide capsules are used to treat active ulcerative colitis in patients 5 years of age and older. Balsalazide tablets are used to treat mild to moderately active ulcerative colitis in male patients 18 years of age and older.
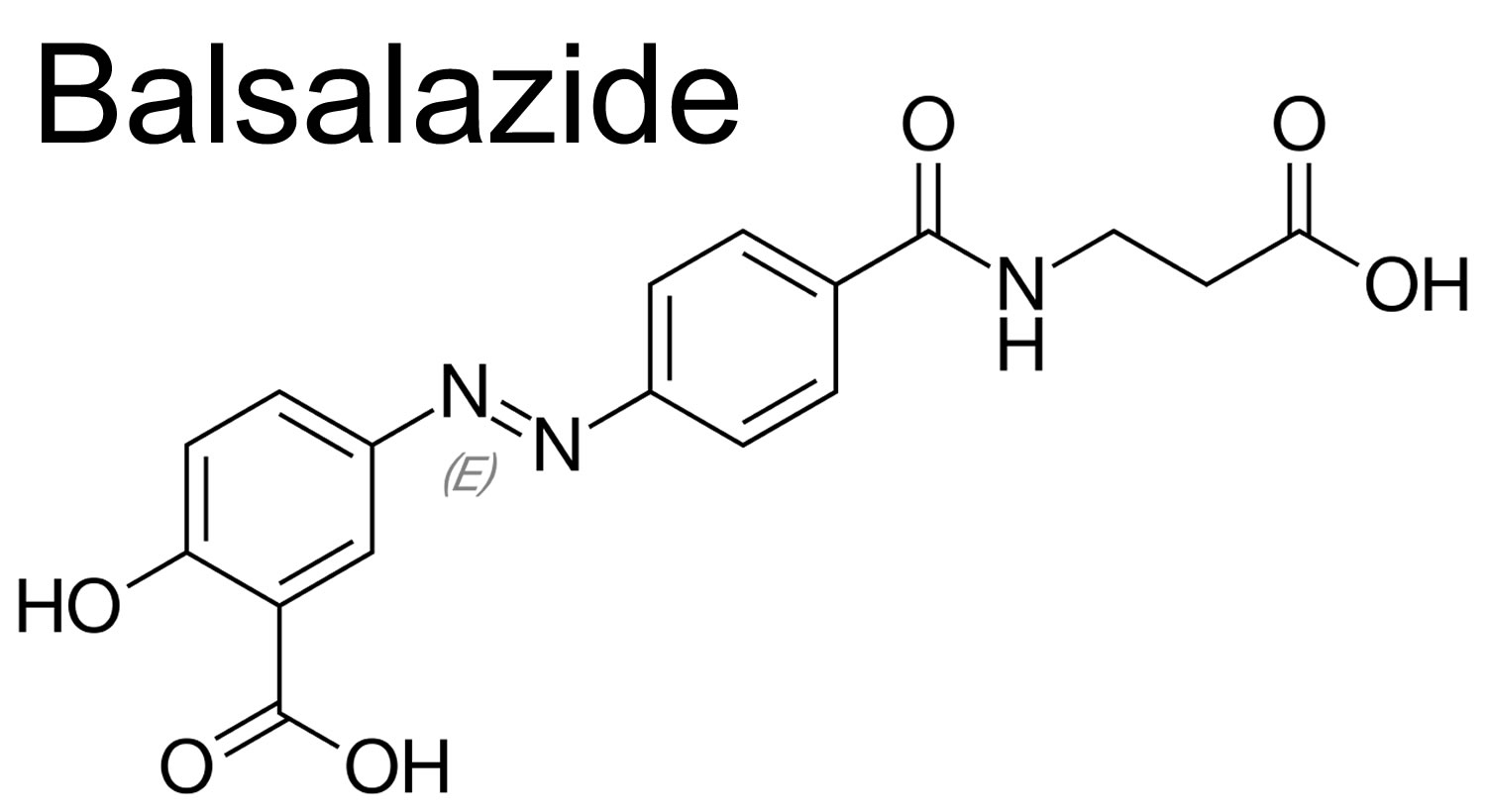
The chemical classification of balsalazide is aminosalicylic acids. Balsalazide is a pro-drug of mesalamine that consists of 5-aminosalicylate with an azo bond to a phenyl-hydroxybenzoid acid moiety which is cleaved off in the large intestine by bacterial enzymes, releasing free mesalamine.
Balsalazide was approved as treatment of mildly to moderately active ulcerative colitis in adults in the United States in 2000 and is available generically and under the brand name Colazal in capsules of 750 mg; the usual dosage being 2.25 to 6.75 g daily in three divided doses.
Balsalazide medication is available only with your doctor’s prescription.
Balsalazide medication is usually taken three times a day. You may take balsalazide with or without food. Also, tell your doctor if you are on a low-sodium diet. If you cannot swallow the capsule, you may open it and pour balsalazide into a small amount of applesauce. Stir this mixture well and swallow right away. Do not keep the mixture for future use.
Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take balsalazide exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Balsalazide is usually taken for 8 weeks, but it may be taken for up to 12 weeks. Continue to take balsalazide even if you feel well. Do not stop taking balsalazide without talking to your doctor.
It is important that your doctor check your progress at regular visits. This will allow your doctor to see if this medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for any unwanted effects.
Check with your doctor right away if you have abdominal or stomach pain, bloody diarrhea, cramps, fever, headache, or a rash while you are using this medicine. These may be symptoms of a condition called mesalamine-induced acute intolerance syndrome.
If your symptoms do not improve or if they become worse, check with your doctor.
Balsalazide special precautions
Before taking balsalazide:
- tell your doctor and pharmacist if you are allergic to balsalazide, aspirin, choline magnesium trisalicylate (Tricosal, Trilisate), choline salicylate (Arthropan), diflunisal (Dolobid), magnesium salicylate (Nuprin Backache, Mobidin, Extra Strength Doan’s, others), mesalamine (Asacol, Pentasa, Rowasa), salsalate (Argesic-AS, Disalcid, others), sodium salicylate, sodium thiosalicylate (Rexolate), sulfasalzine (Azulfidine), or any other drugs.
- tell your doctor and pharmacist what prescription and nonprescription medications you are taking, especially oral antibiotics and vitamins and herbal products.
- tell your doctor if you have or have ever had liver or kidney disease or pyloric stenosis (a condition in which the stomach empties slowly).
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking balsalazide, call your doctor.
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Children
Appropriate studies have not been performed on the relationship of age to the effects of balsalazide capsules in children younger than 5 years of age. Safety and efficacy have not been established.
Appropriate studies have not been performed on the relationship of age to the effects of balsalazide tablets in the pediatric population. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of balsalazide in the elderly. However, elderly patients are more likely to have blood problems (e.g., neutropenia, pancytopenia) and age-related kidney disease, which may require caution and an adjustment in the dose for patients receiving balsalazide.
Breastfeeding
Although no information exists on the excretion of balsalazide into breastmilk, it is metabolized to the active drug mesalamine. A few cases of diarrhea have been reported in infants exposed to mesalamine, although the rate is not high. Most experts consider mesalamine derivatives to be safe during breastfeeding 1. If balsalazide is required by the mother, it is not a reason to discontinue breastfeeding, but observe breastfed infants for diarrhea.
Other medical problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
Allergy to aminosalicylates or salicylates (e.g., aspirin)—Should not be used in patients with this condition.
Kidney disease, or history of or
Liver disease——Use with caution. May make this condition worse.
Pyloric stenosis (tube is too narrow where food passes out of the stomach )—May delay the release of balsalazide into the body.
Balsalazide interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking balsalazide, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this balsalazide with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aceclofenac
- Acemetacin
- Amtolmetin Guacil
- Bismuth Subsalicylate
- Bromfenac
- Bufexamac
- Celecoxib
- Choline Magnesium Trisalicylate
- Choline Salicylate
- Clonixin
- Dexibuprofen
- Dexketoprofen
- Diflunisal
- Dipyrone
- Droxicam
- Etodolac
- Etofenamate
- Etoricoxib
- Felbinac
- Fenoprofen
- Fepradinol
- Feprazone
- Floctafenine
- Flufenamic Acid
- Flurbiprofen
- Ibuprofen
- Ketoprofen
- Lornoxicam
- Loxoprofen
- Lumiracoxib
- Magnesium Salicylate
- Meclofenamate
- Mefenamic Acid
- Meloxicam
- Mesalamine
- Morniflumate
- Nabumetone
- Naproxen
- Nepafenac
- Niflumic Acid
- Nimesulide
- Nimesulide Beta Cyclodextrin
- Olsalazine
- Oxaprozin
- Oxyphenbutazone
- Parecoxib
- Phenylbutazone
- Phenyl Salicylate
- Piketoprofen
- Piroxicam
- Proglumetacin
- Propyphenazone
- Proquazone
- Rofecoxib
- Salicylamide
- Salicylic Acid
- Salsalate
- Sodium Salicylate
- Sulfasalazine
- Sulindac
- Tenoxicam
- Tiaprofenic Acid
- Tolfenamic Acid
- Tolmetin
- Trolamine Salicylate
- Valdecoxib
Using balsalazide with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Tamarind
- Warfarin
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your balsalazide with food, alcohol, or tobacco.
Balsalazide dosage
Balsalazide comes as a 750 mg capsule or tablets to be taken by mouth. The dose of balsalazide will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of balsalazide. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of balsalazide that you take depends on the strength of the balsalazide. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take balsalazide depend on the medical problem for which you are using balsalazide.
For treatment of ulcerative colitis:
- For oral dosage form (capsules):
- Adults—Three 750-milligram (mg) capsules three times a day, for a total daily dose of 6750 mg for 8 weeks. You may need to take balsalazide for up to 12 weeks as ordered by your doctor.
- Children 5 years of age and older—Three 750-mg balsalazide capsules three times a day for a total daily dose of 6750 mg for 8 weeks or one 750-mg balsalazide capsule three times a day for a total daily dose of 2250 mg for 8 weeks.
- Children younger than 5 years of age—Use and dose must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—Three 1.1-gram (g) tablets two times a day, for a total daily dose of 6.6 g, taken for up to 8 weeks.
- Children—Use and dose must be determined by your doctor.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Balsalazide side effects
Side effects from balsalazide can occur. Tell your doctor if any of these symptoms are severe or do not go away:
- headache
- abdominal pain
- upset stomach
- diarrhea
- vomiting
- joint pain
- difficulty falling or staying asleep
- tiredness
- gas
- runny nose
- muscle or back pain
- coughing
- loss of appetite
- urinary tract infection
- constipation
- dry mouth
Check with your doctor immediately if any of the following side effects occur:
- yellowing of the skin or eyes
- bloody diarrhea
- dark urine
- bloating or swelling of the stomach
- increased diarrhea
- rectal bleeding
- fever, sore throat, or flu-like symptoms
- skin rash
Less common
- bladder pain
- bloody or cloudy urine
- bloody stools
- difficult, burning, or painful urination
- frequent urge to urinate
- heavy bleeding
- lower back or side pain
Rare
- difficult or labored breathing
- shortness of breath
- tightness in the chest
- wheezing
Incidence not known
- abdominal or stomach pain or tenderness
- chills
- clay colored stools
- dark urine
- decreased appetite
- decreased frequency or amount of urine
- dizziness
- general feeling of tiredness or weakness
- headache
- increased blood pressure
- increased thirst
- itching
- joint pain
- light-colored stools
- loss of appetite
- nausea and vomiting
- stomach pain, continuing
- swelling of the face, fingers, feet, or lower legs
- unpleasant breath odor
- unusual tiredness or weakness
- vomiting of blood
- weight gain
- yellow eyes or skin
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- diarrhea
- mild headache
- muscle aches
- sore throat
- stuffy or runny nose
Less common
- acid or sour stomach
- belching
- bloated or full feeling
- body aches or pain
- bone pain
- congestion
- constipation
- coughing
- cramps
- difficulty with moving
- dry mouth
- dryness of the throat
- excess air or gas in the stomach or intestines
- general feeling of discomfort or illness
- heartburn
- hoarseness
- indigestion
- muscle pain or stiffness
- pale skin
- passing of gas
- shivering
- sleeplessness
- sneezing
- stomach discomfort or upset
- sweating
- swelling or inflammation of the mouth
- swollen joints
- tender, swollen glands in the neck
- trouble with sleeping
- trouble with swallowing
- troubled breathing with exertion
- unable to sleep
- unusual bleeding or bruising
- voice changes
- weight loss
Rare
- back pain
- ear congestion
- loss of appetite
- loss of voice
- pain in the ankles or knees
- painful, red lumps under the skin, mostly on the legs
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
Incidence not known
- Hair loss or thinning of the hair
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
References