Basilar artery
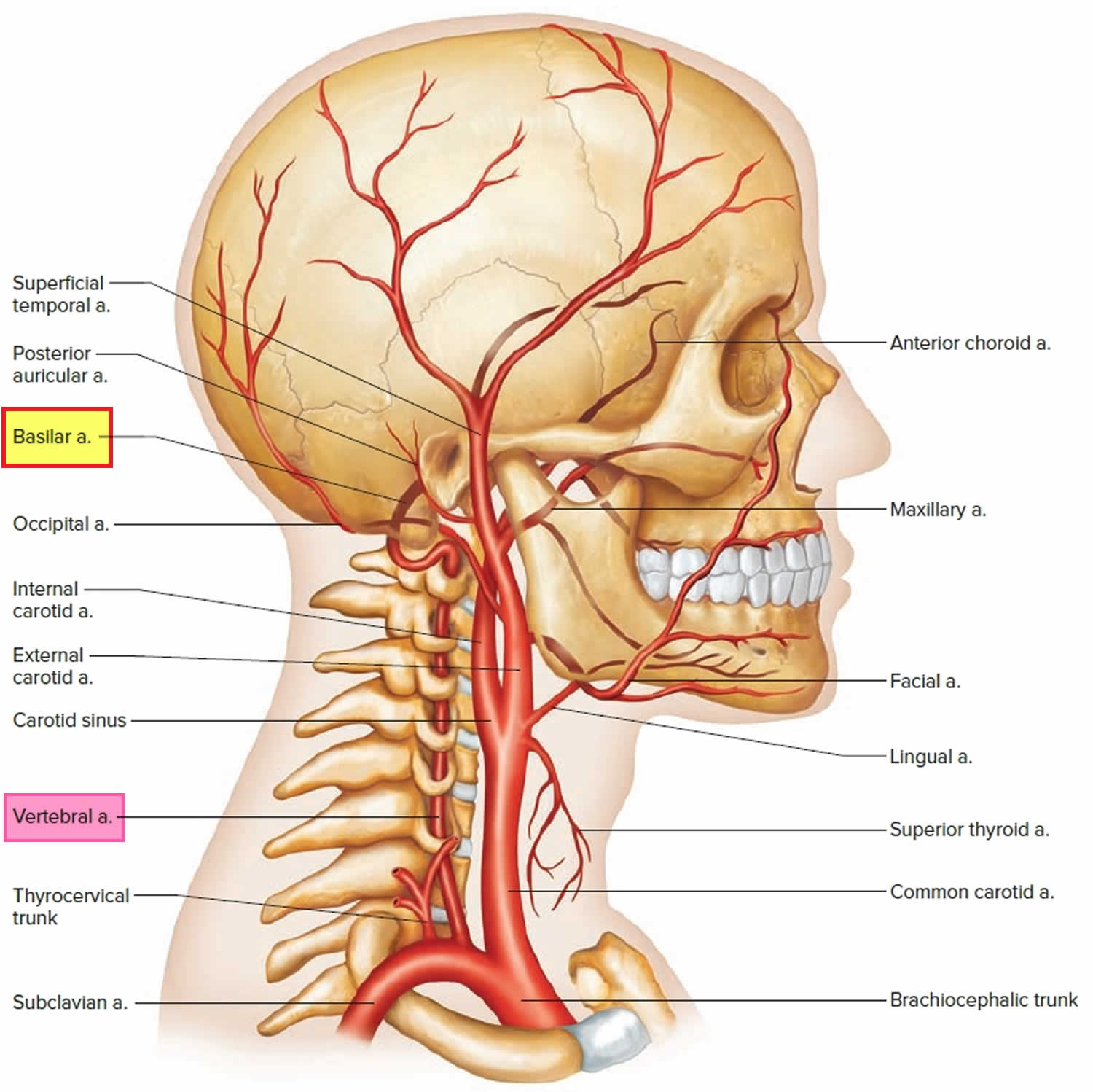
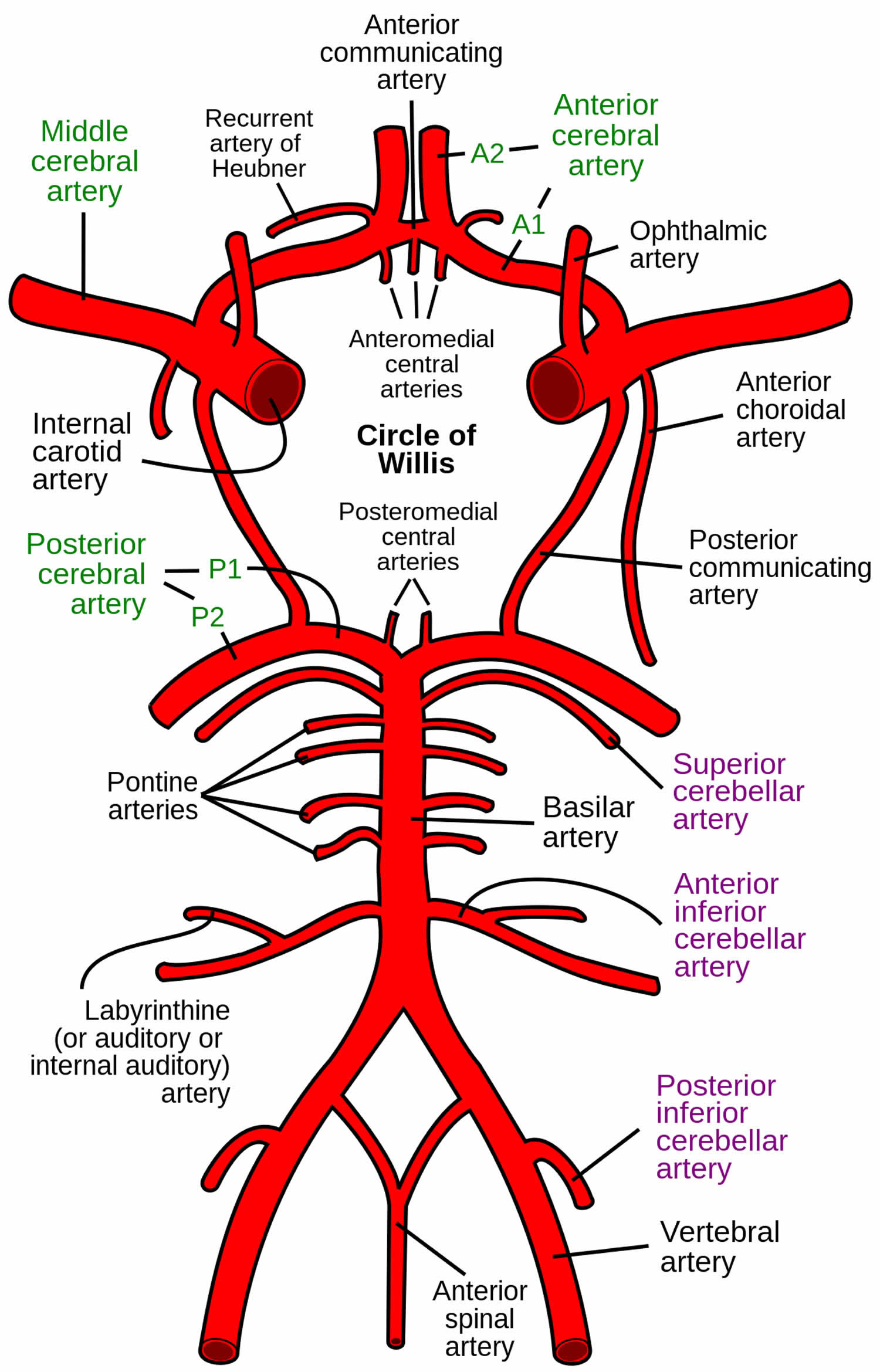
The basilar artery is the union of two vertebral arteries at the front of the brainstem. The basilar artery runs cranially in the central groove of the pons towards the midbrain within the pontine cistern. The basilar artery travels within this groove from the lower pontine border adjacent to the exit of the abducens nerve (CN VI) to the upper pontine border and the appearance of the oculomotor nerve (CN III). The basilar artery gives rise to the posterior cerebral and cerebellar arteries branches that supply the pons, midbrain, cerebellum and inner ear. At the pons–midbrain junction, the basilar artery ends by dividing into two posterior cerebral arteries that supply parts of the occipital and temporal lobes of the cerebrum. Before terminating at the upper pontine border where the basilar artery divides into the two posterior cerebral arteries, basilar artery provides several paired branches:
- Anterior inferior cerebellar artery (AICA). Anterior inferior cerebellar arteries supply the inferolateral pons, anteroinferior cerebellum, and the middle cerebellar peduncle
- Labyrinthine artery (variable origin; more commonly a branch of anterior inferior cerebellar artery)
- Pontine arteries. The pontine arteries are a number of small arteries which come off at right angles from either side of the basilar artery and supply the pons and adjacent parts of the brain. The pontine arteries include the paramedian arteries, the short circumferential, and the long circumferential arteries.
- Superior cerebellar artery (SCA). Superior cerebellar arteries supply the superior cerebellum and parts of the midbrain
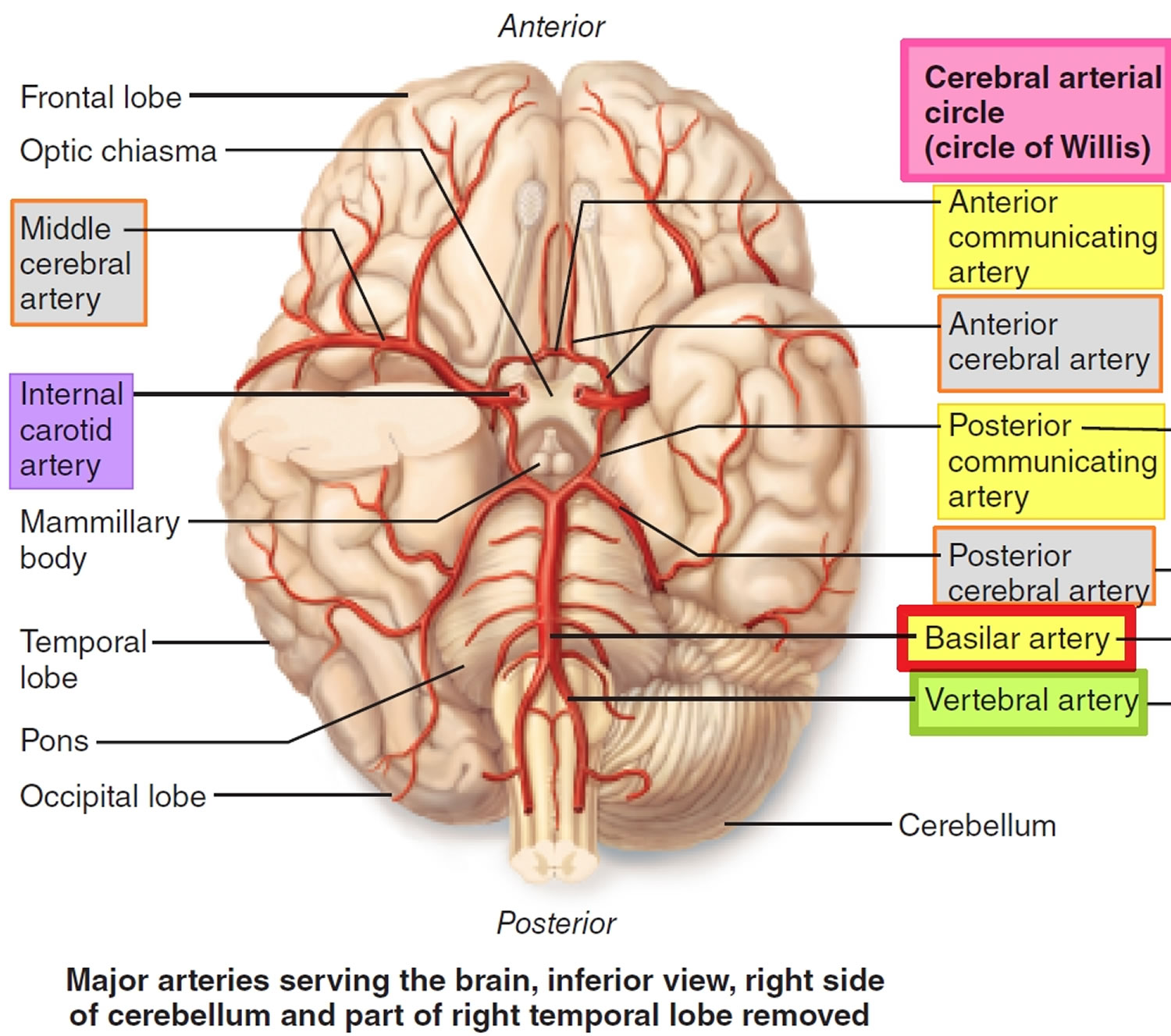
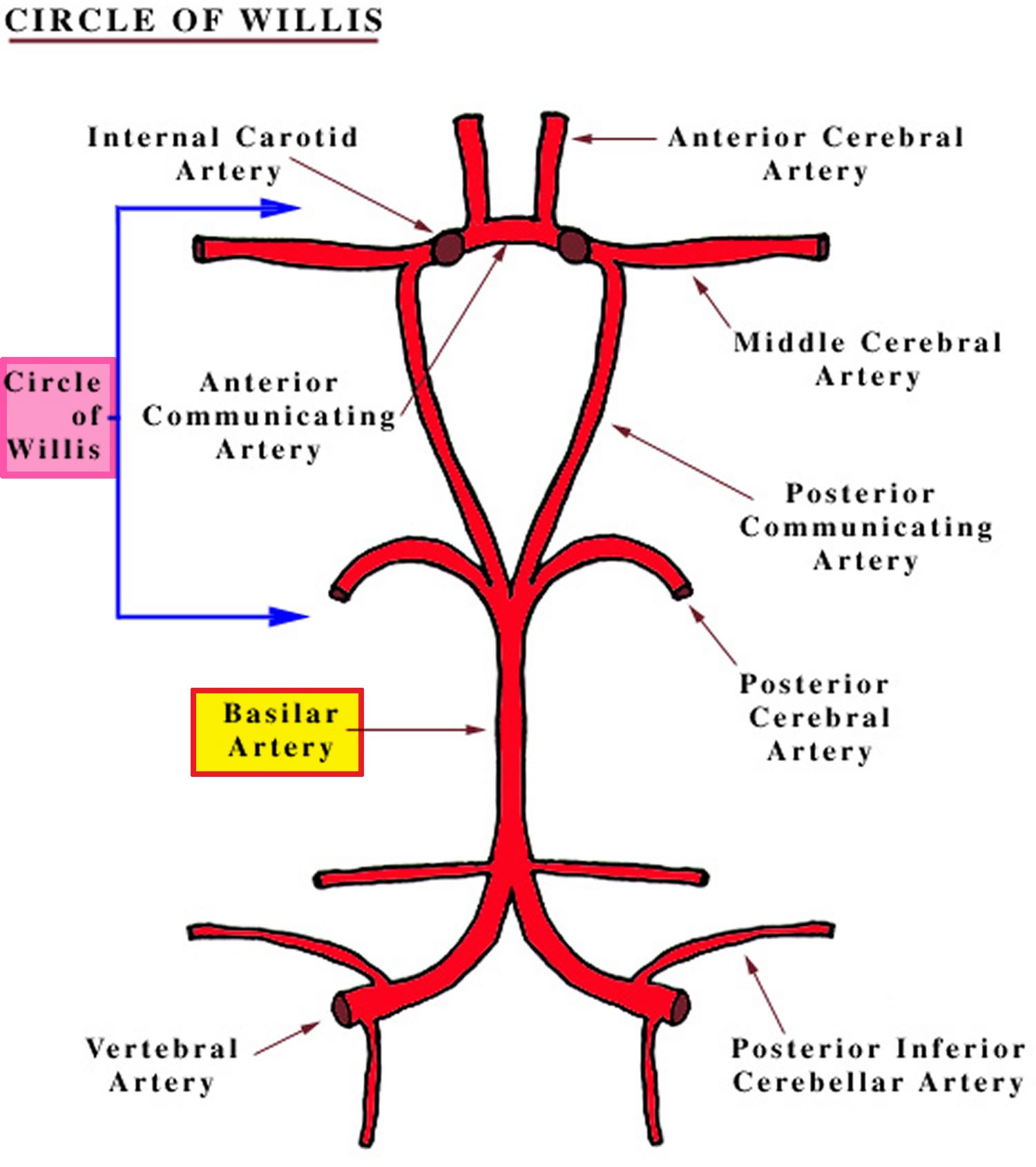
The posterior cerebral arteries also help form the cerebral arterial circle (circle of Willis) that surrounds the pituitary gland and optic chiasm, which connects the basilar artery and internal carotid artery systems. The cerebral arterial circle (circle of Willis) provides alternate pathways for blood to circumvent blockages and reach brain tissues. It also equalizes blood pressure in the brain’s blood supply. From the circle of Willis, other arteries — the anterior cerebral artery (ACA), the middle cerebral artery (MCA), and the posterior cerebral artery (PCA) — arise and travel to all parts of the brain. Brain aneurysms tend to occur at the junctions between the arteries that make up the Circle of Willis.
Most people have abnormalities or anomalies in their Circle of Willis and 18–32% have one hypoplastic and 24–49% have bilateral hypoplastic posterior communicating arteries; only 20% have a complete cerebral arterial circle (circle of Willis) 1. Knowledge of the distribution of the arteries arising from the cerebral arterial circle (circle of Willis) is crucial for understanding the effects of blood clots, aneurysms, and strokes on brain function.
Figure 1. Basilar artery and basilar artery branches
Figure 2. Cerebral arterial circle (circle of Willis)
Basilar artery stroke
Basilar artery occlusion (BAO) is a rare but devastating form of stroke with high disability or death rates approaching 70%-95% 2, 3. Acute basilar artery occlusion (BAO) represents 1-4% of all ischemic strokes and 5% of large vessel occlusion strokes 4, 5. The clinical presentation of basilar artery occlusion is often extremely nonspecific and hence diagnosis may be delayed 6. Basilar artery occlusion can cause many symptoms such as dizziness, blurring of vision, isolated cranial nerve palsies or hemiplegia, but also a locked-in syndrome or coma 7, 8. Successful treatment of acute ischemic stroke is incumbent on rapid recanalization of the occluded vascular territory, whether this is achieved via intravenous thrombolysis, intra-arterial thrombolysis or mechanical thrombectomy 9.
One of the most devastating locations for a basilar artery occlusion is a mid-basilar occlusion with bilateral pontine ischemia. These patients may appear to be comatose but can be fully conscious and paralyzed with only limited vertical eye movements. This “locked-in syndrome” has a high mortality rate of approximately 75% in the acute phase 10. Another basilar artery occlusion syndrome involves occlusion at the distal top of the basilar artery where the superior cerebellar arteries (SCAs) and posterior cerebral arteries (PCAs) represent the final terminal branches. This “top of the basilar” syndrome may cause ischemia of the midbrain, thalami, inferior temporal lobes, and occipital lobes. Occlusion of paramedian perforator branches, which originate from the distal basilar artery, results in midbrain and thalamic ischemia. Examination findings may include vertical gaze and convergence disorders, slowed smooth pursuit movements, skew deviation, see-saw, and convergence-retraction nystagmus 11. Pupillary light reflex is often affected such that pupils react to light slowly and incompletely or not at all. If superior cerebellar arteries (SCAs) are involved, then dizziness, vomiting, dysarthria, ipsilateral or bilateral dysmetria, and gait ataxia may be observed with ischemia of the superior cerebellum. An embolus to one posterior cerebral artery can result in contralateral vision loss, whereby infarction of both posterior cerebral artery territories can cause cortical blindness, disorientation, and inability to form new memories.
Infarction of the middle midbrain can result in nuclear third nerve palsy or fascicular third nerve palsy, which can be associated with crossed hemiplegia, ipsilateral, or contralateral hemiataxia. An infarct in the lower midbrain can cause internuclear ophthalmoplegia, fourth nerve palsy, and bilateral ataxia. Long anteromedial perforators arise from the mid-basilar portion of the artery. Occlusion of the mid-basilar artery that supply the pons and lower midbrain can also result in prominent eye findings including primary-position, down-beating nystagmus, ipsilateral gaze paralysis (ipsilateral or complete), and internuclear ophthalmoplegia (both unilateral and bilateral) 12.
Infarcts in the paramedian pons cause pure unilateral motor strokes with or without incoordination (ataxic hemiparesis). Ocular bobbing can be seen in pontine strokes. Less common are lateral pontine syndromes like Gasperinin syndrome, which comprises abducens palsy plus complete anterior inferior cerebellar artery syndrome 12.
The frequency, incidence, and prevalence of basilar artery occlusion (BAO) are not well known in the medical literature. 20% of cerebral blood flow goes through the posterior circulation (vertebrobasilar system), that is why vertebral basilar circulation occlusions represent 20–40% of all the strokes in a year 13, 14. Basilar artery occlusion has been reported in 2 out of 1000 post-mortem cases. Basilar artery thrombosis may explain as many as 27% of ischemic strokes occurring in the posterior circulation. Symptomatic atherosclerotic vertebrobasilar occlusive disease is associated with a high risk of recurrent stroke despite medical therapy, occurring in 10% to 15% of the patients within 2 years 15, 16, 17. An increased prevalence exists in males, with a 2:1 ratio. Occlusion due to atherosclerotic disease is most prevalent in patients of advanced age, usually in the sixth and seventh decades of life. Distal basilar artery occlusion is usually secondary to embolism and is most prevalent in the fourth decade of life 18.
Basilar artery stroke symptoms
Most commonly, patients experiencing basilar artery occlusion exhibit acute neurologic signs including motor deficits, hemiparesis or quadriparesis, and facial palsies, dizziness, headache, and speech abnormalities–especially dysarthria and difficulty articulating words 19. Patients may also complain of nausea, vomiting, and changes in vision. An altered level of consciousness is commonly present. Other misleading presentations of acute basilar artery occlusion include either unilateral or bilateral shaking, twitching, jerking, or posturing which can potentially be mistaken for epileptic events 20.
Basilar artery thrombosis may present in three general constellations:
- Rapid onset of advanced motor and bulbar symptoms with a decreased level of consciousness.
- Insidious or stuttering symptoms over a few days as a combination of the above that end with disabling motor and bulbar symptoms, a decreased level of consciousness, or both.
- Prodromal symptoms may include headache, neck pain, loss of vision, binocular diplopia, dysarthria, dizziness, hemiparesis, paresthesias, ataxia, and tonic-clonic type movements. “Herald hemiparesis” is the phrase to describe the momentary, unilateral weakness that may precede later permanent symptoms.
An abnormal level of consciousness and focal motor weakness are the hallmark symptoms manifested in the majority of patients. Pupillary abnormalities, oculomotor signs, and pseudobulbar manifestations (facial palsy, dysphonia, dysarthria, dysphagia) are seen in more than 40% of patients 21, 8. Variable degrees of hemiparesis or quadriparesis are part of the clinical picture. As basilar artery thrombosis presents in various ways it is very important to have high clinical suspicion to detect basilar artery thrombosis.
Basilar artery stroke complications
Basilar artery stroke complications can include the following: aspiration, aspiration pneumonia, thromboembolic disease (deep vein thrombosis and pulmonary embolism), myocardial infarction, and recurrent stroke. Patients with advanced functional debility secondary to stroke are increasingly prone to contractures, pressure ulcers, and sepsis. Many patients who survive basilar artery thrombosis require ongoing physical and occupational therapy to regain and maintain functionality 22, 23.
Basilar artery stroke causes
The cause of basilar artery stroke can occur from thromboembolism, atherosclerotic disease, or vascular dissection 19. The mechanism differs depending on the affected segment. Atherosclerotic disease more commonly affects the mid-portion of the basilar artery, followed by the vertebrobasilar junction 19. Lodging of an embolic source is much more frequent in the distal third of the basilar artery especially at the top of the basilar artery and the vertebrobasilar junction 19. Arterial dissection is more common in the extracranial vertebral artery and has been associated with neck injuries and cervical chiropractic adjustments. Intracranial dissections are exceedingly rare 6.
Intrinsic atherosclerotic basilar artery stenosis is the most common cause and occurs most often in the sixth and seventh decade of life. The basilar artery occlusion secondary to embolism from the heart or vertebral arteries is another significant cause. Patients with embolic etiology are younger than those with atherosclerotic disease 24.
The most common risk factor for basilar artery stroke is hypertension which is found in as many as 70% of cases 19. Other risk factors include diabetes mellitus, coronary artery disease, peripheral vascular disease, cigarette smoking, and hyperlipidemia.
Dissection of a vertebral artery can either expand directly into the wall of the basilar artery resulting in low-flow or no-flow state, or cause formation of a thrombus that can embolize distally. Traumatic vertebral artery dissection is one of the most common causes of acute basilar artery occlusion in young patients and should be suspected in patients presenting with cervical pain with or without headache and neurological deterioration 25. Rarer causes which are more specific to the posterior circulation include cervical spine or skull base fracture, cervical instability 26, arteritis, meningitis, aneurysms, hereditary arteriopathies, and neurosyphilis 27. Behcet vasculitis more commonly involves the posterior circulation 28.
Basilar artery stroke diagnosis
Doctors also need to rule out other possible causes of your symptoms, such as a brain tumor or a drug reaction.
Some of the tests you may have include:
- A physical exam. Your doctor will do a number of tests you’re familiar with, such as listening to the heart and checking the blood pressure. You’ll also have a neurological exam to see how a potential stroke is affecting your nervous system.
- Blood tests. You may have several blood tests, including tests to check how fast the blood clots, whether the blood sugar is too high or low, and whether you have an infection.
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed image of your brain. A CT scan can show bleeding in the brain, an ischemic stroke, a tumor or other conditions. Doctors may inject a dye into your bloodstream to view the blood vessels in the neck and brain in greater detail (computerized tomography angiography [CTA]).
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and a magnetic field to create a detailed view of the brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiography [MRA]).
- Carotid ultrasound. In this test, sound waves create detailed images of the inside of the carotid arteries in the neck. This test shows buildup of fatty deposits (plaques) and blood flow in the carotid arteries.
- Cerebral angiogram. In this test, your doctor inserts a thin, flexible tube (catheter) through a small incision, usually in the groin, and guides it through the major arteries and into the carotid or vertebral artery. Then your doctor injects a dye into the blood vessels to make them visible under X-ray imaging. This procedure gives a detailed view of arteries in the brain and neck.
- Echocardiogram. An echocardiogram uses sound waves to create detailed images of the heart. An echocardiogram can find a source of clots in the heart that may have traveled from the heart to the brain and caused a stroke.
Computed tomography (CT) scanning is usually the first imaging study performed. CT may be effective at identifying larger areas of ischemic insult and can highlight hemorrhagic pathology. A hyperdense basilar artery may be present on the CT scan. However, CT scanning has a low sensitivity for early ischemia and is less effective at evaluating the brainstem, cerebellum, and posterior circulation. Ultimately, one needs a high index of suspicion in the correct clinical context to diagnosis an easily missed disease. Additional evaluation with CT angiography may be considered, and a filling defect noted within the basilar artery. Catheter angiography is still a criterion for diagnosis; however, with the availability of noninvasive imaging modalities such as magnetic resonance imaging (MRI) and angiography (MRA), the role of angiography has changed. MRI/MRA is more sensitive than CT scanning for identifying early ischemia and vascular occlusion 29. MRI is the best imaging modality for any posterior fossa lesion including acute ischemic infarction. Diffusion-weighted imaging (DWI) MRI sequence can show an acute brainstem or cerebellar infarct within seconds of the arterial occlusion. MR angiogram can show the site of vascular occlusion non-invasively. The presence of microhemorrhages in GRE-T2 or SWI imaging can help to indicate underlying hypertensive etiology.
Basilar artery stroke treatment
Acute occlusion of the basilar artery is potentially life-threatening. All patients should be admitted to a stroke unit when available. Recanalization of the basilar artery is key to the successful treatment of basilar artery thrombosis and to improving prognosis. This can be accomplished by intravenous thrombolysis (IVT), intra-arterial thrombolysis (IAT) or mechanical endovascular thrombectomy 30, 19. A noncontrast head CT and CT angiography (CTA) should be the next step in diagnostic testing. If the head CT shows no hemorrhage and symptom onset is within 4.5 hours, IV tissue-type plasminogen activator (t-PA) is standard of care. The high morbidity and mortality in patients with basilar artery occlusion who do not recanalize may lead to consideration of endovascular treatment to revascularize the basilar artery by intra-arterial thrombolysis or thrombectomy 7.
Recanalization occurs in more than half of basilar artery occlusion patients treated with intra-arterial treatment (IAT) or intravenous thrombolysis (IVT) 31, 32. Treatment is time-sensitive; the earlier the intervention, the better the functional outcomes. There is no good large-scale study to define the treatment window for basilar artery thrombosis. It is clearly much longer than the accepted window of 6 to 8 hours recommended for large vessel occlusion in anterior circulation infarct. The commonly accepted time window is at least 12 hours and potentially up to 24 hours. In some situations, if the patient is having symptoms and minimal stroke on the MRI brain it is reasonable to consider for mechanical endovascular thrombectomy up to 2-3 days. Subsequent therapy for secondary prevention focuses on treating the underlying causes and modifying risk factors 33, 34, 35, 36.
Basilar artery stroke prognosis
Overall outcomes can be expected to be poor in patients with basilar artery thrombosis. The patient mortality rate is greater than 85%, although it drops to as low as 40% in patients with recanalization 19. Successful recanalization appears to be the single most important predictor of a good outcome 37. The thrombolysis in cerebral infarction (TICI) score is a widely used method to describe angiographic findings after endovascular treatment of acute ischemic stroke. Although definitions vary within the literature, TICI 2b (>50% reperfusion of vascular territory according to the original TICI 38 and >67% of the vascular territory in the modified TICI 39 and TICI 3 (100% reperfusion) are generally regarded to represent a successful angiographic outcome. Lindsberg and Mattle 40 found that only 2% of patients who did not recanalize the basilar artery had good outcomes versus 38% who did. In the Helsinski Stroke Thrombolysis Registry, 14% of patients who did not recanalize had good outcomes compared to 86% who did recanalize 41. In a small case series of 6 consecutive basilar artery occlusion’s treated at a single institution, 5 of the 6 patients treated with endovascular treatment had a TICI score of 3 and the other had TICI 2b resultant recanalization, and all but 1 patient was independent with activities of daily living at 90 days 42. In lieu of randomized controlled trials, a recent meta-analysis by Kumar et al 37 showed that recanalization was associated with a 1.5-fold reduction in dependency and 2.0-fold reduction in mortality.
Predictors of recanalization include clot location and clot length. Top of the basilar clot location 41 and shorter thrombus length 43 have increased probability of recanalization. Strbian 43 reported that thrombi shorter than 100 mm had a 70% to 80% probability of recanalization. The probability of recanalization decreased in a clot length-dependent fashion, such that thrombi >30 mm long had only a 20% to 30% chance of opening with IV t-PA. In this study, patients with complete or partial recanalization had significantly less morbidity at 3 months and less mortality at 3 months and 1 year 43.
One can expect good functional outcomes in as few as 24 to 35% of patients treated with intravenous thrombolysis (IVT) or intra-arterial thrombolysis (IAT). For symptomatic patients who survive, the risk of recurrent stroke is 10 to 15% 23. The most important prognostic factors are the extent and duration of thrombosis. Therefore, a high index of suspicion of the diagnosis followed by expedited recanalization will give the patient the best hope of an improved outcome.
In the New England registry of posterior circulation strokes, a prospective, single institution registry, only 29% of patients died or were left with a major deficit 24. Outcomes were dependent on the etiology of the occlusion. Those patients with embolic etiology had a 2.4-fold higher risk of poor outcome compared with patients with diffuse or localized atherosclerosis 24. Overall, the mortality rate in their study was lower compared to previously reported findings of mortality rates of 45% to 86% 40, 44.
Basilar artery aneurysm
A brain aneurysm is a weak, bulging area in an artery in the brain, analogous to a thin balloon or a weak spot on a tire’s inner tube. Because its walls may be weak and thin, an aneurysm is at risk of rupturing. If an aneurysm ruptures, blood spills into the space between the skull and the brain. Most strokes are caused by loss of blood flow to a portion of the brain (called an ischemic stroke or cerebral infarction) or by injury related to bleeding within the brain tissue (an intracerebral hemorrhage) or into the space around the brain (the subarachnoid space) also known as subarachnoid hemorrhage (SAH). Basilar artery aneurysm is a rare vascular lesion than anterior circulation aneurysm and rupture less frequently, but basilar artery aneurysm can rupture and lead to severe subarachnoid hemorrhage (SAH) that tends to recur 45. A subarachnoid hemorrhage (SAH) is bleeding in the space between your brain and the surrounding membrane (subarachnoid space). Basilar artery aneurysms compromise about 5% of all intracranial aneurysms, and they are the most common aneurysms of the vertebrobasilar vascular system 46. Subarachnoid hemorrhage (SAH) as a result of ruptured intracranial artery aneurysm constitutes approximately 5% of the strokes 47. The hallmark of subarachnoid hemorrhage (SAH) is a sudden, severe headache described as “the worst headache of my life,” which is referred to occur in approximately 80% of patients 48. The headache is sometimes associated with nausea, vomiting and a brief loss of consciousness. Noncontrast head computed tomography (CT) remains the gold standard of diagnosis of subarachnoid hemorrhage (SAH) 49. However, in the suspected ruptured aneurysm, the patient should undergo computed tomography angiography of the brain, due to its high accuracy and increased sensitivity in diagnosing cerebral aneurysms 50.
Both unruptured and ruptured basilar artery aneurysms can be considered for microsurgical clipping or endovascular stenting of the aneurysm. Direct surgery for basilar artery aneurysm is complicated because the aneurysms are close to the critical structures of the brain stem, cranial nerves, and the perforators that supply blood to them, and the approach requires complex skull base procedures 51. Due to lower rates of disability and death, the first-line management is usually an endovascular treatment 52. In particular, treatment by stent-assisted coil embolization is often chosen because of the shape of the aneurysm. Stent-assisted coil embolization procedure’s post-treatment complete occlusion rate for basilar artery aneurysms is high, with reports of 83.3–85% 53, 54. On the other hand, the complication rate associated with this procedure was relatively high, with reports of morbidity and mortality of 7.8% 55. There have been reports of cases of subarachnoid hemorrhage (SAH) due to rupture in the early postoperative period, and the recurrence rate is relatively high. Thus, caution should be paid in its indication 56.
Flow diversion for fusiform basilar artery aneurysms has become a promising treatment option. Initial reports with flow diversion for fusiform basilar artery aneurysms were mixed with poor outcomes 51. But the flow diversion treatment has been recently reported to have a good result with long-term aneurysm occlusion rate in many patients when flow diversion is used in carefully selected patients 57, 58. On the other hand, there are reports of acute occlusion of the basilar artery and brain stem perforator occlusion after flow diversion treatment 59, 60. These cause significant postoperative death and disability. Since hypercoagulable state occurs in the acute phase of subarachnoid hemorrhage (SAH), these ischemic complications are likely to occur. Thus, the indication of flow diversion for ruptured fusiform basilar artery aneurysms should be restricted to otherwise untreatable lesions 59.
Direct surgery for giant fusiform basilar artery aneurysms is still challenging today. Due to the aneurysm’s shape, direct clipping is usually tricky, and parent artery occlusion following bypass surgery is often selected 61, 62. According to a review by Sughrue et al. 61, direct surgery for giant aneurysms has a higher complete occlusion rate and lower retreatment and rebleeding rated than endovascular treatment but has relatively high morbidity. Nakatomi et al. 62 reported the surgical results of giant fusiform basilar artery aneurysms by various methods, including bypass surgery; a good prognosis was achieved in about 25% of the patients. Although this was better than the conservative treatment groups, the result indicates that the direct surgery for this aneurysm is still of great difficulty even with the latest technique.
Achieving complete occlusion in brain aneurysm clipping is crucial from the perspective of rupture and recurrence prevention. Obermueller et al. 63 reported post clipping broad-based remnants are at a higher risk of regrowth. And postoperative regrowth is at a higher risk of rupture of the aneurysm 64. On the other hand, Nomura et al. 65 reported that acute partial embolization of the ruptured aneurysm was adequate for preventing subsequent rerupture. Dissecting brain aneurysms have a higher frequency of spontaneous regression during follow-up than saccular aneurysms. It has been reported that the natural repair process causes this phenomenon 66. The mechanism is presumed to be that the mural thrombus induces vascular remodeling.
Figure 2. Basilar artery aneurysm
Footnote: Cerebral angiography in oblique incidence. (A) Basilar artery aneurysm (arrowhead), in the junction with the persistent trigeminal artery (arrow). (B) Microcatheterism of the basilar artery aneurysm during the installation of coils, with inflated balloon. (C) Final angiographic control showing the absence of opacification of the basilar artery aneurysm (arrowhead).
[Source 67 ]Basilar artery thrombosis
Basilar artery thrombosis or acute occlusion of the basilar artery may cause brainstem or thalamic ischemia or infarction. Basilar artery thrombosis is a true medical emergency, and if not treated early, brainstem infarction results in rapid deterioration in the level of consciousness and ultimately death. Occlusions of the posterior circulation arteries comprise about a fifth of all strokes but basilar artery occlusion is rare (~1% of all strokes) 4. Acute occlusion of the basilar artery carries a terrible prognosis: ~90% mortality depending on the location, and high morbidity in the survivors 68.
Patients with acute occlusion of the basilar artery will present with sudden and dramatic neurological impairment, the exact characteristics of which will depend on the site of occlusion:
- Sudden death/loss of consciousness
- Top of the basilar syndrome
- visual and oculomotor deficits
- behavioral abnormalities
- somnolence, hallucinations and dream-like behavior
- motor dysfunction is often absent
- Proximal and mid portions of the basilar artery (pons) can result in patients being ‘locked-in syndrome’ 69
- complete loss of movement (quadriparesis and lower cranial dysfunction) and respiratory muscle paralysis
- preserved consciousness
- preserved ocular movements (often only vertical gaze), as the oculomotor nerve is not affected 69
Acute occlusion of the basilar artery can be due to either thromboembolism, atherosclerosis or propagation of intracranial dissection. Although these may occur anywhere, each of these has a predilection for different segments of the basilar artery:
- vertebrobasilar junction
- thromboembolism (e.g. cardioembolic)
- atherosclerosis with thrombosis
- propagation of vertebral arterial dissection (rare)
- midsegment
- atherosclerosis with thrombosis
- distal third or basilar tip
- thromboembolic (e.g. top of the basilar syndrome)
Digital Subtraction Angiography (DSA) remains the gold standard for the diagnosis of basilar artery occlusion. Digital Subtraction Angiography (DSA) provides an image of the blood vessels in the brain to detect a problem with blood flow. The procedure involves inserting a catheter (a small, thin tube) into an artery in the leg and passing it up to the blood vessels in the brain. A contrast dye is injected through the catheter and X-ray images are taken of the blood vessels. Images demonstrate a filling defect within the vessel. However, digital subtraction angiography (DSA) is used only after non-invasive imaging for therapeutic recanalization 4.
Basilar artery thrombosis treatment usually involves catheter-directed intra-arterial thrombolysis and intravenous heparin, which carries a risk of hemorrhage of up to 15%. Mechanical embolectomy with a clot retrieval device has been used in selected cases.
Predictors of outcome after mechanical thrombectomy
- Age and gender: Analysis of the Basilar Artery International Cooperation Study (BASICS) randomized controlled trial reports no significant differences between age groups observed for recanalization rate and incidence of symptomatic intracranial hemorrhage. Patients ≥75 years with basilar artery occlusion have an increased risk of poor outcome compared with younger patients, but a substantial group of patients ≥75 years survive with a good functional outcome 70. No significant gender differences for outcome and recanalization were observed, regardless of treatment modality 71.
- Collateral flow: Several studies, including a series of 21 patients and another of 104 patients, have found that the presence of bilateral posterior communicating arteries on pretreatment CT angiography was associated with more favorable outcomes after mechanical thrombectomy in basilar artery occlusion 72, 73.
- Vertebral artery stenosis: From the Basilar Artery International Cooperation Study (BASICS) randomized controlled trial, in patients with acute basilar artery occlusion, unilateral vertebral artery occlusion or stenosis ≥50% is frequent, but not associated with an increased risk of poor outcome or death. Patients with basilar artery occlusion and bilateral vertebral occlusion had a slightly increased risk of poor outcomes 74.
- Vertebrobasilar artery calcification: In a cohort study of 64 patients, vertebrobasilar artery calcification was found to be an independent predictor of outcome and associated with reduced functional independence and increased mortality in this demographic 75.
Top of the basilar syndrome
Top of the basilar syndrome also known as rostral brainstem infarction, occurs when there is thromboembolic occlusion of the top of the basilar artery. This results in ischemia to the midbrain, temporal, and occipital lobes producing vertical gaze palsy, pupillary palsy, hypersomnolence, abulia, amnesia, and visual hallucinations 76. Notably, sensory and motor dysfunction is generally not present 77.
Clinically, top of the basilar syndrome is characterized by 78:
- visual and oculomotor deficits
- behavioral abnormalities
- somnolence, hallucinations and dreamlike behavior
- motor dysfunction is often absent
Dolichoectasia of the basilar artery
Dolichoectasia of the basilar artery is an anatomic variant in which the basilar artery is elongated, distended and tortuous 79. It is known by various names like dolichoectasia, megadolichoectasia fusiform aneurysm of the vertebral and basilar arteries and tortuous vertebrobasilar system 80. The prevalence of vertebrobasilar dolichoectasia is 4.4%, and it is more commonly observed in women. The major location for vertebrobasilar dolichoectasia is the basilar artery alone (40%), followed by bilateral vertebral arteries, basilar artery (22%) and both vertebral arteries (16%) 81.
Dolichoectasia of the basilar artery is usually asymptomatic and less than 10% of the patients have neurologic symptoms 82. It may manifest clinically by compression of the cranial nerves or brainstem, ischemic symptoms in the vertebrobasilar arterial territory or intracranial bleeding 79. Dolichoectasia of the basilar artery may present with varied clinical syndromes like cerebellar dysfunction, ischemic stroke, transient or permanent motor deficits, central sleep apnea, trigeminal neuralgia, hydrocephalus as well as brain stem compression syndrome 83, 84. Direct cranial nerve compression can lead to isolated cranial nerve dysfunction, usually associated with a normal-sized basilar artery that is tortuous and elongated (neurovascular compression syndrome [NVCS]). Cranial nerve dysfunction most commonly involves the VII (7th) cranial nerve and the V (5th) cranial nerve. Multiple cranial nerve dysfunction is far more likely to occur if there is dilation (ectasia) associated with a tortuous and elongated basilar artery. Cranial nerves affected in descending order of frequency include VII, V, III, VIII, and VI. Symptoms may range from mild to severe.
Rarely, the dilated and ecstatic basilar artery may compress on the floor of the third ventricle causing mild obstructive hydrocephalus. Ikeda et al. 85 studied 7345 adult subjects, and found that 96 of them had asymptomatic vertebrobasilar dolichoectasia. Among these 96 subjects, only four subjects had hydrocephalus as the neuroradiological finding. Hydrocephalus in vertebrobasilar dolichoectasia can be due to compression of the third ventricle by the ectatic, elongated and tortuous basilar artery. Only few cases of hydrocephalus due to direct compression of the aqueduct, foramen of Monro or third ventricle have been reported in the literature 86, 87, 88. Most of these cases have been reported in elderly patients. A peculiar mechanism of hydrocephalus by “water-hammering” effect due to the pulsating blood in the ectatic vessel, which creates cerebrospinal fluid outflow impairment through the third ventricle, has also been described 89.
The cause of vertebrobasilar dolichoectasia is not clear. Hypertension, commonly associated with vertebrobasilar dolichoectasia, may cause continued stress on the walls of the artery and degrade the vessel wall by damaging and loosening the collagen and elastin meshwork that comprises the tunica intima 90.
Traditionally, vertebrobasilar dolichoectasia has been regarded as atherosclerotic in nature, much like aneurysms of the peripheral vascular system. However, recently, Mizutani and Aruga 91 suggested that some cases represent a dissecting process. It may also be a congenital vasculopathy of the elastic layer of the arterial wall 84, 92.
The diagnostic criteria for vertebrobasilar dolichoectasia is a basilar artery or vertebral artery diameter >4.5 mm or deviation of any portion of them higher than 10 mm from the shortest expected course, or basilar length >29.5 mm or intracranial vertebral artery length >23.5 mm 81. The vertebrobasilar system may be considered elongated if the basilar artery lies lateral to the margin of the clivus or dorsum sellae, or if it bifurcates above the plane of the suprasellar cistern 80.
Vertebrobasilar dolichoectasia is characterized by a high degree of variability in clinical outcome. A systematic review of 375 patients determined a fairly high 5-year risk of complications 93:
- brain infarction (17.6%)
- brainstem compression (10.3%)
- transient ischemic attack (10.1%)
- hemorrhagic stroke (4.7%)
- hydrocephalus (3.3%)
- subarachnoid hemorrhage (2.6%)
The same review reported a 5-year mortality risk of 36.2%, with ischemic stroke as the most common cause of death 93.
Factors associated with adverse clinical outcomes include symptoms at the time of diagnosis, the severity of arterial dilation and dolichosis, mural T1 signal, mural thrombi, and interval ectasia progression on follow-up neuroimaging 93.
Management of vertebrobasilar dolichoectasia is limited with intervention restricted to symptomatic cases, although often this is difficult with limited options. For asymptomatic patients with vertebrobasilar dolichoectasia, functional testing such as brainstem auditory-evoked potentials (BAEPs), blink reflex and motor-evoked potentials may be useful for long-term monitoring and may help in the decision-making process prior to the surgical approach for relief of subjective symptoms 92. Patient with obstructive hydrocephalus will get relief in symptoms from ventriculoperitoneal shunt. Cases having obstruction of foramen of Monro may benefit with biventricular shunt 92. Endoscopic third ventriculostomy may be technically difficult in these cases due to the odd anatomy of the basilar trunk.
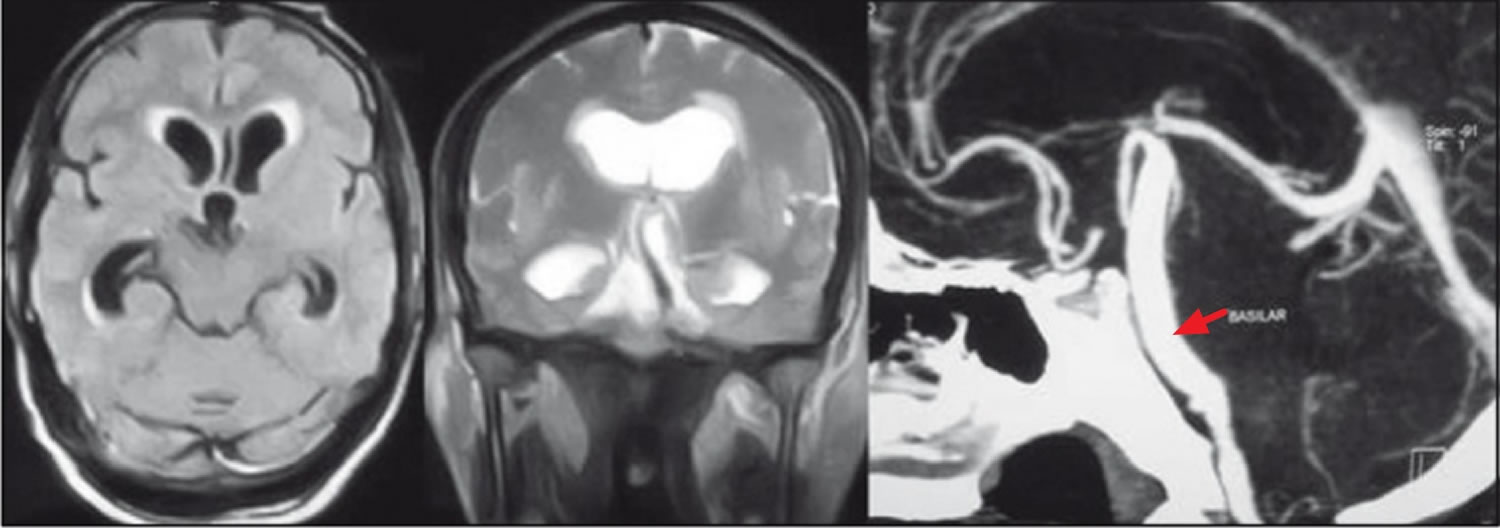
Figure 3. Dolichoectasia of the basilar artery
Footnote: Left and middle pictures show dilated ventricles with dolichoectatic basilar artery compressing the midbrain and outflow of the third ventricle. The right picture shows the computerized tomography angiogram with the dilated and elongated basilar trunk extending into the suprasellar space
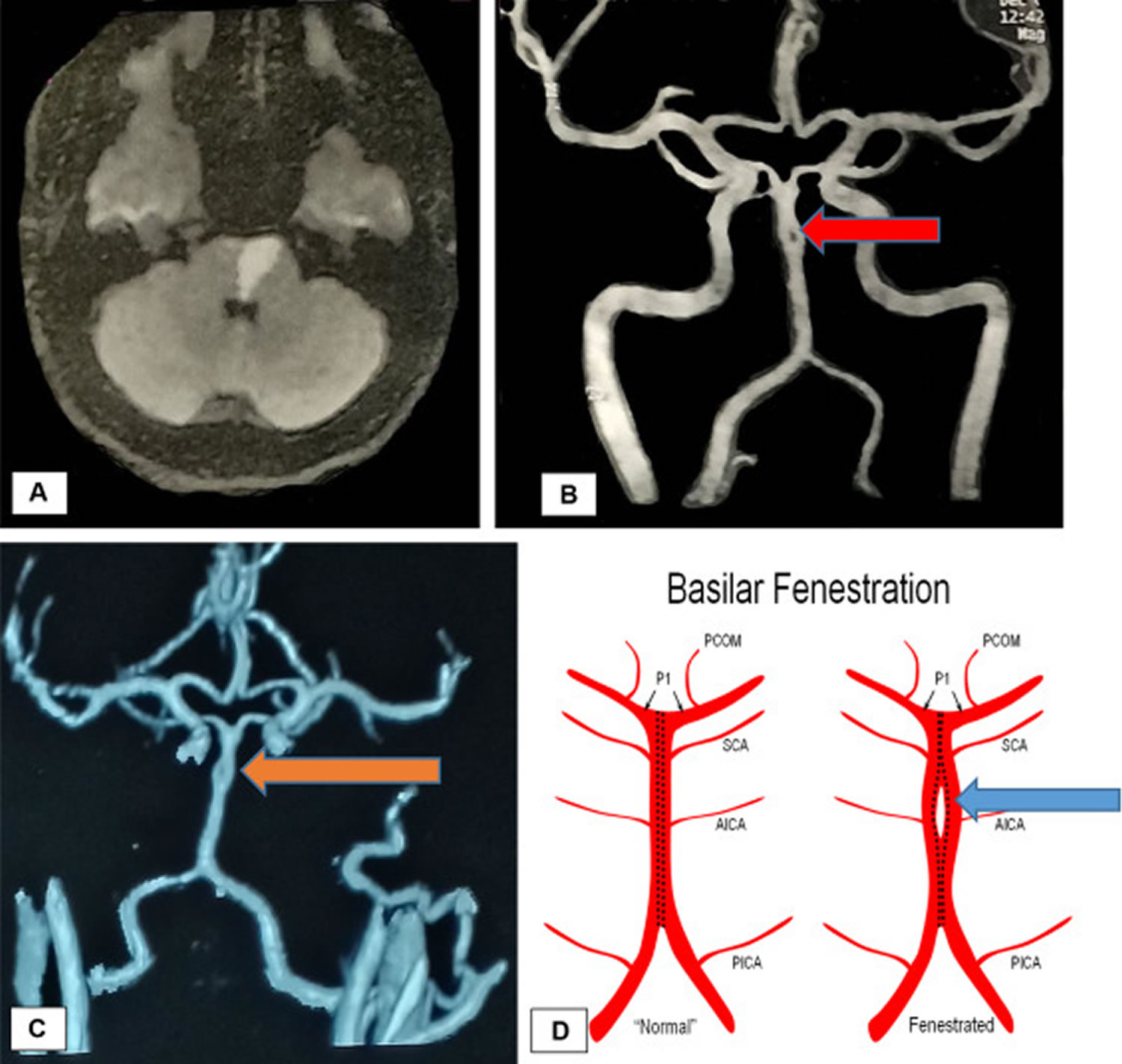
[Source 79 ]Basilar artery fenestration
Basilar artery fenestration also called basilar fenestration, is the second most commonly observed intracranial arterial fenestration and most common congenital anomaly of the basilar artery 94. Fenestration is the luminal division of the vessel into two separate and parallel channels which rejoin distally 95. Basilar artery fenestration is an anatomic variant that is characterized by duplication of a portion of the artery that are connected proximally and distally. Each channel has distinct endothelial and muscularis layers, may be differently sized, and may share adventitial layer depending on degree of embryological fusion 96. Fenestration is thought to occur due to failed fusion of plexiform primitive longitudinal neural arteries 97.
Basilar artery fenestration varies in size. At one extreme, basilar septation is a rare variant considered to be a miniature/aberrant basilar fenestration 98. At the other extreme, complete duplication can be considered extreme fenestration of the basilar artery 99.
Basilar fenestration typically occurs at the lower end of the basilar artery just as the vertebral arteries join. However, it can also be seen in the mid-basilar and distal tip.
Basilar fenestration is generally considered an anatomic variant not requiring observation or treatment. However, adverse complications have been reported in the literature. Although a fenestration is usually of considered to be of minimal significance, there is an association with aneurysm formation near proximal part of fenestration 100. This is hypothesized to be secondary to focal defects in media layer near sites of channel divergence/convergence 101 or due to abnormal flow dynamics 102. Fenestration-associated aneurysms most often occur at the vertebrobasilar junction, followed by the basilar trunk, and are usually saccular in morphology 103. The reported prevalence of aneurysms in cases of basilar fenestration is 7% 96. Thromboembolic posterior circulation infarcts have been reported with basilar artery fenestration 104, 105, 106.
Figure 4. Basilar artery fenestration
[Source 94 ]Hypoplastic basilar artery
Basilar artery hypoplasia is a rare vascular anomaly of the basilar artery. Basilar artery hypoplasia is usually accompanied by one or more fo the following 107:
- persistent carotid-vertebrobasilar anastomoses
- hypoplastic V4 segments of the vertebral arteries
- unilateral or bilateral fetal origin of the posterior cerebral artery
There are some studies suggesting that basilar artery hypoplasia is related to undetermined or lacunar posterior circulation stroke 108, 109, however, further studies are required to confirm this association.
References- Hashemi, S. M., Mahmoodi, R., & Amirjamshidi, A. (2013). Variations in the Anatomy of the Willis’ circle: A 3-year cross-sectional study from Iran (2006-2009). Are the distributions of variations of circle of Willis different in different populations? Result of an anatomical study and review of literature. Surgical neurology international, 4, 65. https://doi.org/10.4103/2152-7806.112185
- Meretoja A, Strbian D, Putaala J, Kaste M, Tatlisumak T; Helsinki Stroke Thrombolysis Registry Group. Hemiplegia and thrombolysis. Eur J Neurol. 2012 Sep;19(9):1235-8. doi: 10.1111/j.1468-1331.2012.03729.x
- van der Hoeven, E. J., Schonewille, W. J., Vos, J. A., Algra, A., Audebert, H. J., Berge, E., Ciccone, A., Mazighi, M., Michel, P., Muir, K. W., Obach, V., Puetz, V., Wijman, C. A., Zini, A., Kappelle, J. L., & BASICS Study Group (2013). The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials, 14, 200. https://doi.org/10.1186/1745-6215-14-200
- Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011 Nov;10(11):1002-14. doi: 10.1016/S1474-4422(11)70229-0
- Smith, W. S., Lev, M. H., English, J. D., Camargo, E. C., Chou, M., Johnston, S. C., Gonzalez, G., Schaefer, P. W., Dillon, W. P., Koroshetz, W. J., & Furie, K. L. (2009). Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke, 40(12), 3834–3840. https://doi.org/10.1161/STROKEAHA.109.561787
- Nagel S. Schlaganfall bei akutem Verschluss der A. basilaris : Diagnostik und Therapie [Stroke due to acute occlusion of the basilar artery : Diagnosis and treatment]. Med Klin Intensivmed Notfmed. 2017 Nov;112(8):679-686. German. doi: 10.1007/s00063-017-0347-0
- Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, Engelter ST, Tanne D, Muir KW, Molina CA, Thijs V, Audebert H, Pfefferkorn T, Szabo K, Lindsberg PJ, de Freitas G, Kappelle LJ, Algra A; BASICS study group. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009 Aug;8(8):724-30. doi: 10.1016/S1474-4422(09)70173-5
- Johnson TM, Romero CS, Smith AT. Locked-in syndrome responding to thrombolytic therapy. Am J Emerg Med. 2018 Oct;36(10):1928.e5-1928.e7. doi: 10.1016/j.ajem.2018.07.003
- O’Reilly, S. T., Rennie, I., McIlmoyle, J., & Smyth, G. (2019). Direct puncture of the V3 segment of the vertebral artery in acute basilar artery stroke: an alternative approach in desperate circumstances. BMJ case reports, 12(8), e231335. https://doi.org/10.1136/bcr-2019-231335
- Nikić PM, Jovanović D, Paspalj D, Georgievski-Brkić B, Savić M. Clinical characteristics and outcome in the acute phase of ischemic locked-in syndrome: case series of twenty patients with ischemic LIS. Eur Neurol. 2013;69(4):207-12. doi: 10.1159/000345272
- Caplan LR. “Top of the basilar” syndrome. Neurology. 1980 Jan;30(1):72-9. doi: 10.1212/wnl.30.1.72
- Demel, S. L., & Broderick, J. P. (2015). Basilar Occlusion Syndromes: An Update. The Neurohospitalist, 5(3), 142–150. https://doi.org/10.1177/1941874415583847
- Amin-Hanjani, S., Pandey, D. K., Rose-Finnell, L., Du, X., Richardson, D., Thulborn, K. R., Elkind, M. S., Zipfel, G. J., Liebeskind, D. S., Silver, F. L., Kasner, S. E., Aletich, V. A., Caplan, L. R., Derdeyn, C. P., Gorelick, P. B., Charbel, F. T., & Vertebrobasilar Flow Evaluation and Risk of Transient Ischemic Attack and Stroke Study Group (2016). Effect of Hemodynamics on Stroke Risk in Symptomatic Atherosclerotic Vertebrobasilar Occlusive Disease. JAMA neurology, 73(2), 178–185. https://doi.org/10.1001/jamaneurol.2015.3772
- Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol. 2013 Oct;12(10):989-98. doi: 10.1016/S1474-4422(13)70211-4
- Gulli G, Marquardt L, Rothwell PM, Markus HS. Stroke risk after posterior circulation stroke/transient ischemic attack and its relationship to site of vertebrobasilar stenosis: pooled data analysis from prospective studies. Stroke. 2013 Mar;44(3):598-604. doi: 10.1161/STROKEAHA.112.669929
- Derdeyn, Colin P et al. Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis Trial Investigators (2014). Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet (London, England), 383(9914), 333–341. https://doi.org/10.1016/S0140-6736(13)62038-3
- Abuzinadah, A. R., Alanazy, M. H., Almekhlafi, M. A., Duan, Y., Zhu, H., Mazighi, M., Lutsep, H. L., Donnon, T., & Hill, M. D. (2016). Stroke recurrence rates among patients with symptomatic intracranial vertebrobasilar stenoses: systematic review and meta-analysis. Journal of neurointerventional surgery, 8(2), 112–116. https://doi.org/10.1136/neurintsurg-2014-011458
- Kjerpeseth LJ, Ellekjær H, Selmer R, Ariansen I, Furu K, Skovlund E. Risk factors for stroke and choice of oral anticoagulant in atrial fibrillation. Eur J Clin Pharmacol. 2018 Dec;74(12):1653-1662. doi: 10.1007/s00228-018-2540-3
- Reinemeyer NE, Tadi P, Lui F. Basilar Artery Thrombosis. [Updated 2021 Sep 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532241
- Ropper AH. ‘Convulsions’ in basilar artery occlusion. Neurology. 1988 Sep;38(9):1500-1. doi: 10.1212/wnl.38.9.1500-a
- Ausman, J. I., Liebeskind, D. S., Gonzalez, N., Saver, J., Martin, N., Villablanca, J. P., Vespa, P., Duckwiler, G., Jahan, R., Niu, T., Salamon, N., Yoo, B., Tateshima, S., Buitrago Blanco, M. M., & Starkman, S. (2018). A review of the diagnosis and management of vertebral basilar (posterior) circulation disease. Surgical neurology international, 9, 106. https://doi.org/10.4103/sni.sni_373_17
- Chatterjee, S. A., Daly, J. J., Porges, E. C., Fox, E. J., Rose, D. K., McGuirk, T. E., Otzel, D. M., Butera, K. A., & Clark, D. J. (2018). Mobility Function and Recovery After Stroke: Preliminary Insights From Sympathetic Nervous System Activity. Journal of neurologic physical therapy : JNPT, 42(4), 224–232. https://doi.org/10.1097/NPT.0000000000000238
- Chen CJ, Chuang TY, Hansen L, Dutta S, Ding D, Buell TJ, Ironside N, Patibandla MR, Southerland AM, Worrall BB, Kalani MYS. Predictors of 30-day mortality after endovascular mechanical thrombectomy for acute ischemic stroke. J Clin Neurosci. 2018 Nov;57:38-42. doi: 10.1016/j.jocn.2018.08.044
- Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar artery occlusive disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004 Apr;61(4):496-504. doi: 10.1001/archneur.61.4.496
- Kuan CY, Hung KL. Vertebral artery dissection complicated by basilar artery occlusion. Pediatr Neonatol. 2014 Aug;55(4):316-9. doi: 10.1016/j.pedneo.2012.12.014
- Oshima K, Sakaura H, Iwasaki M, Nakura A, Fujii R, Yoshikawa H. Repeated vertebrobasilar thromboembolism in a patient with severe upper cervical instability because of rheumatoid arthritis. Spine J. 2011 Feb;11(2):e1-5. doi: 10.1016/j.spinee.2010.11.015
- Bäuerle J, Zitzmann A, Egger K, Meckel S, Weiller C, Harloff A. The great imitator–still today! A case of meningovascular syphilis affecting the posterior circulation. J Stroke Cerebrovasc Dis. 2015 Jan;24(1):e1-3. doi: 10.1016/j.jstrokecerebrovasdis.2014.07.046
- Akman-Demir G, Serdaroglu P, Tasçi B. Clinical patterns of neurological involvement in Behçet’s disease: evaluation of 200 patients. The Neuro-Behçet Study Group. Brain. 1999 Nov;122 ( Pt 11):2171-82. doi: 10.1093/brain/122.11.2171
- Reid, M., Famuyide, A.O., Forkert, N.D. et al. Accuracy and Reliability of Multiphase CTA Perfusion for Identifying Ischemic Core. Clin Neuroradiol 29, 543–552 (2019). https://doi.org/10.1007/s00062-018-0717-x
- Writing Group for the BASILAR Group. Assessment of Endovascular Treatment for Acute Basilar Artery Occlusion via a Nationwide Prospective Registry. JAMA Neurol. 2020;77(5):561–573. doi:10.1001/jamaneurol.2020.0156
- Macleod MR, Davis SM, Mitchell PJ, Gerraty RP, Fitt G, Hankey GJ, Stewart-Wynne EG, Rosen D, McNeil JJ, Bladin CF, Chambers BR, Herkes GK, Young D, Donnan GA. Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovasc Dis. 2005;20(1):12-7. doi: 10.1159/000086121
- Arnold, M., Nedeltchev, K., Schroth, G., Baumgartner, R. W., Remonda, L., Loher, T. J., Stepper, F., Sturzenegger, M., Schuknecht, B., & Mattle, H. P. (2004). Clinical and radiological predictors of recanalisation and outcome of 40 patients with acute basilar artery occlusion treated with intra-arterial thrombolysis. Journal of neurology, neurosurgery, and psychiatry, 75(6), 857–862. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1739049/pdf/v075p00857.pdf
- Xiong, Y. J., Gong, J. M., Zhang, Y. C., Zhao, X. L., Xu, S. B., Pan, D. J., Qu, W. S., & Tian, D. S. (2018). Endovascular thrombectomy versus medical treatment for large vessel occlusion stroke with mild symptoms: A meta-analysis. PloS one, 13(8), e0203066. https://doi.org/10.1371/journal.pone.0203066
- Kheiri B, Osman M, Abdalla A, Haykal T, Ahmed S, Hassan M, Bachuwa G, Al Qasmi M, Bhatt DL. Tenecteplase versus alteplase for management of acute ischemic stroke: a pairwise and network meta-analysis of randomized clinical trials. J Thromb Thrombolysis. 2018 Nov;46(4):440-450. doi: 10.1007/s11239-018-1721-3
- Moussaddy A, Demchuk AM, Hill MD. Thrombolytic therapies for ischemic stroke: Triumphs and future challenges. Neuropharmacology. 2018 May 15;134(Pt B):272-279. doi: 10.1016/j.neuropharm.2017.11.010
- Ritvonen J, Strbian D, Silvennoinen H, Virtanen P, Salonen O, Lindsberg PJ, Sairanen T. Thrombolysis and adjunct anticoagulation in patients with acute basilar artery occlusion. Eur J Neurol. 2019 Jan;26(1):128-135. doi: 10.1111/ene.13781
- Kumar G, Shahripour RB, Alexandrov AV. Recanalization of acute basilar artery occlusion improves outcomes: a meta-analysis. J Neurointerv Surg. 2015 Dec;7(12):868-74. doi: 10.1136/neurintsurg-2014-011418
- Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, Dillon W, Warach S, Broderick J, Tilley B, Sacks D; Technology Assessment Committee of the American Society of Interventional and Therapeutic Neuroradiology; Technology Assessment Committee of the Society of Interventional Radiology. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003 Aug;34(8):e109-37. doi: 10.1161/01.STR.0000082721.62796.09. Epub 2003 Jul 17. Erratum in: Stroke. 2003 Nov;34(11):2774.
- Tomsick, T., Broderick, J., Carrozella, J., Khatri, P., Hill, M., Palesch, Y., Khoury, J., & Interventional Management of Stroke II Investigators (2008). Revascularization results in the Interventional Management of Stroke II trial. AJNR. American journal of neuroradiology, 29(3), 582–587. https://doi.org/10.3174/ajnr.A0843
- Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006 Mar;37(3):922-8. doi: 10.1161/01.STR.0000202582.29510.6b
- Sairanen T, Strbian D, Soinne L, Silvennoinen H, Salonen O, Artto V, Koskela I, Häppölä O, Kaste M, Lindsberg PJ; Helsinki Stroke Thrombolysis Registry (HSTR) Group. Intravenous thrombolysis of basilar artery occlusion: predictors of recanalization and outcome. Stroke. 2011 Aug;42(8):2175-9. doi: 10.1161/STROKEAHA.110.605584
- Jankowitz BT, Aleu A, Lin R, Jumaa M, Kanaan H, Kostov D, Hammer M, Uchino K, Wechsler LR, Horowitz M, Jovin TG. Endovascular treatment of basilar artery occlusion by manual aspiration thrombectomy. J Neurointerv Surg. 2010 Jun;2(2):110-4. doi: 10.1136/jnis.2009.001420
- Strbian D, Sairanen T, Silvennoinen H, Salonen O, Lindsberg PJ. Intravenous thrombolysis of basilar artery occlusion: thrombus length versus recanalization success. Stroke. 2014 Jun;45(6):1733-8. doi: 10.1161/STROKEAHA.114.004884
- Schonewille, W. J., Algra, A., Serena, J., Molina, C. A., & Kappelle, L. J. (2005). Outcome in patients with basilar artery occlusion treated conventionally. Journal of neurology, neurosurgery, and psychiatry, 76(9), 1238–1241. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1739786/pdf/v076p01238.pdf
- Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006 Aug 31;355(9):928-39. doi: 10.1056/NEJMra052760
- Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968 Jan;28(1):14-20. doi: 10.3171/jns.1968.28.1.0014
- Barry C, Turner RJ, Corrigan F, Vink R. New therapeutic approaches to subarachnoid hemorrhage. Expert Opin Investig Drugs. 2012 Jun;21(6):845-59. doi: 10.1517/13543784.2012.683113
- Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009 Apr;8(4):355-69. doi: 10.1016/S1474-4422(09)70025-0
- Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, Duldner JE Jr, Harbaugh RE, Patel AB, Rosenwasser RH; American Heart Association. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009 Mar;40(3):994-1025. doi: 10.1161/STROKEAHA.108.191395. Epub 2009 Jan 22. Erratum in: Stroke. 2009 Jul;40(7):e518.
- Grasso, G., Alafaci, C., & Macdonald, R. L. (2017). Management of aneurysmal subarachnoid hemorrhage: State of the art and future perspectives. Surgical neurology international, 8, 11. https://doi.org/10.4103/2152-7806.198738
- Izumo, T., Fujimoto, T., Morofuji, Y., Tateishi, Y., & Matsuo, T. (2021). Partial Clipping Occlusion Including Rupture Point Is an Effective Strategy for Ruptured Giant Fusiform Basilar Artery Aneurysm: A Technical Case Report. Frontiers in neurology, 12, 743654. https://doi.org/10.3389/fneur.2021.743654
- Dandurand C, Prakash S, Sepehry AA, Tourigny K, Haw CS, Gooderham P, Moore J, Redekop G. Basilar Apex Aneurysm: Case Series, Systematic Review, and Meta-analysis. World Neurosurg. 2020 Jun;138:e183-e190. doi: 10.1016/j.wneu.2020.02.064
- Rho MH, Park HJ, Chung EC, Choi YJ, Lee SY, Won YS, Kim BM. Various techniques of stent-assisted coil embolization of wide-necked or fusiform artherosclerotic and dissecting unruptured vertebrobasilar artery aneurysms for reducing recanalization: mid-term results. Acta Neurochir (Wien). 2013 Nov;155(11):2009-17. doi: 10.1007/s00701-013-1866-y
- Wang Y, Yang X, Youxiang L, Shiqing M, Chuhan J, Zhongxue W, Kocer N. Treatment of symptomatic fusiform aneurysm in basilar artery by stenting following coiling technique. Turk Neurosurg. 2014;24(1):44-7. doi: 10.5137/1019-5149.JTN.8017-13.1
- Juszkat, R., Nowak, S., Smól, S., Kociemba, W., Blok, T., & Zarzecka, A. (2007). Leo stent for endovascular treatment of broad-necked and fusiform intracranial aneurysms. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences, 13(3), 255–269. https://doi.org/10.1177/159101990701300305
- Strange F, Kienzler J, Muehleisen B, Diepers M, Fandino J, Remonda L, Marbacher S. Early Rupture of a Giant Basilar Artery Aneurysm after LEO Stenting: Case Report and Review of the Literature. J Neurol Surg A Cent Eur Neurosurg. 2020 Mar;81(2):177-184. doi: 10.1055/s-0039-1693108
- Awad AJ, Mascitelli JR, Haroun RR, De Leacy RA, Fifi JT, Mocco J. Endovascular management of fusiform aneurysms in the posterior circulation: the era of flow diversion. Neurosurg Focus. 2017 Jun;42(6):E14. doi: 10.3171/2017.3.FOCUS1748
- Jia, L., Wang, J., Zhang, L., Zhang, Y., You, W., Yang, X., & Lv, M. (2020). Pediatric Patient With a Giant Vertebrobasilar Dissecting Aneurysm Successfully Treated With Three Pipeline Embolization Devices. Frontiers in neurology, 11, 633. https://doi.org/10.3389/fneur.2020.00633
- Kulcsár Z, Ernemann U, Wetzel SG, Bock A, Goericke S, Panagiotopoulos V, Forsting M, Ruefenacht DA, Wanke I. High-profile flow diverter (silk) implantation in the basilar artery: efficacy in the treatment of aneurysms and the role of the perforators. Stroke. 2010 Aug;41(8):1690-6. doi: 10.1161/STROKEAHA.110.580308
- Wang, C. B., Shi, W. W., Zhang, G. X., Lu, H. C., & Ma, J. (2016). Flow diverter treatment of posterior circulation aneurysms. A meta-analysis. Neuroradiology, 58(4), 391–400. https://doi.org/10.1007/s00234-016-1649-2
- Sughrue, M. E., Saloner, D., Rayz, V. L., & Lawton, M. T. (2011). Giant intracranial aneurysms: evolution of management in a contemporary surgical series. Neurosurgery, 69(6), 1261–1271. https://doi.org/10.1227/NEU.0b013e31822bb8a6
- Nakatomi, H., Kiyofuji, S., Ono, H., Tanaka, M., Kamiyama, H., Takizawa, K., Imai, H., Saito, N., Shiokawa, Y., Morita, A., Flemming, K. D., & Link, M. J. (2020). Giant Fusiform and Dolichoectatic Aneurysms of the Basilar Trunk and Vertebrobasilar Junction-Clinicopathological and Surgical Outcome. Neurosurgery, 88(1), 82–95. https://doi.org/10.1093/neuros/nyaa317
- Obermueller, K., Hostettler, I., Wagner, A., Boeckh-Behrens, T., Zimmer, C., Gempt, J., Meyer, B., & Wostrack, M. (2021). Frequency and risk factors for postoperative aneurysm residual after microsurgical clipping. Acta neurochirurgica, 163(1), 131–138. https://doi.org/10.1007/s00701-020-04639-5
- Izumo T, Matsuo T, Morofuji Y, Hiu T, Horie N, Hayashi K, Nagata I. Microsurgical clipping for recurrent aneurysms after initial endovascular coil embolization. World Neurosurg. 2015 Feb;83(2):211-8. doi: 10.1016/j.wneu.2014.08.013
- Nomura, M., Kida, S., Uchiyama, N., Yamashima, T., Yamashita, J., Yoshikawa, J., & Matsui, O. (2000). Aneurysm clipping after partial endovascular embolization for ruptured cerebral aneurysms. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences, 6 Suppl 1(Suppl 1), 49–58. https://doi.org/10.1177/15910199000060S105
- Mizutani T. Natural course of intracranial arterial dissections. J Neurosurg. 2011 Apr;114(4):1037-44. doi: 10.3171/2010.9.JNS10668
- Aguiar, G. B., Conti, M. L., Veiga, J. C., Jory, M., & Souza, R. B. (2011). Basilar artery aneurysm at a persistent trigeminal artery junction. A case report and literature review. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences, 17(3), 343–346. https://doi.org/10.1177/159101991101700310
- Connell L, Koerte IK, Laubender RP, Morhard D, Linn J, Becker HC, Reiser M, Brueckmann H, Ertl-Wagner B. Hyperdense basilar artery sign-a reliable sign of basilar artery occlusion. Neuroradiology. 2012 Apr;54(4):321-7. doi: 10.1007/s00234-011-0887-6
- Pope TL. Harris & Harris’ Radiology of Emergency Medicine. LWW. (2012) ISBN:145110720X.
- Vergouwen MDI, Compter A, Tanne D, Engelter ST, Audebert H, Thijs V, et al. Outcomes of basilar artery occlusion in patients aged 75 years or older in the Basilar Artery International Cooperation Study. Journal of neurology. 2012;259(11):2341-6.
- Arnold M, Fischer U, Compter A, Gralla J, Findling O, Mattle HP, et al. Acute basilar artery occlusion in the Basilar Artery International Cooperation Study: does gender matter? Stroke. 2010;41(11):2693-6.
- Goyal N, Tsivgoulis G, Nickele C, Doss VT, Hoit D, Alexandrov AV, et al. Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg. 2016;8(8):783-6.
- Maus V, Kalkan A, Kabbasch C, Abdullayev N, Stetefeld H, Barnikol UB, et al. Mechanical Thrombectomy in Basilar Artery Occlusion. Clinical Neuroradiology. 2019;29(1):153-60.
- Compter A, van der Hoeven EJ, van der Worp HB, Vos JA, Weimar C, Rueckert CM, et al. Vertebral artery stenosis in the Basilar Artery International Cooperation Study (BASICS): prevalence and outcome. J Neurol. 2015;262(2):410-7.
- Diprose William K, Diprose James P, Tarr Gregory P, Sutcliffe J, McFetridge A, Brew S, et al. Vertebrobasilar Artery Calcification and Outcomes in Posterior Circulation Large Vessel Occlusion Thrombectomy. Stroke. 2020;51(4):1301-4.
- Alwood BT, Dossani RH. Vertebrobasilar Stroke. [Updated 2022 Jan 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556084
- Ogawa K, Suzuki Y, Takahashi K, Kamei S, Ishikawa H. Clinical Study of Eleven Patients with Midbrain Infarction-Induced Oculomotor Nerve Palsy. J Stroke Cerebrovasc Dis. 2016 Jul;25(7):1631-1638. doi: 10.1016/j.jstrokecerebrovasdis.2016.03.020
- Top of the basilar syndrome. https://radiopaedia.org/articles/top-of-the-basilar-syndrome?lang=us
- Kansal, R., Mahore, A., Dange, N., & Kukreja, S. (2011). Dolichoectasia of vertebrobasilar arteries as a cause of hydrocephalus. Journal of neurosciences in rural practice, 2(1), 62–64. https://doi.org/10.4103/0976-3147.80106
- Smoker, W. R., Corbett, J. J., Gentry, L. R., Keyes, W. D., Price, M. J., & McKusker, S. (1986). High-resolution computed tomography of the basilar artery: 2. Vertebrobasilar dolichoectasia: clinical-pathologic correlation and review. AJNR. American journal of neuroradiology, 7(1), 61–72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8334773/pdf/3082145.pdf
- Ubogu, E. E., & Zaidat, O. O. (2004). Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: a cohort study. Journal of neurology, neurosurgery, and psychiatry, 75(1), 22–26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1757450/pdf/v075p00022.pdf
- Resta M, Gentile MA, Di Cuonzo F, Vinjau E, Brindicci D, Carella A. Clinical-angiographic correlations in 132 patients with megadolichovertebrobasilar anomaly. Neuroradiology. 1984;26(3):213-6. doi: 10.1007/BF00342416
- Milandre L, Bonnefoi B, Pestre P, Pellissier JF, Grisoli F, Khalil R. Dolichoectasies artérielles vertébrobasilaires. Complications et pronostic [Vertebrobasilar arterial dolichoectasia. Complications and prognosis]. Rev Neurol (Paris). 1991;147(11):714-22. French.
- Tomasello F, Alafaci C, Salpietro FM, Longo M. Bulbar compression by an ectatic vertebral artery: a novel neurovascular construct relieved by microsurgical decompression. Neurosurgery. 2005 Jan;56(1 Suppl):117-24; discussion 117-24. doi: 10.1227/01.neu.0000146684.23593.b4
- Ikeda K, Nakamura Y, Hirayama T, Sekine T, Nagata R, Kano O, Kawabe K, Kiyozuka T, Tamura M, Iwasaki Y. Cardiovascular risk and neuroradiological profiles in asymptomatic vertebrobasilar dolichoectasia. Cerebrovasc Dis. 2010;30(1):23-8. doi: 10.1159/000313440
- Siddiqui A, Chew NS, Miszkiel K. Vertebrobasilar dolichoectasia: a rare cause of obstructive hydrocephalus: case report. Br J Radiol. 2008 Apr;81(964):e123-6. doi: 10.1259/bjr/27603660
- Thiex R, Mull M. Basilar megadolicho trunk causing obstructive hydrocephalus at the foramina of Monro. Surg Neurol. 2006 Feb;65(2):199-201. doi: 10.1016/j.surneu.2005.04.041
- Ricci G, Lenzi J, Esposito V. Hydrocephalus caused by dolichoectatic basilar artery. Case report. J Neurosurg Sci. 2000 Sep;44(3):155-8.
- Marinescu M, Remy A, Dufour H, Derome P, Cambon H. Un mécanisme particulier d’hydrocéphalie: l’effet “coup de marteau” [A peculiar mechanism of hydrocephalus: the “water-hammering” effect]. Neurochirurgie. 1998 Apr;44(2):117-20. French.
- Schulz R, Fegbeutel C, Althoff A, Traupe H, Grimminger F, Seeger W. Central sleep apnoea and unilateral diaphragmatic paralysis associated with vertebral artery compression of the medulla oblongata. J Neurol. 2003 Apr;250(4):503-5. doi: 10.1007/s00415-003-1016-1
- Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995 May;36(5):905-11; discussion 912-3. doi: 10.1227/00006123-199505000-00003
- Passero S, Filosomi G. Posterior circulation infarcts in patients with vertebrobasilar dolichoectasia. Stroke. 1998 Mar;29(3):653-9. doi: 10.1161/01.str.29.3.653
- Franciscus J Wolters, Gabriël J E Rinkel & Mervyn D I Vergouwen (2013) Clinical course and treatment of vertebrobasilar dolichoectasia: a systematic review of the literature, Neurological Research, 35:2, 131-137. https://doi.org/10.1179/1743132812Y.0000000149
- Basilar artery fenestration and ischemic stroke: An unclear causal relationship. JMV-Journal de Médecine Vasculaire, Volume 45, Issue 2,2020, Pages 62-66, ISSN 2542-4513,https://doi.org/10.1016/j.jdmv.2020.01.147
- Gailloud, P., Albayram, S., Fasel, J. H., Beauchamp, N. J., & Murphy, K. J. (2002). Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. AJNR. American journal of neuroradiology, 23(4), 585–587. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7975097
- Dimmick SJ, Faulder KC. Normal variants of the cerebral circulation at multidetector CT angiography. Radiographics. 2009 Jul-Aug;29(4):1027-43. doi: 10.1148/rg.294085730
- Cademartiri, F., Stojanov, D., Dippel, D. W., Van Der Lugt, A., & Tanghe, H. (2003). Noninvasive detection of a ruptured aneurysm at a basilar artery fenestration with submillimeter multisection CT angiography. AJNR. American journal of neuroradiology, 24(10), 2009–2010. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8148929
- Small JE, Macey MB, Wakhloo AK, Sehgal S. CTA Evaluation of Basilar Septations: An Entity Better Characterized as Aberrant Basilar Fenestrations. AJNR Am J Neuroradiol. 2021 Apr;42(4):701-707. doi: 10.3174/ajnr.A7008
- Goldstein JH, Woodcock R, Do HM, Phillips CD, Dion JE. Complete duplication or extreme fenestration of the basilar artery. AJNR Am J Neuroradiol. 1999 Jan;20(1):149-50.
- Uchino A, Takase Y, Nomiyama K, Egashira R, Kudo S. Fenestration of the middle cerebral artery detected by MR angiography. Magn Reson Med Sci. 2006 Apr;5(1):51-5. doi: 10.2463/mrms.5.51
- Cooke, D. L., Stout, C. E., Kim, W. T., Kansagra, A. P., Yu, J. P., Gu, A., Jewell, N. P., Hetts, S. W., Higashida, R. T., Dowd, C. F., & Halbach, V. V. (2014). Cerebral arterial fenestrations. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences, 20(3), 261–274. https://doi.org/10.15274/INR-2014-10027
- Guo X, Gao L, Shi Z, Liu D, Wang Y, Sun Z, Chen Y, Chen W, Yang Y. Intracranial Arterial Fenestration and Risk of Aneurysm: A Systematic Review and Meta-Analysis. World Neurosurg. 2018 Jul;115:e592-e598. doi: 10.1016/j.wneu.2018.04.106
- Sturiale C, Stifano V, Della Pepa G et al. Intracranial Aneurysms of the Posterior Circulation Associated with a Fenestration: A Systematic Review. J Neurosurg Sci. 2019;63(5). doi:10.23736/s0390-5616.18.04225-x
- Gold, J. J., & Crawford, J. R. (2013). An unusual cause of pediatric stroke secondary to congenital basilar artery fenestration. Case reports in critical care, 2013, 627972. https://doi.org/10.1155/2013/627972
- Miyamoto, N., Ueno, Y., Hira, K., Kijima, C., Nakajima, S., Yamashiro, K., & Hattori, N. (2020). Characteristics of Clinical Symptoms, Cerebral Images and Stroke Etiology in Vertebro-Basilar Artery Fenestration-Related Infarction. Brain sciences, 10(4), 243. https://doi.org/10.3390/brainsci10040243
- Ha, S. H., Kim, H. G., & Kim, B. J. (2020). Bilateral pontine infarction with basilar artery fenestration: A case report. Medicine, 99(32), e21530. https://doi.org/10.1097/MD.0000000000021530
- Basilar artery hypoplasia. https://radiopaedia.org/articles/basilar-artery-hypoplasia?lang=us
- Chuang YM, Huang YC, Hu HH, Yang CY. Toward a further elucidation: role of vertebral artery hypoplasia in acute ischemic stroke. Eur Neurol. 2006;55(4):193-7. doi: 10.1159/000093868
- Olindo S, Khaddam S, Bocquet J, Chausson N, Aveillan M, Cabre P, Smadja D. Association between basilar artery hypoplasia and undetermined or lacunar posterior circulation ischemic stroke. Stroke. 2010 Oct;41(10):2371-4. doi: 10.1161/STROKEAHA.110.593145