Becker’s nevus
Becker’s nevus also known as Becker melanosis, is a non-cancerous, large, brown birthmark occurring mostly in males. Becker’s nevus can be present at birth, but is usually first noticed around puberty. Becker’s nevus typically occurs on one shoulder and upper trunk but occasionally occurs elsewhere on the body. A Becker’s nevus often becomes darker, and excessive hair growth (hypertrichosis) and acne may develop within the nevus.
Becker’s nevus is due to overgrowth of the epidermis (upper layer of the skin), pigment cells (melanocytes) and hair follicles 1. The specific underlying cause is unknown 2. Because it often forms around puberty in males and is sometimes associated with acne and hair growth, its development may be triggered by androgens (male sex hormones such as testosterone) 2.
Treatment is primarily for cosmetic reasons (hyperpigmentation or hair growth) and may include Ruby laser treatment or laser-assisted hair removal 2.
In very rare cases, Becker’s nevus is associated with other skin features; muscular or skeletal features; or underdevelopment (hypoplasia) of the breast. When this occurs, the condition is known as Becker’s nevus syndrome 3.
Becker’s nevus is a benign entity and does not require treatment except for cosmetic reasons.
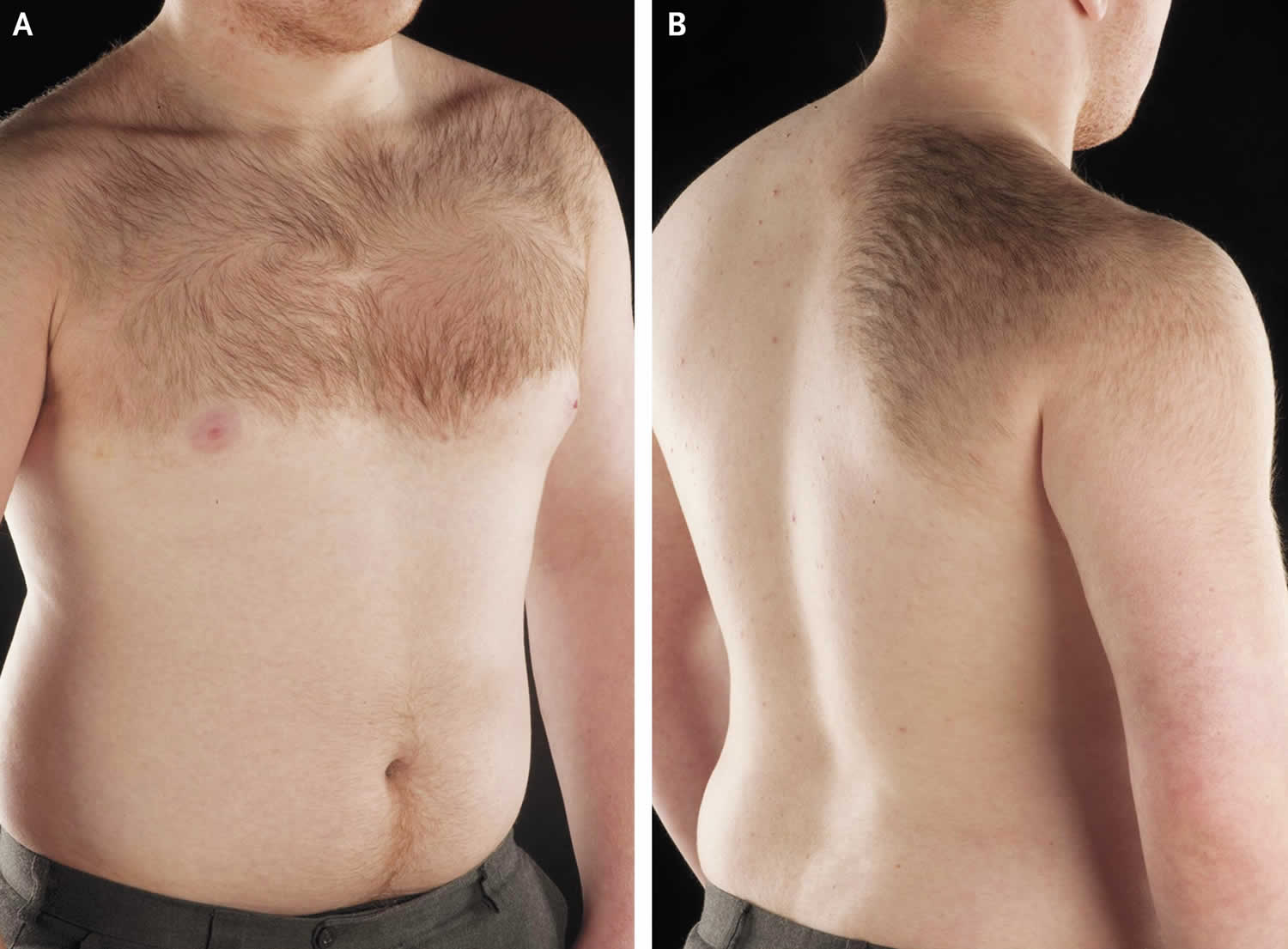
Figure 1. Becker’s nevus (Becker’s nevus of chest wall with associated hypertrichosis)
Figure 2. Becker’s nevus
Becker nevus syndrome
Rarely, like other birthmarks, there may be some abnormality of underlying tissues derived from the same embryonic cell type, the ectoderm. This is known as the Becker nevus syndrome, a type of epidermal nevus syndrome. These abnormalities may include:
- Smooth muscle hamartoma (overgrowth of smooth muscle tissue like a deep birthmark)
- Under-development of underlying structures such as breast, pectoral muscle, fat, limb, chest wall, spine
- Over-development of a tissue such as adrenal gland, limb, fingers or toes, scrotum.
Becker’s nevus causes
The cause and pathogenesis of Becker’s nevus remain uncertain. Androgens may play a role in Becker’s nevus, as evidenced by its peripubertal development, male preponderance, hypertrichosis, occasional development of acneform lesions within the patch, and rare association with accessory scrotum in the genital region. In addition, a significant increase in the number of androgen receptors in Becker’s nevus lesional skin has been reported 4.
Although Becker’s nevus usually is a sporadic condition that manifests in the peripubertal period, both congenital and familial cases have been described 5.
Becker’s nevus signs and symptoms
A Becker nevus is a large one-sided brown patch, sometimes over half the upper back or chest. After puberty it often becomes darker and quite hairy, a feature also called hypertrichosis. Occasionally acne may develop in the nevus.
The earliest finding of Becker’s nevus is an asymptomatic irregular tan-to-brown patch, most commonly located over the shoulder, upper chest, or back, as shown in the images above.
Pigmentation may be subtle, and onset most commonly occurs in the peripubertal period. The patch expands during the first several years as new irregular pigmented macules and patches develop at the periphery and coalesce with the larger patch. This expansion results in a geographic configuration that may cover a large area.
Several months to years after the appearance of pigmentation, thick brown-to-black hairs develop both within and in close proximity to the patch. Hair density is highly variable and occasionally, hypertrichosis does not occur.
The central area in the patch may thicken, and acne vulgaris may develop.
Once present, the patch remains indefinitely, although minimal pigmentary fading may occur in adulthood.
Occasionally, Becker nevus may be associated with smooth muscle hamartoma. Rarely, hypoplasia of underlying structures, such as unilateral breast hypoplasia, has been reported 6.
Other associations seen with Becker nevus include unilateral or ipsilateral pectoralis major aplasia, ipsilateral limb shortening, ipsilateral foot enlargement, spina bifida, scoliosis, pectus carinatum, localized lipoatrophy 7, congenital adrenal hyperplasia 8, polythelia (presence of an additional nipple) 9, and accessory scrotum 10.
Becker’s nevus is considered a benign process; however, an association with melanoma was discussed in a series of 9 patients in whom both Becker nevus and melanoma developed. In this series, 5 patients developed melanoma on the same body site as the Becker nevus, but in 1 patient only did melanoma develop within the Becker nevus.
Becker’s nevus diagnosis
A Becker’s nevus on the upper trunk in a peripubertal male is difficult to confuse with other pigmented lesions.
Occasionally, a congenital Becker nevus may simulate congenital melanocytic nevus or nevus spilus, necessitating histologic examination to distinguish between lesions.
A Becker nevus without hypertrichosis may resemble a café au lait patch or postinflammatory hyperpigmentation.
Skin biopsy provides histologic diagnosis of Becker’s nevus and helps distinguish it from other clinical entities.
Becker’s nevus treatment
There is no effective treatment for the majority of Becker nevi. However, the dark brown color is less obvious if the affected area is kept out of the sun so that it doesn’t tan.
The excessive hairs can be reduced by repeated treatments with a hair removal laser or by electrolysis. The pigmentation can be reduced by a pigment laser, but this is not always effective and it may also be made worse by laser treatment.
Becker nevus-associated acne can be treated with standard acne therapies, including in severe cases, oral isotretinoin.
Q-switched ruby laser (694 nm) has been used with variable success in the treatment of both the hypertrichosis and hyperpigmentation of Becker’s nevus 11. Histopathologic analysis of lesional skin after laser treatment showed selective damage of superficially located melanocytes but a persistence of adnexal melanocytes. Remaining pigment cells may account for the transient improvement noted clinically.
A prospective study 12 demonstrated the superiority of an erbium:YAG laser (n= 11) over a Q-switched neodymium:YAG system (n = 11) in the treatment of Becker nevus. Evaluation 2 years after treatment showed that 54% of subjects treated with the erbium:YAG laser showed complete clinical clearance, while a clearance of greater than 50% occurred in 100% of the subjects. By comparison, none of the patients who received 3 treatments with the neodymium:YAG laser system cleared completely and only one person had marked improvement. Supporting evidence for the role of the 2940-nm erbium:YAG laser in the treatment of Becker nevus comes from a small case series from Saudi Arabia 13. Using this device, seven patients completed a single split-lesion treatment with follow-up to a year. All patients experienced some decrease in pigmentation in the range of 25-75%. Although the authors reported no hyperpigmentation or repigmentation, images from the paper show persisting depigmentation in the test areas performed prior to the full intervention in several of the subjects 13.
A long-pulsed 755-nm alexandrite laser was evaluated in 11 Korean patients with Becker’s nevus 14. Two patients had excellent responses, 5 had good responses, and 4 had fair responses. Hair density simultaneously decreased with treatment in all patients. Fifteen patients with Becker’s nevus underwent 8 sessions of hair removal with low-fluence, high-repetition-rate diode lasers (808-810 nm) 15. All participants experienced significant hair reduction at 6 and 12 months, with no adverse events reported.
Eleven adult patients with Becker’s nevus were included in a prospective, randomized, controlled, observer-blinded, split-lesion trial. In each patient, 2 similar square test regions were randomized to either ablative factional laser therapy at 10 mJ/microbeam, coverage 35-45%, and topical bleaching (to reduce laser-induced post-inflammatory hyperpigmentation), or topical bleaching alone. Treatment was moderately effective in some patients. However, postinflammatory hyperpigmentation and relatively negative patient-reported outcomes still preclude ablative fractional laser therapy from being a standard therapy 16. These results have been observed by this author, and the concern of both postinflammatory hyperpigmentation and hypopigmentation should be discussed with the patient prior to treatment.
In 2016, three patients with Becker nevus (two hypertrichotic) were treated using a combination approach with a 1550-nm erbium-doped nonablative fractional laser and a long-pulsed 1064-nm neodymium:YAG laser in a sequential manner over time 17. Although these individuals had a clinical improvement of greater than 75%, follow up was limited (3-18 months). Patients should be advised that over time (months to several years), pigment may recur at the treated site.
In sum, laser treatment of Becker’s nevus yields variable results and further studies are needed to determine the best way to reduce the appearance of these lesions without causing post laser dyschromia or scarring 18.
References- Becker naevus. https://dermnetnz.org/topics/becker-naevus
- Becker Melanosis. https://emedicine.medscape.com/article/1068257-overview
- BECKER NEVUS SYNDROME. https://omim.org/entry/604919
- Grande Sarpa H, Harris R, Hansen CD, Callis Duffin KP, Florell SR, Hadley ML. Androgen receptor expression patterns in Becker’s nevi: an immunohistochemical study. J Am Acad Dermatol. 2008 Nov. 59(5):834-8.
- Fretzin DF, Whitney D. Familial Becker’s nevus. J Am Acad Dermatol. 1985 Mar. 12(3):589-90.
- Sirka CS, Puhan MR, Behera S, Mohanty P, Nanda M. Becker’s nevus with ipsilateral breast hypoplasia. Indian J Dermatol Venereol Leprol. 2009 Mar-Apr. 75(2):202-3.
- Van Gerwen HJ, Koopman RJ, Steijlen PM, Happle R. Becker’s naevus with localized lipoatrophy and ipsilateral breast hypoplasia. Br J Dermatol. 1993 Aug. 129(2):213.
- Lambert JR, Willems P, Abs R, Van Roy B. Becker’s nevus associated with chromosomal mosaicism and congenital adrenal hyperplasia. J Am Acad Dermatol. 1994 Apr. 30(4):655-7.
- Urbani CE, Betti R. Polythelia within Becker’s naevus. Dermatology. 1998. 196(2):251-2.
- Szylit JA, Grossman ME, Luyando Y, Olarte MR, Nagler H. Becker’s nevus and an accessory scrotum. A unique occurrence. J Am Acad Dermatol. 1986 May. 14(5 Pt 2):905-7.
- Raulin C, Schönermark MP, Greve B, Werner S. Q-switched ruby laser treatment of tattoos and benign pigmented skin lesions: a critical review. Ann Plast Surg. 1998 Nov. 41(5):555-65.
- Trelles MA, Allones I, Moreno-Arias GA, Vélez M. Becker’s naevus: a comparative study between erbium: YAG and Q-switched neodymium:YAG; clinical and histopathological findings. Br J Dermatol. 2005 Feb. 152(2):308-13.
- Al-Saif F, Al-Mekhadab E, Al-Saif H. Efficacy and safety of short-pulse erbium: Yttrium aluminum garnet laser treatment of Becker’s nevus in Saudi patients: A pilot study. Int J Health Sci (Qassim). 2017 jul-sep. 11(3):14-17.
- Choi JE, Kim JW, Seo SH, Son SW, Ahn HH, Kye YC. Treatment of Becker’s nevi with a long-pulse alexandrite laser. Dermatol Surg. 2009 Jul. 35(7):1105-8.
- Lapidoth M, Adatto M, Cohen S, Ben-Amitai D, Halachmi S. Hypertrichosis in Becker’s nevus: effective low-fluence laser hair removal. Lasers Med Sci. 2014 Jan. 29(1):191-3.
- Meesters AA, Wind BS, Kroon MW, Wolkerstorfer A, van der Veen JP, Nieuweboer-Krobotová L. Ablative fractional laser therapy as treatment for Becker nevus: a randomized controlled pilot study. J Am Acad Dermatol. 2011 Dec. 65(6):1173-9.
- Balaraman B, Friedman PM. Hypertrichotic Becker’s nevi treated with combination 1,550 nm non-ablative fractional photothermolysis and laser hair removal. Lasers Surg Med. 2016 Apr. 48 (4):350-3.
- Momen S, Mallipeddi R, Al-Niaimi F. The use of lasers in Becker’s naevus: An evidence-based review. J Cosmet Laser Ther. 2016 Aug. 18 (4):188-92.