Bennett’s fracture
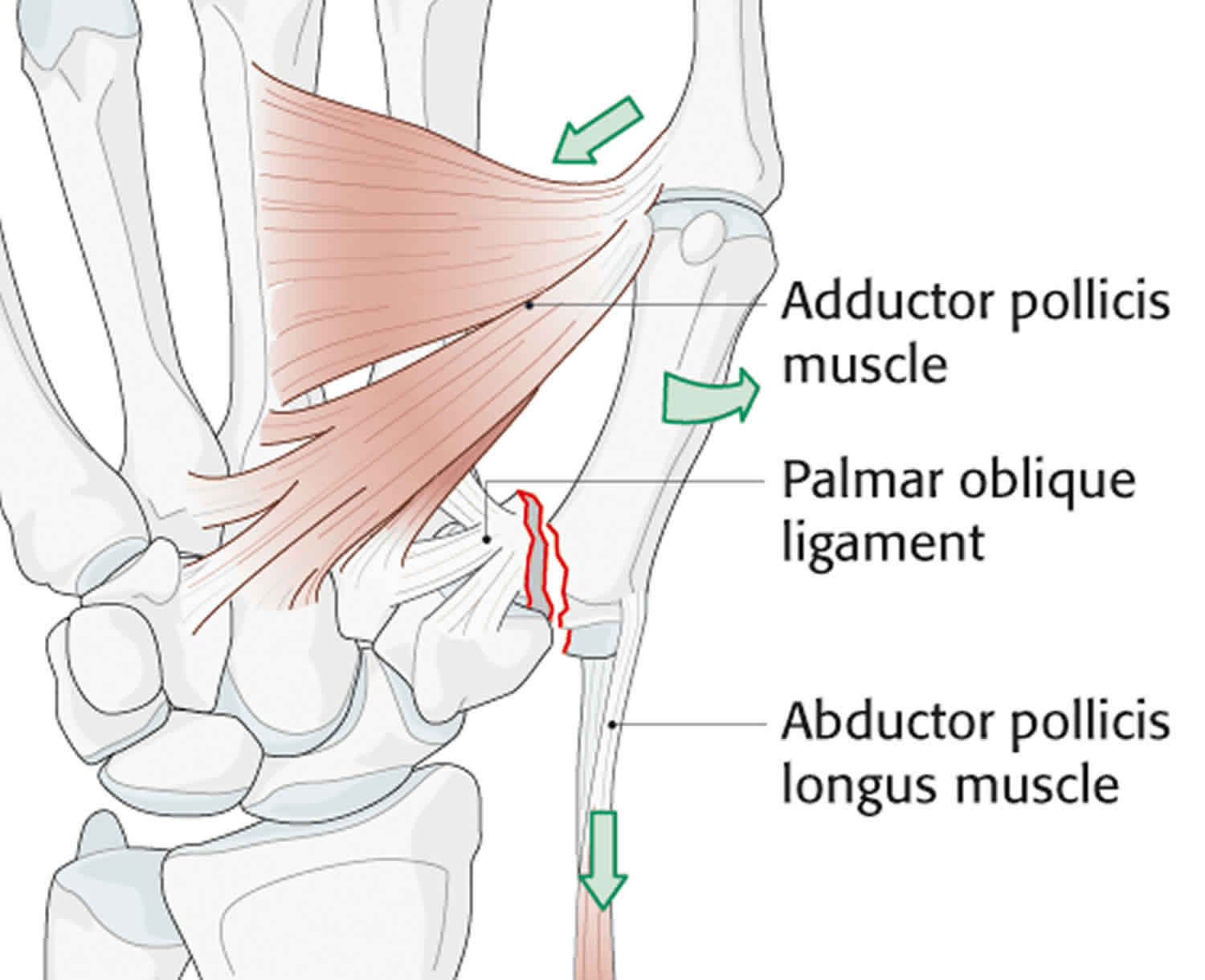
Bennett fracture is a fracture of the base of the thumb resulting from forced abduction of the first metacarpal. Bennett’s fracture is defined as an intra-articular two-part fracture of the base of the first metacarpal bone separating the volar-ulnar aspect of the metacarpal base from the remaining distal metacarpal shaft 1. Thumb carpometacarpal joint stability is maintained by five ligaments and the articular contours. The most critical of these stabilizers is the volar oblique ligament. This ligament courses from the volar lip of the trapezium to the volar ulnar corner of the thumb metacarpal base. The anterior (volar)-ulnar fragment is held in place via the volar anterior oblique ligament, while the large distal fragment is retracted proximally due to the tension from the abductor pollicis tendon 2. The portion of the metacarpal onto which the volar oblique ligament inserts remains in anatomic position, and the remainder of the articular base subluxates in a dorsal, radial, and proximal direction because of the pull of the abductor pollicis longus. Unless properly recognized and treated, Bennett’s fracture (intra-articular fracture subluxation of the first metacarpal bone) may result in an unstable arthritic joint with secondary loss of motion and pain. Because the thumb carpometacarpal joint is critical for pinch and opposition, this injury may severely affect function.
Treatment for Bennett’s fracture depends on whether the broken ends of the bone are displaced. This means that they have moved away from each other. Bennett fracture treatment algorithm is also influenced by the age and profession/hobbies of the patient.
- Non-operative treatment in a thumb spica cast for 3-4 weeks can be considered in stable, non-displaced Bennett’s fractures.
- Operative treatment is recommended for unstable Bennett’s fracture patterns and intra-articular displacement of >1 mm. While open reduction and internal fixation with a screw or Kirschner wire (K-wire) are both common practice, screws are often preferred as Kirschner wires (K-wires) must be removed after union.
Untreated or malreduced Bennett’s fractures can lead to secondary osteoarthritis. Osteoarthritis or malunion can cause significant pain and functional decline.
Treatment often includes reduction of the fracture. This involves moving the broken pieces of bone back into alignment with each other. It also involves moving the bone back into the carpometacarpal joint.
Closed reduction is done without making any incisions. You are given medicine to prevent pain. The provider then moves the bones back into place from outside the skin. In many cases, the provider puts pins through tiny incisions to hold the reduction in place.
Open reduction is done using surgery. You are given medicine to prevent pain and make you sleep. The provider makes Incisions in the skin. He or she then moves the bones back into place. Removable pins or screws are used to hold the bones in place while they heal.
After the reduction:
- A cast or splint is put on your hand to keep the thumb from moving while the bones heal.
- You will be given medicines to help control pain and swelling.
- You will be told to ice and elevate your hand to help control pain and swelling.
- After healing, stretching and strengthening exercises can help regain full use of the thumb and hand.
Bennett’s fracture key points
- Bennett fractures put the patient at significant risk of future morbidity if inadequately treated (including continual dislocation/subluxation, malunion and an increase in osteoarthritis due to incongrual articular surfaces related to inaccurate reduction).
- Methods of treating Bennett fractures include closed reduction with or without percutaneous Kirschner wiring, and open reduction and internal fixation. The most important aspect of treatment is anatomic reduction and maintenance of this until union.
- Studies suggest that open reduction andinternal fixation is associated with more reliable reduction and better long term outcomes, however, this technique is technically demanding. These fractures should therefore be referred to a specialist hand surgeon for definitive management in a timely fashion after initial imaging and immobilisation.
Thumb anatomy
The thumb has two bones. The first bone (distal phalange) extends from the tip of the thumb to the knuckle. The second bone (proximal phalange) extends from the knuckle to the base of the thumb. This is the area of webbing between the thumb and the first finger. The thumb connects with a bone in the hand (first metacarpal), which articulates with the trapezium bone in the distal carpal row.
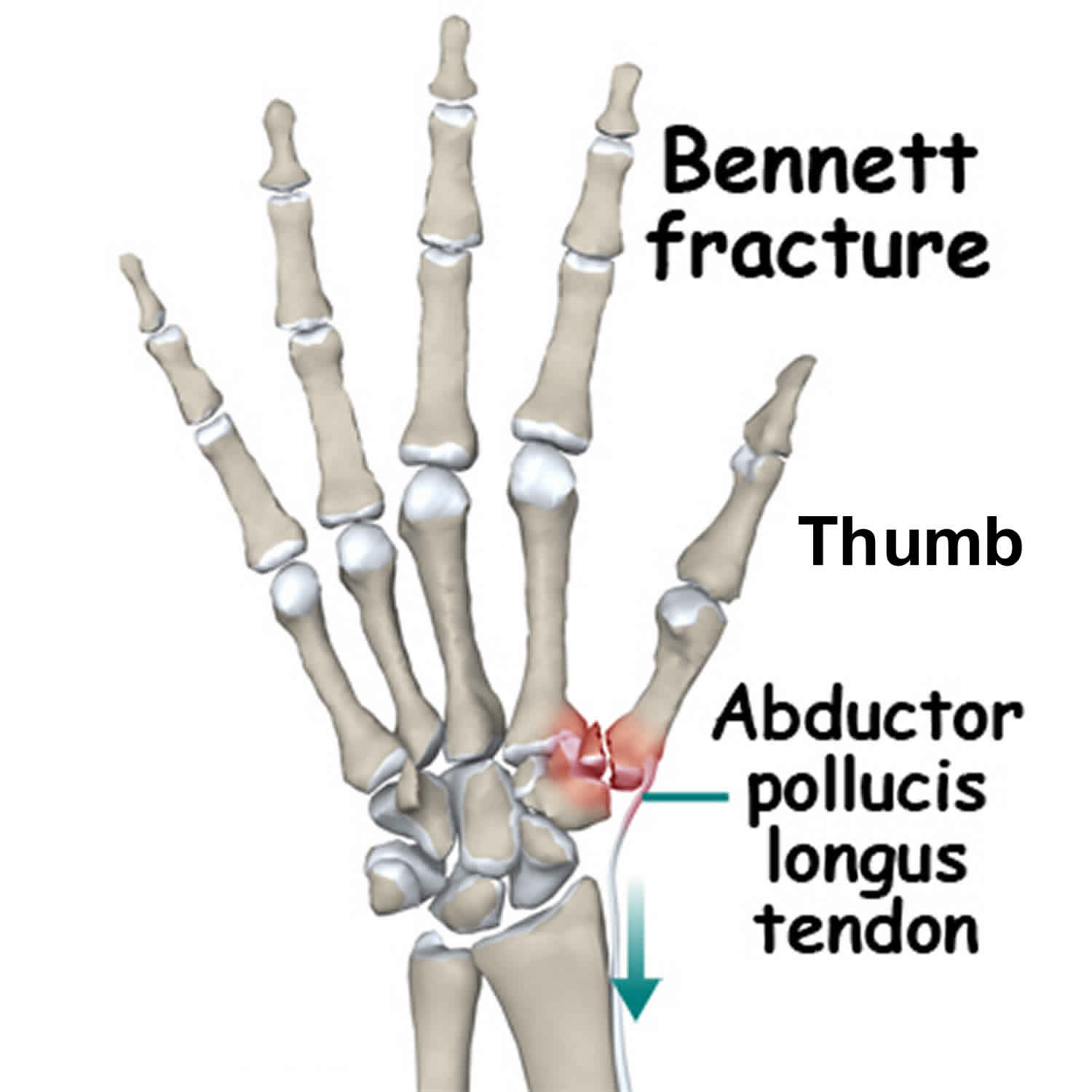
The first carpometacarpal joint is unique in that it includes only an articulation between the trapezium and the base of the first metacarpal. The first carpometacarpal joint is completely isolated from the rest of the carpometacarpal joints of the hand. The articulation is saddle-shaped which allows greater motion, but consequently there is less inherent stability from the bony anatomy. Ligamentous stability at the trapeziometacarpal joint is maintained by the anterior (volar) and posterior oblique ligaments, the anterior and posterior intermetacarpal ligaments, and the dorsal radial ligament. The anterior (volar) oblique ligament originates on the trapezium and inserts into the volar ulnar beak of the thumb metacarpal. This is the most important ligament in maintaining carpometacarpal stability. The dorsal ligament is not as strong as the volar ligament but is reinforced by the abductor pollicis longus. Of significance in Bennett fracture is the volar oblique ligament, or beak ligament, which inserts at the base of the first metacarpal and opposes the action of the abductor pollucis longus 3. When a fracture occurs this opposing action is interrupted, an intra-articular fracture propagates separating a fragment which remains attached to this strong ligament and the pull of the abductor pollucis longus dislocates the remaining base of the thumb metacarpal 4. Figure 1 illustrates the anatomy of a Bennett fracture.
Figure 1. Bennett fracture
Bennett’s fracture causes
Bennett fracture occurs when an axial force is transmitted through a partially flexed thumb metacarpal 5. Most Bennett fractures are caused by indirect forces such as falling on an extended or abducted thumb or an impact onto a clenched fist. Many attribute these fractures to punching, in which the flexed and adducted thumb strikes the opponent’s head or jaw 6. However, the incidence from falls, motor vehicle accidents and work injuries appear similar 4.
Bennett fracture accounts for around one-third of all fractures of the first metacarpal in adults. The fracture predominates in adult males and usually occurs in the dominant hand 3.
Bennett’s fracture symptoms
Symptoms of Bennett’s fracture include:
- Severe pain and weakness of the thumb
- Swelling of the base of the thumb and back of the hand
- Bruising
- Misalignment of the thumb
- Trouble moving the thumb
Patients with Bennett fracture present with swelling and pain at the thumb base and loss of function of the first carpometacarpal joint. Acutely this is always accompanied by haematoma and inflammation. Tenderness to palpation will be present over the proximal part of the first metacarpal. Decreased function will be present including reduced power in the thumb, inability to grip, weakness in pincer grip and reduced range of motion. Occasionally the thumb will appear shortened, and careful examination will reveal bony crepitus 6.
Bennett’s fracture complications
Complications of Bennett’s fracture include:
- Bones not healing or healing in a bad position
- Continued pain in the thumb or hand
- Continued weakness in the thumb or hand
- Stiffness of the thumb joint
- Arthritis
Bennett’s fractures predispose the patient to arthritis and loss of motion within the affected joints. Unfortunately, even after restoration of articular congruity, some patients develop posttraumatic arthritis secondary to the osteocartilaginous injury sustained as a result of the initial trauma.
Loss of motion also occurs following prolonged immobilization. Rigid fixation enables patients to initiate movement sooner postoperatively, minimizing this problem.
Other potential postoperative complications include loss of reduction with recurrent joint subluxation and instability, infection, and sensory nerve injury.
Bennett’s fracture diagnosis
On examination, motion is limited and carpometacarpal joint instability is frequently noted with gentle stress of the thumb metacarpal. If fracture is suspected plain film radiographs should be performed requesting views of the thumb 7. Traction radiography may be used to assess the degree of comminution in appropriate fractures (eg, Bennett, Rolando, comminuted metacarpal base fractures).
It is also important to remember that in cases where the injury has occurred due to trauma, patients should be examined appropriately to ensure they have not suffered any other injuries.
Bennett’s fracture treatment
Bennett fractures may be treated conservatively with closed reduction and plaster casting, closed reduction and percutaneous Kirschner wire (K-wire) fixation or via open reduction and internal fixation (ORIF). Each treatment modality has advantages and disadvantages and each requires significant expertise.
The major issue in closed reduction is to obtain and then maintain adequate fracture reduction to allow healing in an anatomical position. consequences of inadequate fracture reduction in the short term are pain and grip weakness and in the long term, osteoarthritis of the first carpometacarpal joint 8. For this reason these fractures should only be treated by specialist hand surgeons given the risk of future disability associated with inadequate reduction.
There are a number of methods of closed reduction. All of which involve traction on the thumb to pull the metacarpal distally with concurrent gentle pressure pushing the metacarpal base medially to return it to anatomical position 3.
The most basic method of closed reduction is reduction of Bennett’s fracture under adequate analgesia/sedation followed by plaster cast immobilization for up to 6 weeks. Most early methods of closed reduction recommended a plaster slab holding the thumb in radial abduction. However cadaveric studies with simulated Bennett fractures suggested a cast with the thumb in a position of moderate adduction and opposition better reduced the fracture fragments 9.
A second method of reduction described by Wagner involves reduction of the fracture followed by percutaneous insertion of a Kirschner wire through the base of the metacarpal across the joint and into the trapezium to hold the reduction in place 8. This wire remains in place for a period of around 4 weeks, at which time the wire is removed and a rehabilitation program is started.
Spangberg and Thoren 10 described another method in which a Kirschner wire is placed into the distal metacarpal fragment and then traction is exerted on this wire via a frame and rubber bands to reduce the fracture and maintain this position.
Medium term follow up studies by Griffiths 11 and Cannon et al 12 have shown good functional results in patients treated conservatively. However, a long term follow up study by Livesley 13 in which patients were followed for an average of 26 years found a high incidence of joint degeneration and functional problems. Livesley suggested that conservative management should not be advocated 13.
Bennett’s fracture surgery
Generally, closed reduction utilizing the technique described above followed by percutaneous Kirschner wire (K-wire) fixation is successful.
If adequate reduction cannot be achieved by means of this percutaneous technique, open reduction and internal fixation (ORIF) is performed. Open reduction involves opening up the fracture and reduction under direct vision followed by insertion of either Kirschner wires or lag screws in order to hold the reduction in place. All methods of open reduction are followed by treatment in a plaster slab for up to 4 weeks.
An L-shaped incision is made over the subcutaneous border of the thumb metacarpal. The incision is carried down radially to allow subperiosteal reflection of the thenar musculature and direct visualization of the joint. Towel-clip forceps are extremely valuable in obtaining and temporarily maintaining reduction. Fixation is achieved by using either K-wires or mini-screws (2.0 mm) 14.
Many studies have shown unsatisfactory reduction using closed methods 15. Contrasted with this are a number of studies which show a much higher percentage of patients with satisfactory reduction using ORIF 9. Thurston and Dempsey 16 suggested that the best results were achieved in reductions where there was a residual displacement of less than 1 mm. They found that the method used was not important, however it was more reliably achieved through ORIF.
Zhang et al 17 reported success with open tension band wiring as a fixation option for the treatment of Bennett fractures. Mahmoud et al 18 reported good results from performing ORIF of Bennett fractures in young, active manual laborers, using a K-wire and wire loop construct to achieve anatomic reduction. Arthroscopically assisted percutaneous screw fixation has been described 19.
Bennett’s fracture rehabilitation
Rehabilitation involves early mobilization of interphalangeal joints at 2–3 weeks or when K-wires are removed if used 20. With internal fixation, return to work or in the case of athletes, progressive training – can be expected at around 4–6 weeks or when the fracture is nontender and shows radiological evidence of union, incorporating the aid of hand therapy (progressive active and passive range of motion therapy) and splintage (generally with a shortened hand based opponens splint) with the advice of the treating surgeon 7.
Bennett’s fracture prognosis
The prognosis for Bennett fractures is most closely related to the amount of energy associated with the original injury. High-energy injuries produce comminution, articular surface damage, and extensive soft-tissue injury, leading to a poor outcome. With anatomic restoration of the joint surface and reestablishment of stability, the outcome is routinely good, especially in low-energy injuries with simple fracture patterns and limited soft-tissue involvement.
References- Carlsen BT, Moran SL. Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. J Hand Surg [Am] 2009;34(5):945–52. doi: 10.1016/j.jhsa.2009.03.017
- Brownlie C, Anderson D. Bennett fracture dislocation—review and management. Aust Fam Physician. 2011;40(6):394–6.
- Dial WB, Berg E. Bennett fracture. Hand 1972;4:229–35.
- Pollen AG. The conservative treatment of Bennett fracture – subluxation of the thumb metacarpal. J Bone Joint Surg 1968;50B:91–101.
- Carlsen BT, Moran SL. Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. J Hand Surg Am. 2009 May-Jun. 34 (5):945-52.
- Apley AG, Solomon L. Apley’s system of orthopaedics and fractures. 6th edn. London: Butterworth and Co, 1982, p. 411–2.
- Carlsen BT, Moran SL. Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. J Hand Surg Am 2009;34A:945–52.
- Lutz M, Sailer R, Zimmermann R, Gabi M, Ulmer H, Pechlaner S. Closed reduction transarticular kirschner wire fixation versus open reduction internal fixation in the treatment of Bennett fracture dislocation. J Hand Surg Br 2003;28B:142–7.
- Harvey FJ, Bye WD. Bennett fracture. Hand 1976;8:48–53.
- Wagner CJ. Method of treatment of Bennett fracture dislocation. Am J Surg 1950;80:230–1.
- Griffiths JC. Fractures at the base of the first metacarpal bone. J Bone Joint Surg 1964;46B:712–9.
- Cannon SR, Dowd GSE, Williams DH, Scott JM. A long term study following Bennett fracture. J Hand Surg 1986;11B:426–31.
- Livesley PJ. The conservative management of Bennett fracture-dislocation: a 26 year follow-up. J Hand Surg 1990;15B:291–4.
- Day CS. Fractures of the metacarpals and phalanges. Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, eds. Green’s Operative Hand Surgery. 7th ed. Philadelphia: Elsevier; 2017. Vol 1: 231-77.
- Kjaer-Petersen K, Langhoff O, Andersen K. Bennett fracture. J Hand Surg Br 1990;15B:58–61.
- Thurston AJ, Dempsey SM. Bennett fracture: a medium to long-term review. Aust N Z J Surg 1993;63:120–3.
- Zhang X, Shao X, Zhang Z, Wen S, Sun J, Wang B. Treatment of a Bennett fracture using tension band wiring. J Hand Surg Am. 2012 Mar. 37 (3):427-33.
- Mahmoud M, El Shafie S, Menorca RM, Elfar JC. Management of neglected Bennett fracture in manual laborers by tension fixation. J Hand Surg Am. 2014 Sep. 39 (9):1728-33.
- Solomon J, Culp RW. Arthroscopic Management of Bennett Fracture. Hand Clin. 2017 Nov. 33 (4):787-794.
- McNemar TB, Howell JW, Chang E. Management of metacarpal fractures. J Hand Ther 2003;16:143–51.