Bernard-Soulier syndrome
Bernard-Soulier syndrome also called giant platelet syndrome, is a rare inherited bleeding disorder associated with abnormal platelets, which are blood cell fragments involved in blood clotting (coagulation). In affected individuals, platelets are unusually large and fewer in number than usual (a combination known as macrothrombocytopenia) and have prolonged bleeding time (difficulty in clotting). People with Bernard-Soulier syndrome tend to bruise easily and tend to bleed excessively with an increased risk of nosebleeds (epistaxis). They may also experience abnormally heavy or prolonged bleeding following minor injury or surgery or even without trauma (spontaneous bleeding). In some affected individuals, bleeding under the skin causes tiny red or purple spots on the skin called petechiae. Women with Bernard-Soulier syndrome often have heavy or prolonged menstrual periods (menorrhagia).
Bernard-Soulier syndrome is a rare bleeding disorder that estimated to occur in 1 in 1 million individuals; however, some doctors think the condition is underdiagnosed and may be more common 1. Bernard-Soulier syndrome affects males and females in equal numbers. More than 200 cases have been reported worldwide. To date, Bernard-Soulier syndrome has been described primarily in whites of European ancestry, as well as in the Japanese population; its prevalence in other ethnic groups is unknown.
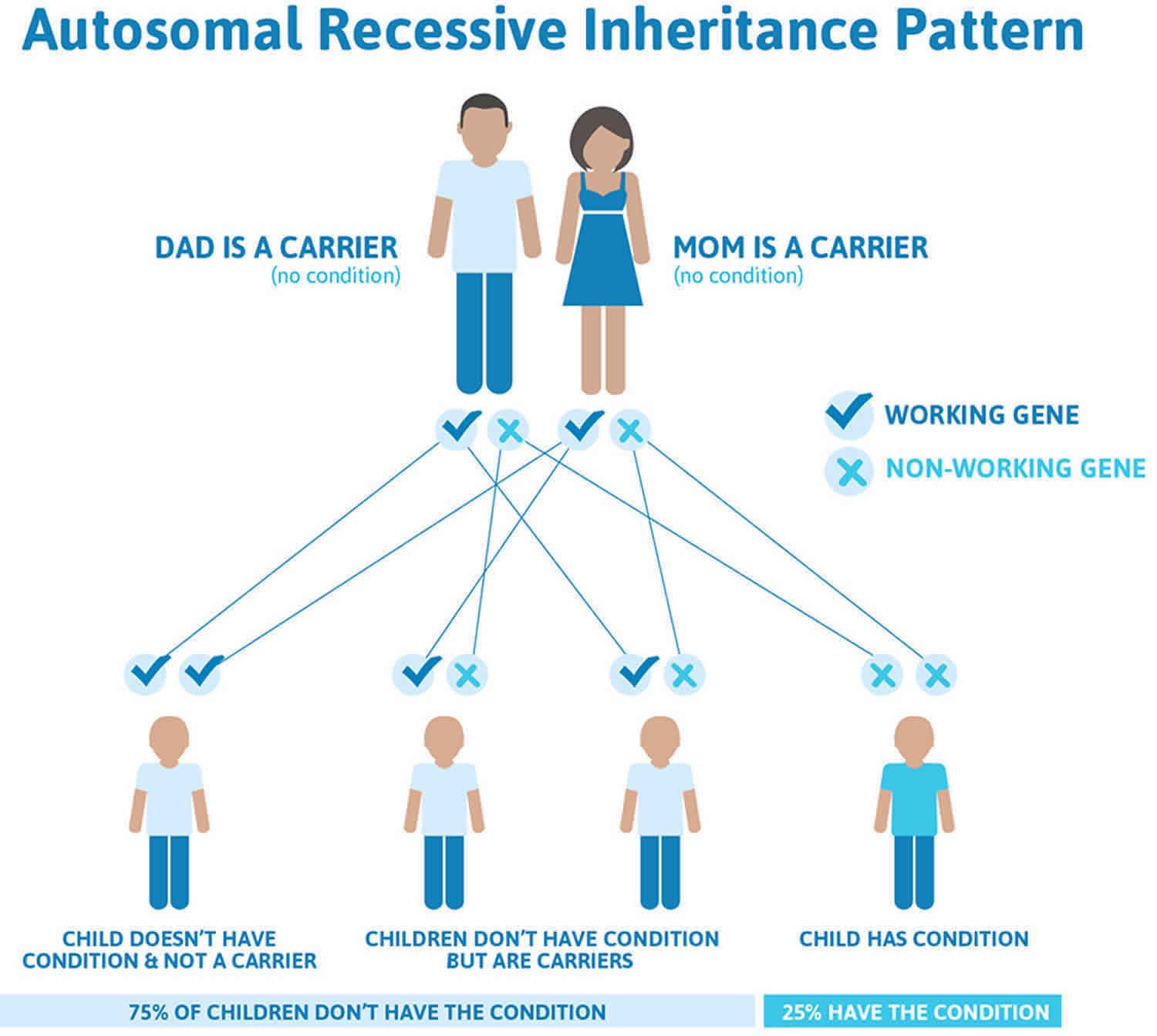
Most cases of Bernard-Soulier syndrome are inherited in an autosomal recessive genetic pattern.
Bernard-Soulier syndrome causes
Bernard-Soulier syndrome is caused by mutations in one of three genes: GP1BA, GP1BB, or GP9. The proteins produced from these genes are pieces (subunits) of a protein complex called glycoprotein (GP)Ib-IX-V. This complex is found on the surface of platelets and plays an important role in blood clotting.
The GPIb-IX-V complex can attach (bind) to a protein called von Willebrand factor, fitting together like a lock and its key. Von Willebrand factor is found on the inside surface of blood vessels, particularly when there is an injury. Binding of the GPIb-IX-V complex to von Willebrand factor allows platelets to stick to the blood vessel wall at the site of the injury. These platelets form clots, plugging holes in the blood vessels to help stop bleeding.
Most mutations in GP1BA, GP1BB, or GP9 prevent the formation of the GPIb-IX-V complex on the surface of platelets. Other mutations impair the complex’s interaction with von Willebrand factor. All of these mutations impair clot formation, which leads to the excessive bleeding characteristic of Bernard-Soulier syndrome.
Bernard-Soulier syndrome inheritance pattern
Most cases of Bernard-Soulier syndrome are inherited in an autosomal recessive pattern, which means both copies of the GP1BA, GP1BB, or GP9 gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene. Although most people with only one copy of the mutated gene do not show signs and symptoms of the condition, some have platelets that are slightly larger than normal or very mild bleeding abnormalities. The risk for two carrier parents to both pass the abnormal gene and, therefore, have an affected child is 25% with each pregnancy. The risk to have a child who is a carrier, like the parents, is 50% with each pregnancy. The chance for a child to receive normal genes from both parents is 25%. The risk is the same for males and females.
Rare cases of Bernard-Soulier syndrome caused by mutations in the GP1BA or GP1BB gene are inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. These individuals inherit the condition from an affected parent.
Figure 1. Bernard-Soulier syndrome autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Bernard-Soulier syndrome symptoms
The symptoms of Bernard-Soulier syndrome, which are typically apparent at birth and continue throughout life, may include the tendency to bleed excessively from cuts and other injuries, nosebleeds (epistaxis), and/or an unusually heavy menstrual flow in women. Some babies and children with BSS have no symptoms and the disorder does not present until adult life. People with this disease also bruise easily and the bruises tend to linger. Bleeding from very small blood vessels under the skin (subcutaneous) may cause small or widespread areas of small red or purple colored spots (purpura or petechiae).
Bernard-Soulier syndrome diagnosis
The diagnosis of Bernard-Soulier syndrome is made by a combination of blood testing to reveal whether platelets are at abnormally low levels (thrombocytopenia), microscopic examination to determine the presence of abnormally large platelets and irregularly shaped platelets, and a test called ‘flow cytometry, which is able to measure the level of expression of the missing protein ion the outside of platelets affected by Bernard-Soulier syndrome. In recent years, most families are offered molecular genetic testing to identify which gene carries the mutations.
Bernard-Soulier syndrome treatment
Platelet transfusion is used to treat Bernard-Soulier syndrome when surgery is necessary or when there is a risk for life-threatening hemorrhage. Some patients with Bernard-Soulier syndrome become resistant (refractory) to platelet transfusions because they develop antibodies against the GPIb protein- to reduce this risk it is now recommended that specially selected platelet transfusions (from HLA-matched single donors) should be used. Where HLA-matched platelets are not available, leucocyte-depleted platelets can be used (these are platelet transfusions from which contaminating white blood cells-leucocytes- have been removed). People with this disorder should not take aspirin or other related drugs because these medications affect the blood’s ability to clot (platelet aggregation). It is suggested that acetaminophen, which is present in medications such as Tylenol, is used for the relief of mild pain. Antifibrinolytic agents (drugs which delay the breakdown of blood clots) are often useful to help reduce bleeding after minor surgery (eg dental surgery) or for prolonged nosebleeds. The most commonly used antifibrinolytic drug is tranexamic acid (also known as epsilon aminocaproic acid).
Desmopressin acetate (DDAVP) has been shown to shorten bleeding time in some, but not all, patients with Bernard-Soulier syndrome. It may be useful for minor bleeding episodes.
More recently, recombinant activated factor VII and hematopoietic stem cell transplantation have been used in patients with congenital platelet disorders including Bernard-Soulier syndrome.
Genetic counseling is recommended for people with Bernard-Soulier syndrome and their families. Other treatment is symptomatic and supportive.
References