Best time to get pregnant
You’re most likely to get pregnant if you have sex within a day or so of ovulation (releasing an egg from the ovary). This is usually about 14 days after the first day of your last period, if your cycle is around 28 days long. An egg lives for about 12-24 hours after being released. For pregnancy to happen, the egg must be fertilized by a sperm within this time. Sperm can live for up to 7 days inside a woman’s body. So if you’ve had sex in the days before ovulation, the sperm will have had time to travel up the fallopian tubes to “wait” for the egg to be released. When the egg and sperm meet, it’s called fertilization. The fertilized egg also called an embryo moves through your fallopian tubes and attaches to the wall of your uterus where it grows and develops into a baby. When the embryo attaches to the uterus, it’s called implantation.
To get pregnant:
- A woman’s body must release an egg from one of her ovaries (ovulation).
- A man’s sperm must join with the egg along the way (fertilize).
- The fertilized egg must go through a fallopian tube toward the uterus (womb).
- The fertilized egg must attach to the inside of the uterus (implantation).
- Infertility may result from a problem with any or several of these steps.
- If you want to get pregnant, having sex every 2 to 3 days throughout the month will give you the best chance. You don’t need to time having sex only around ovulation.
Getting pregnant (conception) happens when a man’s sperm fertilizes a woman’s egg. For some women this happens quickly, but for others it can take longer.
You can get pregnant if you have unprotected sex any time from 5 days before and the day of ovulation. The more often you have sex during this time, the more likely you are to get pregnant. Your egg is fertile (can become an embryo) for 12 to 24 hours after ovulation. Your partner’s sperm can live inside you for up to 72 hours after you have sex.
However, it’s difficult to know exactly when your ovulation happen, unless you are practising natural family planning, or fertility awareness.
Out of every 100 couples trying for a baby, 80 to 90 will get pregnant within 1 year. The rest will take longer, or may need help to conceive.
To understand getting pregnant (conception) and pregnancy, it helps to know about the male and female sexual organs, and to understand how a woman’s monthly menstrual cycle and periods work.
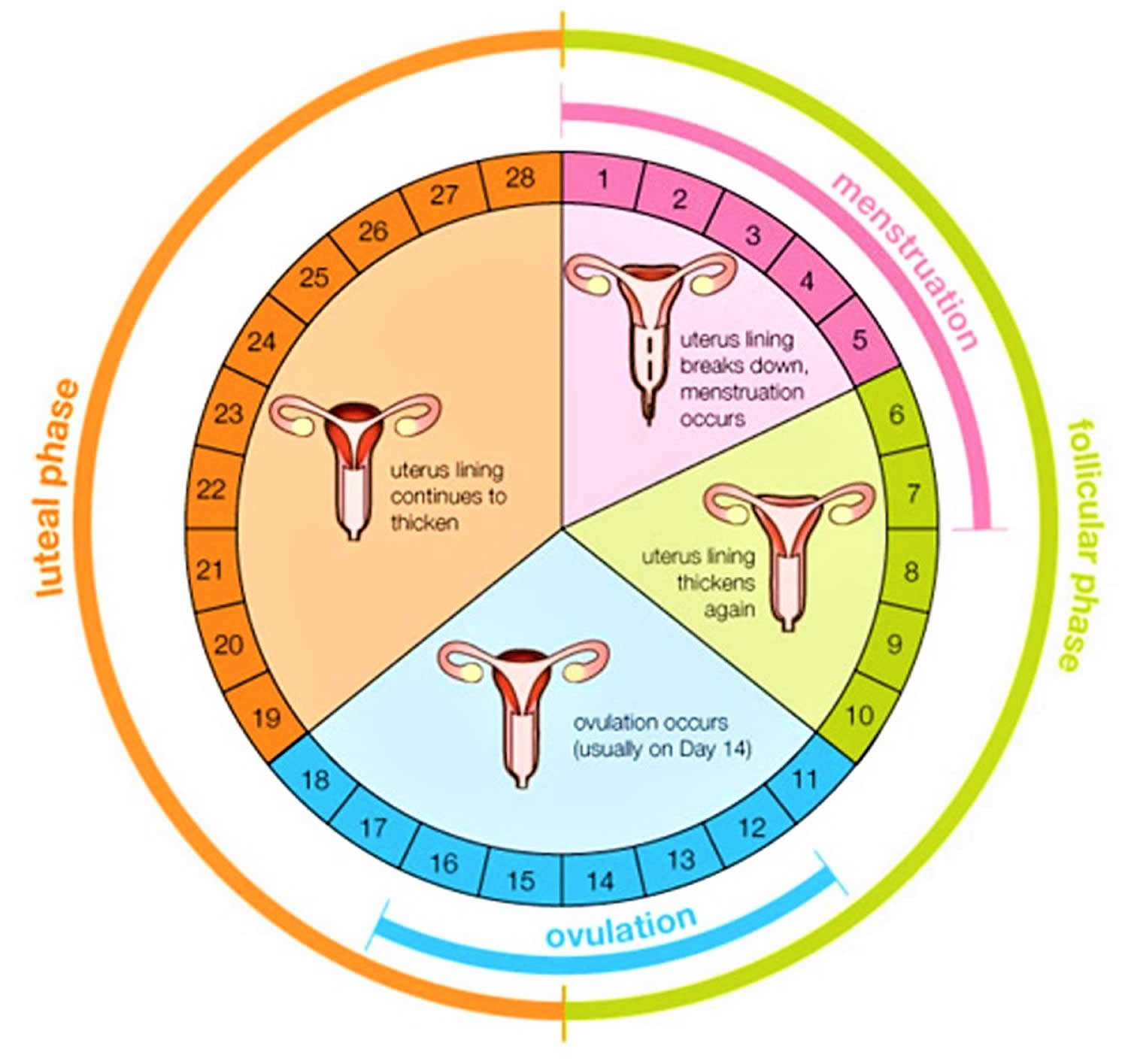
The menstrual cycle is counted from the first day of a woman’s period (day 1). Some time after her period she will ovulate, and then around 12-16 days after this she’ll have her next period.
The average menstrual cycle lasts 28 days. But normal cycles can vary from 21 to 35 days. The amount of time before ovulation occurs is different in every woman and even can be different from month to month in the same woman, varying from 13 to 20 days long. Learning about this part of the cycle is important because it is when ovulation and pregnancy can occur. After ovulation, every woman (unless she has a health problem that affects her periods or becomes pregnant) will have a period within 14 to 16 days.
Being aware of your menstrual cycle and the changes in your body that happen during this time can help you know when you are most likely to get pregnant. See how the menstrual cycle works by watching the video below. Each month your ovaries release an egg about 14 days before the first day of your period. This is called ovulation. When you and your partner have unprotected sex around the time of ovulation, his sperm swim to meet your egg. Unprotected sex means you don’t use any kind of birth control to help prevent pregnancy.
The male sexual organs
- The penis: this is made of sponge-like erectile tissue that becomes hard when filled with blood.
- Testes: men have two testes (testicles), which are glands where sperm are made and stored.
- Scrotum: this is a bag of skin outside the body beneath the penis. It contains the testes and helps to keep them at a constant temperature just below body temperature. When it’s warm, the scrotum hangs down, away from the body, to help keep the testes cool. When it’s cold, the scrotum draws up, closer to the body for warmth.
- Vas deferens: these are two tubes that carry sperm from the testes to the prostate and other glands.
- Prostate gland: this gland produces secretions that are ejaculated with the sperm.
- Urethra: this is a tube that runs down the length of the penis from the bladder, through the prostate gland to an opening at the tip of the penis. Sperm travel down this tube to be ejaculated.
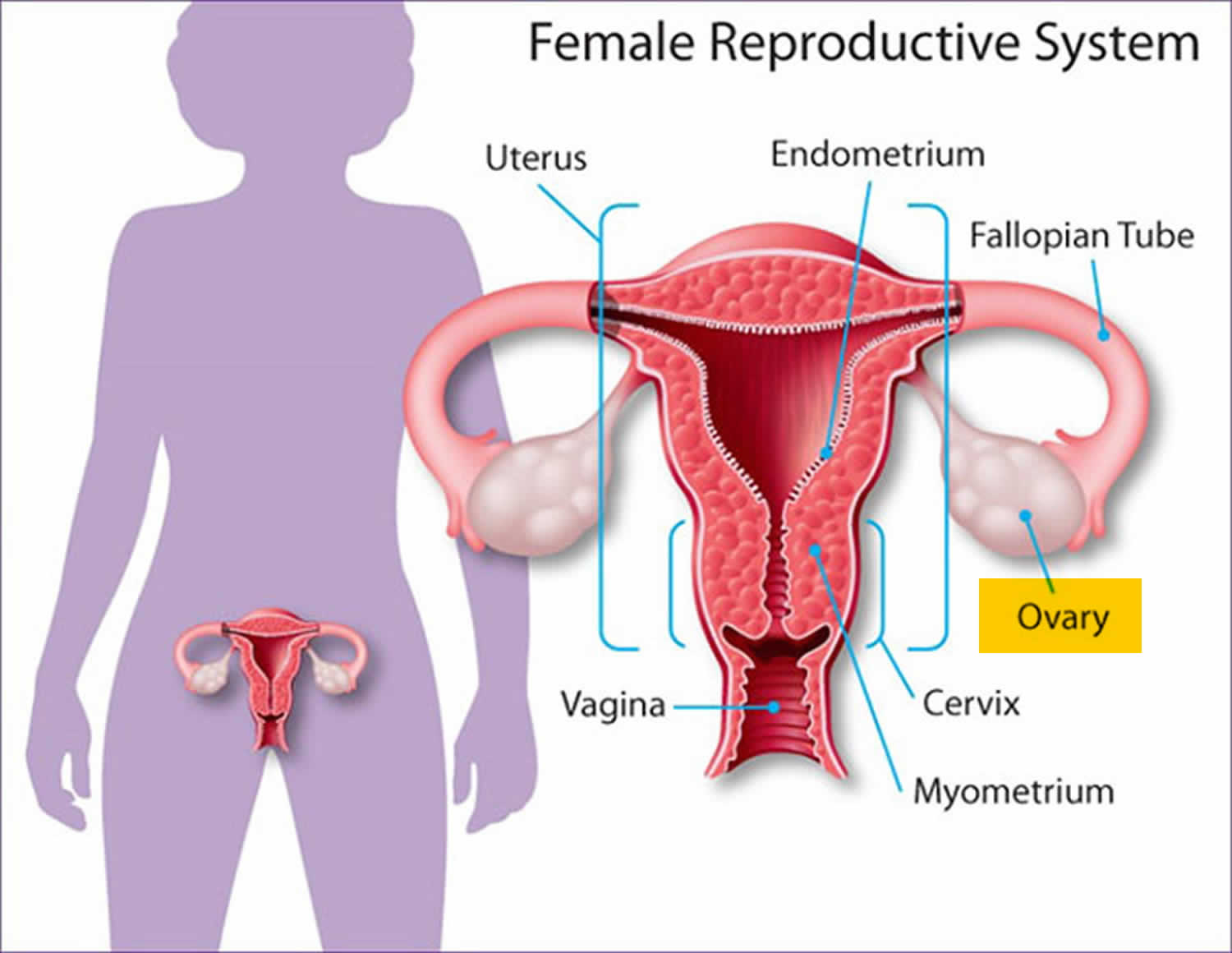
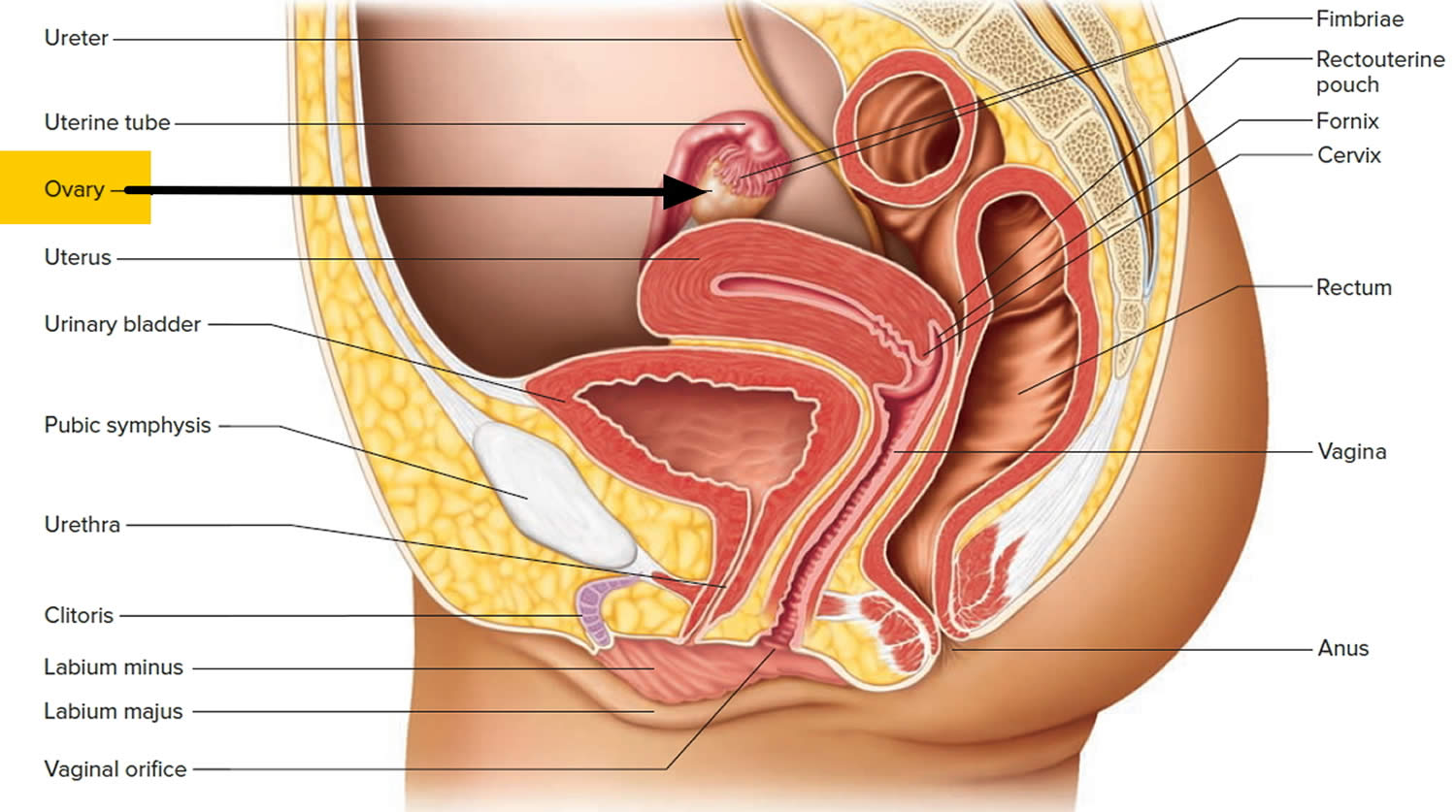
The female sexual organs
A woman’s reproductive system is made up of both external and internal organs. These are found in the pelvic area, the part of the body below the belly button.
The external organs are known as the vulva. This includes the opening of the vagina, the inner and outer lips (labia) and the clitoris.
The woman’s internal organs are made up of:
- The pelvis: this is the bony structure around the hip area, which the baby will pass through when he or she is born.
- Womb or uterus: the womb is about the size and shape of a small, upside-down pear. It’s made of muscle and grows in size as the baby grows inside it.
- Fallopian tubes: these lead from the ovaries to the womb. Eggs are released from the ovaries into the fallopian tubes each month, and this is where fertilization takes place.
- Ovaries: there are 2 ovaries, each about the size of an almond; they produce the eggs, or ova.
- Cervix: this is the neck of the womb. It’s normally almost closed, with just a small opening through which blood passes during the monthly period. During labor, the cervix dilates (opens) to let the baby move from the uterus into the vagina.
- Vagina: the vagina is a tube about 3 inches (8cm) long, which leads from the cervix down to the vulva, where it opens between the legs. The vagina is very elastic, so it can easily stretch around a man’s penis, or around a baby during labor.
Figure 1. Female reproductive organs
You should talk to your doctor about your fertility if:
- You are younger than 35 and have not been able to conceive after one year of frequent sex without birth control.
- You are age 35 or older and have not been able to conceive after six months of frequent sex without birth control.
- You believe you or your partner might have fertility problems in the future (even before you begin trying to get pregnant).
- You or your partner has a problem with sexual function or libido.
Infertility in women, your fertility may depend on:
- your age
- if you have any problems with your fallopian tubes
- if you have endometriosis or an ovulation problem
- any uterine fibroids
- pelvic inflammatory disease or sexually transmitted infections (STI).
Infertility in men may be affected by:
- problems with the tubes connected to the testes
- low sperm production
- high numbers of abnormal sperm
- genetic problems
- problems with sperm DNA.
Happily, doctors are able to help many infertile couples go on to have babies.
Most experts suggest at least one year for women younger than age 35. However, for women aged 35 years or older, couples should see a health care provider after 6 months of trying unsuccessfully. A woman’s chances of having a baby decrease rapidly every year after the age of 30.
If you’re older than 40, your doctor may want to begin testing or treatment right away.
Your doctor may also want to begin testing or treatment right away if you or your partner has known fertility problems, or if you have a history of irregular or painful periods, pelvic inflammatory disease, repeated miscarriages, prior cancer treatment, or endometriosis.
Some health problems also increase the risk of infertility. So, couples with the following signs or symptoms should not delay seeing their health care provider when they are trying to become pregnant:
- Irregular periods or no menstrual periods.
- Very painful periods.
- Endometriosis.
- Pelvic inflammatory disease.
- You’ve had multiple miscarriages.
- You have known fertility problems.
- You’ve been diagnosed with endometriosis.
- You’ve undergone treatment for cancer
- Suspected male factor (i.e., history of testicular trauma, hernia surgery, chemotherapy, or infertility with another partner).
It is a good idea for any woman and her partner to talk to a health care provider before trying to get pregnant. They can help you get your body ready for a healthy baby, and can also answer questions on fertility and give tips on conceiving.
What is ovulation?
Ovulation is when the ovary releases an egg so it can be fertilized by a sperm in order to make a baby. A woman is most likely to get pregnant if she has sex without birth control in the three days before and up to the day of ovulation (since the sperm are already in place and ready to fertilize the egg as soon as it is released). A man’s sperm can live for 3 to 5 days in a woman’s reproductive organs, but a woman’s egg lives for just 12 to 24 hours after ovulation.
Each woman’s cycle length may be different, and the time between ovulation and when the next period starts can be anywhere from one week (7 days) to more than 2 weeks (19 days) 1.
At different times in a woman’s life, ovulation may or may not happen:
- Women who are pregnant do not ovulate.
- Women who are breastfeeding may or may not ovulate. Women who are breastfeeding should talk to their doctor about birth control methods if they do not want to get pregnant.
- During perimenopause, the transition to menopause, you may not ovulate every month.
- After menopause you do not ovulate.
How do I know if I’m ovulating?
A few days before you ovulate, your vaginal mucus or discharge changes and becomes more slippery and clear. This type of mucus helps sperm move up into your uterus and into the fallopian tubes where it can fertilize an egg. Some women feel minor cramping on one side of their pelvic area when they ovulate. Some women have other signs of ovulation.
Luteinizing hormone (LH) is a hormone released by your brain that tells the ovary to release an egg (called ovulation). LH levels begin to surge upward about 36 hours before ovulation, so some women and their doctors test for LH levels. LH levels peak about 12 hours before ovulation 2. Women who are tracking ovulation to become pregnant will notice a slight rise in their basal temperature (your temperature after sleeping before you get out of bed) around ovulation.
If I’ve stopped using birth control, how long should I wait before trying to get pregnant?
There’s no right or wrong amount of time to wait. You can start trying to get pregnant right away. But the kind of birth control you used may affect how soon you start ovulating. For example:
- If you were using birth control pills, you may begin ovulating about 2 weeks after you stop taking them. But your periods may not be regular for a month or 2 after. Your period is regular if it starts the same number of days apart each month.
- If you were taking Depo-Provera, it can take 10 months or more after your last shot before you ovulate regularly. Depo-Provera is a birth control shot that you get every 3 months.
- If you had an implant or an intrauterine device (IUD), you can start trying to get pregnant as soon as you have it removed. An implant is a tiny rod inserted under the skin of your upper arm. It releases a hormone called progestin that prevents you from releasing eggs. An IUD is a t-shaped piece of plastic that’s placed in your uterus to prevent you from getting pregnant.
- If you were using a barrier method of birth control, you can start trying to get pregnant as soon as you stop using it. A barrier method keeps a man’s sperm from reaching a woman’s egg, and some help protect against sexually transmitted infections (also called STIs). An STI is an infection, like HIV and syphilis, you can get by having unprotected sex with someone who’s infected. Barrier methods include dental dams and male and female condoms. A dental dam is a square piece of rubber.
Are there things your partner can do to help improve his sperm?
Yes. Your partner may be able to make his sperm healthier and to make more sperm to help you get pregnant. Here’s what he can do:
- Get treated for health conditions, like diabetes, kidney problems and being obese, that may affect his sperm. Diabetes is when you have too much sugar (called glucose) in your blood. Being obese means you have an excess amount of body fat and your body mass index (also called BMI) is 30 or higher.
- Talk to his doctor about any medicines he takes. This includes prescription and over-the-counter (also called OTC) medicine, supplements and herbal products. A prescription medicine is medicine a health care provider says you can take to treat a health condition. You need a prescription (order) from a provider to get the medicine. OTC medicines, like pain relievers and cough syrup, are medicines you can buy without a prescription. Supplements, like vitamin B and C, are products you take to make up for certain nutrients you don’t get enough of in food. Herbal products, like Ginkgo biloba or green tea, are made from herbs (plants that are used in cooking and medicine). Ask your partner to talk to his provider to make sure the medicine he takes doesn’t affect his sperm.
- Stop smoking, drinking alcohol and using drugs that can affect his fertility (his ability to get you pregnant). Street drugs that can affect your partner’s fertility include marijuana and cocaine. Anabolic steroids also can affect his fertility. An anabolic steroid is a man-made form of testosterone (a male hormone). Providers may prescribe steroids to treat certain hormone problems and diseases, like cancer and AIDS. Some athletes and bodybuilders use steroids to improve physical performance and appearance. If your partner needs help to quit smoking, drinking alcohol or using certain drugs, encourage him to talk to his provider.
- Talk to his doctor about chemicals that can affect fertility, including metals (like lead) and radiation and chemotherapy for cancer.
What if I’ve trying to get pregnant, but I don’t get pregnant right away?
If you’ve been trying to get pregnant for 3 or 4 months, keep trying. It may just take more time. You may want to think about fertility treatment (medical treatment to help you get treatment) if:
- You’re younger than 35 and have been trying to get pregnant for more than a year.
- You’re older than 35 and have been trying to get pregnant for 6 months.
Your provider can give you and your partner some tests to help find out why you’re having trouble getting pregnant. If there’s a problem, there’s a good chance it can be treated.
Your menstrual cycle
Menstruation often called your “period”, is a woman’s monthly vaginal bleeding that occurs as part of a woman’s monthly menstrual cycle. When you menstruate, your body discards the monthly buildup of the lining of your uterus (womb). Menstrual blood and tissue flow from your uterus through the small opening in your cervix and pass out of your body through your vagina.
During the monthly menstrual cycle, the uterus lining builds up to prepare for pregnancy. If you do not get pregnant, estrogen and progesterone hormone levels begin falling. Very low levels of estrogen and progesterone tell your body to begin menstruation.
Your menstrual cycle is the monthly hormonal cycle a female’s body goes through to prepare for pregnancy. Your menstrual cycle is counted from the first day of your period up to the first day of your next period. Your hormone levels (estrogen and progesterone) usually change throughout the menstrual cycle and can cause menstrual symptoms.
The typical menstrual cycle is 28 days long, but each woman is different 3. Also, a woman’s menstrual cycle length might be different from month-to-month. Your periods are still “regular” if they usually come every 24 to 38 days 4. This means that the time from the first day of your last period up to the start of your next period is at least 24 days but not more than 38 days.
Some women’s periods are so regular that they can predict the day and time that their periods will start. Other women are regular but can only predict the start of their period within a few days.
Periods usually start between age 11 and 14 (a girl’s first period is called menarche) and continue until menopause at about age 51 5. In the United States, most girls start menstruating shortly after 12 years of age 6. The average menstruation time in normally menstruating women is 3 to 5 days 7 but a normal menstrual period can lasts up to 8 days 8. Besides bleeding from the vagina, you may have:
- Abdominal or pelvic cramping pain
- Lower back pain
- Bloating and sore breasts
- Food cravings
- Mood swings and irritability
- Headache and fatigue
Premenstrual syndrome or PMS, is a group of symptoms that start before the period. It can include emotional and physical symptoms.
Consult your health care provider if you have big changes in your cycle. They may be signs of other problems that should be treated.
Bleeding in any of the following situations is considered abnormal uterine bleeding:
- Bleeding or spotting between periods
- Bleeding or spotting after sex
- Heavy bleeding during your period
- Menstrual cycles that are longer than 38 days or shorter than 24 days
- “Irregular” periods in which cycle length varies by more than 7–9 days
- Bleeding after menopause
Some of the causes of abnormal bleeding include the following:
- Problems with ovulation
- Fibroids and polyps
- A condition in which the endometrium grows into the wall of the uterus
- Bleeding disorders
- Problems linked to some birth control methods, such as an intrauterine device (IUD) or birth control pills
- Miscarriage
- Ectopic pregnancy
- Certain types of cancer, such as cancer of the uterus
Your obstetrician–gynecologist (ob-gyn) or other health care professional may start by checking for problems most common in your age group. Some of them are not serious and are easy to treat. Others can be more serious. All should be checked.
Based on your symptoms and your age, other tests may be needed. Some of these tests can be done in your ob-gyn’s office. Others may be done at a hospital or surgical center:
- Ultrasound exam—Sound waves are used to make a picture of the pelvic organs.
- Hysteroscopy—A thin, lighted scope is inserted through the vagina and the opening of the cervix. It allows your ob-gyn or other health care professional to see the inside of the uterus.
- Endometrial biopsy—A sample of the endometrium is removed and looked at under a microscope.
- Sonohysterography—Fluid is placed in the uterus through a thin tube while ultrasound images are made of the inside of the uterus.
- Magnetic resonance imaging (MRI)—An MRI exam uses a strong magnetic field and sound waves to create images of the internal organs.
- Computed tomography (CT)—This X-ray procedure shows internal organs and structures in cross section.
You also may have a pregnancy test and tests for sexually transmitted infections (STIs).
Medications often are tried first to treat irregular or heavy menstrual bleeding. The medications that may be used include the following:
- Hormonal birth control methods—Birth control pills, the skin patch, and the vaginal ring contain hormones. These hormones can lighten menstrual flow. They also help make periods more regular.
- Gonadotropin-releasing hormone (GnRH) agonists: These drugs can stop the menstrual cycle and reduce the size of fibroids.
- Tranexamic acid: This medication treats heavy menstrual bleeding.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs, which include ibuprofen, may help control heavy bleeding and relieve menstrual cramps.
- Antibiotics: If you have an infection, you may be given an antibiotic.
- Special medications: If you have a bleeding disorder, your treatment may include medication to help your blood clot.
- If medication does not reduce your bleeding, a surgical procedure may be needed. There are different types of surgery depending on your condition, your age, and whether you want to have more children.
Endometrial ablation destroys the lining of the uterus. It stops or reduces the total amount of bleeding. Pregnancy is not likely after ablation, but it can happen. If it does, the risk of serious complications, including life-threatening bleeding, is greatly increased. If you have this procedure, you will need to use birth control until after menopause.
Uterine artery embolization is a procedure used to treat fibroids. This procedure blocks the blood vessels to the uterus, which in turn stops the blood flow that fibroids need to grow. Another treatment, myomectomy, removes the fibroids but not the uterus.
Hysterectomy, the surgical removal of the uterus, is used to treat some conditions or when other treatments have failed. Hysterectomy also is used to treat endometrial cancer. After the uterus is removed, a woman can no longer get pregnant and will no longer have periods.
Figure 2. Menstrual cycle
Figure 3. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Abbreviations: GnRH = Gonadotropin-Releasing Hormone; FSH = Follicle-Stimulating Hormone; LH= Luteinizing Hormone
Figure 4. Ovarian Follicle Maturation
Figure 5. Ovarian activity during the Menstrual cycle
Footnote: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
Abbreviations: FSH = Follicle-Stimulating Hormone; LH= Luteinizing Hormone
See your doctor about your period if:
- You have gone three months without a period and are not pregnant, breastfeeding, or in perimenopause or menopause.
- You get irregular periods (your period happens more often than every 24 days or less often than every 38 days, or lasts longer than 8 days).
- You feel dizzy, lightheaded, weak, or tired, or you have chest pain or trouble breathing during or after your period.
- You bleed through one or more pads or tampons every one to two hours.
- You suddenly get a fever and feel sick after using tampons.
- You have menstrual pain that doesn’t get better with over-the-counter pain medicine, such as ibuprofen or naproxen.
- You have period pain, cramps, or heavy bleeding that makes you miss work, school, or other daily activities.
- You get a migraine around your period or your regular migraine treatment stops working.
- You have blood clots in your menstrual flow that are larger than a quarter.
- You have bleeding after sex, more than once.
- You have spotting or bleeding any time in the menstrual cycle other than during your period.
- You have bleeding after menopause.
How does my menstrual cycle affect my health?
Changing hormone levels throughout your menstrual cycle can cause health problems or make health problems worse:
- Anemia. Heavy menstrual bleeding is the most common cause of iron-deficiency anemia in women of childbearing age. Anemia is a condition that happens when your blood cannot carry enough oxygen to all of the different parts of your body because it does not have enough iron. This makes you pale or feel tired or weak.
- Asthma. Your asthma symptoms may be worse during some parts of your cycle.
- Depression. Women with a history of depression are more likely to have PMS or premenstrual dysphoric disorder (PMDD). Symptoms of depression may be worse just before their periods.
- Diabetes. Women with irregular menstrual cycles, especially those longer than 40 days, have a higher risk for type 2 diabetes.
- Irritable bowel syndrome (IBS). IBS causes cramping, bloating, and gas. Your IBS symptoms may get worse right before your period.
- Problems getting pregnant. Health problems, such as endometriosis, polycystic ovary syndrome (PCOS) or underweight or obesity, can cause irregular periods. This can make it harder to get pregnant.
How long does a woman usually have periods?
On average, women get a period for about 40 years of their life 9. Most women have regular periods until perimenopause, the time when your body begins the change to menopause. Perimenopause, or transition to menopause, may take a few years. During this time, your period may not come regularly. Menopause happens when you have not had a period for 12 months in a row. For most women, this happens between the ages of 45 and 55. The average age of menopause in the United States is 52.
Periods also stop during pregnancy and may not come back right away if you breastfeed.
But if you don’t have a period for 90 days (three months), and you are not pregnant or breastfeeding, talk to your doctor or nurse. Your doctor will check for pregnancy or a health problem that can cause periods to stop or become irregular.
Day 1
The first day of bleeding is considered the first day of the menstrual cycle. After bleeding ends, usually around day 5, levels of the hormone estrogen begin to rise. The rise in estrogen causes the lining of the uterus to thicken as it prepares to hold a fertilized egg. At the same time, the changes in hormone levels cause follicles (the sacs in the ovary that contain eggs) to grow and mature, in preparation for one follicle to go through ovulation.
Ovulation
Around day 12 to 14 in an average 28-day cycle, the egg is released from a follicle on the ovary in a process called ovulation. Ovulation can occur anywhere between 10 and 21 days after the first day of a woman’s menstrual cycle. Ovulation is when the ovary releases an egg so it can be fertilized by a sperm to make a baby. A woman is most likely to get pregnant if she has sex without birth control in the three days before and up to the day of ovulation.
It may be difficult to know when you ovulate, but you can watch for signs. A few days before you ovulate, your vaginal mucus or discharge changes and becomes
more slippery and clear. A woman can also tell when she has begun ovulating using several methods, including at-home tests that measure levels of luteinizing hormone (LH) in the urine and keeping track of her body temperature, which typically rises slightly at ovulation. At mid-cycle, some women experience pain on one side of their pelvic area; this pain is called “Mittelschmerz” (meaning “middle pain,” because it occurs in the middle of the cycle) and may be a signal of ovulation 10.
More than 90 percent of women say they get symptoms of premenstrual syndrome (PMS) in the time after ovulation and before their period starts.
If a pregnancy does not occur, decreasing hormone levels signal for the lining of the uterus, called the endometrium, to be shed during menstruation.
The endometrium builds up and breaks down during the menstrual cycle. The endometrium is thickest halfway through the 28-day cycle. Then, if there is no pregnancy, it breaks down. This breakdown causes the bleeding of the menstrual phase. Figure 5 above illustrates an average 28-day cycle.
How do I know if I’m ovulating?
A few days before you ovulate, your vaginal mucus or discharge changes and becomes more slippery and clear. This type of mucus helps sperm move up into your uterus and into the fallopian tubes where it can fertilize an egg. Some women feel minor cramping on one side of their pelvic area when they ovulate. Some women have other signs of ovulation.
Luteinizing hormone (LH) is a hormone released by your brain that tells the ovary to release an egg (called ovulation). LH levels begin to surge upward about 36 hours before ovulation, so some women and their doctors test for LH levels. LH levels peak about 12 hours before ovulation 11. Women who are tracking ovulation to become pregnant will notice a slight rise in their basal temperature (your temperature after sleeping before you get out of bed) around ovulation.
How long is a typical menstrual cycle?
The typical menstrual cycle is 28 days long, but each woman is different 12. Also, a woman’s menstrual cycle length might be different from month-to-month. Your periods are still “regular” if they usually come every 24 to 38 days 13. This means that the time from the first day of your last period up to the start of your next period is at least 24 days but not more than 38 days.
Some women’s periods are so regular that they can predict the day and time that their periods will start. Other women are regular but can only predict the start of their period within a few days.
How can I keep track of my menstrual cycle?
You can keep track of your menstrual cycle by marking the day you start your period on a calendar. After a few months, you can begin to see if your periods are regular or if your cycles are different each month.
You may want to track:
- Premenstrual syndrome (PMS) symptoms: Did you have cramping, headaches, moodiness, forgetfulness, bloating, or breast tenderness?
- When your bleeding begins: Was it earlier or later than expected?
- How heavy the bleeding was on your heaviest days: Was the bleeding heavier or lighter than usual? How many pads or tampons did you use?
- Period symptoms: Did you have pain or bleeding on any days that caused you to miss work or school?
- How many days your period lasted: Was your period shorter or longer than the month before?
You can also download apps (sometimes for free) for your phone to track your periods. Some include features to track your PMS symptoms, energy and activity levels, and more.
How does my menstrual cycle change as I get older?
Your cycles may change in different ways as you get older. Often, periods are heavier when you are younger (in your teens) and usually get lighter in your 20s and 30s. This is normal.
- For a few years after your first period (menarche), menstrual cycles longer than 38 days are common. Girls usually get more regular cycles within three years of starting their periods. If longer or irregular cycles last beyond that, see your doctor or nurse to rule out a health problem, such as polycystic ovary syndrome (PCOS) 14.
- In your 20s and 30s, your cycles are usually regular and can last anywhere from 24 to 38 days.
- In your 40s, as your body starts the transition to menopause, your cycles might become irregular. Your menstrual periods might stop for a month or a few months and then start again. They also might be shorter or last longer than usual, or be lighter or heavier than normal.
Talk to your doctor or nurse if you have menstrual cycles that are longer than 38 days or shorter than 24 days, or if you are worried about your menstrual cycle.
Why should I keep track of my menstrual cycle?
If your periods are regular, tracking them will help you know when you ovulate, when you are most likely to get pregnant, and when to expect your next period to start.
If your periods are not regular, tracking them can help you share any problems with your doctor or nurse.
If you have period pain or bleeding that causes you to miss school or work, tracking these period symptoms will help you and your doctor or nurse find treatments that work for you. Severe pain or bleeding that causes you to miss regular activities is not normal and can be treated.
When does a girl usually get her first period?
The average age for a girl in the United States to get her first period is 12 15. This does not mean that all girls start at the same age.
A girl may start her period anytime between 8 and 15. The first period normally starts about two years after breasts first start to develop and pubic hair begins to grow. The age at which a girl’s mother started her period can help predict when a girl may start her period.
A girl should see her doctor if:
- She starts her period before age 8.
- She has not had her first period by age 15.
- She has not had her first period within three years of breast growth.
What is a normal amount of bleeding during my period?
The average woman loses about two to three tablespoons of blood during her period. Your periods may be lighter or heavier than the average amount. What is normal for you may not be the same for someone else. Also, the flow may be lighter or heavier from month to month.
Your periods may also change as you get older. Some women have heavy bleeding during perimenopause, the transition to menopause. Symptoms of heavy menstrual bleeding may include:
- Bleeding through one or more pads or tampons every one to two hours
- Passing blood clots larger than the size of quarters
- Bleeding that often lasts longer than eight days
How often should I change my pad, tampon, menstrual cup, sponge, or period panties?
Follow the instructions that came with your period product. Try to change or rinse your feminine hygiene product before it becomes soaked through or full.
- Most women change their pads every few hours.
- A tampon should not be worn for more than 8 hours because of the risk of toxic shock syndrome
- Menstrual cups and sponges may only need to be rinsed once or twice a day.
- Period panties (underwear with washable menstrual pads sewn in) can usually last about a day, depending on the style and your flow.
Use a product appropriate in size and absorbency for your menstrual bleeding. The amount of menstrual blood usually changes during a period. Some women use different products on different days of their period, depending on how heavy or light the bleeding is.
What is toxic shock syndrome?
Toxic shock syndrome (TSS) is a rare but sometimes deadly condition caused by bacteria that make toxins or poisons. In 1980, 63 women died from toxic shock syndrome. A certain brand of super absorbency tampons was said to be the cause. These tampons were taken off the market.
Today, most cases of toxic shock syndrome are not caused by using tampons. But, you could be at risk for toxic shock syndrome if you use more absorbent tampons than you need for your bleeding or if you do not change your tampon often enough (at least every four to eight hours). Menstrual cups, cervical caps, sponges, or diaphragms (anything inserted into your vagina) may also increase your risk for toxic shock syndrome if they are left in place for too long (usually 24 hours). Remove sponges within 30 hours and cervical caps within 48 hours 16.
If you have any symptoms of toxic shock syndrome, take out the tampon, menstrual cup, sponge, or diaphragm, and call your local emergency services number or go to the hospital right away.
Symptoms of toxic shock syndrome include 17:
- Sudden high fever
- Muscle aches
- Vomiting
- Nausea
- Diarrhea
- Rash
- Kidney or other organ failure
Charting your fertility pattern
Knowing when you’re most fertile will help you plan pregnancy. There are three ways you can keep track of your fertile times. They are:
- Basal body temperature method – Basal body temperature is your temperature at rest as soon as you awake in the morning. A woman’s basal body temperature rises slightly with ovulation. So by recording this temperature daily for several months, you’ll be able to predict your most fertile days. Basal body temperature differs slightly from woman to woman. Anywhere from 96 to 98 degrees Fahrenheit orally is average before ovulation. After ovulation most women have an oral temperature between 97 and 99 degrees Fahrenheit (36.1 and 37.2 degrees Celsius). The rise in temperature can be a sudden jump or a gradual climb over a few days. Usually a woman’s basal body temperature rises by only 0.4 to 0.8 degrees Fahrenheit. To detect this tiny change, women must use a basal body thermometer. These thermometers are very sensitive. Most pharmacies sell them for about $10. The rise in temperature doesn’t show exactly when the egg is released. But almost all women have ovulated within three days after their temperatures spike. Body temperature stays at the higher level until your period starts.
- You are most fertile and most likely to get pregnant:
- Two to three days before your temperature hits the highest point (ovulation)
- And 12 to 24 hours after ovulation
- A man’s sperm can live for up to three days in a woman’s body. The sperm can fertilize an egg at any point during that time. So if you have unprotected sex a few days before ovulation, you could get pregnant.
- Many things can affect basal body temperature. For your chart to be useful, make sure to take your temperature every morning at about the same time. Things that can alter your temperature include:
- Drinking alcohol the night before
- Smoking cigarettes the night before
- Getting a poor night’s sleep
- Having a fever
- Doing anything in the morning before you take your temperature — including going to the bathroom and talking on the phone
- You are most fertile and most likely to get pregnant:
- Calendar method – This involves recording your menstrual cycle on a calendar for eight to 12 months. The first day of your period is Day 1. Circle Day 1 on the calendar. The length of your cycle may vary from month to month. So write down the total number of days it lasts each time. Using this record, you can find the days you are most fertile in the months ahead:
- To find out the first day when you are most fertile, subtract 18 from the total number of days in your shortest cycle. Take this new number and count ahead that many days from the first day of your next period. Draw an X through this date on your calendar. The X marks the first day you’re likely to be fertile.
- To find out the last day when you are most fertile, subtract 11 from the total number of days in your longest cycle. Take this new number and count ahead that many days from the first day of your next period. Draw an X through this date on your calendar. The time between the two Xs is your most fertile window.
- This method always should be used along with other fertility awareness methods, especially if your cycles are not always the same length.
- Cervical mucus method also known as the ovulation method – This involves being aware of the changes in your cervical mucus throughout the month. The hormones that control the menstrual cycle also change the kind and amount of mucus you have before and during ovulation. Right after your period, there are usually a few days when there is no mucus present or “dry days.” As the egg starts to mature, mucus increases in the vagina, appears at the vaginal opening, and is white or yellow and cloudy and sticky. The greatest amount of mucus appears just before ovulation. During these “wet days” it becomes clear and slippery, like raw egg whites. Sometimes it can be stretched apart. This is when you are most fertile. About four days after the wet days begin the mucus changes again. There will be much less and it becomes sticky and cloudy. You might have a few more dry days before your period returns. Describe changes in your mucus on a calendar. Label the days, “Sticky,” “Dry,” or “Wet.” You are most fertile at the first sign of wetness after your period or a day or two before wetness begins. The cervical mucus method is less reliable for some women. Women who are breastfeeding, taking hormonal birth control (like the pill), using feminine hygiene products, have vaginitis or sexually transmitted infections (STIs), or have had surgery on the cervix should not rely on this method.
To most accurately track your fertility, use a combination of all three methods. This is called the symptothermal method. You can also purchase over-the-counter ovulation kits or fertility monitors to help find the best time to conceive. These kits work by detecting surges in a specific hormone called luteinizing hormone (LH), which triggers ovulation.
References- Wilcox AJ, Dunson D, Baird DD. The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. BMJ. 2000;321(7271):1259‐1262. doi:10.1136/bmj.321.7271.1259
- Reed, B.G., Carr, B.R. (2015). The Normal Menstrual Cycle and the Control of Ovulation. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.
- Chiazze L, Brayer FT, Macisco JJ, Parker MP, Duffy BJ. The Length and Variability of the Human Menstrual Cycle. JAMA. 1968;203(6):377–380. doi:10.1001/jama.1968.03140060001001
- Fraser, I.S., Critchley, H., Broder, M., Munro, M.G. (2011). The FIGO Recommendations on Terminologies and Definitions for Normal and Abnormal Uterine Bleeding. The Seminars in Reproductive Medicine; 29(5): 383-390. http://www.pharllc.com/wp-content/uploads/2014/03/Fraser-Semin-Reprod-Med-2011.pdf
- Sweet, M. G., Schmidt-Dalton, T. A., Weiss, P. M., & Madsen, K. P. (2012). Evaluation and management of abnormal uterine bleeding in premenopausal women. American Family Physician, 85, 35–43.
- McDowell, M. A., Brody, D. J., & Hughes, J.P. (2007). Has age at menarche changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999-2004. Journal of Adolescent Health, 40, 227–231.
- Dasharathy, S. S., Mumford, S. L., Pollack, A. Z., Perkins, N. J., Mattison, D. R., Wactawski-Wende, J., & Schisterman, E. F. (2012). Menstrual bleeding patterns among regularly menstruating women. American Journal of Epidemiology, 175, 536–545.
- Abnormal Uterine Bleeding. https://www.acog.org/Patients/FAQs/Abnormal-Uterine-Bleeding
- Shifren, J.L., Gass, M.L.S., for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. (2014). The North American Menopause Society Recommendations for Clinical Care of Midlife Women (link is external). Menopause; 21(10): 1038–1062.
- Krohn, P. L. (1949). Intermenstrual pain (the “Mittelschmerz”) and the time of ovulation. British Medical Journal, 1(4609), 803–805. Retrieved September 27, 2016
- Reed BG, Carr BR. The Normal Menstrual Cycle and the Control of Ovulation. [Updated 2018 Aug 5]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279054
- Chiazze, L., Brayer, F.T., Macisco, J.J., Parker, M.P., Duffy, B.J. (1968). The Length and Variability of the Human Menstrual Cycle (link is external). JAMA; 203(6): 377–380.
- Fraser, I.S., Critchley, H., Broder, M., Munro, M.G. (2011). The FIGO Recommendations on Terminologies and Definitions for Normal and Abnormal Uterine Bleeding. (link is external)The Seminars in Reproductive Medicine; 29(5): 383-390.
- Menstruation in Girls and Adolescents: Using the Menstrual Cycle as a Vital Sign. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2015/12/menstruation-in-girls-and-adolescents-using-the-menstrual-cycle-as-a-vital-sign
- McDowell, M.A., Brody, D.J., Hughes, J.P. (2007). Has Age at Menarche Changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999–2004 (link is external). Journal of Adolescent Health; 40(3): 227–231.
- American College of Obstetricians and Gynecologists. (2016). Barrier Methods of Birth Control: Spermicide, Condom, Sponge, Diaphragm, and Cervical Cap.
- Matsuda, Y., Kato, H., Ono, E., Kikuchi, K., Muraoka, M., Takagi, K. (2008). Diagnosis of toxic shock syndrome by two different systems; clinical criteria and monitoring of TSST-1-reactive T cells. Microbiol Immunol; 52(11):513-21.