Blunt force trauma
Blunt trauma is physical trauma to a body part, either by impact, injury or physical attack with an object that is blunt, or not sharp, with enough force to cause significant damage. Blunt trauma is the initial trauma, from which develops more specific types such as contusions, abrasions, lacerations, and/or bone fractures. The majority of serious traumatic injuries are due to blunt trauma from motor vehicle crashes and pedestrian injuries. Falls are also an important cause, particularly in the elderly. Direct blows, assaults, and sporting injuries are also common. Non-accidental trauma is an important cause and should be suspected with certain presentations and injury patterns. Blunt impact to the body may result in a variety of injuries. Severity is related to both the mechanism of injury as well as the underlying comorbidities of the patient. Blunt impact injuries generally can be classified into four categories: contusion, abrasion, laceration, and fracture 1. Trauma is the leading cause of morbidity and mortality in patients under 35-years of age and the sixth leading cause of death worldwide 2. Blunt impact injuries are commonly seen in forensic autopsy practice, and appropriate interpretation of wounds is essential for accurate medicolegal testimony.
Blunt force injuries result from direct contact of a blunt object with a body. A contusion results from the blunt impact of significant force to rupture capillaries underneath the skin surface while leaving the skin surface intact, while an abrasion results from scraping off of the superficial epidermis. Contusions and abrasions may show distinct patterns which can be used to match a specific wound to a potential weapon or implement; for example, a contusion over the forehead with multiple parallel, zig-zag lines may be matched to the sole of a shoe collected at the crime scene. A laceration results from the blunt impact of significant force to tear the skin, leaving strands of subcutaneous tissues bridging the wound 3. Contusions and lacerations may also be present on internal organs. Blunt impact of significant force to a bone results in a fracture.
Blunt force injuries are commonly seen in living and deceased patients. The appearance of wounds depends on multiple factors, including the force, speed, length of time of impact, the surface area of contact, and elasticity of tissues impacted. A large, crushing force applied to a sizable area over several minutes will result in vast tissue damage; for example, failure of the integrity of a retaining wall at a construction site will likely cause significant blunt impact injury if the wall collapses on and traps the legs of an individual. Alternatively, a smaller force applied to a smaller area will result in less tissue damage; for example, the impact of a thrown baseball to the shoulder of an individual will likely cause minor blunt trauma.
Head trauma and exsanguination are the most common early causes of death due to blunt traumatic injury.
Patients presenting with acute blunt trauma should be carefully assessed to ensure serious injuries are not missed. This entails obtaining a history of mechanism, events, comorbidities, allergies, medications, and last meal. Primary, secondary, and tertiary surveys are important, with appropriate intervention and resuscitation as required.
Blunt impact injuries usually manifest immediately after impact; however, deep contusions may not be visible on the skin surface for several days after the injury occurs. Examination of adjacent or underlying subcutaneous soft tissues may aid in distinguishing between contusion, in which there will be hemorrhage due to rupture of blood vessels, and lividity, a postmortem change in which blood is contained within blood vessels. Characteristics of fractures and associated soft tissue and/or skeletal muscle injuries may aid in establishing directionality of the impact causing the wound; for example, bumper impact to a pedestrian’s legs often results in comminuted fractures of the tibia and/or fibula with a triangular bone fragment pointing in the direction the vehicle was moving.
The management of blunt force trauma patients is with an interprofessional team that includes a trauma surgeon, emergency department physician, nurse practitioner, anesthesiologist, internist, and specialty-trained emergency and trauma nurses. After the secondary survey is done by the team, other specialists can be consulted as appropriate. All over the U.S., hospitals now have protocols to manage blunt force trauma. The outcomes of these patients depend on their age, type of injury, other comorbidities, time to treatment and number of organs involved. While mortality rates have dropped over the past 3 decades, a significant number of trauma patients still die either at the scene or upon arrival to the trauma center.
- The clinicians should focus on completing the first and secondary survey and performing procedures.
- The emergency and trauma nurses should provide patient monitoring, assist with procedures, and providing medications and blood products.
- The pharmacist should double-check dosing and assist in evaluating any medications that may cause deterioration or drug-drug interactions.
- A clinician or nurse should coordinate with the team to provide family education during and after the recitation.
The importance of coordination and communication between members of the team will improve outcomes 4.
Blunt trauma pathophysiology
Blunt trauma may result in internal or external hemorrhage depending on location and mechanism. Recent contusions are typically red/purple and go through a series of color changes as they heal. In general, a red/purple contusion will be more recent than a yellow/green contusion on the same patient. Similarly, recent abrasions and lacerations are typically red/purple and heal through the process of scab formation which imparts a tan/brown, crusted appearance to the wound. Postmortem abrasions will demonstrate a more tan/yellow, parchment-paper-like appearance indicating the absence of blood flow at the time the injury occurred 5. Fractures heal through the process of callus formation and bony remodeling, features which can be examined microscopically to estimate the approximate age of the fracture and time since the injury.
Blunt trauma diagnosis
The Advanced Trauma Life Support course was developed by the American College of Surgeons to promote a standardized, methodical approach to the evaluation of trauma patients 6. The course teaches the initial assessment of trauma patients with a focus on preparation, triage, the primary survey, resuscitation, adjuncts to primary survey and resuscitation, consideration of the need for patient transfer, secondary survey, adjuncts to post-resuscitation monitoring, and reevaluation and definitive care.
Diagnosis of various blunt impact injuries and estimation of time since the injury occurred are made by gross and microscopic examination of wounds. Recent blunt impact injuries are typically characterized by acute hemorrhage microscopically without evidence of organization or hemosiderin deposition, while older blunt impact injuries show evidence of red and white blood cell degeneration, fibroblast proliferation, and hemosiderin deposition.
Blunt trauma treatment
Victims of blunt trauma who meet certain triage criteria have been demonstrated to have improved outcomes when managed in a trauma center. Patients with a Glasgow Coma Scale (GCS) score greater than 13, respiratory rates less than 10/minute or greater than 29/minute, or patients who need ventilatory support warrant triage to a trauma center 7. Patients with two or more long bone fractures, crushed or pulseless extremities, amputations proximal to the ankle or wrist, pelvic fractures, paralysis, or depressed skull fractures warrant trauma center triage based on injuries. The mechanism is also important as victims of high-risk auto crashes, falls from heights, motorcycle crashes, and pedestrian accidents with significant impact should be managed in a trauma center. Elderly patients, pregnant patients, anticoagulated patients, and young children should be managed in trauma centers capable of providing specialized care.
Mortality from trauma is declining for those who survive to reach trauma centers, representing improvements in resuscitation and management. A methodical approach that adheres to evidence-based guidelines for resuscitation and treatment is critical. Many traumatic injuries will heal with supportive care alone, while some may require surgery or interventional radiology for hemorrhage control 8.
Blunt head trauma
Blunt head trauma also known as blunt traumatic brain injury (TBI), caused by an external force that produces movement of the brain within the skull and is a significant cause of morbidity and mortality in the United States, with an annual occurrence of more than 1.5 million 9. Causes include falls, motor vehicle crashes, sports injuries, or being struck by an object. Blast injury due to explosions is a focus of intense study but how it causes brain injury is not fully known. Falls are the most common cause of traumatic brain injury, and motor vehicle-related incidents are the second leading cause of traumatic brain injury. Motor vehicle-related traumatic brain injury includes automobile, motorcycle, and bicycle accidents and pedestrians struck by those vehicles. Sports, recreation, and work-related injuries are the third leading cause of traumatic brain injury, and assaults are the fourth leading cause of traumatic brain injury. Blast injuries are the leading cause of traumatic brain injury in active duty military personnel in war zones 10. Not all blows or jolts to the head result in a traumatic brain injury. For the ones that do, traumatic brain injuries can range from mild (a brief change in mental status or consciousness) to severe (an extended period of unconsciousness or amnesia after the injury).
According to data from the Centers for Disease Control and Prevention (CDC), falls are the most common cause of traumatic brain injuries and occur most frequently among the youngest and oldest age groups. From 2006 to 2010 alone, falls caused more than half (55 percent) of traumatic brain injuries among children aged 14 and younger. Among Americans age 65 and older, falls accounted for more than two-thirds (81 percent) of all reported traumatic brain injuries.
The second and third most common causes of traumatic brain injury are unintentional blunt trauma (accidents that involved being struck by or against an object), followed closely by motor vehicle accidents. Blunt trauma is especially common in children younger than 15 years old, causing nearly a quarter of all traumatic brain injuries. Assaults account for an additional 10 percent of traumatic brain injuries, and include abuse-related traumatic brain injuries, such as head injuries that result from shaken baby syndrome.
Unintentional blunt trauma includes sports-related injuries, which are also a major cause of traumatic brain injury. Overall, bicycling, football, playground activities, basketball, and soccer result in the most traumatic brain injury-related emergency room visits. The cause of these injuries does vary slightly by gender. According to the CDC, among children age 10 to 19, boys are most often injured while playing football or bicycling. Among girls, traumatic brain injury occur most often while playing soccer or basketball or while bicycling. Anywhere from 1.6 million to 3.8 million sports- and recreation-related traumatic brain injuries are estimated to occur in the United States annually.
Adults age 65 and older are at greatest risk for being hospitalized and dying from a traumatic brain injury, most likely from a fall. traumatic brain injury-related deaths in children aged 4 years and younger are most likely the result of assault. In young adults aged 15 to 24 years, motor vehicle accidents are the most likely cause. In every age group, serious traumatic brain injury rates are higher for men than for women. Men are more likely to be hospitalized and are nearly three times more likely to die from a traumatic brain injury than women.
Patients with moderate and severe traumatic brain injury comprise the about 20% of traumatic brain injury, and those with moderate traumatic brain injury have a mortality of about 15% while those with severe traumatic brain injury have an associated mortality approaching 40%. The majority (approximately 80%) of patients with traumatic brain injury have mild traumatic brain injury which is associated with a less than 0.5% mortality, but about 25% experience extended post-concussive symptoms including a headache, dizziness, difficulty concentrating, and depression 11.
Blunt force trauma to the head-related damage can be confined to one area of the brain, known as a focal injury, or it can occur over a more widespread area, known as a diffuse injury 12. The type of injury is another determinant of the effect on the brain. Some injuries are considered primary, meaning the damage is immediate. Other consequences of traumatic brain injury can be secondary, meaning they can occur gradually over the course of hours, days, or weeks. These secondary brain injuries are the result of reactive processes that occur after the initial head trauma.
There are a variety of immediate effects on the brain, including various types of bleeding and tearing forces that injure nerve fibers and cause inflammation, metabolic changes, and brain swelling 12.
- Diffuse axonal injury (DAI) is one of the most common types of brain injuries. Diffuse axonal injury refers to widespread damage to the brain’s white matter. White matter is composed of bundles of axons (projections of nerve cells that carry electrical impulses). Like the wires in a computer, axons connect various areas of the brain to one another. Diffuse axonal injury is the result of shearing forces, which stretch or tear these axon bundles. This damage commonly occurs in auto accidents, falls, or sports injuries. It usually results from rotational forces (twisting) or sudden deceleration. It can result in a disruption of neural circuits and a breakdown of overall communication among nerve cells, or neurons, in the brain. It also leads to the release of brain chemicals that can cause further damage. These injuries can cause temporary or permanent damage to the brain, and recovery can be prolonged.
- Concussion– a type of mild traumatic brain injury that may be considered a temporary injury to the brain but could take minutes to several months to heal. Concussion can be caused by a number of things including a bump, blow, or jolt to the head, sports injury or fall, motor vehicle accident, weapons blast, or a rapid acceleration or deceleration of the brain within the skull (such as the person having been violently shaken). The individual either suddenly loses consciousness or has sudden altered state of consciousness or awareness, and is often called “dazed” or said to have his/her “bell rung.” A second concussion closely following the first one causes further damage to the brain — the so-called “second hit” phenomenon — and can lead to permanent damage or even death in some instances.
- Hematomas — a pooling of blood in the tissues outside of the blood vessels. Hematomas can develop when major blood vessels in the head become damaged, causing severe bleeding in and around the brain. Different types of hematomas form depending on where the blood collects relative to the meninges. The meninges are the protective membranes surrounding the brain, which consist of three layers: dura mater (outermost), arachnoid mater (middle), and pia mater (innermost).
- Epidural hematomas involve bleeding into the area between the skull and the dura mater. These can occur with a delay of minutes to hours after a skull fracture damages an artery under the skull, and are particularly dangerous.
- Subdural hematomas involve bleeding between the dura and the arachnoid mater, and like epidural hematomas exert pressure on the outside of the brain . Their effects vary depending on their size and extent to which they compress the brain. They are very common in the elderly after a fall.
- Subarachnoid hemorrhage is bleeding that occurs between the arachnoid mater and the pia mater and their effects vary depending on the amount of bleeding.
Bleeding into the brain itself is called an intracerebral hematoma and damages the surrounding tissue.
- Contusions — a bruising or swelling of the brain that occurs when very small blood vessels bleed into brain tissue. Contusions can occur directly under the impact site (i.e, a coup injury) or, more often, on the complete opposite side of the brain from the impact (i.e., a contrecoup injury). They can appear after a delay of hours to a day.
- Coup or Contrecoup lesions — contusions or subdural hematomas that occur at the site of head impact as well as directly opposite the coup lesion. Generally they occur when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (such as in a high-speed car crash). This type of injury also occurs in shaken baby syndrome, a severe head injury that results when an infant or toddler is shaken forcibly enough to cause the brain to bounce back and forth against the skull.
- Skull fractures — breaks or cracks in one or more of the bones that form the skull. They are a result of blunt force trauma and can cause damage to the underlying areas of the skull such as the membranes, blood vessels, and brain. One main benefit of helmets is to prevent skull fracture.
Most patients with moderate to severe traumatic brain injury have a combination of intracranial injuries. The majority of patients with moderate to severe traumatic brain injury have related diffuse axonal injury to some degree. Diffuse axonal injury typically is caused by a rapid rotational or deceleration force that causes stretching and tearing of neurons, leading to focal areas of hemorrhage and edema that are not always detected on initial CT scan. Subarachnoid hemorrhage is the most common CT finding in traumatic brain injury and is caused by tears in the pial vessels. Subdural and epidural hematomas are the most frequent type of mass lesion identified in traumatic brain injury. Cerebral contusions occur in about a third of patients with moderate to severe traumatic brain injury, caused by direct impact or acceleration-deceleration forces that cause the brain to strike the frontal or temporal regions of the skull. Intracerebral bleeding or hematoma, caused by coalescence of contusions or a tear in a parenchymal vessel, occurring in up to a third of patients with moderate to severe traumatic brain injury 13.
The first 24 hours after mild blunt force trauma to the head are particularly important because subdural hematoma, epidural hematoma, ontusion, or excessive brain swelling (edema) are possible and can cause further damage. For this reason doctors suggest watching a person for changes for 24 hours after a concussion 12.
- Hemorrhagic progression of a contusion contributes to secondary injuries. Hemorrhagic progression of a contusions occur when an initial contusion from the primary injury continues to bleed and expand over time. This creates a new or larger lesion — an area of tissue that has been damaged through injury or disease. This increased exposure to blood, which is toxic to brain cells, leads to swelling and further brain cell loss.
- Secondary damage may also be caused by a breakdown in the blood-brain barrier. The blood-brain barrier preserves the separation between the brain fluid and the very small capillaries that bring the brain nutrients and oxygen through the blood. Once disrupted, blood, plasma proteins, and other foreign substances leak into the space between neurons in the brain and trigger a chain reaction that causes the brain to swell. It also causes multiple biological systems to go into overdrive, including inflammatory responses which can be harmful to the body if they continue for an extended period of time. It also permits the release of neurotransmitters, chemicals used by brain cells to communicate, which can damage or kill nerve cells when depleted or over-expressed.
- Poor blood flow to the brain can also cause secondary damage. When the brain sustains a powerful blow, swelling occurs just as it would in other parts of the body. Because the skull cannot expand, the brain tissue swells and the pressure inside the skull rises; this is known as intracranial pressure (ICP). When the intracranial pressure becomes too high it prevents blood from flowing to the brain, which deprives it of the oxygen it needs to function. This can permanently damage brain function.
Blunt head trauma prevention
The best treatment for traumatic brain injury is prevention. Unlike most neurological disorders, head injuries can be prevented. According to the CDC, doing the following can help prevent traumatic brain injuries:
- Wear a seatbelt when you drive or ride in a motor vehicle.
- Wear the correct helmet and make sure it fits properly when riding a bicycle, skateboarding, and playing sports like hockey and football.
- Install window guards and stair safety gates at home for young children.
- Never drive under the influence of drugs or alcohol.
- Improve lighting and remove rugs, clutter, and other trip hazards in the hallway.
- Use nonslip mats and install grab bars next to the toilet and in the tub or shower for older adults.
- Install handrails on stairways.
- Improve balance and strength with a regular physical activity program.
- Ensure children’s playgrounds are made of shock-absorbing material, such as hardwood mulch or sand.
Blunt force trauma to the head signs and symptoms
The effects of traumatic brain injury can range from severe and permanent disability to more subtle functional and cognitive difficulties that often go undetected during initial evaluation. These problems may emerge days later. Headache, dizziness, confusion, and fatigue tend to start immediately after an injury, but resolve over time. Emotional symptoms such as frustration and irritability tend to develop later on during the recovery period. Many of the signs and symptoms can be easily missed as people may appear healthy even though they act or feel different. Many of the symptoms overlap with other conditions, such as depression or sleep disorders. If any of the following symptoms appear suddenly or worsen over time following a traumatic brain injury, especially within the first 24 hours after the injury, people should see a medical professional on an emergency basis..
People should seek immediate medical attention if they experience any of the following symptoms:
- loss of or change in consciousness anywhere from a few seconds to a few hours
- decreased level of consciousness, i.e., hard to awaken
- convulsions or seizures
- unequal dilation in the pupils of the eyes or double vision
- clear fluids draining from the nose or ears
- nausea and vomiting
- new neurologic deficit, i.e., slurred speech; weakness of arms, legs, or face; loss of balance
Other common symptoms that should be monitored include:
- mild to profound confusion or disorientation
- problems remembering, concentrating, or making decisions
- headache
- light-headedness, dizziness, vertigo, or loss of balance or coordination
- sensory problems, such as blurred vision, seeing stars, ringing in the ears, bad taste in the mouth
- sensitivity to light or sound
- mood changes or swings, agitation (feeling sad or angry for no reason), combativeness, or other unusual behavior
- feelings of depression or anxiety
- fatigue or drowsiness; a lack of energy or motivation
- changes in sleep patterns (e.g., sleeping a lot more or having difficulty falling or staying asleep); inability to wake up from sleep
Diagnosing traumatic brain injury in children can be challenging because they may be unable to let others know that they feel different. A child with a traumatic brain injury may display the following signs or symptoms:
- changes in eating or nursing habits
- persistent crying, irritability, or crankiness; inability to be consoled
- changes in ability to pay attention; lack of interest in a favorite toy or activity
- changes in the way the child plays
- changes in sleep patterns
- sadness or depression
- loss of a skill, such as toilet training
- loss of balance or unsteady walking
- vomiting
In some cases, repeated blows to the head can cause chronic traumatic encephalopathy (CTE) – a progressive neurological disorder associated with a variety of symptoms, including cognition and communication problems, motor disorders, problems with impulse control and depression, confusion, and irritability. Chronic traumatic encephalopathy occurs in those with extraordinary exposure to multiple blows to the head and as a delayed consequence after many years. Studies of retired boxers have shown that repeated blows to the head can cause a number of issues, including memory problems, tremors, and lack of coordination and dementia. Recent studies have demonstrated rare cases of chronic traumatic encephalopathy in other sports with repetitive mild head impacts (e.g., soccer, wrestling, football, and rugby). A single, severe traumatic brain injury also may lead to a disorder called post-traumatic dementia (PTD), which may be progressive and share some features with chronic traumatic encephalopathy. Studies assessing patterns among large populations of people with traumatic brain injury indicate that moderate or severe traumatic brain injury in early or mid-life may be associated with increased risk of dementia later in life.
Effects on consciousness
A traumatic brain injury can cause problems with arousal, consciousness, awareness, alertness, and responsiveness. Generally, there are four abnormal states that can result from a severe traumatic brain injury:
- Brain death – The lack of measurable brain function and activity after an extended period of time is called brain death and may be confirmed by studies that show no blood flow to the brain.
- Coma – A person in a coma is totally unconscious, unaware, and unable to respond to external stimuli such as pain or light. Coma generally lasts a few days or weeks after which an individual may regain consciousness, die, or move into a vegetative state.
- Vegetative state – A result of widespread damage to the brain, people in a vegetative state are unconscious and unaware of their surroundings. However, they can have periods of unresponsive alertness and may groan, move, or show reflex responses. If this state lasts longer than a few weeks it is referred to as a persistent vegetative state.
- Minimally conscious state – People with severely altered consciousness who still display some evidence of self-awareness or awareness of one’s environment (such as following simple commands, yes/no responses).
Blunt head trauma complications
Blunt head trauma complications include:
- Intracranial hemorrhage
- Brain edema
- Elevated intracranial pressure
- Vasospasm
- Seizures
- Infection
- Hydrocephalus
- Memory loss
- Hyponatremia
- Effects on consciousness:
- Brain death – The lack of measurable brain function and activity after an extended period of time is called brain death and may be confirmed by studies that show no blood flow to the brain.
- Coma – A person in a coma is totally unconscious, unaware, and unable to respond to external stimuli such as pain or light. Coma generally lasts a few days or weeks after which an individual may regain consciousness, die, or move into a vegetative state.
- Vegetative state – A result of widespread damage to the brain, people in a vegetative state are unconscious and unaware of their surroundings. However, they can have periods of unresponsive alertness and may groan, move, or show reflex responses. If this state lasts longer than a few weeks it is referred to as a persistent vegetative state.
- Minimally conscious state – People with severely altered consciousness who still display some evidence of self-awareness or awareness of one’s environment (such as following simple commands, yes/no responses).
Blunt head trauma diagnosis
The majority of patients with traumatic brain injury have a straightforward clinical presentation, but it is also important to solicit the mechanism of injury, current anticoagulation use, symptoms of head or neck pain, post-traumatic seizure, and any history of repeat head injury or past central nervous system surgeries.
Although the majority of traumatic brain injuries are mild they can still have serious health implications. Of greatest concern are injuries that can quickly grow worse. All traumatic brain injuries require immediate assessment by a professional who has experience evaluating head injuries. A neurological exam will assess motor and sensory skills and the functioning of one or more cranial nerves. It will also test hearing and speech, coordination and balance, mental status, and changes in mood or behavior, among other abilities. Screening tools for coaches and athletic trainers can identify the most concerning concussions for medical evaluation.
Initial assessments may rely on standardized instruments such as the Acute Concussion Evaluation form from the Centers for Disease Control and Prevention or the Sport Concussion Assessment Tool 2, which provide a systematic way to assess a person who has suffered a mild traumatic brain injury. Reviewers collect information about the characteristics of the injury, the presence of amnesia (loss of memory) and/or seizures, as well as the presence of physical, cognitive, emotional, and sleep-related symptoms. The Acute Concussion Evaluation is also used to track symptom recovery over time. It also takes into account risk factors (including concussion, headache, and psychiatric history) that can impact how long it takes to recover from a traumatic brain injury.
When necessary, medical providers will use brain scans to evaluate the extent of the primary brain injuries and determine if surgery will be needed to help repair any damage to the brain. The need for imaging is based on a physical examination by a doctor and a person’s symptoms.
Computed tomography (CT) is the most common imaging technology used to assess people with suspected moderate to severe traumatic brain injury. Non-contrast cranial CT is the imaging modality of choice for patients with traumatic brain injury. CT findings associated with a poor outcome in traumatic brain injury include midline shift, subarachnoid hemorrhage into the verticals, and compression of the basal cisterns. MRI may be indicated when the clinical picture remains unclear after a CT to identify more subtle lesions 14.
Magnetic resonance imaging (MRI) may be used after the initial assessment and treatment as it is a more sensitive test and picks up subtle changes in the brain that the CT scan might have missed.
Unlike moderate or severe traumatic brain injury, milder traumatic brain injury may not involve obvious signs of damage (hematomas, skull fracture, or contusion) that can be identified with current neuroimaging. Instead, much of what is believed to occur to the brain following mild traumatic brain injury happens at the cellular level. Significant advances have been made in the last decade to image milder traumatic brain injury damage. For example, diffusion tensor imaging (DTI) can image white matter tracts, more sensitive tests like fluid-attenuated inversion recovery (FLAIR) can detect small areas of damage, and susceptibility-weighted imaging very sensitively identifies bleeding. Despite these improvements, currently available imaging technologies, blood tests, and other measures remain inadequate for detecting these changes in a way that is helpful for diagnosing the mild concussive injuries.
Neuropsychological tests to gauge brain functioning are often used in conjunction with imaging in people who have suffered mild traumatic brain injury. Such tests involve performing specific cognitive tasks that help assess memory, concentration, information processing, executive functioning, reaction time, and problem solving. The Glasgow Coma Scale is the most widely used tool for assessing the level of consciousness after traumatic brain injury. The standardized 15-point test measures a person’s ability to open his or her eyes and respond to spoken questions or physical prompts for movement. A total score of 3-8 indicates a severe head injury; 9-12 indicates moderate injury; and 13-15 is classified as mild injury.
Many athletic organizations recommend establishing a baseline picture of an athlete’s brain function at the beginning of each season, ideally before any head injuries have occurred. Baseline testing should begin as soon as a child begins a competitive sport. Brain function tests yield information about an individual’s memory, attention, and ability to concentrate and solve problems. Brain function tests can be repeated at regular intervals (every 1 to 2 years) and also after a suspected concussion. The results may help health care providers identify any effects from an injury and allow them make more informed decisions about whether a person is ready to return to their normal activities.
Blunt head trauma treatment
Many factors, including the size, severity, and location of the brain injury, influence how a traumatic brain injury is treated and how quickly a person might recover. One of the critical elements to a person’s prognosis is the severity of the injury. Although brain injury often occurs at the moment of head impact, much of the damage related to severe traumatic brain injury develops from secondary injuries which happen days or weeks after the initial trauma. For this reason, people who receive immediate medical attention at a certified trauma center tend to have the best health outcomes 12.
Treating mild traumatic brain injury
Individuals with mild traumatic brain injury, such as concussion, should focus on symptom relief and “brain rest.” In these cases, headaches can often be treated with over-the-counter pain relievers. People with mild traumatic brain injury are also encouraged to wait to resume normal activities until given permission by a doctor. People with a mild traumatic brain injury should:
- Make an appointment for a follow-up visit with their health care provider to confirm the progress of their recovery.
- Inquire about new or persistent symptoms and how to treat them.
- Pay attention to any new signs or symptoms even if they seem unrelated to the injury (for example, mood swings, unusual feelings of irritability). These symptoms may be related even if they occurred several weeks after the injury.
Even after symptoms resolve entirely, people should return to their daily activities gradually. Brain functionality may still be limited despite an absence of outward symptoms. Very little is known about the long-term effects of concussions on brain function. There is no clear timeline for a safe return to normal activities although there are guidelines such as those from the American Academy of Neurology (https://www.aan.com/Guidelines/Home/GetGuidelineContent/586) and the American Medical Society for Sports Medicine (https://journals.lww.com/acsm-msse/Fulltext/2012/12000/The_Team_Physician_and_the_Return_to_Play.25.aspx) to help determine when athletes can return to practice or competition. Further research is needed to better understand the effects of mild traumatic brain injury on the brain and to determine when it is safe to resume normal activities.
Preventing future concussions is critical. While most people recover fully from a first concussion within a few weeks, the rate of recovery from a second or third concussion is generally slower.
In the days or weeks after a concussion, a minority of individuals may develop post-concussion syndrome. People can develop this syndrome even if they never lost consciousness. The symptoms include headache, fatigue, cognitive impairment, depression, irritability, dizziness and balance trouble, and apathy. These symptoms usually improve without medical treatment within one to a few weeks but some people can have longer lasting symptoms.
In some cases of moderate to severe traumatic brain injury, persistent symptoms may be related to conditions triggered by imbalances in the production of hormones required for the brain to function normally. Hormone imbalances can occur when certain glands in the body, such as the pituitary gland, are damaged over time as result of the brain injury. Symptoms of these hormonal imbalances include weight loss or gain, fatigue, dry skin, impotence, menstrual cycle changes, depression, difficulty concentrating, hair loss, or cold intolerance. When these symptoms persist 3 months after their initial injury or when they occur up to 3 years after the initial traumatic brain injury, people should speak with a health care provider about their condition.
Treating severe traumatic brain injury
Immediate treatment for the person who has suffered a severe traumatic brain injury focuses on preventing death; stabilizing the person’s spinal cord, heart, lung, and other vital organ functions; and preventing further brain damage. Persons with severe traumatic brain injury generally require a breathing machine to ensure proper oxygen delivery and breathing.
During the acute management period, health care providers monitor the person’s blood pressure, flow of blood to the brain, brain temperature, pressure inside the skull, and the brain’s oxygen supply. A common practice called intracranial pressure ICP monitoring involves inserting a special catheter through a hole drilled into the skull. Doctors frequently rely on ICP monitoring as a way to determine if and when medications or surgery are needed in order to prevent secondary brain injury from swelling. People with severe head injury may require surgery to relieve pressure inside the skull, get rid of damaged or dead brain tissue (especially for penetrating traumatic brain injury), or remove hematomas.
In-hospital strategies for managing people with severe traumatic brain injury aim to prevent conditions including:
- Infection, particularly pneumonia
- Deep vein thrombosis (DVT) (blood clots that occur deep within a vein; risk increases during long periods of inactivity)
People with traumatic brain injuries may need nutritional supplements to minimize the effects that vitamin, mineral, and other dietary deficiencies may cause over time. Some individuals may even require tube feeding to maintain the proper balance of nutrients.
Following the acute care period, people with severe traumatic brain injury are often transferred to a rehabilitation center where a multidisciplinary team of health care providers help with recovery. The rehabilitation team includes neurologists, nurses, psychologists, nutritionists, as well as physical, occupational, vocational, speech, and respiratory therapists.
Cognitive rehabilitation therapy is a strategy aimed at helping individuals regain their normal brain function through an individualized training program. Using this strategy, people may also learn compensatory strategies for coping with persistent deficiencies involving memory, problem solving, and the thinking skills to get things done. Cognitive rehabilitation therapy programs tend to be highly individualized and their success varies. A 2011 Institute of Medicine report concluded that cognitive rehabilitation interventions need to be developed and assessed more thoroughly.
Other factors that influence recovery
Genes
Evidence suggests that genetics play a role in how quickly and completely a person recovers from a traumatic brain injury. For example, researchers have found that apolipoprotein E ε4 (ApoE4) — a genetic variant associated with higher risks for Alzheimer’s disease — is associated with worse health outcomes following a traumatic brain injury. Much work remains to be done to understand how genetic factors, as well as how specific types of head injuries in particular locations, affect recovery processes. It is hoped that this research will lead to new treatment strategies and improved outcomes for people with traumatic brain injury.
Age
Studies suggest that age and the number of head injuries a person has suffered over his or her lifetime are two critical factors that impact recovery. For example, traumatic brain injury-related brain swelling in children can be very different from the same condition in adults, even when the primary injuries are similar. Brain swelling in newborns, young infants, and teenagers often occurs much more quickly than it does in older individuals. Evidence from very limited chronic traumatic encephalopathy studies suggest that younger people (ages 20 to 40) tend to have behavioral and mood changes associated with chronic traumatic encephalopathy, while those who are older (ages 50+) have more cognitive difficulties.
Compared with younger adults with the same traumatic brain injury severity, older adults are likely to have less complete recovery. Older people also have more medical issues and are often taking multiple medications that may complicate treatment (e.g., blood-thinning agents when there is a risk of bleeding into the head). Further research is needed to determine if and how treatment strategies may need to be adjusted based on a person’s age.
Researchers are continuing to look for additional factors that may help predict a person’s course of recovery.
Blunt head trauma prognosis
The outcome after blunt head trauma depends on the type of injury, the severity of the injury, patient age, the presence of any neurological deficit, comorbidity and any secondary injury. The GCS at 24 hours is a strong predictor of cognitive recovery at 24 months after the injury. The mortality rates do vary from 4-40% at five years after blunt head trauma. Younger people fare much better than older individuals. Individuals with a neurological deficit and those taking oral anticoagulants at the time of injury often have a poor outcome. The pupillary function before and after the injury is also predictive of outcome. Those with bilateral unresponsive pupils tend to have a grave prognosis and a higher risk of remaining in a vegetative state. Finally, studies show that diabetics also tend to fare worse with blunt head trauma compared to nondiabetics 15.
Blunt cardiac injury
Blunt cardiac injury is used to reflect injury to the heart after blunt chest trauma 16. Histologically, blunt cardiac injury was characterized by a contused myocardium, hemorrhagic infiltrate, localized necrosis, and edema 17. Because of the term’s ambiguity in describing a spectrum of myocardial injuries secondary to blunt trauma, “cardiac contusion” is now termed “blunt cardiac injury” 17. This is the term trauma experts agree is more appropriate since it encompasses the various types of cardiac injuries seen after blunt chest trauma 18. Blunt cardiac injury Injuries can range from clinically silent, transient arrhythmias to fatal cardiac rupture 19. Significant blunt cardiac injury usually occurs from high-impact trauma from motor vehicle accidents (50%), pedestrian struck by motor vehicles (35%), motorcycle crashes (9%), and falls from significant heights (6%) 20. Diagnosing blunt cardiac injury can be challenging as there is no accepted gold standard diagnostic testing. Blunt cardiac injury can be even more complicated in a patient with multiple traumas. The reported incidence of cardiac injury following blunt chest trauma is in the range of 8% to 76%; this reflects the lack of standardized diagnostic criteria 21.
In essence, myocardial tissue damage is the only way that blunt cardiac injury can be confirmed, either at surgery or autopsy 22. In the vast majority of cases, however, this option is not available, and the clinical and diagnostic tools available in our armamentarium are variable and nonspecific. More importantly, in the absence of severe arrhythmia and hemodynamic instability, the significance of blunt cardiac injury becomes more questionable despite the results of noninvasive studies 23. In the setting of blunt trauma, a high, clinical suspicion for blunt cardiac injury is warranted, and if suspicion is high enough, patients should be monitored for adverse sequelae since there are no pathognomonic clinical signs or symptoms that correlate with the risk of cardiac complications 20. Indeed, it is the complications of blunt cardiac injury that is of importance and not necessarily its label.
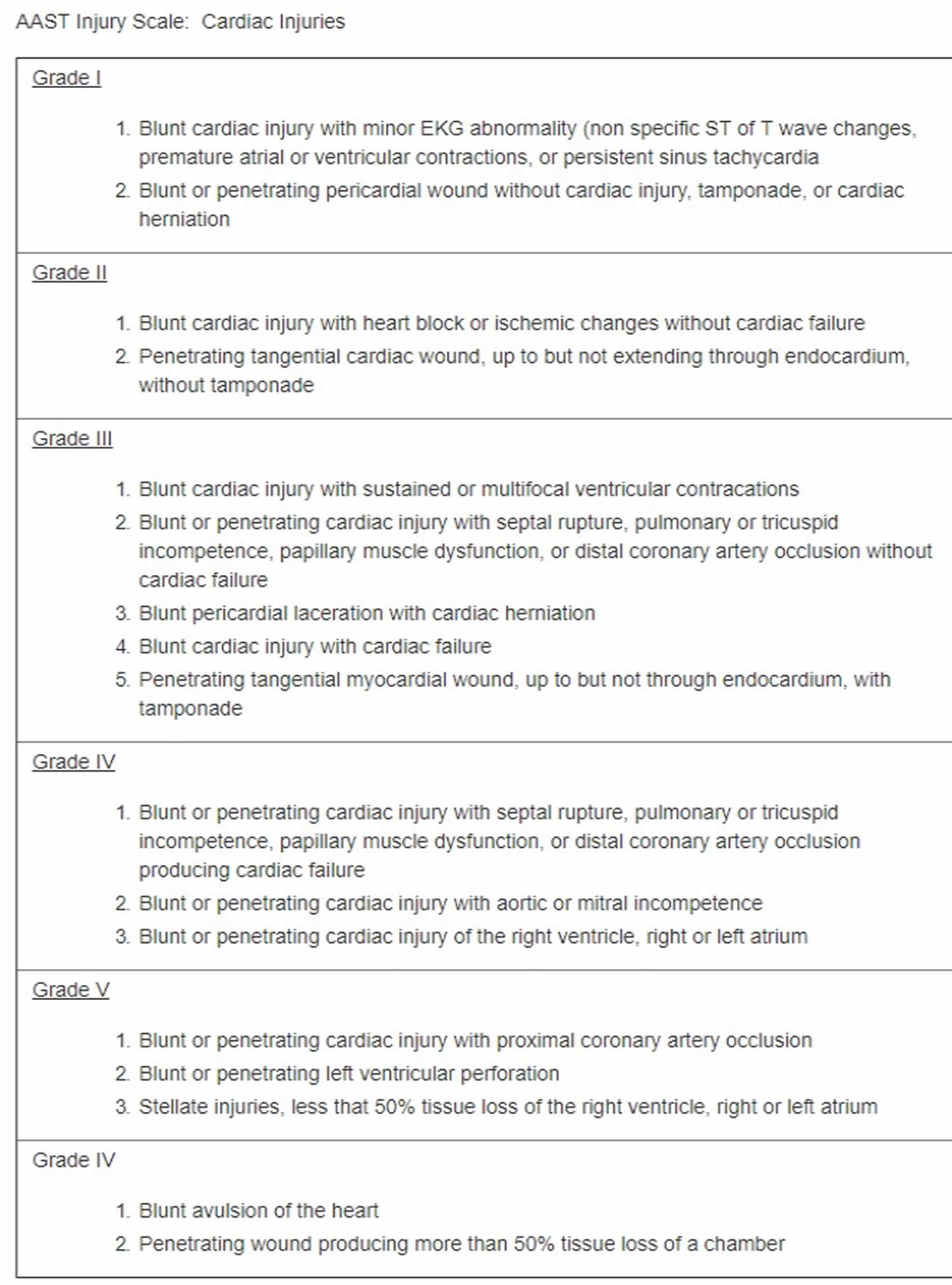
The incidence of blunt cardiac injury has a broad range (8% to 76%) 21 because of the lack of a clear, accepted diagnostic criteria, lack of consensus on the definition, and the inconsistency of nomenclature that makes it difficult to quantify the incidence. Diagnosis can be based on symptoms that are not necessarily related to blunt cardiac injury while some blunt cardiac injury complications, like arrhythmias, can be due to pre-existing heart conditions-particularly in the elderly population. Diagnostic criteria, like elevated troponins, can also be due to trauma unrelated to the chest 24. In the United States, trauma is the 4th leading cause of death. The American Association for the Surgery of Trauma (AAST) developed the AAST Cardiac Injury Scale that applies to blunt and penetrating cardiac injuries to use when quantifying cardiac injuries (see Table 1). Note: When using the table, advance one grade for multiple penetrating wounds to a single chamber or multiple chamber involvement.
Table 1. American Association for the Surgery of Trauma – Cardiac Injury Scale
Blunt cardiac injury causes
Blunt cardiac injury from blunt chest trauma is most commonly due to motor vehicle collisions (50%), with 20% of all motor vehicle collision deaths involving blunt chest trauma 18. Other mechanisms such as falls, blast injuries, assault, and other blunt mechanisms also play a role 16. The mechanism and magnitude of force determine the cardiac injury that is sustained. The heart sits in the thorax where it is caged in by the sternum, ribs, and spine; therefore, a significant amount of force is needed to result in blunt cardiac injury. Nevertheless, there can be a direct impact to the chest, resulting in compression of the heart between the sternum and spine. In the setting of a deceleration injury, the heart can tear from its attachments as it hits the bony thoracic cage. Most often, these types of injuries are not survivable, with the patients not even make it to the hospital. Although blunt cardiac injury has been associated with multiple other injuries, such as thoracic aorta, lung, rib, or sternal fractures and spinal injuries, none of those injuries are specific enough to be highly suggestive of blunt cardiac injury 25. Associated injuries only raise the index of suspicion for the provider who should be alerted to the possibility of blunt cardiac injury, but they are not pathognomonic and, most often, are not indicative of blunt cardiac injury.
Six potential mechanisms have been suggested for blunt cardiac injury: direct, indirect, bidirectional, deceleration, blast, crush, concussive, or combined 18. Direct impact to the chest is considered the most common mechanism, and cardiac injury is most likely when the ventricles are maximally distended at the end of diastole 20. Indirect cause is due to an increase in preload by way of abdominal or extremity veins that results in a sudden increase in the intracardiac pressure, thereby making the heart susceptible to rupture 20. Bidirectional forces result in compression of the heart between the spine and sternum 20. Deceleration mechanisms allow the heart to move freely, resulting in valvular, myocardial, coronary artery tears, or laceration 20.
The cardiac chamber injury distribution reflects the position of the heart in the chest where the right ventricle and right atrium are more anterior compared to the left ventricle and left atrium 20.
The most common cardiac injuries from blunt trauma resulting in death are often due to one or more cardiac chamber rupture (64%), venous-atrial confluence tears (33%), or coronary artery tear or dissection 25.
Of note, commotio cordis is sudden death due to cardiac arrest from blunt cardiac injury in the absence of preexisting disease and with no morphological injury to the heart at autopsy. It is usually seen in the young, male athlete. The thought process is that the impact occurs during ventricular repolarization and sets the heart to ventricular fibrillation 18.
Most patients who survive blunt cardiac injury due to blunt trauma have less severe injuries that range from structural injuries to electrical and conduction disturbances 25. An intramural hematoma is one such structural injury that, for the most part, has a benign clinical course that resolves in 4 to 12 weeks. It can cause premature ventricular contraction (PVC) and transient bundle branch block (BBB). Another common structural injury is papillary muscle rupture that can lead to regurgitation of the valves and require valve repair or salvage 25. On clinical exam, septal injuries can present with a murmur or arrhythmias on echocardiogram (ECG). The course of this injury begins with contusion followed by necrosis and then delayed rupture. Hence, early diagnosis is important as it can be treatable if discovered 20. Dysrhythmias are fairly common in blunt cardiac injury and, most commonly, are evident by sinus tachycardia on ECG followed by premature atrial or ventricular contractions, atrial fibrillation, and BBBs 18. The most common cardiac abnormality seen in blunt cardiac injury is tachycardia; however, most ECG changes have been noted to be clinically irrelevant 25. That finding does not relinquish the importance of monitoring these patients closely because most trauma patients will exhibit tachycardia on initial assessment, and ECG with persistent tachycardia is more suggestive of blunt cardiac injury rather than the transient tachycardia seen in the patient who is polytraumatized. Health care provider should also realize, however, that tachycardia in the trauma patient should raise greater suspicion of ongoing bleeding than blunt cardiac injury. Once bleeding is ruled out, blunt cardiac injury becomes more probable in the differential diagnosis.
Blunt cardiac injury symptoms
It is important to first identify the trauma patient with blunt chest injury by the mechanism of force. For instance, patients involved in an motor vehicle collision should be queried on whether there was a steering wheel impact. Furthermore, 54% of patients with a history of a fall greater than 20 feet had blunt cardiac injury 25.
The most common complaint is chest pain or shortness of breath 18, but some may report palpitations or even present with typical angina symptoms 18. It is also important to assess for cardiac risk factors such as a history of myocardial infarction, cardiovascular disease, and/or comorbidities. Medication assessment is important, especially in the patient taking cardiac drugs which can alter the patient presentation such as beta blockers and calcium channel blockers (which can mask tachycardia).
The physical exam should be thorough. Patients can present with cardiac tamponade, and suspicion should be high for jugular venous distention and hypotension. The focused assessment with sonography for trauma (FAST exam) will help in the assessment for pericardial fluid and cardiac tamponade. Tachypnea, irregular lung sounds, chest wall tenderness, chest abrasion or ecchymosis, rib or sternal fractures, and seatbelt sign across the chest are some of the physical findings that should raise suspicion for blunt cardiac injury 26, although they are non-specific 18. Furthermore, patients with severe blunt cardiac injury are more likely to have other significant traumatic injuries that can mask some of the physical effects of blunt cardiac injury 27.
Blunt cardiac injury complications
Overall, complications from blunt cardiac trauma are rare 25. Acute complications from severe cardiac injury usually necessitate immediate management, and those that survive may have long-term complications related to their specific injury. Most blunt cardiac injury patients, do not have long-term sequelae, but a few, late complications have been reported, including delayed cardiac rupture, complete atrioventricular block, heart failure, pericardial effusion, and constrictive pericarditis 25. Therefore, good practice entails reevaluating these patients in 3 to 6 months 25.
Blunt cardiac injury diagnosis
No consensus has been established to diagnose blunt cardiac injuries. In 2012, the Eastern Association of Trauma (EAST) published blunt cardiac injury practice guidelines that supported obtaining an ECG in all patients with suspected blunt cardiac injury 20. Patients with abnormal findings should be admitted for continuous cardiac monitoring; however, a normal ECG does not entirely exclude blunt cardiac injury as it has been reported that a significant number of patients with an initial normal ECG were noted to have a cardiac injury 24 hours later, measured by laboratory results of elevated cardiac troponin I (cTnI) levels 20. Nevertheless, patients with a normal ECG in conjunction with normal levels of cTnI can be safely discharged home 20. Furthermore, it should be noted that a normal ECG and cardiac troponin I levels do not rule out all blunt cardiac injury as some may have a delayed presentation (e.g., septal injury). Following an abnormal ECG and cTnI level, an echocardiography is usually obtained to further characterize the injury. Computerized tomography (CT) and magnetic resonance imaging (MRI) do not play a role in the initial diagnostic evaluation of blunt cardiac injury; however, these modalities can be complementary or useful in the patient with symptoms without a clear clinical etiology and can be considered on a case-by-case basis 20.
Blunt cardiac injury treatment
Patients with abnormal ECG and/or cardiac troponin I (cTnI) levels should be admitted for cardiac monitoring for 24 to 48 hours because life-threatening arrhythmias or cardiac failure will most likely present during this time 18. Patients can be admitted to the intensive care unit or placed under telemetry, depending on concurrent injuries, type of ECG change, and the grade of hemodynamic imbalance. It is not necessary to admit all sternal fractures with a normal ECG to rule out blunt cardiac injury. The most prevalent of the blunt cardiac injurys are the subset of patients with isolated abnormal ECG and/or cardiac troponin I elevations which usually has a benign course with the rare occurrence of long-term functional impairment 16.
Management of dysrhythmias should be approached and treated as in the non-blunt cardiac injury patient. Replete electrolytes accordingly, avoid hypoxia and acidosis, and utilize antidysrhythmics and any additional intervention or defibrillation if clinically indicated. Although rare with isolated blunt cardiac injury, the occasional patient may present with complete heart block, necessitating a pacemaker. ST segment elevations can be due to either a contused heart or traumatic myocardial infarction, necessitating coronary angiography 18.
Patients with severe clinical or imaged structural cardiac injury require emergent cardiology evaluation for further management. Temporizing measures such as resuscitation, inotropes, or vasopressors may be indicated in the interim based on the specific clinical findings and associated injuries. A patient presenting with high suspicion for cardiac tamponade, most frequently seen in cardiac rupture, will benefit from surgical intervention as an emergency 18. Cardiothoracic intervention is required and time is of the essence in the majority of those cases. Refractory cardiogenic shock can benefit from intra-aortic balloon pump (IABP) to help increase coronary blood flow, allowing the stunned heart to recover in days or weeks 16.
Blunt cardiac injury prognosis
Prognosis in blunt cardiac injury is highly dependent on the specified injury and its association with concomitant injuries and a history of previous cardiac disease or injuries 27. The patient with isolated blunt cardiac injury that is presented by way of an abnormal ECG or cardiac troponin I level has a more favorable outcome than the patient who is hemodynamically compromised with cardiac structural injury one who has an associated high trauma injury score 25. Given that the former represents the largest pool of blunt cardiac injury patients, blunt cardiac injury can be presumed to have a favorable prognosis overall.
Blunt eye trauma
Blunt eye trauma can result in eyelid to orbital injury.
Blunt eye trauma key points
- Consult an ophthalmologist if an eyelid laceration is complicated (eg, through the margin, tarsal plate, or canaliculus, causing ptosis, or exposing orbital fat).
- Globe trauma may cause globe laceration, cataract, lens dislocation, glaucoma, vitreous hemorrhage, or retinal damage (hemorrhage, detachment, or edema).
- Suspect globe rupture if trauma results in a visible corneal or scleral laceration, leaking aqueous humor, an unusually shallow or deep anterior chamber, or an irregular pupil.
- Hyphema, best diagnosed by slit-lamp examination, requires bed rest with head elevation at 30 to 45° and close monitoring of intraocular pressure.
- Refer patients for surgical repair of blowout fractures that cause diplopia or unacceptable enophthalmos.
- Do immediate lateral canthotomy on patients with orbital compartment syndrome.
Eyelids injury
Eyelid contusions which result in black eyes are more cosmetically than clinically significant, although more serious injuries may sometimes accompany them and should not be overlooked. Uncomplicated contusions are treated with ice packs to inhibit swelling during the first 24 to 48 hours.
Minor eyelid lacerations not involving the lid margin or tarsal plate may be repaired with nylon (or, in children, plain gut) 6-0 or 7-0 sutures. Lacerations of the lid margin are best repaired by an ophthalmic surgeon to ensure accurate apposition and to avoid a notch in the contour. Complicated lid lacerations, which include those of the medial portion of the lower or upper eyelid (possibly involving the lacrimal canaliculus), through-and-through lacerations, those in which the patient has ptosis, and those that expose orbital fat or involve the tarsal plate, should also be repaired by an ophthalmic surgeon.
Eye injury
Globe trauma may cause the following:
- Conjunctival, anterior chamber, and vitreous hemorrhage
- Retinal hemorrhage, edema, or retinal detachment
- Laceration of the iris
- Cataract
- Dislocated lens
- Glaucoma
- Globe rupture (laceration)
Evaluation can be difficult when massive lid edema or laceration is present. Even so, unless the need for immediate eye surgery is obvious (necessitating evaluation by an ophthalmologist as soon as possible), the lid is opened, taking care not to exert pressure on the globe, and as complete an examination as possible is conducted. At a minimum, the following are noted:
- Visual acuity
- Pupil shape and pupillary responses
- Extraocular movements
- Anterior chamber depth or hemorrhage
- Presence of red reflex
An analgesic or after obtaining any surgical consent, an anxiolytic may be given to facilitate examination. Gentle and careful use of eyelid retractors or an eyelid speculum makes it possible to open the lids. If a commercial instrument is not available, the eyelids can be separated with makeshift retractors fashioned by opening a paperclip to an S shape, then bending the U-shaped ends to 180°. Globe laceration should be suspected with any of the following:
- A corneal or scleral laceration is visible.
- Aqueous humor is leaking (positive Seidel sign).
- The anterior chamber is very shallow (eg, making the cornea appear to have folds) or very deep (due to rupture posterior to the lens).
- The pupil is irregular.
- The red reflex is absent.
If globe laceration is suspected, measures that can be taken before an ophthalmologist is available consist of applying a protective shield and combating possible infection with systemic antimicrobials as for intraocular foreign bodies. Topical antibiotics are avoided. Vomiting, which can increase intraocular pressure (IOP) and contribute to extravasation of ocular contents, is suppressed using antiemetics as needed. Because fungal contamination of open wounds is dangerous, corticosteroids are contraindicated until after wounds are closed surgically. Tetanus prophylaxis is indicated for open globe injuries. Very rarely, after laceration of the globe, the uninjured, contralateral eye becomes inflamed (sympathetic ophthalmia) and may lose vision to the point of blindness unless treated. The mechanism is an autoimmune reaction; corticosteroid drops can prevent the process and may be prescribed by an ophthalmologist.
Hyphema (anterior chamber hemorrhage)
Hyphema may be followed by recurrent bleeding, glaucoma, and blood staining of the cornea, any of which may result in permanent vision loss. Symptoms are of associated injuries unless the hyphema is large enough to obstruct vision. Direct inspection typically reveals layering of blood or the presence of clot or both in the anterior chamber. Layering is seen as a meniscus-like blood level in the dependent (usually inferior) part of the anterior chamber. Microhyphema, a less severe form, may be detectable by direct inspection as haziness in the anterior chamber or by slit-lamp examination as suspended red blood cells.
An ophthalmologist should attend to the patient as soon as possible. The patient is placed on bed rest with the head elevated 30 to 45° and is given an eye shield to protect the eye from further trauma (see Corneal Abrasions and Foreign Bodies). Patients who are at high risk of recurrent bleeding (eg, those with large hyphemas, bleeding diatheses, anticoagulant use, or sickle cell disease), who have intraocular pressure (IOP) that is difficult to control, or who are likely to be nonadherent to recommended treatment may be hospitalized. Oral and topical nonsteroidal anti-inflammatory drugs (NSAIDs) are contraindicated because they may contribute to recurrent bleeding.
Intraocular pressure (IOP) can rise acutely (within hours, usually in patients with sickle cell disease or trait) or months to years later. Thus, IOP is monitored daily for several days and then regularly over subsequent weeks and months and if symptoms develop (eg, eye ache, decreased vision, nausea—similar to symptoms of acute angle-closure glaucoma). If pressure rises, timolol 0.5% twice a day, brimonidine 0.2% or 0.15% twice a day, or both are given. Response to treatment is determined by pressure, often checked every 1 or 2 hours until controlled or until a significant rate of reduction is demonstrated; thereafter, it is usually checked once or twice daily. Mydriatic drops (eg, scopolamine 0.25% 3 times a day or atropine 1% three times a day for 5 days) and topical corticosteroids (eg, prednisolone acetate 1% four to 8 times a day for 2 to 3 weeks) are often given to reduce inflammation and scarring.
If bleeding is recurrent, an ophthalmologist should be consulted for management. Administration of aminocaproic acid 50 to 100 mg/kg orally every 4 hours (not exceeding 30 g/day) for 5 days or transexamic acid 25 mg/kg administered 3 times daily for 5 to 7 days may reduce recurrent bleeding, and miotic or mydriatic drugs must also be given. Rarely, recurrent bleeding with secondary glaucoma requires surgical evacuation of the blood.
Blowout fracture
Blowout fracture occurs when blunt trauma forces the orbital contents through one of the most fragile portions of the orbital wall, typically the floor. Medial and roof fractures also can occur. Orbital hemorrhage can cause or contribute to complications, such as inferior displacement of the globe, entrapment of the infraorbital nerve, lid edema, and ecchymosis. Patients may have facial or orbital pain, diplopia, enophthalmos, hypesthesia of the cheek and upper lip (due to infraorbital nerve entrapment or injury), epistaxis, and subcutaneous emphysema. Other facial fractures or injuries must also be ruled out. Diagnosis is best made using CT with thin cuts through the facial bones. If ocular motility is impaired (eg, causing diplopia), extraocular muscles should be assessed for signs of entrapment. If there is diplopia or cosmetically unacceptable enophthalmos, surgical repair may be indicated. Patients should be told to avoid blowing the nose to prevent orbital compartment syndrome from air reflux. Using a topical vasoconstrictor for 2 to 3 days may alleviate epistaxis. Oral antibiotics should be used if patients have sinusitis.
Orbital compartment syndrome
Orbital compartment syndrome is an ophthalmic emergency. Orbital compartment syndrome occurs when intraocular pressure (IOP) increases suddenly, usually due to trauma that causes hemorrhage (often in the orbit). Symptoms can include sudden vision loss, as well as diplopia, eye pain, and/or swelling. Physical exam findings may include decreased vision, chemosis, afferent pupillary defect, proptosis, and elevated intraocular pressure. Diagnosis is clinical and treatment should not be delayed for imaging. Treatment is immediate lateral canthotomy followed by:
- Monitoring with possible inpatient hospitalization with elevation of the bed to 45°
- Treatment of elevated IOP as in acute angle-closure glaucoma
- Reversal of any coagulopathy
- Prevention of further increasing intraocular pressure (preventing or minimizing pain, nausea, cough, straining, severe hypertension).
- Vester MEM, Bilo RAC, Loeve AJ, van Rijn RR, van Zandwijk JP. Modeling of inflicted head injury by shaking trauma in children: what can we learn? : Part I: A systematic review of animal models. Forensic Sci Med Pathol. 2019 Sep;15(3):408-422.
- Simon LV, Lopez RA, King KC. Blunt Force Trauma. [Updated 2019 Dec 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470338
- Gentile S, Kneubuehl BP, Barrera V, Dobay A, Thali MJ, Bolliger SA. Fracture energy threshold in parry injuries due to sharp and blunt force. Int. J. Legal Med. 2019 Sep;133(5):1429-1435.
- Keane M. Triad of death: the importance of temperature monitoring in trauma patients. Emerg Nurse. 2016 Sep;24(5):19-23.
- O’Toole JE, Kaiser MG, Anderson PA, Arnold PM, Chi JH, Dailey AT, Dhall SS, Eichholz KM, Harrop JS, Hoh DJ, Qureshi S, Rabb CH, Raksin PB. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Evaluation and Treatment of Patients with Thoracolumbar Spine Trauma: Executive Summary. Neurosurgery. 2019 Jan 01;84(1):2-6.
- Sears BW, Luchette FA, Esposito TJ, Dickson EL, Grant M, Santaniello JM, Jodlowski CR, Davis KA, Poulakidas SJ, Gamelli RL. Old fashion clinical judgment in the era of protocols: is mandatory chest X-ray necessary in injured patients? J Trauma. 2005 Aug;59(2):324-30; discussion 330-2.
- Lee JK, Brady KM, Deutsch N. The Anesthesiologist’s Role in Treating Abusive Head Trauma. Anesth. Analg. 2016 Jun;122(6):1971-82.
- Yeung LL, McDonald AA, Como JJ, Robinson B, Knight J, Person MA, Lee JK, Dahm P. Management of blunt force bladder injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2019 Feb;86(2):326-336.
- Haydel MJ, Burns B. Blunt Head Trauma. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430770
- Abolfotouh MA, Hussein MA, Abolfotouh SM, Al-Marzoug A, Al-Teriqi S, Al-Suwailem A, Hijazi RA. Patterns of injuries and predictors of inhospital mortality in trauma patients in Saudi Arabia. Open Access Emerg Med. 2018;10:89-99.
- Lamb LC, DiFiori M, Comey C, Feeney J. Cost Analysis of Direct Oral Anticoagulants Compared with Warfarin in Patients with Blunt Traumatic Intracranial Hemorrhages. Am Surg. 2018 Jun 01;84(6):1010-1014.
- Traumatic Brain Injury: Hope Through Research. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Traumatic-Brain-Injury-Hope-Through
- Leetch AN, Wilson B. Pediatric Major Head Injury: Not a Minor Problem. Emerg. Med. Clin. North Am. 2018 May;36(2):459-472.
- Masterson Creber RM, Dayan PS, Kuppermann N, Ballard DW, Tzimenatos L, Alessandrini E, Mistry RD, Hoffman J, Vinson DR, Bakken S., Pediatric Emergency Care Applied Research Network (PECARN) and the Clinical Research on Emergency Services and Treatments (CREST) Network. Applying the RE-AIM Framework for the Evaluation of a Clinical Decision Support Tool for Pediatric Head Trauma: A Mixed-Methods Study. Appl Clin Inform. 2018 Jul;9(3):693-703.
- Watanabe T, Kawai Y, Iwamura A, Maegawa N, Fukushima H, Okuchi K. Outcomes after Traumatic Brain Injury with Concomitant Severe Extracranial Injuries. Neurol. Med. Chir. (Tokyo). 2018 Sep 15;58(9):393-399.
- Elie MC. Blunt cardiac injury. Mt. Sinai J. Med. 2006 Mar;73(2):542-52.
- Singh S, Angus LD. Blunt Cardiac Injury. [Updated 2019 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532267
- Marcolini EG, Keegan J. Blunt Cardiac Injury. Emerg. Med. Clin. North Am. 2015 Aug;33(3):519-27.
- Skinner DL, Laing GL, Rodseth RN, Ryan L, Hardcastle TC, Muckart DJ. Blunt cardiac injury in critically ill trauma patients: a single centre experience. Injury. 2015 Jan;46(1):66-70.
- Huis In ‘t Veld MA, Craft CA, Hood RE. Blunt Cardiac Trauma Review. Cardiol Clin. 2018 Feb;36(1):183-191.
- Leite L, Gonçalves L, Nuno Vieira D. Cardiac injuries caused by trauma: Review and case reports. J Forensic Leg Med. 2017 Nov;52:30-34.
- Hammer MM, Raptis DA, Cummings KW, Mellnick VM, Bhalla S, Schuerer DJ, Raptis CA. Imaging in blunt cardiac injury: Computed tomographic findings in cardiac contusion and associated injuries. Injury. 2016 May;47(5):1025-30.
- Kalbitz M, Pressmar J, Stecher J, Weber B, Weiss M, Schwarz S, Miltner E, Gebhard F, Huber-Lang M. The Role of Troponin in Blunt Cardiac Injury After Multiple Trauma in Humans. World J Surg. 2017 Jan;41(1):162-169.
- Martin M, Mullenix P, Rhee P, Belzberg H, Demetriades D, Salim A. Troponin increases in the critically injured patient: mechanical trauma or physiologic stress? J Trauma. 2005 Nov;59(5):1086-91.
- Yousef R, Carr JA. Blunt cardiac trauma: a review of the current knowledge and management. Ann. Thorac. Surg. 2014 Sep;98(3):1134-40.
- Salim A, Velmahos GC, Jindal A, Chan L, Vassiliu P, Belzberg H, Asensio J, Demetriades D. Clinically significant blunt cardiac trauma: role of serum troponin levels combined with electrocardiographic findings. J Trauma. 2001 Feb;50(2):237-43.
- Sybrandy KC, Cramer MJ, Burgersdijk C. Diagnosing cardiac contusion: old wisdom and new insights. Heart. 2003 May;89(5):485-9.