What is branchial cleft cyst
Branchial cleft cyst is a developmental cyst or cavities containing fluid that is formed within the neck that is congenital (present from birth), that occurs during early embryonic development when the structures and tissues that form the neck and throat do not properly grow together 1. The tissues form pockets and pathways that contain cells from other parts of the neck and throat. Branchial cleft cysts are lined with skin and lymph cells and contain fluid that is secreted by these cells. Branchial cleft fistulas also contain skin cells but drain mucus and fluids from other internal areas of the neck and throat.
Branchial cleft cysts are the most common neck masses in adults 2. The term “branchial cleft cyst” refers to the lesions which can be considered synonymous with the cervical lymphoepithelial cyst 3.
Branchial cleft cyst, although relatively rare, is the second major cause of head and neck pathology in childhood. Of the congenital masses related to embryonic remnants, approximately 70% are thyroglossal duct sinuses and cysts, 25% are branchial cysts and sinuses, and 5% are cystic hygromas 1.
The vast majority (90 %) of branchial malformations arise from the second cleft. Second branchial cleft cysts have been divided into four classes by Bailey classification 4. Second branchial cleft cysts can be bilateral and the present as soft, mobile, asymptomatic masses covered with normal skin. Second branchial cleft cysts are generally located along the anterior edge of the sternocleidomastoid muscle although they can develop anywhere along the course of second branchial cleft fistulae, from the skin on the lateral region of the neck, between the internal and external carotid arteries, to the palatine tonsils 5. Second branchial cleft cysts grow slowly over periods of weeks to years. Depending on the size (which ranges from 1 to 10 cm) and location, they can produce local symptoms such as dysphagia (difficulty swallowing), dysphonia (hoarse voice), dyspnea (difficulty breathing), and stridor (noisy breathing). Second branchial cleft cysts can become painful or tender secondary to infection, with suppuration and fistula formation. They contain a viscous, turbid, yellow-green liquid with cholesterine crystals in the sediment. The walls are thin and coated with the stratified squamous non-keratinized epithelium that covers the lymphoid tissue. The differential diagnosis includes parapharyngeal masses, such as enlarged lymph nodes, parotid masses, paragangliomas of the vagus nerve.
Various theories have been proposed regarding the origin of the branchial cleft cyst. Ascherson 6, in his “branchial theory”, suggested that incomplete obliteration of branchial cleft mucosa, which remains dormant until stimulated to grow later in life, results in cyst formation. Since then, a number of investigators have reinforced this link between the pharyngeal arches and the branchial cyst 7.
Branchial cleft cysts may arise from remnants of the first, second or third branchial arches; these are categorized in Table 1. Most branchial cleft cysts are of second branchial arch origin and are commonly found in the anterior triangle of the neck anterior to the upper third of the sternocleidomastoid muscle at the mandibular angle 8. These have rarely been reported in the lower third of the sternocleidomastoid and in the posterior triangle of the neck 9. Rarely branchial cysts may be present in the parapharyngeal space. The parapharyngeal space is a deep potential neck space, with inverted pyramid in shape and extends from the base of the skull to the hyoid bone below.
Table 1. Types of branchial cleft cyst
| Type of cyst | Branchial arch | Occurrence | Location |
| First branchial cleft cyst | First branchial arch | 8% | Type I: near external auditory canal or in parotid gland or at angle of mandible Type II: associated with submandiublar gland OR in the anterior triangle of neck |
| Second branchial cleft cyst | Second branchial arch | 95% | Along anterior border of upper third of sternocleidomastoid anywhere from skin of <1?show=[sr]?>lateral neck, between the internal and external carotid arteries and into the palatine tonsil |
| Third branchial cleft cyst | Third branchial arch | 2%—rare | Deep inside the sternocleidomastoid, may be with fistulous tract into larynx |
| Fourth branchial cleft cyst | Fourth branchial arch | Very rare | Arises from lateral neck and parallels recurrent laryngeal nerve. Various locations (including mediastinum) |
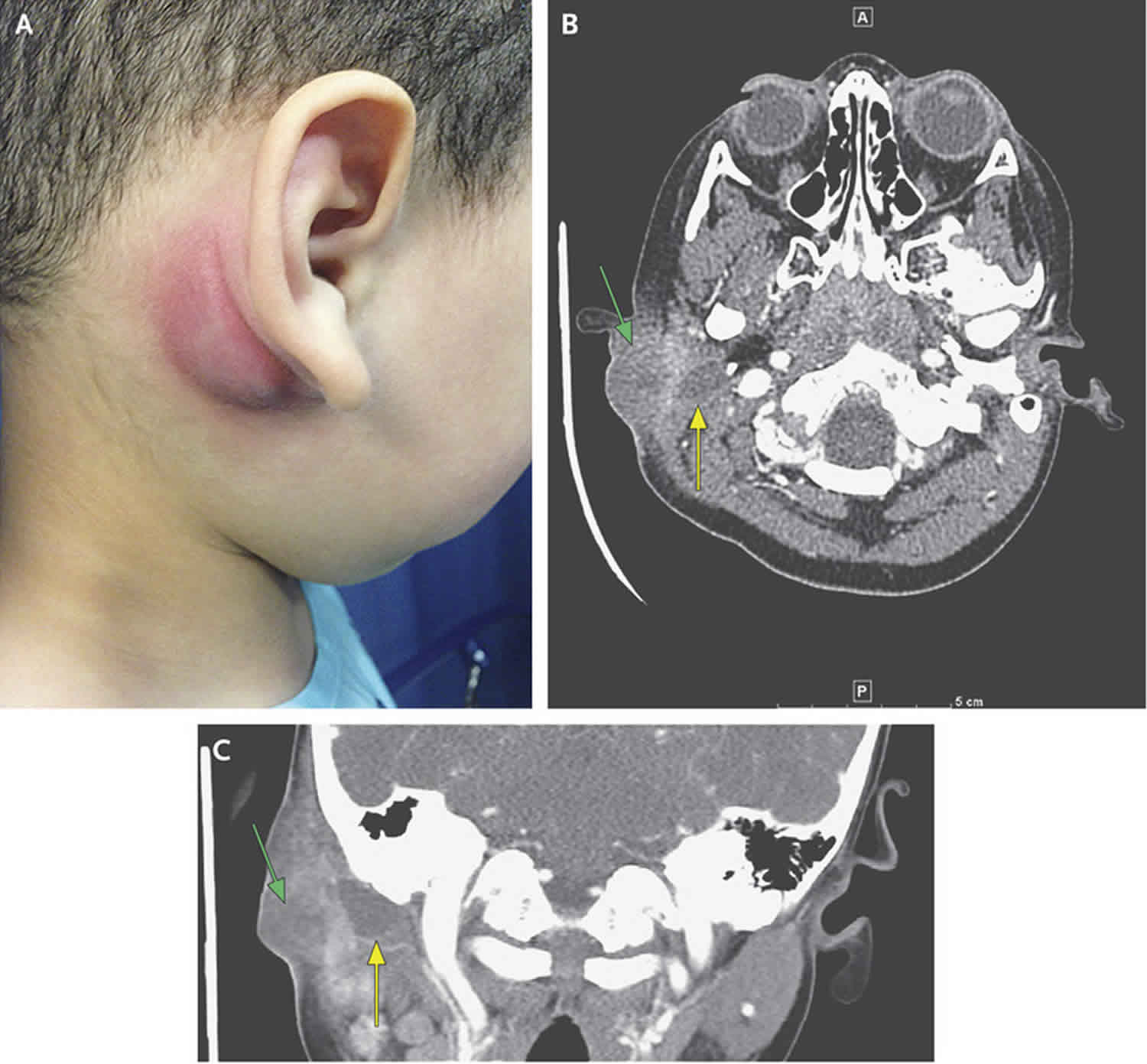
Figure 1. Branchial cleft cyst
Footnotes: A 3-year-old boy presented to the emergency department with pain in the right ear and swelling in the postauricular area that had begun 3 days earlier. His father reported that the boy had had a whitish discharge from his right ear 8 days earlier, for which a pediatrician had prescribed antibiotic eardrops. The patient had no fever or leukocytosis. On physical examination, the swollen postauricular area was fluctuant and tender (Panel A), and white secretions were observed in the external auditory canal. A computed tomographic scan of the temporal bone (Panels B and C) showed a hypointense cystic fluid collection (yellow arrows) with adjacent inflammation (green arrows) in the perimastoid area. There was no evidence of an infectious process in the middle ear or mastoid area. The patient was taken to the operating room, where examination of the right external auditory canal revealed a small fistula track, which raised suspicion of a first branchial cleft cyst. When gentle pressure was applied to the swollen postauricular area, keratin debris and purulence were expressed through the tract and into the osteocartilaginous junction of the ear canal (see video). In a child who presents with a neck mass, the diagnosis of a branchial cleft anomaly should be considered in addition to inflammatory, infectious, congenital, and neoplastic processes. Branchial cleft defects can manifest as cysts, sinuses, or fistulas. Branchial clefts are categorized into first, second, and third branchial cleft defects, depending on the location of the defect. First branchial cleft anomalies account for less than 10% of all branchial cleft defects; have close involvement with the external auditory canal, the facial nerve, or both; and are typically located in the periauricular area. Approximately 6 weeks after presentation, the cyst was excised in the operating room. On follow-up, the surgical site was well healed, and the patient has not had any further issues.
[Source 11 ]Branchial cleft cyst types
First branchial cleft cyst
First branchial cleft cysts are a type of branchial cleft anomaly. They are uncommon and represent only ~7% of all branchial cleft cysts.
First branchial cleft cysts are typically well-defined cystic masses located superficial to, within, or deep to the parotid gland. If they form a sinus, the sinus tract can be identified draining into the external auditory canal or even extending to the hyoid bone.
First branchial cleft cysts are usually diagnosed in middle-aged women 12.
First branchial cleft cyst subtypes
First branchial cleft cysts can be divided into three types based on location:
- Type I: inferoposteromedial to the pinna (near external auditory canal or in parotid gland or at angle of mandible)
- type II: associated with submandiublar gland OR in the anterior triangle of neck (between the angle of the mandible and the external auditory canal)
- type III: periparotid
First branchial cleft cysts can also be classified based on histology:
Type I
- purely ectodermal
- extremely rare
- appear histologically as cysts lined by squamous epithelium
- presents as a cystic mass or fistula posterior to the pinna
- usually located superior to the main trunk of the facial nerve and ends in a cul-de-sac on or near a bony plate at the level of the mesotympanum
Type II
- contain ectodermal and mesodermal elements
- comparatively common
- represent a duplication of both membranous and cartilaginous portions of the external auditory canal
- contain skin as well as adnexal structures and cartilage
- may be associated with the parotid gland
- often associated with fistulae in the concha or external auditory canal +/- fistulous openings in the neck
- incorporates some portion of the first and second arch as well as the cleft
First branchial cleft cyst signs and symptoms
First branchial cleft cysts presentation can in the form of 13:
- asymptomatic, e.g. incidental finding on imaging
- a palpable lump or inflammatory mass in the parotid region
- spontaneous fluid draining from a pit-like depression on the skin, which may be mucus or pus depending on the presence of associated infection
- facial nerve palsy 12
Second branchial cleft cyst
Second branchial cleft cysts are a cystic dilatation of the remnant of the 2nd branchial apparatus, and along with 2nd branchial fistulae and sinuses accounts for 95% of all branchial cleft anomalies.
Second branchial cleft cyst is typically filled with mucoid material, is well circumscribed and other than presenting as localized swelling, is asymptomatic. However, if infected, surrounding fat stranding and skin changes are evident.
Second branchial clefts can occur anywhere along the course of the second branchial apparatus, from the pharyngeal wall to the skin, as it passes laterally and inferiorly between the internal and external carotid arteries. The angle of the mandible is a common location.
Bailey classification of second branchial cleft cysts
This classification was initially proposed by Bailey in 1929 4 and remains the most widely used classification system.
Bailey classification of second branchial cleft cysts provides a structure for classing second branchial cleft cysts into four types. It is no longer used in practice, having been superseded by the sensible approach of describing the lesion. However, it is worth noting this classification because it gives a sense of the variability in location and helps to frame a description.
- type I: deep to platysma, anterior to sternocleidomastoid
- type II: abutting internal carotid artery and adherent to internal jugular vein (most common)
- type III: extending between internal and external carotid arteries
- type IV: abutting pharyngeal wall and potentially extending superiorly to skull base
Second branchial cleft cyst signs and symptoms
Although a congenital abnormality, second branchial cleft tend to present in early adulthood (10-40 years of age) often after minor trauma or infection. Second branchial cleft sinus or fistulas, on the other hand, present earlier. Fistulas extend from the skin surface anterior to the middle of the sternocleidomastoid muscle, pass between the internal and external carotid arteries and eventually drain into the tonsillar fossa.
Typically, second branchial cleft cysts present as a rounded swelling just below the angle of mandible, anterior to sternocleidomastoid (although the position is variable).
Third branchial cleft cyst
Third branchial cleft cysts are a very rare type of branchial cleft cysts. Although they are extremely rare, they remain the second most common congenital lesion of the posterior cervical region after cervical lymphatic malformations or cystic hygromas 14.
By definition, a third branchial cleft cyst must lie posterior to the common or internal carotid artery, between the hypoglossal nerve below and the glossopharyngeal nerve above 15. Cysts may occur anywhere along the course of the third branchial cleft or pouch. Most third branchial cleft cysts tend to lie in the posterior cervical space, posterior to the sternocleidomastoid muscle 16.
Third branchial cleft cysts are typically located in the posterior cervical region. Occasionally third branchial cleft cysts can have retropharyngeal extension 17. The proximity of the third and fourth branchial arches makes distinguishing 3rd from 4th branchial cleft abnormalities radiologically difficult (for accurate diagnosis, the relationship of the sinus tract to the superior laryngeal nerve must be determined surgically). If they form a sinus, the sinus tract will drain into the pyriform sinus.
Fourth branchial cleft cyst
Fourth branchial cleft cysts are very rare, and parallel the course of the recurrent laryngeal nerve. They are most commonly on the left side (80%) and usually form a sinus which extends from the apex of the piriform sinus, as do third branchial cleft sinuses, but passes inferiorly rather than superiorly to reach anterior left upper thyroid lobe. Cysts can be anywhere in the neck down to the mediastinum, however, in most cases, they are located adjacent to the thyroid gland.
The proximity of the third and fourth branchial arches makes distinguishing 3rd from 4th branchial cleft abnormalities radiologically difficult (for accurate diagnosis, the relationship of the sinus tract to the superior laryngeal nerve must be determined surgically).
The most common presentation is abscess within or anterior to the left thyroid lobe.
Branchial cleft cyst causes
Branchial cleft cysts form during development of the embryo. The anomalies result from branchial apparatus (six arches; five clefts), which are the embryologic precursors of the ear and the muscles, blood vessels, bones, cartilage, and mucosal lining of the face, neck, and pharynx 18. Branchial cleft cysts occur when tissues in the neck area (branchial cleft) fail to develop normally. During the 2nd to 7th week of embryonic development, the second arch grows caudally and covers the third, fourth and sixth arches. When it fuses to the skin caudal to these arches, the cervical sinus is formed. Eventually, the edges of cervical sinus fuse and the ectoderm within the tube disappears 19. Persistence of branchial cleft or pouch results in a cervical anomaly located along the anterior border of the sternocleidomastoid muscle from the tragus of the ear to the clavicle 20.
The birth defect may appear as open spaces called cleft sinuses, which may develop on one or both sides of the neck. A branchial cleft cyst may form from fluid drained from a sinus. The cyst or sinus can become infected.
The range of branchial anomalies can include:
- cyst: no internal or external communication
- fistula: communicates both internally and externally
- sinus: incomplete tract
Cysts are the most common, outnumbering fistulas and sinuses ~2:1 21. Among fistulae and sinuses, the order prevalence is thought to be: external draining sinus > complete fistula > internal draining sinus 21; although some anomalies can occur in combination.
The full list of branchial anomalies includes:
- first branchial cleft anomalies (5-8%)
- first branchial cleft cyst
- first branchial cleft fistula
- first branchial cleft sinus
- second branchial cleft anomalies (commonest by far: 90-95%)
- second branchial cleft cyst
- second branchial cleft fistula
- second branchial cleft sinus
- third branchial cleft anomalies (rare)
- third branchial cleft cyst
- third branchial cleft fistula
- third branchial cleft sinus
- fourth branchial cleft anomalies (rare)
- fourth branchial cleft cyst
- fourth branchial cleft fistula
- fourth branchial cleft sinus
- the fifth cleft does not give rise to the cervical sinus of His which is part of the reason that there are no fifth branchial cleft anomalies
The 3rd and 4th branchial arches tend to be very close and therefore the distinction between these two cleft anomalies can be difficult on imaging 22.
Branchial cleft cyst symptoms
Branchial cleft cysts are most often seen in children. In some cases, they are not seen until adulthood.
Branchial cleft cyst symptoms may include any of the following:
- Small pits, lumps, mass or skin tags at either side of the neck or just below the jawbone near the front edge of the sternocleidomastoid muscle (usually only on one side of the neck, rarely on both sides; usually painless unless infected)
- Small opening in the skin that drains mucus or fluid near the front edge of the sternocleidomastoid muscle
- Noisy breathing (if the cyst is large enough to block part of the airway)
Branchial cleft abnormalities are usually small, but can enlarge enough to cause difficulty swallowing and breathing. The following are the most common symptoms of a branchial cleft abnormality. However, each child may experience symptoms differently.
The symptoms of a branchial cleft abnormality may resemble other neck abnormalities or medical problems. Always consult your child’s doctor for a diagnosis.
Branchial cleft cyst complications
Branchial cleft cysts or sinuses may become infected if not removed, and repeat infections may make surgical removal more difficult.
Branchial cleft cyst cancer
There are rare case reports of malignancies having been identified in branchial cleft lesions, including branchiogenic carcinoma and papillary thyroid carcinoma 23.
Branchial cleft cyst diagnosis
Branchial cleft abnormalities are diagnosed by physical examination. Generally, the specific location of the mass or the fistula opening on the skin can help in the diagnosis. A branchial cleft cyst may not be noticed unless it becomes infected and is painful. The skin opening of a branchial cleft fistula drains mucus, and often pulls back into the skin with swallowing movement.
In addition to a complete medical history and physical examination, diagnostic procedures for a branchial cleft abnormality may include the following:
- Computed tomography scan (also called CT or CAT scan). A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays and are used to determine the exact location and extent of the abnormality.
- MRI scan
- Ultrasound
- Biopsy. A procedure in which tissue samples are removed (with a needle or during surgery) from the body for examination under a microscope.
- Fine needle aspiration of the fluid (for further examination)
On computed tomography (CT scan), branchial cleft cysts typically appear well-circumscribed and, in the absence of complications, they are uniformly hypodense with thin walls; wall thickness may increase after an infection. The branchial cleft cyst generally causes posteromedial displacement of the sternocleidomastoid muscle and the vessels of the carotid space and anterior displacement of the submandibular gland 24.
Magnetic resonance imaging provides better depiction of the deep extent of the branchial cleft cyst and a more previse preoperative assessment. The content of the branchial cleft cysts varies from hypo- to isointense (relative to the muscles) in T1-weighted sequences; it is hyperintense in T2-weighted sequences. The presence of an inflammatory process is often reflected by thickening and increased enhancement of the walls, which resembles an abscess or lymphadenopathy 25.
Fine-needle aspiration cytology is useful (albeit invasive) for reaching a preoperative diagnosis. The cytological criteria are: yellow, pus-like fluid, keratinized anuclear cells, squamous epithelium, and a matrix of amorphous debris. Surgical excision is currently the treatment of choice.
Branchial cleft cyst treatment
Antibiotics will be given if the cyst or sinuses are infected.
Surgery is generally needed to remove a branchial cyst to prevent complications such as infections. If there is an infection when the cyst is found, surgery will likely be done after the infection has been treated with antibiotics. If there have been several infections before the cyst is found, it may be harder to remove.
Sclerotherapy with OK-432 (picibanil) has been reported to be an effective alternative to surgical excision of branchial cleft cysts by some groups 26, including those using ultrasound guidance 27.
Branchial cleft cyst surgery
Surgical excision is definitive treatment for branchial cleft cysts 28. A series of horizontal incisions, known as a stairstep or stepladder incision, is made to fully dissect out the occasionally tortuous path of the branchial cleft cysts. Branchial cleft cyst surgery is best delayed until the patient is at least age 3 months. Definitive branchial cleft cyst surgery should not be attempted during an episode of acute infection or if an abscess is present. Surgical incision and drainage of abscesses is indicated if present, usually along with concurrent antimicrobial therapy.
The traditional surgical approach has the main downfall of relatively significant scarring. Alternatives to the open surgical method have been proposed, including a retroauricular approach, a facelift approach, and endoscopic-assisted removal. All of the newer surgical methods may be limited in the full visualization of the lesion. A recent case-controlled study suggested that an endoscopic retroauricular approach may provide good surgical clearing with minimal scarring for second branchial cleft cysts 29.
Complications of surgical excision of branchial cleft cysts result from damage to nearby vascular or neural structures, which include carotid vessels and the facial, hypoglossal, vagus, and lingual nerves.
Postoperatively, patients should be monitored for branchial cleft cyst recurrence. Because some patients have bilateral branchial cleft cyst lesions, the contralateral side should be examined.
Branchial cleft cyst prognosis
Many branchial cleft cysts are asymptomatic. They may become tender, enlarged, or inflamed, or they may develop abscesses, especially during periods of upper respiratory tract infection, due to the lymphoid tissue located beneath the epithelium. Spontaneous rupture of an abscessed branchial cleft cyst may result in a purulent draining sinus to the skin or the pharynx.
Depending on the size and the anatomical extension of the mass, local symptoms, such as dysphagia, dysphonia, dyspnea, and stridor, may occur.
Following surgical excision of branchial cleft cysts, recurrence is uncommon, with a risk estimated at 3%, unless previous surgery or recurrent infection has occurred, in which case, it may be as high as 20%.
References- Branchial Cleft Cyst. https://emedicine.medscape.com/article/1110351-overview
- Gupta M, Gupta M. A rare parapharyngeal space branchial cleft cyst. BMJ Case Rep. 2013;2013:bcr2013008952. Published 2013 Apr 29. doi:10.1136/bcr-2013-008952 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3645224/
- Howard DJ, Lund VJ. Pharynx, larynx and neck—branchial cleft cyst. In: NS Williams, CJK Butstrode, PR O’Connell, A Hodder, editors. , eds. Bailey and Love’s short practise of surgery (20th edn). London, UK: Harcourt, 2008. pp. 727–729
- Bailey H. Branchial cysts and other essays on surgical subjects in the faciocervical region. London, England: Lewis 1929.
- Thomaidis V, Seretis K, Tamiolakis D, Papadopoulos N, Tsamis I. Branchial cysts. A report of 4 cases. Acta Dermatovenerol Alp Panonica Adriat. 2006;15(2):85–89.
- Ascherson GM. Defistulis Colli congenitis fissuratum branchialium in mammalibus avibusque historica succincta. CH Jonas, Berolini, 1832:1–21
- Thomaidis V, Seretis K, Tamiolakis D, Papadopoulos N, Tsamis I. Branchial cysts—a report of 4 cases. Acta Dermatoven APA 2006;15:85–89
- Branchial anomalies: a review of 52 cases. Choi SS, Zalzal GH. Laryngoscope. 1995 Sep; 105(9 Pt 1):909-13.
- Vaidya S, Pagare RS, Sharma VK. Lateral cervical cyst. Inter J Otorhinolaryngol 2008;7:1–6
- Panchbhai AS, Choudhary MS. Branchial cleft cyst at an unusual location: a rare case with a brief review. Dentomaxillofac Radiol. 2012;41(8):696-702. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3528200/
- First Branchial Cleft Cyst. N Engl J Med 2016; 375:e33 DOI: 10.1056/NEJMicm1503044 https://www.nejm.org/doi/pdf/10.1056/NEJMicm1503044
- Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 19 (1): 121-46; quiz 152-3. doi:10.1148/radiographics.19.1.g99ja06121
- D’Souza AR, Uppal HS, De R, Zeitoun H. Updating concepts of first branchial cleft defects: a literature review. International journal of pediatric otorhinolaryngology. 62 (2): 103-9
- Joshi MJ, Provenzano MJ, Smith RJ et-al. The rare third branchial cleft cyst. AJNR Am J Neuroradiol. 2009;30 (9): 1804-6. AJNR Am J Neuroradiol – doi:10.3174/ajnr.A1627
- Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics. 1999 Jan-Feb;19(1):121-46; quiz 152-3. https://www.ncbi.nlm.nih.gov/pubmed/9925396
- Computed tomography and magnetic resonance imaging appearances of cystic lesions in the suprahyoid neck: a pictorial review. Dentomaxillofac Radiol. 2007 Dec;36(8):451-8. https://www.ncbi.nlm.nih.gov/pubmed/18033940
- Hewel K, Kioumehr F, So G et-al. Infected third branchial cleft cyst: retropharyngeal extension to the superior mediastinum. Can Assoc Radiol J. 1996;47 (2): 111-3
- Whetstone J, Branstetter BF, Hirsch BE. Fluoroscopic and CT fistulography of the first branchial cleft. AJNR Am J Neuroradiol. 2006;27 (9): 1817-9.
- Sadler TW. Langman’s Medical Embryology. LWW. ISBN:1451191642.
- Sahu S, Kumar A, Ramakrishnan T. Medical Journal Armed Forces India. 2011;67 (3): . doi:10.1016/S0377-1237(11)60056-7
- Second branchial cleft cyst and fistula. BM Gold. American Journal of Roentgenology 1980 134:5, 1067-1069 https://www.ncbi.nlm.nih.gov/pubmed/6768251
- The rare third branchial cleft cyst. AJNR Am J Neuroradiol. 2009 Oct;30(9):1804-6. doi: 10.3174/ajnr.A1627. Epub 2009 May 27. https://www.ncbi.nlm.nih.gov/pubmed/19474121
- Branchial Cleft Cyst Treatment & Management. https://emedicine.medscape.com/article/1110351-treatment
- Mitroi M, Dumitrescu D, Simionescu C, Popescu C, Mogoanta C, Cioroianu L, et al. Management of second branchial cleft anomalies. Rom J Morphol Embryol. 2008;49(1):69–74
- Ibrahim M, Hammoud K, Maheshwari M, Pandya A (2011) Congenital cystic lesions of the head and neck. Neuroimaging Clin N Am 21(3):621–639, viii
- Kim MG, Kim SG, Lee JH, Eun YG, Yeo SG. The therapeutic effect of OK-432 (picibanil) sclerotherapy for benign neck cysts. Laryngoscope. 2008 Dec. 118(12):2177-81
- Kim JH. Ultrasound-guided sclerotherapy for benign non-thyroid cystic mass in the neck. Ultrasonography. 2014 Apr. 33(2):83-90
- Donegan JO. Congenital neck masses. Cummings CW, Schuller DE, eds. Otolaryngology – Head and Neck Surgery. 2nd ed. St. Louis, Mo: Mosby; 1993. 1554-9.
- Chen L, Huang X, Lou X, Xhang S, Song X, Lu Z, et al. [A comparison between endoscopic-assisted second branchial cleft cyst resection via retroauricular hairline approach and conventional second branchial cleft cyst resection]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2013 Nov. 27(22):1258-62