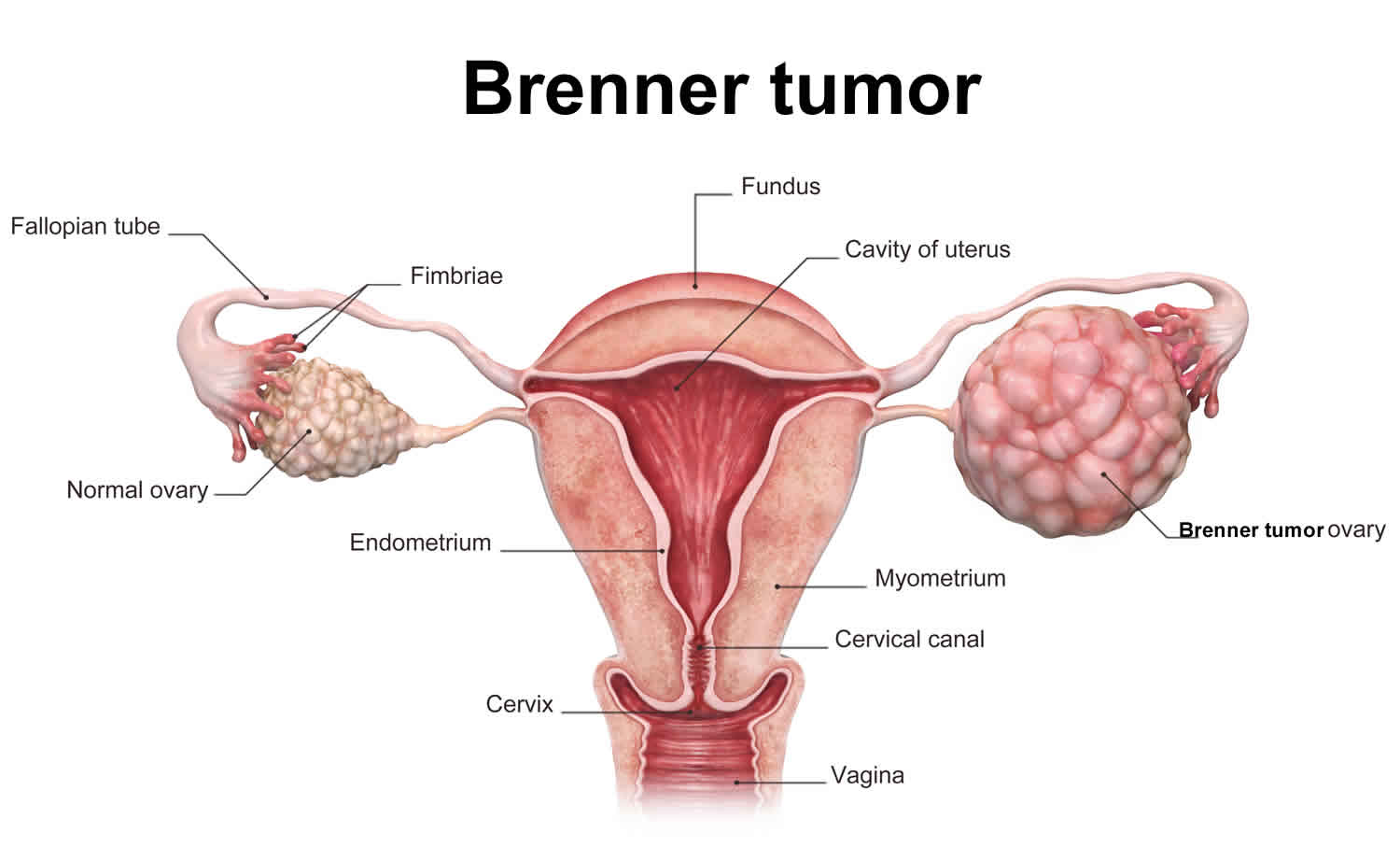
Brenner tumor ovary
Brenner tumor is a very rare tumor (adenofibroma) of the ovary representing 5% of all ovarian tumors 1. Brenner tumor is classified into benign, malignant and borderline Brenner tumor 2. Over 95% of Brenner tumors are not cancerous (benign). About 5% of Brenner tumors are cancerous (malignant) or have a small chance of spreading beyond its original location (borderline) 3.
Most Brenner tumor is solid tumor and is generally thought to be derived from surface epithelial cells 2. Although Brenner tumors are predominantly solid on imaging and pathologic examination, association with serous and mucinous cystadenomas is up to 30% 4. Their size varies from less than 1 cm to up to 30 cm 3. They are usually unilateral and are characterized by their epithelial lining that contains clusters of transitional cells that resemble the urinary tract epithelium. Sometimes these nests have microcysts or mucinous glands in the center 5.
The exact number of people who develop Brenner tumors is not known 6. Brenner tumors most often occur in women after menopause. The average age at presentation is 50 years with 71% of the patients being more than 40 years 7. Brenner tumors usually do not cause symptoms unless they are very large 8. When symptoms are present, common symptoms may include abdominal pain, pelvic pain, palpable pelvic mass or vaginal bleeding 9. Brenner tumors are usually found by accident during surgery for another reason or during a routine doctor’s examination. Most of the time it is found to be unilateral. Bilaterality is seen only in 5–7% of the cases 10. It is usually an incidental pathological finding. The diagnosis is made by microscopic examination of a piece of tumor obtained by a surgical biopsy. The histological patterns observed in Brenner tumor are typically benign, with a few reports of borderline or malignant counterparts 7.
Brenner tumors treatment usually consists of surgery to remove the tumor 3. If a Brenner tumor has not spread into surrounding tissues or to more distant parts of the body, there is a good-to-excellent long-term outcome 6.
Are Brenner tumors of the ovary benign?
Most Brenner tumors of the ovary are benign and do not spread into surrounding tissues 6. Approximately 1-2% of these tumors can become malignant and may spread into surrounding tissues or to more distant parts of the body 11.
Brenner tumor causes
The cause of Brenner tumor is unknown. It is generally accepted that Brenner tumors are derived from the surface epithelium of the ovary or the pelvic mesothelium through transitional cell metaplasia to form the typical urothelial-like components 12. Most of the literature favors the germ cell origin of Brenner tumor and struma ovarii 2. For example, Yoshida et al 13 reported a case of coexisting Brenner tumor and struma ovarii of the ovary. They found that both Brenner tumor and struma ovarii were immunoreactive for thyroglobulin, and suggested that the Brenner tumor element was metaplastic one and the ovarian tumor is germ cell origin. Similar case was reported by Takeuchi et al 14 who found thyroglobulin immunoreactivity in both the Brenner tumor and struma ovarii. They also speculated that this peculiar combination tumor may be derived from germ cells.
About 30% of the time, benign Brenner tumors are found along with ovarian cancer 9. Women who have any type of ovarian cancer, including a malignant Brenner tumor, may want to ask their health care professional about genetic counseling because ovarian cancer is sometimes associated with a gene mutation that can be inherited in families 15.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Brenner tumor signs and symptoms
Most Brenner tumors do not cause any symptoms 9. If the tumor is quite large, it may cause pain or discomfort in one side of the abdomen 3. Women who are post-menopausal may experience vaginal bleeding as a symptom 3. If the Brenner tumor is malignant (cancerous), it may cause symptoms similar to other types of ovarian cancer, including abdominal swelling and difficulty with bladder control 16.
Brenner tumor diagnosis
Approximately 90% of Brenner tumors of the ovary are first discovered by chance during surgery, a routine pelvic exam or an ultrasound 17. Brenner tumors are ultimately diagnosed by a surgical biopsy. Brenner tumors have specific microscopic findings that help guide diagnosis. Grossly benign Brenner tumors are well circumscribed, with a hard or fibromatous, gray, white, or slightly yellow cut surface. Occasionally the tissue becomes gritty because of calcific deposit. Borderline Brenner tumors are characteristically cystic and unilocular or multilocular with cauliflower like papillomatous masses protruding into one or more of the locules 9. Malignant Brenner tumor may be solid or cystic with mural nodules; they usually do not have any distinctive features 18.
Blood test for specific tumor markers may also be helpful 16. Reliable tumor markers for malignant Brenner tumor have not been identified 19. Yamamoto et al. 20 have published two case reports of malignant Brenner tumor, one with elevated CA72-4 and CA125 and the other with elevated CA72-4 and squamous cell carcinoma (SCC) antigen which suggested these may be tumor markers of interest. CA125 is elevated in some patients with malignant Brenner tumor, with reports ranging from 30 to 70%, but was not correlative to stage or tumor burden 21. Despite the low sensitivity (50–62%) and moderate specificity (94–98.5%) of CA125, it remains the most widely used serologic marker in patients with epithelial ovarian cancer traditionally used to monitor for recurrence after treatment 22. Given that malignant Brenner tumor is a member of this neoplastic family, it remains sensible to check pre-operative CA125 in these patients and to use it as a marker of recurrence if an elevated CA125 returns to normal after treatment.
It is difficult to diagnose Brenner tumor with imaging studies. Ultrasound and computed tomography, both the techniques are limited in specificity because of the tumor’s nonspecific appearance. In imaging studies benign Brenner tumors are generally similar to those of other solid ovarian masses such as fibroma, fibrothecoma, and pedunculated leiomyoma 4. One retrospective study failed to identify any ultrasound features specific to Brenner tumors, which had been discovered incidentally after adnexal masses of unknown etiology were removed 23. One identified CT and MRI finding is extensive calcification within a solid component of a cystic mass 24.
Brenner tumor treatment
Treatment of Brenner tumors of the ovary usually consists of surgery to remove the tumor 3. If the tumor is found to be cancerous, it may be necessary to do more extensive surgery, including removing both ovaries, fallopian tubes and the uterus (total abdominal hysterectomy and bilateral salpingo-oophorectomy), followed by chemotherapy or radiation. The age of the woman and whether she has a hereditary cancer syndrome may be factors in deciding the best course of treatment 16. For women who are past the age of menopause, it is recommended that both ovaries, fallopian tubes and the uterus be removed. Younger women may want to consider less surgery to help preserve fertility and keep one working ovary 17. The ovaries produce hormones that regulate a woman’s menstrual cycle; it is the loss of these hormones, either naturally or by the removal of the ovaries, that causes the signs and symptoms of menopause 25. Women who take low doses of hormone replacement drugs after surgery up until the age of 50 may reduce the chance of having the symptoms typically associated with menopause. But hormone replacement therapy has risks of its own. It is recommended that women who are thinking about taking hormone replacement therapy discuss the benefits and limitations of this therapy with their personal physicians 25.
Additional treatment may depend on the stage of the cancer and the extent it has spread beyond the ovary.
Brenner tumor prognosis
For individuals with non-cancerous Brenner tumors, and no other findings, there is a good to excellent long-term outlook. While Brenner tumors usually don’t recur, one study showed that in about 28% of cases, the tumor comes back after it is removed 19.
The long-term outlook for individuals with cancerous or borderline Brenner tumors depends on the stage of the cancer when it is diagnosed and if the cancer has spread beyond the ovary. In general, the earlier the tumor is diagnosed and the less it has spread, the better the outcome 19.
References- Lee KR, Russell P, Tavassoli FA, et al. Surface epithelial-strumal tumor. In: Tavassoli FA, Devilee P, editors. World Health Organization Classification od Tumours. Pathology and genetics of tumours of the breast and female genital organs. Lyon: IARC press; 2003. pp. 142–143.
- Terada T, Tateoka K. Ovarian cystic tumor composed of Brenner tumor and struma ovarii. Int J Clin Exp Pathol. 2012;5(3):274-277. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3341679
- Dougherty D, Onyemkpa C, Engel M, Oyasiji T. A case report of an incidental Brenner tumor found after resection of a large ovarian mucinous neoplasm. Int J Surg Case Rep. 2018;49:40-43. doi:10.1016/j.ijscr.2018.05.007 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039703
- Green GE, Mortele KJ, Glickman JN, Benson CB. Brenner tumors of the ovary sonographic and computed tomographic imaging features. J Ultrasound Med. 2006;25:1245–51.
- Crum C.P. The female genital tract. In: Kumar V., Abbas A.K., Fausto N., Robbins S.L., Cotran R.S., editors. Robbins Cotran Pathol. Basis Dis. 7th edition. Elsevier Saunders; Philadelphia: 2005. pp. 1098–1099.
- Benign Lesions of the Ovaries. https://emedicine.medscape.com/article/265548-overview
- Hemalatha AL, Konanahalli P. Bilateral malignant Brenner tumor of ovary. J Obstet Gynecol India. 2005;55:81–2.
- Nasioudis D, Sisti G, Holcomb K, Kanninen T, Witkin SS. Malignant Brenner tumors of the ovary; a population-based analysis. Gynecol Oncol. 2016 Jul;142(1):44-49. doi: 10.1016/j.ygyno.2016.04.538. Epub 2016 May 11.
- Borah T, Mahanta RK, Bora BD, Saikia S. Brenner tumor of ovary: An incidental finding. J Midlife Health. 2011;2(1):40-41. doi:10.4103/0976-7800.83273 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3156501
- Moon WJ, Koh BH, Kim SK, Kim YS, Rhim HC, Cho OK, et al. Brenner tumor of the ovary: CT and MR findings. J Comput Assist Tomogr. 2000;24:72–6.
- Katz VL, Lentz GM, Lobo RA, Gershenson DM. Comprehensive Gynecology, 5th edition. Philadelphia, PA: Mosby Elsevier; 2007
- Arey LB. The origin and form of the Brenner tumor. Am J Obstet Gynecol. 1961;81:743–51.
- Yoshida M, Okabayashi C, Tachibana M, Minami R. Coexisting Brenner tumor and struma ovarii in the right ovary: case report and review of the literature. Pathol Int. 2004;54:793–797.
- Takeuchi K, Ohbayashi C, Kitazawa S, Ohara N, Maruo T. Coexistence of Brenner tumor and struma ovarii: case report. Eur J Gynecol Oncol. 2005;26:109–110.
- Toboni MD, Smith HJ, Dilley SE, Novak L, Leath CA. Malignant Brenner tumor associated with a germline BRCA2 mutation. Gynecol Oncol Reports. 2017; 21:17-19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5458647/pdf/main.pdf
- Lang SM, Mills AM, Cantrell LA. Malignant Brenner tumor of the ovary: Review and case report. Gynecol Oncol Reports. 2017; 22:26-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5608552
- Nasioudis D, Sisti G, Holcomb K, Kanninen T, Witkin S. Malignant Brenner tumors of the ovary; a population-based analysis. Gynecol Oncol. 2016; 142:44-49. https://www.ncbi.nlm.nih.gov/pubmed/27130406
- Clemet PB, Young RH. Ovarian Surface Epithelial – Stromal Tumors. In: Mills SE, editor. Sternberg’s Diagnostic Surgical Pathology. 5th ed. Philadelphia: Lippincott Williams and Wilkins, A Wolters Kluwer business; 2010. pp. 2278–308.
- Lang SM, Mills AM, Cantrell LA. Malignant Brenner tumor of the ovary: Review and case report. Gynecol Oncol Rep. 2017;22:26-31. Published 2017 Jul 3. doi:10.1016/j.gore.2017.07.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5608552
- Yamamoto R., Fujita M., Kuwabara M., Sogame M., Ebina Y., Sakuragi N., Kato H., Fujimoto S. Malignant Brenner tumors of the ovary and tumor markers: case reports. Jpn. J. Clin. Oncol. 1999;29:308–313.
- Nasioudis D., Sisti G., Holcomb K., Kanninen T., Witkin S.S. Malignant Brenner tumors of the ovary; a population-based analysis. Gynecol. Oncol. 2016;142:44–49.
- Sölétormos G., Duffy M., Hassan S., Verheijen R., Tholander B., Bast R., Gaarenstroom K., Sturgeon C., Bonfrer J., Petersen P., Troonen H., CarloTorre G., Kulpa J., Tuxen M., Molina R. Clinical use of cancer biomarkers in epithelial ovarian cancer: updated guidelines from the European Group on Tumor Markers. Int. J. Gynecol. Cancer. 2016;26:43.
- Dierickx I, Valentin L, Van Holsbeke C, Jacomen G, Lissoni AA, Licameli A, Testa A, Bourne T, Timmerman D. Imaging in gynecological disease (7): clinical and ultrasound features of Brenner tumors of the ovary. Ultrasound Obstet Gynecol. 2012 Dec;40(6):706-13. doi: 10.1002/uog.11149. Epub 2012 Nov 8.
- Moon W.J., Koh B.H., Kim S.K., Kim Y.S., Rhim H.C., Cho O.K., Hahm C.K., Byun J.Y., Cho K.S., Kim S.H. Brenner tumor of the ovary: CT and MR findings. J. Comput. Assist. Tomogr. 2005;24:72–76.
- Oophorectomy (ovary removal surgery). https://www.mayoclinic.org/tests-procedures/oophorectomy/about/pac-20385030