Chilaiditi syndrome
Chilaiditi syndrome is a medical condition in which a portion of the colon is abnormally positioned between the liver and the right hemidiaphragm 1. Chilaiditi syndrome refers to the interposition of the colon through the anterior hepatic space or the posterior hepatic space between the liver and the diaphragm 2. Chilaiditi syndrome symptoms vary, but the most common presenting symptoms are abdominal pain, distention, nausea, vomiting, constipation and small bowel obstruction 1. More morbid presentations include abnormal twisting of the intestines (volvulus) causing obstruction, cecal perforation, and perforated sub-diaphragmatic appendicitis 3. Rarely, patients present with respiratory symptoms including shortness of breath (dyspnea) and chest pain mimicking angina and require intensive care. In many cases, there are no symptoms and the malpositioned colon is an incidental finding. When no symptoms are present, the clinical finding is called Chilaiditi’s sign 1.
The incidence of Chilaiditi syndrome is less than 0.3% and underlying cause of Chilaiditi syndrome is unknown, but may be congenital or acquired 4.
The risk of an undiagnosed Chilaiditi’s sign is perforation during colonoscopy or liver biopsy. The best diagnostic imaging modality is CT scan.
Chilaiditi syndrome treatment is symptomatic and supportive 5. Conservative management should be attempted first to relieve constipation, pain, and distention. Surgery is rarely required and is reserved for patients who fail conservative management and in cases of obstruction, volvulus, or ischemia 1.
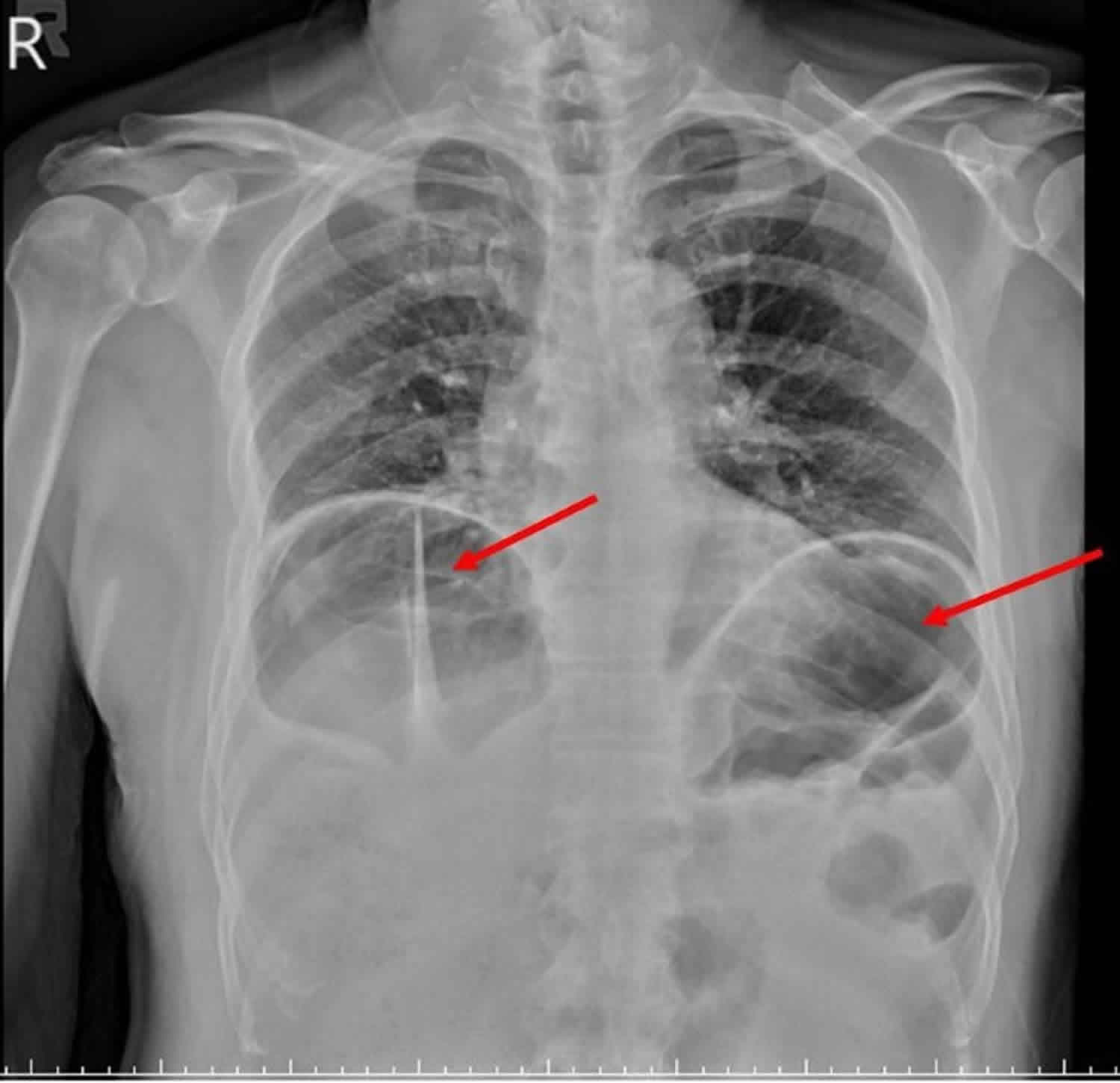
Figure 1. Chilaiditi syndrome chest X-ray
Footnote: Colonic interposition beneath the right hemidiaphragm. In this case the haustral markings are well delineated indicating colon between the diaphragm and liver. Right upper lobe fibrosis.
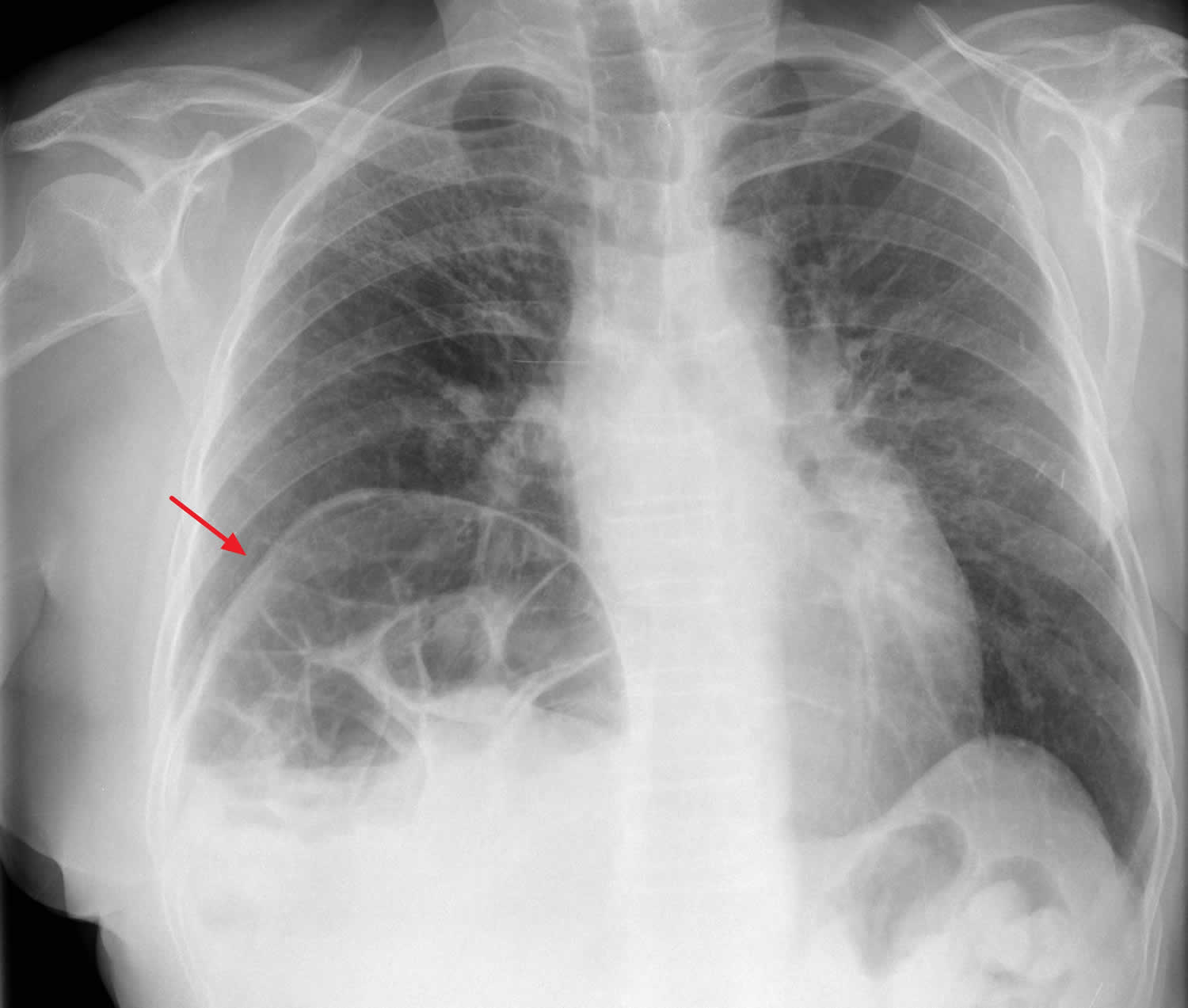
Figure 2. Chilaiditi syndrome abdominal CT scan
Footnote: Abdominal CT scan shows malpositioned cecum adjacent to the right lobe of liver.
[Source 1 ]Chilaiditi syndrome causes
The exact cause of Chilaiditi syndrome is unknown. Chilaiditi’s syndrome appears to occur with higher frequency among individuals with chronic lung disease, scarring of the liver (cirrhosis), and in those with the accumulation of fluid within the abdominal cavity (ascites). Other risk factors may include reduced liver volume, abnormal elongation of the colon or abnormal looseness (laxity) of certain ligaments of the colon and liver, paralysis of the motor nerve to the diaphragm (phrenic nerve palsy), and obesity 5. In some cases, the condition is present from birth (congenital) 6.
Chilaiditi syndrome symptoms
Chilaiditi syndrome symptoms may vary from one person to another. Chronic recurrent abdominal pain is a common finding. Abdominal pain may be mild and come and go (intermittent). However, abdominal pain can be severe and force affected individuals to go to the emergency room. Other symptoms might include nausea, vomiting, constipation, indigestion (dyspepsia), abdominal swelling (distention), difficulty swallowing (dysphagia), and abdominal tenderness, especially in the upper, central area (epigastric region). In some cases, breathing problems (respiratory distress) may develop 5.
Chilaiditi syndrome diagnosis
A diagnosis of Chilaiditi’s syndrome is made based upon imaging (radiographic) confirmation of the abnormal positioning of the colon and the occurrence of associated symptoms. Such imaging techniques may include chest and abdominal X-rays, ultrasounds, or computerized tomography (CT) scanning. The best diagnostic imaging modality is CT scan 1.
Chilaiditi sign is defined by the presence of air below the right diaphragm on a radiograph 7. To diagnose Chilaiditi sign based upon radiologic findings, the following criteria must be met 8:
- The right hemidiaphragm must be adequately elevated above the liver by the intestine, the bowel must be distended by air to illustrate pseudopneumoperitoneum, and the superior margin of the liver must be depressed below the level of the left hemidiaphragm.
Important differential diagnoses of this radiographic sign include pneumoperitoneum and subphrenic abscess. The finding of normal plicae circulares or haustral markings of the colon under the diaphragm can rule out these more serious entities. Moreover, changing the position of a patient with Chilaiditi sign will not change the position of the radiolucency, unlike in a patient with free air. Similarly, when using ultrasound, altering the position of a patient with Chilaiditi sign will not lead to a change in the location of the gas echo, as opposed to a patient with pneumoperitoneum 9. If a radiograph or ultrasound cannot clearly determine whether the subdiaphragmatic air is free or intraluminal, a computed tomography scan is recommended to establish an accurate diagnosis, assuming that the patient is clinically stable 10.
Chilaiditi syndrome treatment
Treatment of Chilaiditi syndrome is directed at the individual symptoms present. In some cases, treatment is not needed. Conservative management should be attempted first to relieve constipation, pain, and distention. Reducing (or removing) the pressure within the abdomen may help alleviate symptoms 5. This may be achieved through conservative measure that address constipation, pain, and distention, such as nasogastric decompression, administration of stool softeners and enemas, and intravenous fluids 2. Conservative treatment has been shown to be effective.
Surgery is rarely required and is reserved for patients who fail conservative management and in cases of obstruction, volvulus, or ischemia.
Chilaiditi syndrome surgery
The appropriate surgical approach depends on the nature of the interposed segment of the colon. Surgical intervention may include the removal of a portion of the colon (transverse colectomy or right hemicolectomy) or the anchoring of a displaced liver to the abdominal wall (hepatopexy) 5. Cecopexy may be adequate to eliminate the possibility of recurrence in an uncomplicated cecal volvulus, unless gangrene or perforation necessitates surgical resection. However, colonic resection is the best option for a volvulus of the transverse colon, and attempts at colonoscopic reduction are not recommended due to a high frequency of gangrene (16%) in this type of volvulus 11.
References- Jangouk P, Zaidi F, Hashash JG. Chilaiditi’s Sign: A Rare Cause of Abdominal Pain. ACG Case Rep J. 2014;1(2):70-71. Published 2014 Jan 10. doi:10.14309/crj.2014.3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4435277
- Xu Y, Wang Q, Meng G, et al. A rare cause of sudden chest pain and dyspnea: A CARE-compliant case report of Chilaiditi syndrome. Medicine (Baltimore). 2020;99(20):e20220. doi:10.1097/MD.0000000000020220 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253721
- Aldoss IT, Abuzetun JY, Nusair M, et al. . Chilaiditi syndrome complicated by cecal perforation. South Med J. 2009;102(8):841–3.
- Moaven O, Hodin RA. Chilaiditi syndrome: A rare entity with important differential diagnoses. Gastroenterol Hepatol. 2012;8(4):276–8.
- Chilaiditi’s Syndrome. https://rarediseases.org/rare-diseases/chilaiditis-syndrome
- Jangouk P, Zaidi F, Hashash JG. Chilaiditi’s Sign: A Rare Cause of Abdominal Pain. ACG Case Rep J. 2014; 1(2):70-71. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4435277
- Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol (N Y). 2012;8(4):276-278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3380266
- Lekkas CN, Lentino W. Symptom-producing interposition of the colon. Clinical syndrome in mentally deficient adults. JAMA. 1978;240:747–750.
- Sato M, Ishida H, Konno K, et al. Chilaiditi syndrome: sonographic findings. Abdom Imaging. 2000;25:397–399.
- Fitzgerald JF, Tronconi R, Morris LD, Nowicki MJ. Clinical quiz. Chilaiditi’s sign. J Pediatr Gastroenterol Nutr. 2000;30:425, 471.
- Flores N, Ingar C, Sánchez J, et al. The Chilaiditi syndrome and associated volvulus of the transverse colon [in Spanish] Rev Gastroenterol Peru. 2005;25:279–284.