Bullous keratopathy
Bullous keratopathy is characterized by corneal edema with formation of epithelial bullae. Bullous keratopathy is a visually-disabling corneal disorder caused by endothelial cell dysfunction 1. Bullous keratopathy is caused by loss or dysfunction of the corneal endothelial cells which actively pumps water out of the cornea, maintaining the cornea’s dehydrated state. Without sufficient endothelial function, fluid accumulates in the extracellular spaces between collagen fibers and lamellae causing corneal swelling or edema. Subepithelial fluid-filled bullae form on the corneal surface as the corneal stroma (the deeper dense connective tissue layer of the cornea) swells, leading to decreased visual acuity, loss of contrast, glare, and photophobia. Sometimes bullae rupture, causing pain and foreign body sensation. Bacteria can invade a ruptured bulla, leading to a corneal ulcer.
Most frequently, bullous keratopathy is due to Fuchs corneal endothelial dystrophy or corneal endothelial trauma. Fuchs dystrophy is a genetic disorder that causes bilateral, progressive corneal endothelial cell loss, sometimes leading to symptomatic bullous keratopathy by age 50 to 60. Fuchs dystrophy may be autosomal dominant with incomplete penetrance. Another frequent cause of bullous keratopathy is corneal endothelial trauma, which can occur during intraocular surgery (eg, cataract removal) or after placement of a poorly designed or malpositioned intraocular lens implant. Bullous keratopathy after cataract removal is called pseudophakic bullous keratopathy (if an intraocular lens implant is present) or aphakic bullous keratopathy (if no intraocular lens implant is present).
Pseudophakic bullous keratopathy has recently emerged as a leading cause of endothelial keratoplasty 2.
During the development of pseudophakic bullous keratopathy, there are pathological changes in the corneal stroma, such as scar formation, the proliferation of a collagenous layer and fibrillar material deposits 2. An abnormal proliferation of the posterior collagenous layer and a significantly lower keratocyte density was found in the posterior part of the stroma of patients with long-term pseudophakic bullous keratopathy 3. It has also been reported that abnormal fibrillar materials posterior to Descemet’s membrane and subepithelial fibrocellular materials disrupt the epithelial basement membrane and Bowman’s layer in the corneas of bullous keratopathy patients 4.
Although treatment with a topical hypertonic solution temporarily improves corneal clarity, cornea transplant or keratoplasty is the only treatment that will significantly improve visual acuity 5. The preferred surgical procedure for bullous keratopathy has changed recently from penetrating keratoplasty to endothelial keratoplasty such as Descemet’s stripping automated endothelial keratoplasty (DSAEK) 6 or Descemet’s membrane endothelial keratoplasty (DMEK) 7. This change has improved visual outcome 8 and reduced the frequency of graft rejection 9. The Eye Bank Association of America Statistical Report has revealed that endothelial keratoplasty has accounted for up to 30% of total corneal grafting since 2008, underlining the facts that the number of endothelial keratoplasty operations is increasing and that the indications for such surgery are expanding worldwide 10.
Clinical investigations have shown that endothelial keratoplasty provides patients with a favorable postoperative visual acuity 11. A recent study, however, found that 77% of eyes treated with Descemet’s membrane endothelial keratoplasty (DMEK) and 23% of those treated with Descemet’s stripping automated endothelial keratoplasty (DSAEK) achieved a visual acuity of 20/25 or better 12 months after surgery 12. This means that 23% of DMEK eyes and 77% of DSAEK eyes did not manifest a favorable visual acuity after surgery 13. The rationale for endothelial keratoplasty is based on the supposition that the clarity of the edematous cornea can be recovered and visual acuity improved if stromal edema is removed. The discrepancy between this supposition and clinical outcome may suggest that subclinical stromal changes may affect the postoperative visual acuity of patients undergoing endothelial keratoplasty 13.
Corneal transplantation is not a good option in the case of poor visual potential. Therefore, other palliative modalities were introduced such as stromal puncture and bandage contact lenses in symptomatic cases 14.
Recently a new therapeutic option with cultured corneal endothelial cells has surfaced 15. A group of researchers in Japan 15 investigated whether cultured human corneal endothelial cells injected into the anterior chamber could restore endothelial function and corneal transparency. Eleven patients (mean age, 64.4 years) diagnosed with pseudophakic bullous keratopathy who had no detectable corneal endothelial cells were enrolled. Each patient had a corneal thickness > 630 µm and visual acuity less than 20/40. The degenerated endothelial cells were surgically removed, and then cultured human endothelial cells were injected into the anterior chamber. A rho-associated protein kinase inhibitor (ROCK) was injected along with the cultured cells to promote cell survival and adhesion. After the injection, patients lay in a prone position for 3 hours. Systemic and topical glucocorticoids as well as antibiotics were administered after the injections. Although the study was small, the results were impressive 16. All 11 eyes obtained a corneal endothelial cell density > 500 cells/mm², with 10 eyes achieving 1000 cells/mm² and six eyes exceeding 2000 cells/mm² at 24 weeks post-injection 15. An improvement in both corneal structure and function was demonstrated, with a corneal thickness < 630 µm achieved in 10 of the 11 eyes and 82% of eyes having a two-line improvement in visual acuity. A sustained therapeutic effect was achieved; after 2 years, all 11 eyes maintained corneal transparency. One patient developed steroid-induced glaucoma, but no other major systemic or ocular adverse effects were reported.
The promise of cultured corneal endothelial cells does not come without concerns, such as the fate of those cells that do not attach to the cornea, because of the risk for ectopic tumor formation. Serology and systemic health evaluations were completed in participants and no abnormalities developed over the course of the study, but that evidence is insufficient to definitely exclude the possibility of tumor development, owing to the small sample size and limited study duration.
It is also difficult to discern which element of the treatment was actually responsible for the increased corneal cell density. The authors hypothesized that the cultured cells were primarily responsible for the restored endothelial function, but acknowledged that the action of the rho-associated protein kinase (ROCK) inhibitor could have also prompted the recipient’s own endothelial cells to replicate 15. Regardless of the mechanism, the treatment was largely successful in attaining meaningful gains in endothelial function and visual function.
The ability to dramatically and rapidly increase endothelial cell counts would be revolutionary. Even partial restoration of endothelial function would potentially allow patients with bullous keratopathy to be candidates for other treatments that improve vision, such as contact lens fitting and cataract surgery, which are currently contraindicated in low endothelial function.
The safety of cultured endothelial cells with rho-associated protein kinase (ROCK) inhibitors must be confirmed, but this proof-of-concept study should be considered a success.
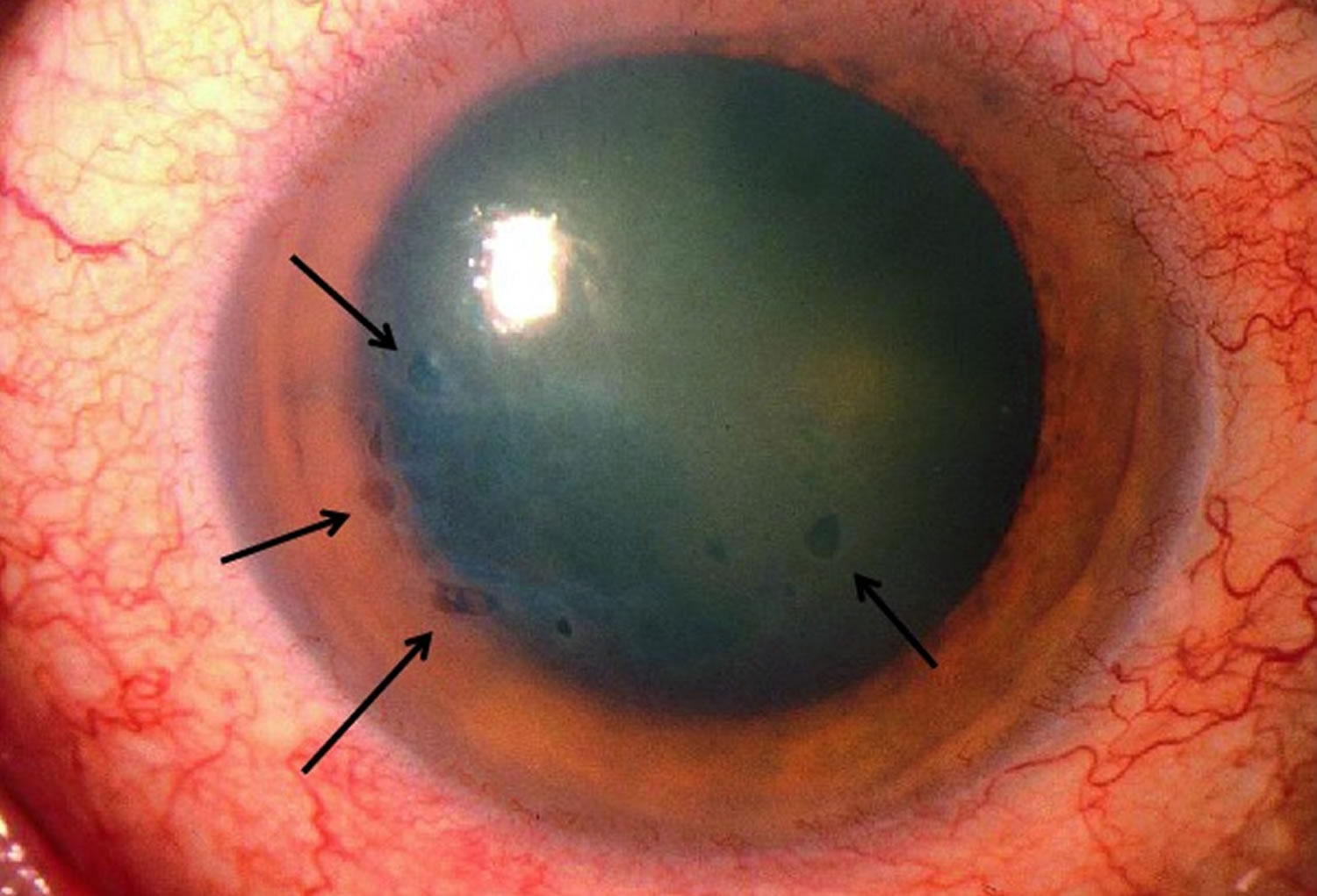
Figure 1. Bullous keratopathy
Footnote: This photo shows bullous keratopathy in a patient with Fuchs endothelial corneal dystrophy. The arrows show multiple medium-sized epithelial bullae. The light reflex is irregular, demonstrating multiple small bullae (showing microcystic edema, see arrows). There is also general cloudiness of the cornea, which can be seen by the blurring of the iris border, for example, at the 6 o’clock position.
Bullous keratopathy causes
Bullous keratopathy is caused by edema of the cornea, resulting from failure of the corneal endothelium to maintain the normally dehydrated state of the cornea. Most frequently, bullous keratopathy is due to Fuchs corneal endothelial dystrophy or corneal endothelial trauma. Fuchs dystrophy is a genetic disorder that causes bilateral, progressive corneal endothelial cell loss, sometimes leading to symptomatic bullous keratopathy by age 50 to 60 17. Fuchs dystrophy may be autosomal dominant with incomplete penetrance 18. Another frequent cause of bullous keratopathy is corneal endothelial trauma, which can occur during intraocular surgery (eg, cataract removal) or after placement of a poorly designed or malpositioned intraocular lens implant. Bullous keratopathy after cataract removal is called pseudophakic bullous keratopathy (if an intraocular lens implant is present) or aphakic bullous keratopathy (if no intraocular lens implant is present).
Bullous keratopathy treatment
Treatment requires an ophthalmologist and includes topical dehydrating agents (eg, hypertonic [5%] sodium chloride 5% drops and ointment), intraocular pressure–lowering agents, occasional short-term use of therapeutic soft contact lenses for some mild to moderate cases, and treatment of any secondary microbial infection. Although treatment with a topical hypertonic solution temporarily improves corneal clarity, cornea transplant or keratoplasty is the only treatment that will significantly improve visual acuity 5. Endothelial keratoplasty maintains most of the corneal structure and the integrity of the eye as a result of a small incision, no sutures and rapid recovery; therefore, it is increasingly becoming the preferred method for treating bullous keratopathy 19. The preferred surgical procedure for bullous keratopathy has changed recently from penetrating keratoplasty to endothelial keratoplasty such as Descemet’s stripping automated endothelial keratoplasty (DSAEK) 6 or Descemet’s membrane endothelial keratoplasty (DMEK) 7. This change has improved visual outcome 8 and reduced the frequency of graft rejection 9. The Eye Bank Association of America Statistical Report has revealed that endothelial keratoplasty has accounted for up to 30% of total corneal grafting since 2008, underlining the facts that the number of endothelial keratoplasty operations is increasing and that the indications for such surgery are expanding worldwide 10.
However, not all of the patients with bullous keratopathy can benefit from endothelium transplantation. Particularly in patients with a long duration of bullous keratopathy, endothelial keratoplasty cannot produce good vision because of the intense corneal stromal scars and neovascularization; thus, penetrating keratoplasty should be used 20.
References- Gharaee H, Ansari-Astaneh MR, Armanfar F. The effects of riboflavin/ultraviolet: a corneal cross-linking on the signs and symptoms of bullous keratopathy. Middle East Afr J Ophthalmol. 2011;18(1):58–60. doi:10.4103/0974-9233.75889 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3085154
- Liu T, Xu Y, Sun D, Xie L. Histological evaluation of corneal scar formation in pseudophakic bullous keratopathy. PLoS One. 2012;7(6):e39201. doi:10.1371/journal.pone.0039201 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375240
- Liu GJ, Okisaka S, Mizukawa A, Momose A. Histopathological study of pseudophakic bullous keratopathy developing after anterior chamber of iris-supported intraocular lens implantation. Jpn J Ophthalmol. 1993;37:414–425.
- Kenney MC, Chwa M. Abnormal extracellular matrix in corneas with pseudophakic bullous keratopathy. Cornea. 1990;9:115–121.
- Tan DT Janardhanan P Zhou H Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology . 2008;115:975–982.
- Price MO Price FW Jr. Descemet stripping with endothelial keratoplasty for treatment of iridocorneal endothelial syndrome. Cornea . 2007;26:493–497.
- Ham L van Luijk C Dapena I Endothelial cell density after Descemet membrane endothelial keratoplasty: 1- to 2-year follow-up. Am J Ophthalmol . 2009;148:521–527.
- Terry MA. Endothelial keratoplasty: clinical outcomes in the two years following deep lamellar endothelial keratoplasty (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc . 2007;105:530–563.
- Lee WB Jacobs DS Musch DC Kaufman SC Reinhart WJ Shtein RM. Descemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology . 2009;116:1818–1830.
- Boimer C Lee K Sharpen L Mashour RS Slomovic AR. Evolving surgical techniques of and indications for corneal transplantation in Ontario from 2000 to 2009. Can J Ophthalmol . 2011;46:360–366.
- Shih CY Ritterband DC Rubino S Visually significant and nonsignificant complications arising from Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol . 2009;148:837–843.
- Guerra FP Anshu A Price MO Price FW. Endothelial keratoplasty: fellow eyes comparison of Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Cornea . 2011;30:1382–1386.
- Abnormalities of Stromal Structure in the Bullous Keratopathy Cornea Identified by Second Harmonic Generation Imaging Microscopy. Investigative Ophthalmology & Visual Science July 2012, Vol.53, 4998-5003. doi:https://doi.org/10.1167/iovs.12-10214
- Gomes JA, Haraguchi DK, Zambrano DU, Izquierdo Júnior L, Cunha MC, de Freitas D. Anterior stromal puncture in the treatment of bullous keratopathy: Six-month follow-up. Cornea. 2001;20:570–2.
- Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N Engl J Med. 2018;378:995-1003.
- Brianne N. Hobbs, Robert Fintelmann. Cultured Cells and Inhibitor May Restore Cornea in Patients with Bullous Keratopathy – Medscape – 01Jan https://www.medscape.com/viewarticle/898384
- Moshirfar M, Somani AN, Vaidyanathan U, et al. Fuchs Endothelial Dystrophy (FED) [Updated 2019 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545248
- Zhang J, McGhee CNJ, Patel DV. The Molecular Basis of Fuchs’ Endothelial Corneal Dystrophy. Mol Diagn Ther. 2019 Feb;23(1):97-112.
- Khor WB, Mehta JS, Tan DT. Descemet stripping automated endothelial keratoplasty with a graft insertion device: surgical technique and early clinical results. Am J Ophthalmol. 2011;151:223–232.
- Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, et al. Descemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116:1818–1830.