Anorectal malformation
Anorectal malformation is the general term a wide spectrum of diseases often referred to as imperforate anus (the lower end of the digestive tract don’t develop properly), which can affect boys and girls, and involve the distal anus and rectum as well as the urinary and genital tracts 1. Babies with anorectal malformation do not have a normal anal opening, but instead, a fistulous tract opens onto the perineum anterior to the anal muscle complex or into adjacent anatomical structures. In the male, the fistulous tract can connect to the urinary system and in a female, to the gynecologic structures 1. The distance the fistulous tract opens from where the proper location of the anal opening usually determines the severity of the defect. The further the fistulous tract opens from the normal anatomic location, the more likely it is that there are additional associated issues such as underdeveloped musculature and anal muscle complex. Correctly classifying the anorectal malformation has significance regarding the patient’s prognosis, and it is a crucial component of determining the patients’ long term potential for bowel control.
During a bowel movement, stool passes from the large intestine to the rectum and then to the anus, where stool exits the body. Muscles in the anal area help to control when we have a bowel movement. Nerves in the area help the muscles sense the need for a bowel movement and also stimulate muscle activity. In anorectal malformations, the anus, rectum, surrounding nerves and muscles (the lower end of the digestive tract) do not develop properly. The severity of the condition can vary greatly from child to child.
Anorectal malformations include several different abnormalities, including:
- The anal passage may be narrow.
- A membrane may be present over the anal opening.
- The rectum may not connect to the anus (imperforate anus).
- The rectum may connect to a part of the urinary tract or the reproductive system through an abnormal passage called a fistula.
Newborns who have an imperforate anus may also have other congenital anomalies. A commonly used acronym, VACTERL, describes the associated problems that infants with imperforate anus may have:
- Vertebral defects
- Anorectal malformation
- Cardiac anomalies
- Tracheoesophageal fistula
- Esophageal atresia
- Renal (kidney) anomalies
- Limb anomalies
Anorectal malformations occur in approximately 1 in every 5000 live births 2. Anorectal malformations are slightly more common in males (1.2 to 1). The majority of male patients with an anorectal malformation have some form of connection to the urinary system, or a recto-urethral fistula (approximately 70% of this patient population). The most common type of anorectal malformation in female patients is a recto-vestibular fistula.
Defects range from the very minor and easily treated with an excellent functional prognosis, to those that are complex, difficult to manage, are often associated with other anomalies, and have a poor functional prognosis 1. The surgical approach to repairing these defects changed dramatically in 1980 with the introduction of the posterior sagittal approach, which allowed surgeons to view the anatomy of these defects clearly, to repair them under direct vision, and to learn about the complex anatomic arrangement of the junction of rectum and genitourinary tract. Better imaging techniques, and a better knowledge of the anatomy and physiology of the pelvic structures at birth have refined diagnosis and initial management, and the analysis of large series of patients allows better prediction of associated anomalies and functional prognosis. The main concerns for the surgeon in correcting these anomalies are bowel control, urinary control, and sexual function. With early diagnosis, management of associated anomalies and efficient meticulous surgical repair, patients have the best chance for a good functional outcome. Fecal and urinary incontinence can occur even with an excellent anatomic repair, due mainly to associated problems such as a poorly developed sacrum, deficient nerve supply, and spinal cord anomalies. For these patients, an effective bowel management program, including enema and dietary restrictions has been devised to improve their quality of life.
Key points about anorectal malformations in newborn
- Anorectal malformations are birth defects. The anus and rectum do not develop properly.
- An anorectal malformation causes problems with how a child has a bowel movement.
- Most babies with this problem will need surgery to correct it.
- Depending on the type of malformation, your child may have good control of bowel movements after the problem is repaired.
- If your child can’t control his or her bowel movements, a bowel management program can be very helpful.
How can I help my child live with an anorectal malformation?
Sometimes children are able to gain good control over their bowel movements after the problem is repaired. This is often the case for children with an anal membrane or a narrow anal passage.
If your child has a more complex type of anorectal malformation, he or she may need to take part in a bowel management program. This can help your child control bowel movements and prevent constipation. The nurses and other healthcare professionals who work with your child’s doctor can help create a program for your child.
Anorectal malformation cause
Most of the time, the cause for an anorectal malformation is unknown, but in rare cases, it appears to run in families, it is very likely that genetic factors play a role in their development 1. Boys are at a slightly higher risk for anorectal malformation than girls. The incidence of having a second child with an anorectal malformation is approximately one percent 3.
Up to one third of babies who have genetic syndromes, chromosomal abnormalities or other congenital defects also have imperforate anus or other anorectal malformations. These genetic syndromes and other congenital problems include:
- VACTERL association (vertebral anomalies, anal atresia, cardiac malformations, tracheoesophageal fistula, renal anomalies, and limb anomalies), a syndrome in which there are vertebral (spine), anus, cardiac (heart), trachea, esophagus, kidneys and limb (arms and legs) abnormalities.
- Down syndrome (Trisomy 21)
- Townes-Brocks syndrome. This syndrome includes problems with the anus, kidneys, ears, and arms and legs.
- Digestive system abnormalities
- Urinary tract abnormalities
- Abnormalities of the spine
There are several genetic syndromes with an increased incidence of anorectal malformations such as the Currarino triad which exhibits autosomal dominant inheritance, and patients with Trisomy 21 (Down syndrome) have a known association with anorectal malformation without fistula. Approximately 95% of patients with trisomy 21 have anorectal malformation without fistula compared to only 5% of all patients with anorectal malformations 2. There is also some data to suggest environmental factor exposures may be related to the development of anorectal malformations such as in vitro fertilization, thalidomide exposure, and diabetes 4. Animal models have also shown exposure to trans-retinoic acid, and ethylene thiourea correlates with anorectal malformations 4.
Several theories address the pathophysiology and development of anorectal malformations. One theory is related to the hypothesis that embryonically the urinary tract, reproductive tract, and gastrointestinal tract form a common channel called a cloaca, which is followed by separation of these structures and the migration of the anorectal septum around the seventh week of gestation 5. This theory hypothesizes that abnormal development of the anorectal septum results in the formation of anorectal malformations. However, there is still ongoing discussion about how the septum forms or if it is even related to the creation of anorectal malformations. A second theory hypothesizes that the rectum migrates towards the perineum during development, and this is abnormal in the formation of anorectal malformations. Neither of these theories has confirmation from embryologic models, and further work is needed to improve our understanding of anorectal malformations and their cause 6.
Anorectal malformation types
Comparing the results of reported series has always been a problem with anorectal malformations because different surgeons use different terminology when referring to types of imperforate anus. There is a spectrum of defects, so every attempt to classify them is arbitrary and somewhat inaccurate. Consequently, the traditional classification of “high”, “intermediate”, and “low” defects renders the results dubious 2.
There are several types of imperforate anus, each of which can affect your child’s ability to have normal bowel movements. These include:
- A membrane covering the anal opening
- Anal opening in an abnormal location
- Rectum is not connected to the anus and ends in a blind pouch
- Rectum is connected to part of the urinary tract or the reproductive system through a passage called a fistula, with no anal opening
Classification of non-syndromic anorectal malformations:
- Males
- Recto-perineal fistula
- Recto-urethral-bulbar fistula
- Recto-urethral-prostatic fistula
- Recto-bladderneck fistula
- Imperforated anus without fistula
- Complex and unusual defects
- Females
- Recto-perineal fistula
- Recto-vestibular fistula
- Cloaca with short common channel (< 3 cm)
- Cloaca with long common channel (> 3 cm)
- Imperforated anus without fistula
- Complex and unusual defects
- Cloacal extrophy, covered cloacal extra
- Posterior cloaca
- Associated to presacral mass
- Rectal atresia
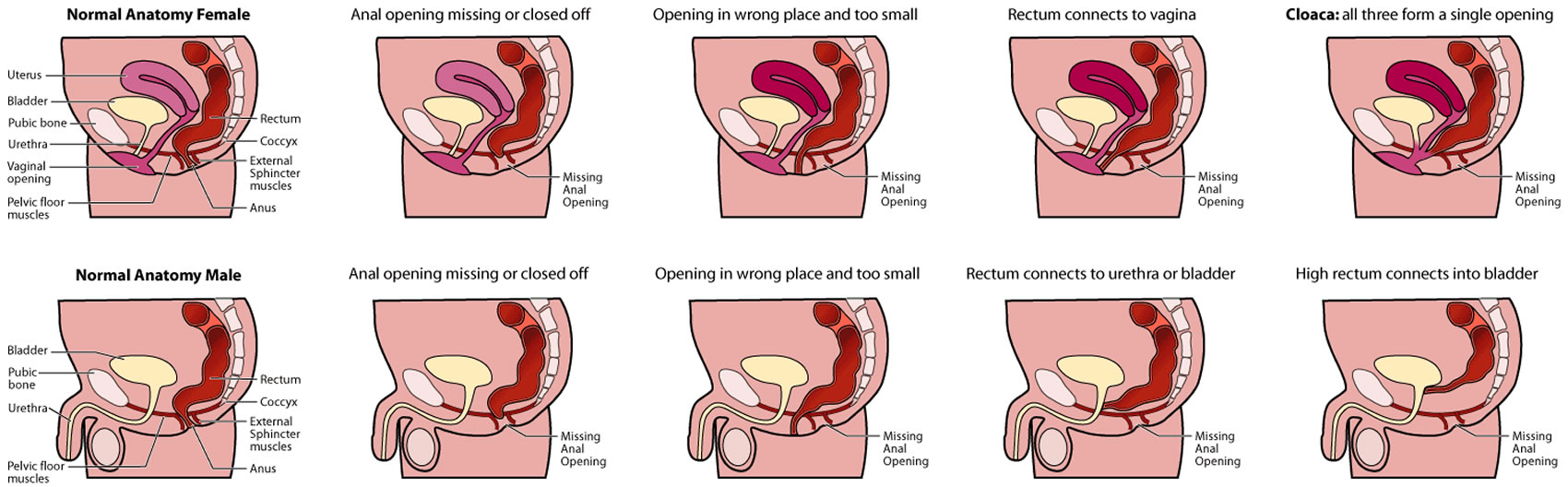
Anorectal malformations, including imperforate anus, can affect male and female babies in different ways 7.
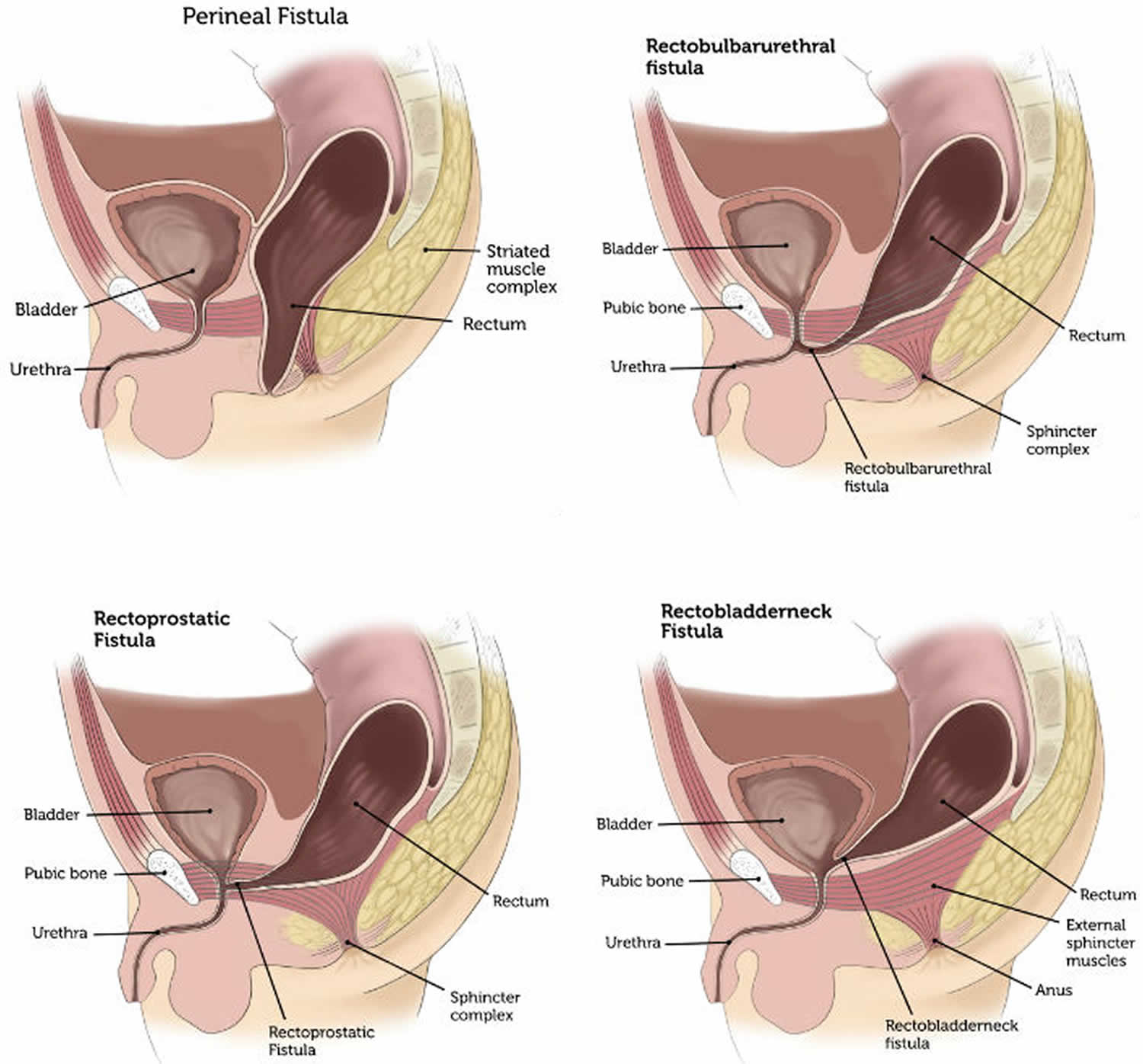
- In boys, the main anorectal malformations are perineal fistula, rectobulbarurethral fistula, rectoprostatic fistula and rectobladderneck fistula.
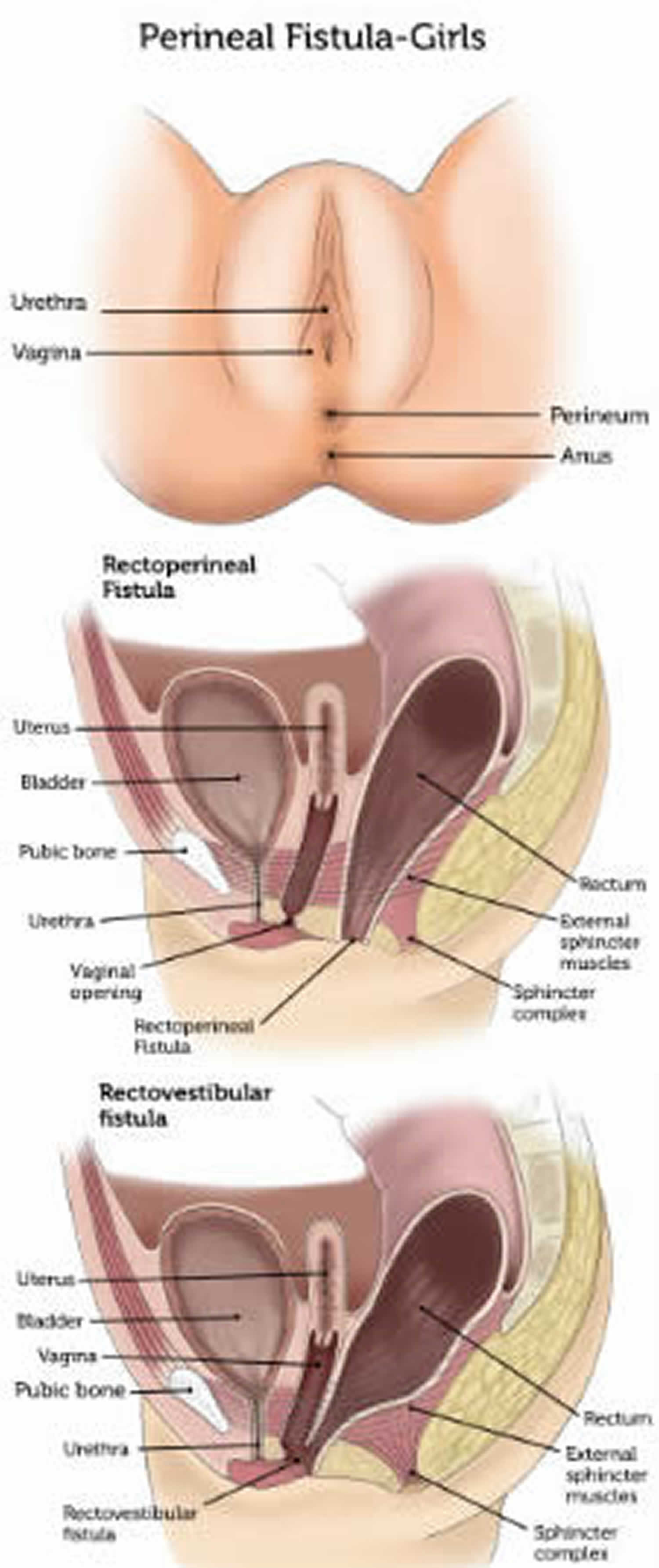
- In girls, the main anorectal malformations are rectoperineal fistula, rectovestibular fistula and cloaca.
- A type of anorectal malformation called imperforate anus can occur in both boys and girls.
Table 1. Detailed classification of anorectal malformations
| Non-syndromic anorectal malformation | Non-syndromic anorectal malformation with fistula | Recto-perineal malformations | |
| Imperforate anus with recto-urethral fistula | ◦ Recto-urethral bulbar fistula ◦ Recto-urethral prostatic fistula ◦ Bladderneck fistula | ||
| Imperforate anus in female | ◦ Recto-vestibular fistula ◦ Recto-vaginal fistula ◦ Cloacal malformation | ||
| Non-syndromic anorectal malformation without fistula | Imperforate anus without fistula | ||
| Complex anorectal malformation | ◦ Cloacal malformations with a short common channel (< 3 cm) | ||
| ◦ Cloacal malformations with a long common channel (> 3 cm) | |||
| ◦ H-shaped fistula (recto-vaginal) | |||
| ◦ Rectal duplication | |||
| Syndromic anorectal malformation | VACTERL (Vertebral anomalies, anal atresia, cardiac malformations, tracheoesophageal fistula, renal anomalies, and limb anomalies) | ||
| MURCS (Mullerian duct aplasia, renal aplasia, and cervicothoracic somite dysplasia) | |||
| OEIS (Omphalocele, exstrophy, imperforate anus, and spinal defects) | |||
| Axial mesodermal dysplasia | |||
| Klippel-Feil syndrome | |||
| Sirenomelia-caudal regression | |||
| Trisomy 21 | |||
| Trisomy 13 | |||
| Trisomy 18 | |||
| Pallister-Killian syndrome | |||
| Cat-eye syndrome | |||
| Parental unidisomy 16 | |||
| Deletion 22q11 syndrome (del22q11.2) | |||
| Currarino syndrome | |||
| Pallister-Hall syndrome | |||
| Townes-Brock syndrome | |||
| Ulnar-mammary syndrome | |||
| Okihiro syndrome | |||
| Rieger syndrome | |||
| Thanatophoric dwarfism | |||
| Hirschsprung disease | |||
| Feingold syndrome | |||
| Kabuki syndrome | |||
| Optitz BBB/G syndrome | |||
| Johanson-Blizzard syndrome | |||
| Spondylocostal dysostosis | |||
| Short rib – polydactyly syndrome | |||
| Baller-Gerold syndrome | |||
| Ciliopathies | |||
| Fraser syndrome | |||
| Lowe syndrome | |||
| Heterotaxia | |||
| FG syndrome | |||
| X-linked mental retardation | |||
| MIDAS syndrome | |||
| Christian syndrome | |||
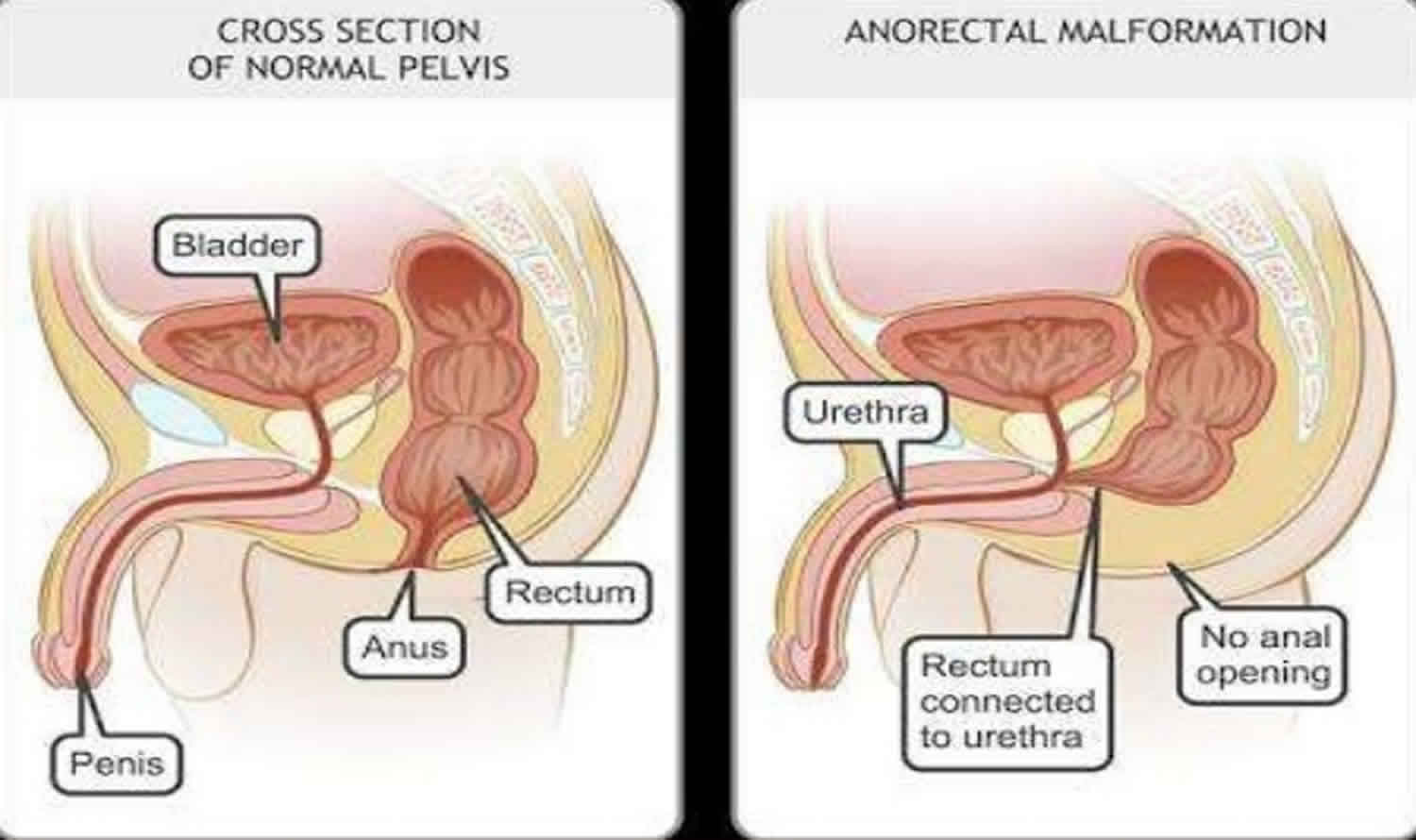
Figure 1. Anorectal malformation types
Figure 2. Anorectal malformation types in boys
Figure 3. Anorectal malformation types in girls
Figure 4. Anorectal malformation type imperforate anus
Anorectal malformation symptoms
Anorectal malformations like imperforate anus cause abnormalities in the way your child has a bowel movement. These problems will vary depending on the type of anorectal malformation:
- If the anal passage is narrow, your baby may have a difficult time passing a stool, causing constipation and possibly discomfort.
- If there is a membrane over the anal opening, your baby may be unable to have a bowel movement.
- If the rectum is not connected to the anus but there is a fistula present, stool will leave your baby’s body through the fistula and enter the urinary tract instead of the anus. This can cause urinary infection.
- If the rectum is not connected to the anus and there is not a fistula present, there is no way for the stool to leave the intestine. Then, your baby will be unable to have a bowel movement and will have a blockage of the intestine as a newborn.
Most anorectal malformations are found before a newborn leaves the hospital. If anorectal malformation is not found in the hospital, symptoms may include:
- Lack of stool
- Stool coming from the vagina
- Stool in the urine
- Urine coming from the anus
- Trouble having a bowel movement, or constipation
See your child’s healthcare provider right away if an anorectal malformation was not found in the hospital but your child:
- Passes stool from her vagina
- Passes stool in the urine
- Passes urine from the anus
- Has constipation
If your baby does not pass stool, it is a medical emergency. You should seek medical care right away.
Anorectal malformation complications
An anorectal malformation can cause problems in the way your child has a bowel movement. These problems will vary depending on the type of malformation your child has. These include:
- Narrow anal passage. Your child may have trouble passing a bowel movement. This causes constipation and possibly mild pain.
- Membrane over the anal opening. Your baby may be unable to have a bowel movement.
- Rectum is not connected to the anus, but there is a fistula. Stool will leave your baby’s body through the fistula instead of the anus. This can cause infections.
- Rectum is not connected to the anus, and there is no fistula. There is no way for stool to leave the intestine. Your baby will be unable to have a bowel movement. If this is not treated, it can be fatal.
Anorectal malformation diagnosis
Your baby’s physician will perform a physical examination when your baby is born, and will look at the anus to see if it is open and in the proper position. If the doctor suspects an anorectal malformation, he or she may order diagnostic imaging to get more details on the severity of the problem.
Diagnostic tests for evaluation of imperforate anus and associated anomalies may include:
- Abdominal X-rays to help locate the degree and position of the anorectal malformation; evaluate for possible esophageal abnormalities; evaluate the bones of the spine and limbs; identify an abnormal connection of the rectum
- Abdominal ultrasound to identify associated problems of the kidneys and genitourinary tract and evaluate the spinal cord
- MRI to evaluate the pelvic anatomy and the spine
- Echocardiogram to evaluate the heart
- CT scan. This test uses X-rays and a computer to make images of any part of the body. This includes the bones, muscles, fat, and organs. A CT scan is more detailed than a general X-ray. Older children may have a general X-ray.
- Lower GI or gastrointestinal series, also called a barium enema. This test checks the rectum, the large intestine, and the lower part of the small intestine. A metallic, chalky fluid called barium is put into the rectum as an enema. It coats the inside of organs so that they will show up on an X-ray. An X-ray of the belly or abdomen shows narrowed areas called strictures, blockages, and other problems.
- Upper GI or gastrointestinal series, also called barium swallow. This test checks the organs of the upper part of the digestive system. That includes the food pipe or esophagus, the stomach, and the first section of the small intestine, called the duodenum. A metallic, chalky fluid called barium is swallowed. It coats the inside of organs so that they will show up on an X-ray. Then X-rays are taken to check the digestive organs.
The majority of patients with anorectal malformations receive their diagnosis as newborns. A full newborn physical exam is vital in these patients as is a thorough work up as approximately 60% of patients will have an associated anomaly.
In addition to a perineal/anal exam, which is mandatory, a full physical newborn examination in a patient with an anorectal malformation includes listening to heart sounds to see if a murmur can be auscultated, examining the limbs for any anatomic abnormality, and a full genitourinary exam.
For an anus to be normal, it should be in the correct location and the proper size, based on age. The normal size anus of a full-term infant is a 10 to 12 Hegar dilator (an instrument used to size the anus), and the size of a 12-month-old should be about a 15 Hegar dilator. The basis of the correct location is on the anal opening being in the center of the anal muscle complex. The position of the anal opening to the muscle complex cannot always be discerned in the clinic and often requires an exam under anesthesia.
The perineum should be thoroughly evaluated taking care to pay attention to features such as the development of the buttocks, the presence of a gluteal fold, and the examination for any type of opening or orifice on the perineum. In female patients with an anorectal malformation, a thorough vaginal exam should also take place, taking care to note the number of openings on the perineum. These physical exam features can help give clues as to the type of anorectal malformation.
Multiple diagnostic studies are necessary for patients diagnosed with an anorectal malformation. While anorectal malformations can occur as an isolated finding, they require additional workup as 60% of patients have an associated anomaly, and there is a correlation of anorectal malformations with the VACTERL defects (vertebral, anorectal, cardiac, tracheoesophageal fistula/esophageal atresia, renal, and limb) 2.
Because of the known VACTERL association with anorectal malformations, for every newborn diagnosed with an anorectal malformation on physical exam, the following radiographic studies are necessary. After placement of a nasogastric or orogastric tube, plain abdominal and chest films should be obtained to rule out the presence of esophageal atresia with or without tracheoesophageal fistula. Spine radiographs should also be obtained to rule out vertebral anomalies. In male patients, if the presence of meconium on the perineum without an apparent perineal fistula does not present at 24 hours of life, a lateral prone film, or invertogram, should be obtained. Before obtaining the invertogram, the patient should be positioned prone with the buttocks elevated for at least 15 minutes so that air in the gastrointestinal tract has time to migrate to the most distal rectum; this will aid in the assessment of the most distal level of the bowel and help to determine the need for a colostomy. For female patients with a single perineal orifice and a cloaca diagnosis, an abdominal ultrasound should be obtained to both evaluate for hydrocolpos and hydronephrosis. Additionally, an echocardiogram is in order for all patients with an anorectal malformation to rule out congenital heart issues, and a spinal ultrasound should be obtained to screen for the tethered spinal cord. The sacral ratio should also be calculated from anteroposterior and lateral films as this helps give prognostic information to the families about bowel control for the child as they grow and develop 2.
Anorectal malformation treatment
The majority of newborns with anorectal malformations will need to have surgery to correct the problem. There are several different approaches to surgery for pediatric anorectal malformations. The specific approach and number of operations necessary depends on the complexity and type of malformation.
- A posterior sagittal anorectoplasty (PSARP) is the standard technique used for repair. This surgical method can be used when the pediatric colorectal surgeon is certain of the anatomy. Posterior sagittal anorectoplasty repair is performed by making an incision which divides the muscles in the middle of the bottom where the new anal opening will be located. The rectum is then moved into the correct position between the muscles, and a new anus is created in the perineum. Sometimes the posterior sagittal anorectoplasty surgery can be performed in the newborn period.
- More commonly, the malformation is complex and a temporary colostomy will be performed, followed by imperforate anus surgery at a later date. A colostomy is an operation that diverts the path of stool to a bag which is secured to the skin. Your child is allowed to go home and grow for a few months. Your child will return to the doctor for additional X-rays to assess the location and severity of the malformation before undergoing surgery to move the rectum to the correct position and create a new anal opening. The colostomy will be reversed at a later date, often one to two months after surgery.
After surgery, the newly formed anus needs to be regularly dilated for several months. Anal dilation helps prevent narrowing of the scar tissue that could block the opening. Our Colorectal Program team will assist you with anal dilations.
Narrow anal passage
Babies who have the type of malformation that causes the anal passage to be narrow may not need an operation. A procedure known as anal dilatation may be done periodically to help stretch the anal muscles so stool can pass through it easily. However, if the anal opening is positioned incorrectly, an operation may be needed to relocate it.
Anal membrane
Babies with this type of malformation will need to have the membrane removed during surgery. Anal dilatations may need to be done afterward to help prevent narrowing of the anal passage.
Lack of rectal-anal connection (with or without a fistula)
These babies may need a series of operations in order to have the malformation repaired.
The first procedure is called a colostomy. In a colostomy, the large intestine is divided into two sections and the ends of intestine are brought through openings in the abdomen. The upper section allows stool to pass through the opening (called a stoma) and then into in a collection bag. The lower section allows mucus that is produced by the intestine to pass into a collection bag. By doing a colostomy, the baby’s digestion will not be impaired and she can grow before the time for the next operation. Also, when the next operation is done on the lower section of intestine, there will not be any stool present to infect the area. The nursing staff and other health care professionals that work with your baby’s surgeon can help you learn to take care of the colostomy. Local and national support groups may also be of help to you during this time.
The next operation attaches the rectum to the anus and is usually done within the first few months of a baby’s life. The colostomy remains in place for a few months after this operation so the area can heal without being infected by stool. Even though the rectum and anus are now connected, stool will leave the body through the colostomy until it is closed with surgery. A few weeks after surgery, parents may start performing anal dilatations to help the baby get ready for the next phase of treatment.
Two to three months later, an operation is done to close the colostomy. The baby is not allowed to eat anything for a few days after surgery while the intestine is healing.
Several days after surgery, the baby will start passing stools through the rectum. At first, stools will be frequent and loose. Diaper rash and skin irritation can be a problem at this time. Within a few weeks after surgery, the stools become less frequent and more solid, often causing constipation. Your baby’s physician may recommend a high fiber diet (including fruits, vegetables, juices, whole-wheat grains and cereals) to help with constipation.
Perineal fistulas and rectovestibular fistulas
For patients with perineal fistulas, a repair can be performed in the neonatal period if the surgeon is comfortable with the procedure, and there are no other anomalies that would preclude anesthesia such as a cardiac defect. The clinician can also delay the repair if the fistulous tract is large enough to perform dilations with a Hegar dilator and stool evacuation can be reliable. The same dilation strategy works for a female patient with a rectovestibular fistula as the anatomy can be challenging in the neonatal period, and dilating can allow the child to grow and improve the ease of surgical intervention.
For either patient population, it is crucial to ensure that stool is decompressing well with the dilation management, and the child is not becoming distended. If being managed with dilations, the surgical repair should occur at approximately 3 months of age. This way, the defect can undergo correction before transitioning to solid food, reducing the risk of development of constipation leading to rectal dilation that would impact function.
Surgical repair of these malformations is generally through a posterior sagittal incision, and the abdominal entry is not necessary.
Rectourethral fistulas or cloaca
Any male patient with a urinary fistula should undergo diversion in the neonatal period with a diverting descending sigmoid colostomy with a separated mucus fistula. This strategy allows for the child to grow before surgical intervention, and also evacuate stool from the distal limb of the bowel that connects to the urinary system. Furthermore, the mucus fistula allows for a distal colostogram to be performed preoperatively to determine the exact type of rectourethral fistula assisting with preoperative planning and operative strategy for repair.
Patients with a single perineal orifice consistent with a diagnosis of cloaca should also undergo a diverting ostomy and mucous fistula in the neonatal period. These patients also require much more complex preoperative and operative management as well as lifelong care and should be considered for referral to a specialty center.
The timing of the definitive repair of high malformations can depend on the exact type of malformation and other associated anomalies, especially cardiac defects. Typically, surgical repair occurs sometime around or after 3 months of age. Surgical repair can still be performed with a posterior sagittal incision if the rectum and the fistula present on the distal colostogram below the level of the coccyx. Laparoscopy can be a crucial surgical strategy for high malformations such as a recto-bladder neck fistula.
Anorectal malformation surgical complications
Complications can occur intraoperatively if care is not taken to stay in the correct tissue plane, which can also lead to misplacement of the anus or placement outside the center of anal muscle complex. Additional intraoperative complications for males can include injury to the urinary structures, including the urethra, seminal vesicles, and vas deferens. In females, the vagina can suffer injury.
Post-operative complications can include superficial and deep wound infection, dehiscence of the anastomosis, prolapse of the anoplasty, or stricture of the anoplasty. Recurrent fistulas between the urinary system in males or gynecologic system in females can also occur. These usually occur if the surgical repair is on excessive tension or there is inadequate blood supply to the rectum. Recurrent fistulas can also occur in the setting of an intraoperative injury to the anterior structures such as the urethra or the vagina. In this setting, care should be taken to ensure the healthy rectal wall as opposed to the repaired structure, and a fat pad should also be placed to buttress the repair.
Anorectal malformation prognosis
The long-term outlook depends on the type of anorectal malformation and is related to long term potential for bowel control, or the ability to be continent. The three factors that can help predict continence are the type of anorectal malformation, the sacral ratio, and the spinal cord quality. The further the fistula is from the normal anatomic location, the less the chance of continence for the child as they grow older. A low sacral ratio can also be indicative of decreased continence. Spinal issues, such as tethered cord, if present, are also a negative prognostic indicator for continence. However, despite these predictors being present, a child with these prognostic factors can still be clean and socially continent with an appropriate bowel management program and specialty care.
Children with a low lesion, especially those who require only a perineal anoplasty, may have constipation that can generally be treated with oral medications.
Children with spinal abnormalities of the lower sacrum and a high imperforate anus often do not have normal bowel continence or function. These patients are helped by a bowel management program with dietary changes, medications, and regular enemas.
Children who had the type of malformation that involves an anal membrane or a narrow anal passage are usually able to gain good control over their bowel movements after the malformation is repaired.
Children with more complex anorectal malformations may need to participate in a bowel management program to help them achieve control over their bowel movements and prevent constipation.
Your child can begin toilet training at the usual age, which is generally between two and three years old. However, children who have had anorectal malformations repaired may be slower than others to gain bowel control. Some children may not be able to gain good control over their bowel movements, while others may be chronically constipated, depending on the type of malformation and its repair.
Sometimes these children also have difficulty controlling urine and do not properly toilet train, remain wet after training or develop repeated urinary infection. Imaging of the urinary tract with a renal ultrasound and a voiding cystourethrogram (a special bladder X-ray) may help clarify the cause of these problems.
References- Smith CA, Avansino J. Anorectal Malformations. [Updated 2019 May 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542275
- Levitt MA, Peña A. Anorectal malformations [published correction appears in Orphanet J Rare Dis. 2012;7:98]. Orphanet J Rare Dis. 2007;2:33. Published 2007 Jul 26. doi:10.1186/1750-1172-2-33 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1971061
- Falcone RA, Levitt MA, Peña A, Bates M. Increased heritability of certain types of anorectal malformations. J. Pediatr. Surg. 2007 Jan;42(1):124-7; discussion 127-8.
- Mundt E, Bates MD. Genetics of Hirschsprung disease and anorectal malformations. Semin. Pediatr. Surg. 2010 May;19(2):107-17.
- Kluth D. Embryology of anorectal malformations. Semin. Pediatr. Surg. 2010 Aug;19(3):201-8.
- Penington EC, Hutson JM. The cloacal plate: the missing link in anorectal and urogenital development. BJU Int. 2002 May;89(7):726-32.
- Anorectal Malformations. http://www.childrenshospital.org/conditions-and-treatments/conditions/a/anorectal-malformation