Cervicogenic headache
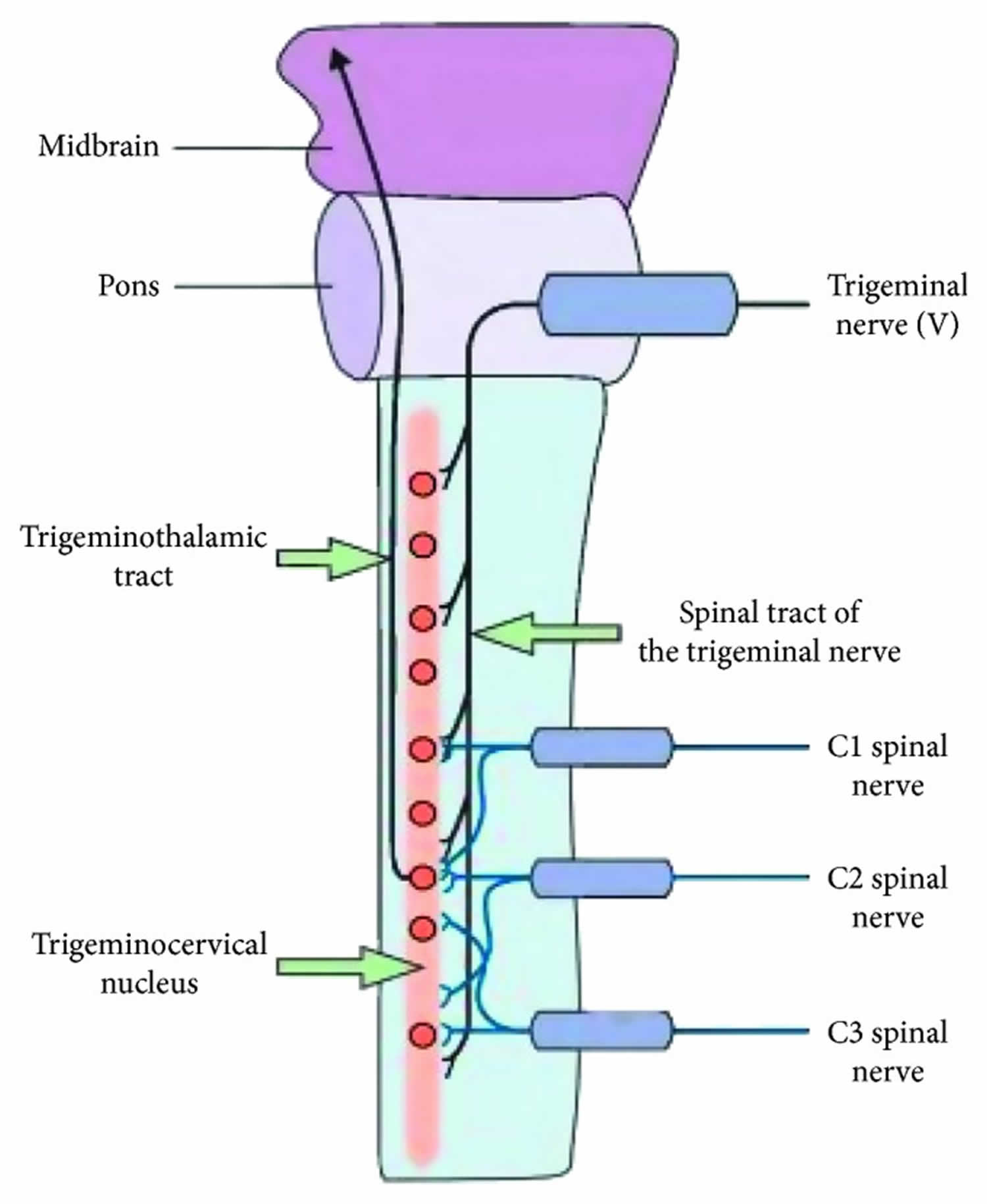
Cervicogenic headache presents as unilateral chronic headache that starts in the neck that is often misdiagnosed 1. Cervicogenic headaches pose a challenge for many sports physical therapists because the head pain results from somewhere other than the head: the cervical spine 2. The presenting features can be complex and similar to many primary headache syndromes that are encountered daily. Cervicogenic headache is a common chronic and recurrent headache that usually starts after neck movement. It usually accompanies a reduced range of motion (ROM) of the neck. Cervicogenic headache could be confused with a migraine, tension headache, or other primary headache syndromes. The symptoms of cervicogenic headache many arise from any of the components of the cervical spine, including vertebrae, disks, or soft tissue 3, though some research has shown that cervicogenic headache pain most commonly arises from the atlanto-occipital joint, atlantoaxial joint, the second and third cervical spine (C2/3) facet joints (zygapophysial joint), C2-3 intervertebral disc, cervical myofascial trigger points, followed by C5/6 facet joints 4. Furthermore, cervicogenic headache symptoms can be successfully managed at the second and third cervical rami (C2/3) with cervical rami blocks 5. The afferent fibers of the trigeminal nerve and the upper three cervical nerves converge on second-order sensory neurons at the dorsal horn of the upper cervical spinal cord 6. This convergence is the anatomical basis for the clinical observation that patients with cervicogenic headache often present with headache at both cervical and trigeminal dermatomes 7. Upper cervical spine mobility restriction (hypomobility), cervical pain, and muscle tightness are clinical findings associated with cervicogenic headache during physical examination 8.
A cervicogenic headache is a common cause of a chronic headache . The main symptoms of a cervicogenic headache are a combination of unilateral pain, ipsilateral diffuse shoulder, and arm pain. ROM in the neck is reduced, and pain is relieved with anesthetic blockades. Treatment includes physical therapy, exercise, and interventional procedures. Common treatments include blockade of the greater occipital nerve, the lesser occipital nerve, and the stellate ganglion. The differential diagnosis includes a migraine, hemicrania continua, spondylosis of the cervical spine, and tension-type headache.
A cervicogenic headache is a rare chronic headache in people who are 30 to 44 years old 1. It has been estimated that 4.1% of the population may experience cervicogenic headache, depending on how many criteria fulfilled and based on many different studies 9. Cervicogenic headache is one of the more common types of headache and may account for 0.4–15% of the headache population 10 and up to 15–20% of all chronic and recurrent headaches 11. Women have been reported to be affected four times more frequently than men 12, although some research about prevalence between the sexes is contradictory 9. Age at onset is thought to be the early 30s, but the age the patients seek medical attention and diagnosis is 49.4 1. When compared with other headache patients, these patients have a pericranial muscle tenderness on the painful side and a significantly reduced cervicogenic headache 1. Patients who have sustained concussion 13 or whiplash injuries 3 with resulting neck pain and limitation of movement can also develop cervicogenic headache.
The International Headache Society has validated cervicogenic headache as a secondary headache type that is hypothesized to originate due to nociception in the cervical area 14. Cervicogenic headache was originally described as a unique disorder in 1983 and differentiated from other forms of headaches, such as migraine, that may present with some common symptoms 15. The International Headache Society issued its initial International Classification of Headache Disorders in 1988 16 and published revised editions in 2004 17 and in 2013 14. The current International Classification of Headache Disorders 3 beta version classifies cervicogenic headache as a secondary headache arising from musculoskeletal disorders in the cervical spine and is frequently accompanied by neck pain 14. Additionally, the Cervicogenic Headache International Study Group has also developed a list of clinically relevant diagnostic criteria that include pain with neck movement or sustained improper positioning, restricted cervical range of motion (ROM), and ipsilateral shoulder and arm pain 18.
Diagnostic criteria must include all the following points 19:
- Source of the pain must be in the neck and perceived in head or face.
- Evidence that the pain can be attributed to the neck. It must have one of the following: demonstration of clinical signs that implicate a source of pain in the neck or abolition of a headache following diagnostic blockade of a cervical structure or its nerve supply using a placebo or other adequate controls.
- Pain resolves within three months after successful treatment of the causative disorder or lesion.
People suspected of having cervicogenic headache should be carefully assessed by their doctor to exclude other primary (migraine, tension-type) or secondary (vessel dissection, posterior fossa lesions) causes of headaches.
Nerve blocks are used both for diagnostic and treatment purposes. If numbing the cervical structures abolishes the headache, that can confirm the diagnosis of cervicogenic headache and also provide relief from the pain.
Treatment for cervicogenic headache should target the cause of the pain in the neck and varies depending on what works best for the individual patient. Treatments include nerve blocks, medications and physical therapy and exercise. Physical therapy and an ongoing exercise regimen often produce the best outcomes. Other providers that may need to be involved in management of cervicogenic headache include physical therapists, pain specialists (who can do the injections/blocks) and sometimes neurosurgeons or orthopedic surgeons.
Because cervicogenic headache is a secondary type of headache, it is important for physical therapists to perform a manual examination of the vertebral segments in order to determine the primary cause of the headache from the dysfunctional cervical spine segment 20. Manual examinations may include passive physiological intervertebral motion as well as passive accessory intervertebral motion such as posteroanterior pressures. Motion limitation and symptoms, such as pain, headache reproduction, and stiffness, indicate the most dysfunctional segment at the time of the manual assessment 21. Due to the various anatomical and physiological dysfunctions, cervical mobilization and manipulation (manipulative therapy) are the frequently used treatments for patients diagnosed with cervicogenic headache, although the evidence surrounding the efficacy of these practices is conflicting 22.
Many studies on the short-term effectiveness and manual therapy to the cervical spine (mobilization and manipulative therapy) have found it beneficial in reducing headache pain or disability 23, intensity 23, frequency 24 and duration 23. Therapeutic effects for cervicogenic headache patients were also found in terms of improvement in neck pain and disability 25. Current research suggests that afferent input induced by manual therapy may stimulate neural inhibitory pathways in the spinal cord and can also activate descending inhibitory pathways in the lateral periaqueductal gray area of the midbrain 5. Jull et al. 26 concluded that manual therapy is effective in managing cervicogenic headache, and the effects of this study were maintained at a long-term follow-up. Thus, patients with cervicogenic headache could benefit from manual therapy techniques, including spinal manipulative therapy 27. If cervical manipulation is effective in reducing pain intensity and headache frequency in this patient population, this could be a beneficial treatment for physical therapists to incorporate into their interventions. However, evidence regarding the efficacy of this practice is conflicting 28.
Cervical spine anatomy
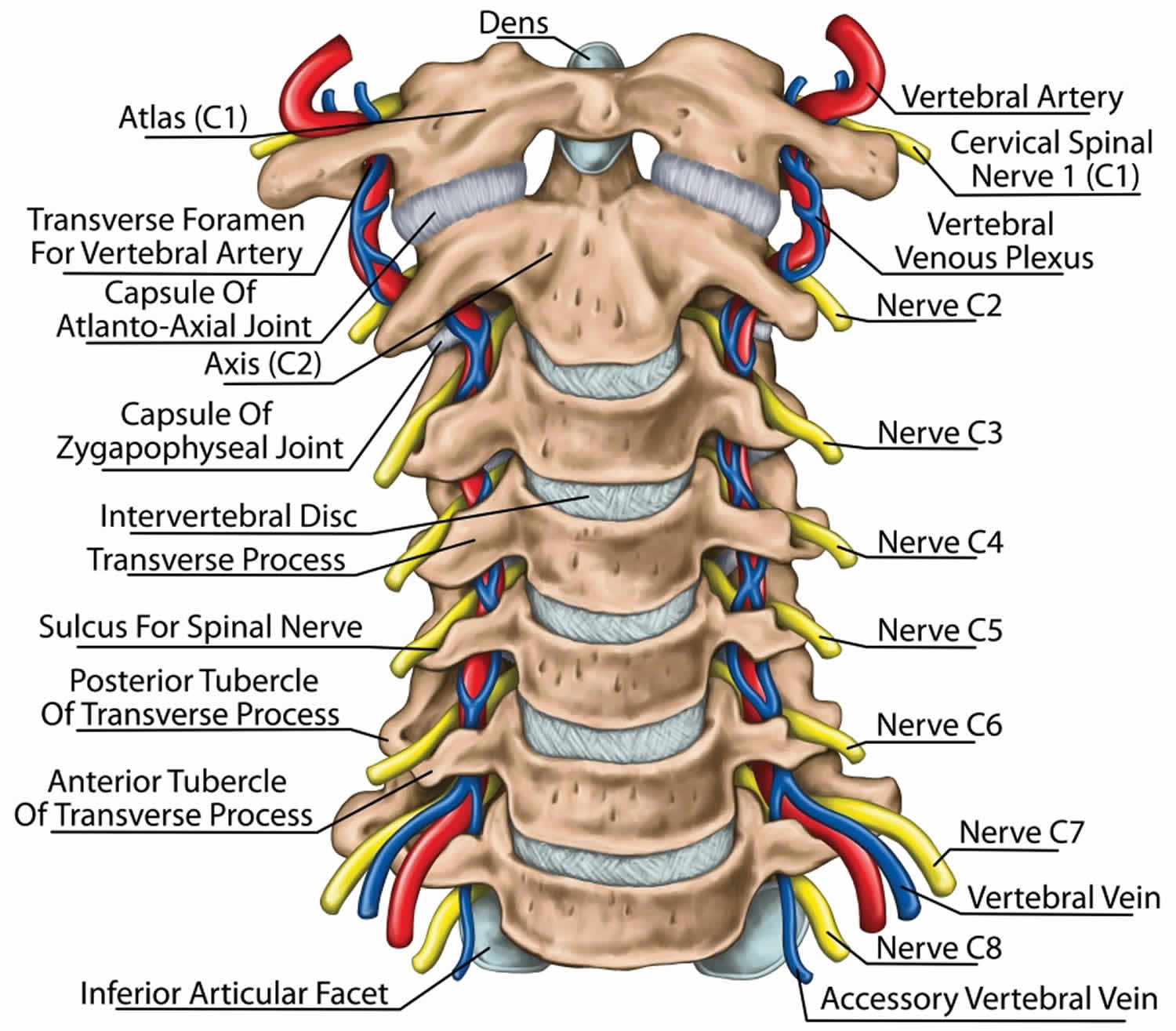
The cervical spine is made up of the first 7 vertebrae and functions to provide mobility and stability to the head, while connecting it to the relative immobile thoracic spine (see the image below). The first 2 vertebral bodies are quite different from the rest of the cervical spine. The atlas, or C1, articulates superiorly with the occiput and inferiorly with the axis, or C2.
The atlas is ring-shaped and does not have a body, unlike the rest of the vertebrae. The body has become part of C2, and it is called the odontoid process, or dens. The atlas is made up of an anterior arch, a posterior arch, 2 lateral masses, and 2 transverse processes. The transverse foramen, through which the vertebral artery passes, is enclosed by the transverse process. On each lateral mass is a superior and inferior facet (zygapophyseal) joint. The superior articular facets are kidney-shaped, concave, and face upward and inward. These superior facets articulate with the occipital condyles, which face downward and outward. The relatively flat inferior articular facets face downward and inward to articulate with the superior facets of the axis.
The axis has a large vertebral body, which contains the fused remnant of the C1 body, the dens. The dens articulates with the anterior arch of the atlas via its anterior articular facet and is held in place by the transverse ligament. The axis is composed of a vertebral body, heavy pedicles, laminae, and transverse processes, which serve as attachment points for muscles. The axis articulates with the atlas by its superior articular facets, which are convex and face upward and outward.
The remaining cervical vertebrae, C3-C7, are similar to each other, but they are very different from C1 and C2. They each have a vertebral body, which is concave on its superior surface and convex on its inferior surface. On the superior surfaces of the bodies are raised processes or hooks called uncinate processes, which articulate with depressed areas on the inferior aspect of the superior vertebral bodies called the echancrure or anvil. These uncovertebral joints are most noticeable near the pedicles and are usually referred to as the joints of Luschka 29. These joints are believed to be the result of degenerative changes in the annulus, which leads to fissuring in the annulus and the creation of the joint. The spinous processes of C3-C5 are usually bifid, in comparison to the spinous processes of C6 and C7, which are usually tapered.
The facet joints in the cervical spine are diarthrodial synovial joints with fibrous capsules. The joint capsules in the lower cervical spine are more lax compared with other areas of the spine to allow for gliding movements of the facets. The joints are inclined at 45° from the horizontal plane and angled 85° from the sagittal plane. This alignment helps to prevent excessive anterior translation and is important in weight bearing 30.
The fibrous capsules are innervated by mechanoreceptors (types I, II, and III), and free nerve endings have been found in the subsynovial loose areolar and dense capsular tissues 31. In fact, there are more mechanoreceptors in the cervical spine than in the lumbar spine 32. This neural input from the facets may be important for proprioception and pain sensation and may modulate protective muscular reflexes that are important in preventing joint instability and degeneration.
The facet joints in the cervical spine are innervated by both the anterior and dorsal rami. The occipitoatlantal joint and atlantoaxial joint are innervated by the ventral rami of the first and second cervical spinal nerves. Two branches of the dorsal ramus of the third cervical spinal nerve innervate the C2-C3 facet joint, a communicating branch and a medial branch known as the third occipital nerve.
The remaining cervical facets, C3-C4 to C7-T1, are supplied by the dorsal rami medial branches that arise one level cephalad and caudad to the joint 33. Therefore, each joint from C3-C4 to C7-T1 is innervated by the medial branches above and below. These medial branches send off articular branches to the facet joints as they wrap around the waists of the articular pillars.
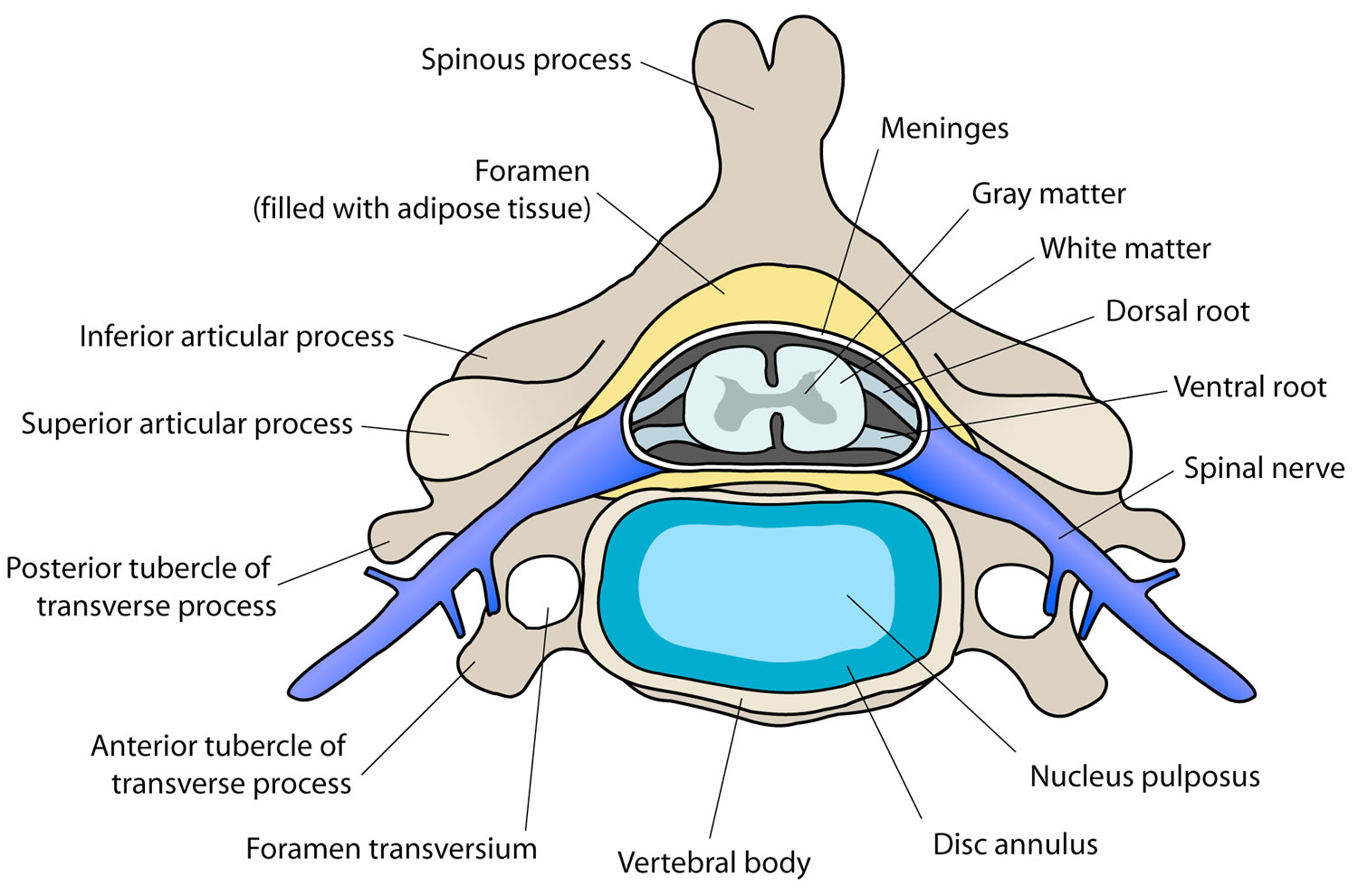
Intervertebral discs are located between each vertebral body caudad to the axis. The discs are composed of 4 parts, including the nucleus pulposus in the middle, the annulus fibrosis surrounding the nucleus, and 2 end plates that are attached to the adjacent vertebral bodies. The discs are involved in cervical spine motion, stability, and weight bearing. The annular fibers are composed of collagenous sheets called lamellae, which are oriented 65-70° from the vertical and alternate in direction with each successive sheet. Therefore, the annular fibers are prone to injury with rotation forces because only one half of the lamellae are oriented to withstand the force in this direction 32. The middle and outer one third of the annulus is innervated by nociceptors, and phospholipase A2 has been found in the disc and may be an inflammatory mediator 34.
Several ligaments of the cervical spine, which provide stability and proprioceptive feedback, are worth mentioning 35. The transverse ligament, the major portion of the cruciate ligament, arises from tubercles on the atlas and stretches across its anterior ring while holding the dens against the anterior arch. A synovial cavity is located between the dens and the transverse process. This ligament allows for rotation of the atlas on the dens and is responsible for stabilizing the cervical spine during flexion, extension, and lateral bending. The transverse ligament is the most important ligament in preventing abnormal anterior translation 36.
The alar ligaments run from the lateral aspects of the dens to the ipsilateral medial occipital condyles and to the ipsilateral atlas. The alar ligaments limit axial rotation and side bending. If the alar ligaments are damaged, as in a whiplash injury, the joint complex becomes hypermobile, which can lead to kinking of the vertebral arteries and stimulation of the nociceptors and mechanoreceptors. This may be associated with the typical complaints of patients with whiplash injuries such as headache, neck pain, and dizziness. The alar ligaments prevent excessive lateral and rotational motions, while allowing flexion and extension.
The anterior longitudinal ligament and the posterior longitudinal ligament are the major stabilizers of the intervertebral joints. Both ligaments are found throughout the entire length of the spine; however, the anterior longitudinal ligament is closely adhered to the discs in comparison to the posterior longitudinal ligament, and it is not well developed in the cervical spine. The anterior longitudinal ligament becomes the anterior atlantooccipital membrane at the level of the atlas, whereas the posterior longitudinal ligament merges with the tectorial membrane. Both ligaments continue onto the occiput. The posterior longitudinal ligament prevents excessive flexion and distraction 37.
The supraspinous ligament, interspinous ligament, and ligamentum flavum maintain stability between the vertebral arches. The supraspinous ligament runs along the tips of the spinous processes, the interspinous ligament runs between the spinous processes, and the ligamentum flavum runs from the anterior surface of the cephalad vertebra to the posterior surface of the caudad vertebra. The interspinous ligament and especially the ligamentum flavum control for excessive flexion and anterior translation 37. The ligamentum flavum also connects to and reinforces the facet joint capsules on the ventral aspect. The ligamentum nuchae is the cephalad continuation of the supraspinous ligament and has a prominent role in stabilizing the cervical spine.
Figure 1. Cervical spine
Figure 2. Cervical disc
Figure 3. Cervical facet joint
Cervicogenic headache causes
Recent studies have indicated that head and face pain in cervicogenic headache originate from disorders of the upper cervical nerves (C1–C3); therefore, any structure innervated by the C1–C3 spinal nerves could be the source for a cervicogenic headache [38. Lesions in the atlantooccipital joint, atlantoaxial joint, C2-C3 zygapophyseal joint, and intervertebral disk can all cause occipital pain 39. In contrast, there is no evidence that regions innervated by the lower cervical nerves directly induce headache. Thus, the spinal nerves and branches from C1–C3 are thought to be the main anatomical bases of cervicogenic headache.
The C1 spinal nerve (suboccipital nerve) innervates the atlantooccipital joint. Pathological change in or damage to this joint may cause pain to be referred in the occipital region. The C2 spinal nerve innervates the atlantoaxial and C2-C3 zygapophyseal joints and is adjacent to the lateral portion of the articular capsule of the C1-C2 zygapophyseal joint (atlantoaxial joint). Pathological changes or injures in these joints or the surrounding tissues can lead to referred pain in the head. The third occipital nerve (C3 medial branch) approaches and dominates the C2-C3 zygapophyseal joint, from where pain can radiate to the occipital, frontal, temporal, and periorbital regions (third occipital neuropathic headache) of the head.
Although the pain resulting from each pathology is not always consistent among patients, the distribution range of pain is typically similar. Neck pain originating near the cranium can radiate to the head, including the frontal and periorbital regions. Conversely, neck pain originating from the pars caudalis of the upper three cervical spines always causes pain in the occipital region. Moreover, a study showed that impairment of the C2-C3 zygapophyseal joint causes cervicogenic headache in 70% of patients 40, of whom 27% can be diagnosed with third occipital neuropathic headache. Deterioration of the C3-C4 zygapophyseal joints, upper cervical intervertebral discs, and lower cervical zygapophyseal joints are less common causes of cervicogenic headache.
Cervicogenic headache pathophysiology
The pathophysiology of cervicogenic headache is poorly understood, but it is thought to be a referred pain originating from pathological changes in the upper cervical zygapophyseal joints. As shown in Figure 4 41, anatomical convergence of pain fibers from the trigeminal nerve (including the ophthalmic division) and the upper three cervical nerves forms the basis for pain to be referred from the upper cervical region to the head, including radiation to the frontal and periorbital regions [13, 14]. The trigeminocervical nucleus receives not only the C1–C3 afferents but also the first branch of the trigeminal sensory afferents, indicating that it receives second-order neuron afferents from the trigeminal and upper three cervical spinal nerves. Therefore, pathological changes in the cervical zygapophyseal joints can generate pain in the areas innervated by either the trigeminal nerve (e.g., frontal and periorbital regions) or the upper three cervical spinal nerves (e.g., occipital and ear regions). Convergence between the trigeminal sensory descending tracts and the upper cervical nerve roots can also cause referred pain in the neck, face, and head.
The C1-C3 nerves relay pain signals to the nociceptive nucleus of the head and neck, the trigeminocervical nucleus. This connection is thought to be the cause for referred pain to the occiput and/or eyes 39. Aseptic inflammation and neurotransmission within the C-fibers that is caused by cervical disc pathology is thought to produce and worsen the pain in a cervicogenic headache. The trigeminocervical nucleus receives afferents from the trigeminal nerve as well as the upper three cervical spinal nerves. Neck trauma, whiplash, strain, or chronic spasm of the scalp, neck, or shoulder muscles can increase the sensitivity of the area which is similar to the allodynia that is seen in late chronic migraines. A lower pain threshold makes patients more susceptible to more severe pain. For this reason, early diagnosis and therapeutic intervention is very important.
Figure 4. Cervicogenic headache pathophysiology
Footnote: Mechanism of pain referral from the cervical spine to the head.
[Source 42 ]Cervicogenic headache symptoms
Patients usually complain of a unilateral pain without side shift. It is ordinarily predominant in females. Pain topography is usually stemming from the neck, spreading to the oculofrontotemporal area with episodes of carrying duration or fluctuating continuous pain. Pain is moderate to severe, but not excruciating. Pain can mimic primary headache syndromes such as tension headache or migraine headache, although the patient will be less likely to complain of sensitivity to light and noise as in migraine headache. It typically is associated with a reduced ROM of the neck. Patients will complain that the pain is not resolving with a triptan, ergotamine, or indomethacin. Autonomic symptoms such as photophobia or phonophobia, nausea, and vomiting are not as common.
Cervicogenic headache symptoms 42:
- Cervicogenic headache is a chronic unilateral headache; it is also a side-locked headache 43.
- Pain is first noted in the neck or occipital region before it radiates to the ipsilateral frontotemporal and orbital regions. Temporal regions are the most commonly affected.
- Cervicogenic headache is usually a deep, blunt, distending, and tense pain without pulsation. The frontotemporal region is the most painful, and the headache is aggravated by neck movements, fatigue, or an unhealthy neck position and relieved by rest.
- Headache may intermittently occur and last for hours or days, but during the late stages, it can cause persistent pain.
- Stiffness and a restricted range of motion in the neck may occur and be accompanied by ipsilateral shoulder or arm pain.
- Most patients also have concomitant symptoms of nausea, tinnitus, dizziness, phonophobia, photophobia, blurred vision, or disordered sleep.
Physical examination
Patients with cervicogenic headache are more likely to have myofascial trigger points on the transverse processes of the second cervical vertebra that can spread to the head and splenius capitis, trapezius, sternocleidomastoid, and suboccipital muscles 44. Tenderness is observed in the occiput, paravertebral muscles, mastoid process, unilateral or bilateral outlets of the greater occipital nerve, and transverse process of the third cervical vertebra 45. Patients often present with a limited range of motion of the cervical spine. There is no tenderness of the head and face.
Cervicogenic headache diagnosis
Imaging of the cervical spine is not sensitive enough for diagnosing a cervicogenic headache. No specific radiologic abnormalities were found by recent studies such as Pfaffenrath et al. and Fredriksen et al. The most frequent findings in the literature were a rectilinearization of the cervical spine and/or disc protrusions. Although not widely used in the clinical world, functional imaging shows a hypomobility or hypermobility at a certain level of the cervical spine. Magnetic resonance imaging (MRI) may show cervical disc degeneration, herniation, or bulging, mostly in the discs of C2–C5. Radiographs may show degenerative changes in the atlantoaxial, zygapophyseal, and uncovertebral joints 46. However, radiography, MRI, and computed tomography (CT) are typically of limited value in the diagnosis of cervicogenic headache 42. An MRI is commonly ordered to help rule out Chiari malformations, nerve root pathology assessment, or even in the spinal cord pathology 47.
Cervicogenic headache ciagnostic criteria recommended by the International Classification of Headache Disorders (ICHD) 3rd edition 48:
- A) Any headache fulfilling criterion C
- B) Clinical and/or imaging evidence 1 of a disorder or lesion within the cervical spine or soft tissues of the neck, known to be able to cause headache 2
- C) Evidence of causation demonstrated by at least two of the following:
- headache has developed in temporal relation to the onset of the cervical disorder or appearance of the lesion
- headache has significantly improved or resolved in parallel with improvement in or resolution of the cervical disorder or lesion
- cervical range of motion is reduced and headache is made significantly worse by provocative manoeuvre
- headache is abolished following diagnostic blockade of a cervical structure or its nerve supply
- D) Not better accounted for by another International Classification of Headache Disorders-3 diagnosis 3;4;5.
Notes 48:
- Imaging findings in the upper cervical spine are common in patients without headache; they are suggestive but not firm evidence of causation.
- Tumors, fractures, infections and rheumatoid arthritis of the upper cervical spine have not been formally validated as causes of headache, but are accepted to fulfill criterion B in individual cases. Cervical spondylosis and osteochondritis may or may not be valid causes fulfilling criterion B, again depending on the individual case.
- When cervical myofascial pain is the cause, the headache should probably be coded under 2. Tension-type headache; however, awaiting further evidence, an alternative diagnosis of A11.2.5 Headache attributed to cervical myofascial pain is in the Appendix.
- Headache caused by upper cervical radiculopathy has been postulated and, considering the now well-understood convergence between upper cervical and trigeminal nociception, this is a logical cause of headache. Pending further evidence, this diagnosis is in the Appendix as A11.2.4 Headache (https://ichd-3.org/appendix/a11-headache-or-facial-pain-attributed-to-disorder-of-the-cranium-neck-eyes-ears-nose-sinuses-teeth-mouth-or-other-facial-or-cervical-structure/a11-2-headache-attributed-to-disorder-of-the-neck/a11-2-4-headache-attributed-to-upper-cervical-radiculopathy/) attributed to upper cervical radiculopathy.
- Features that tend to distinguish cervicogenic headache from 1. Migraine and 2. Tension-type headache include side-locked pain, provocation of typical headache by digital pressure on neck muscles and by head movement, and posterior-to-anterior radiation of pain. However, while these may be features of cervicogenic headache, they are not unique to it and they do not necessarily define causal relationships. Migrainous features such as nausea, vomiting and photo/phonophobia may be present with cervicogenic headache, although to a generally lesser degree than in 1. Migraine, and may differentiate some cases from 2. Tension-type headache.
A11.2.4 Headache attributed to upper cervical radiculopathy (https://ichd-3.org/appendix/a11-headache-or-facial-pain-attributed-to-disorder-of-the-cranium-neck-eyes-ears-nose-sinuses-teeth-mouth-or-other-facial-or-cervical-structure/a11-2-headache-attributed-to-disorder-of-the-neck/a11-2-4-headache-attributed-to-upper-cervical-radiculopathy/)
Diagnostic criteria:
- A) Head and/or neck pain fulfilling criterion C
- B) Clinical, electrodiagnostic or radiological evidence of a C2 or C3 radiculopathy
- C) Evidence of causation demonstrated by both of the following:
- at least two of the following:
- a) pain has developed in temporal relation to onset of the radiculopathy, or led to its discovery
- b) pain has significantly improved or significantly worsened in parallel with improvement in or worsening of the radiculopathy
- c) pain is temporarily abolished by local anaesthesia of the relevant nerve root
- headache is ipsilateral to the radiculopathy
- at least two of the following:
- D) Not better accounted for by another International Classification of Headache Disorders-3 diagnosis.
Comment:
Pain is usually posterior but may radiate to more anterior regions. Often there are lancinations of pain in one of the areas subserved by the upper cervical roots on one or both sides, generally in the occipital, retroauricular or upper posterior cervical regions.
Cervicogenic headache differential diagnosis
Primary headache
Primary headaches can be identified by their typical clinical manifestations 49.
- Tension-type headache has the following characteristics:
- bilateral;
- pressing or tightening (nonpulsating) pain;
- paroxysmal pain;
- not aggravated by routine physical activity;
- no nausea or vomiting;
- can be aggravated by compression of the frontal, temporal, masseter, pterygoid, sternocleidomastoid, splenius, and trapezius muscles.
- Migraine has the following characteristics:
- unilateral,
- pulsating pain,
- headache lasting 4–72 hours,
- aggravation by routine physical activity (e.g., walking or climbing stairs),
- accompanied by nausea/vomiting/photophobia/phonophobia,
- ipsilateral premonitory visual symptoms (e.g., flashing, darkness, lines, or blindness), or sensory symptoms (e.g., numbness) lasting >5 min,
- ergotamine or triptans can be effective, and
- alleviated by pregnancy.
Secondary headaches
- Posttraumatic headache can be diagnosed based on its clinical manifestation and MRI and CT findings.
- Vascular headache, including poststroke, hemangioma, and hypertensive headaches, can be diagnosed based on its clinical manifestation and MRI (including angiography) and CT (including CT or digital subtraction angiography) findings.
- Headache caused by high or low intracranial pressure. High intracranial pressure is usually caused by tumor or inflammation, which can result in a persistent, nonpulsatile, and severe headache with papilledema and emesis. Low intracranial pressure is usually caused by lumbar puncture, which can be relieved after lying down and aggravated by sitting in an upright posture.
- Referred headache from skull structures, such as eyes, ears, sinuses, and teeth (e.g., glaucoma, sinusitis, and periodontitis). Specialist examination can aid in the diagnosis, such as intraocular pressure determination, sinus CT, and dental examination.
- Somatoform disorders should also be considered. Physical and auxiliary examinations are normal in these patients. Repeated and changing physical symptoms are presented, and pain areas are not fixed. The patient may also have anxiety and depression.
Cervicogenic headache treatment
Physical therapy is considered the first line of treatment. Manipulative therapy and therapeutic exercise regimen are effective in treating a cervicogenic headache. According to a study by Jull and Richardson, 72% of patients had achieved a reduction of 50% or more in headache frequency at the 12-month follow-up, and 42% of patients reported 80% or higher relief of some sort. These manipulative maneuvers stimulate neural inhibitory systems at various levels in the spinal cord and activate descending inhibitory pathways 50.
Another option for treatment of a cervicogenic headache is interventional treatment, which will differ depending on the cause of a headache. For example, a lateral atlantoaxial joint intra-articular injection can be useful to diagnose and treat the condition when it has an osteoarthritis or post-traumatic cause. Another cause of a cervicogenic headache is arthritis of the C2-3 facet joint which is innervated by a superficial branch of the C3 nerve called the third occipital nerve. This is seen after whiplash injury from a motor accident. Injection into the facet joint will reduce pain, and third occipital nerve block will provide temporary cervicogenic headache pain relief while radiofrequency ablation can be used for long-term pain relief. Common treatments include blockade of the greater occipital nerve, the lesser occipital nerve, and the stellate ganglion.
There is some evidence that cervical epidural steroid injection has some benefits in treating pain in a cervicogenic headache. Steroids can work in this setting due to the theory that the pain continues sensitizing the cervical nerve roots and initiates a pain-producing loop involving nerve root and microvascular inflammation as well as mechanically-induced micro-injury.
Cervical epidural steroids injections with an interlaminar needle approach at C7-T1 or C6-7 epidural space is relatively safe compared to other interventional cervical procedures. According to He et al.’s study, steroids injection reduced the daily nonsteroidal anti-inflammatory drug (NSAID) usage at both 3 and 6 months.
Cervicogenic headache medication
Despite a lack of convincing clinical studies on effective medications for cervicogenic headache, pharmacotherapy remains among the best available treatments 51. Several types of medications are commonly used 52:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can be effective, including nonselective COX and selective COX-2 inhibitors.
- Muscle relaxants, particularly tizanidine, baclofen, and eperisone hydrochloride, that have central mechanisms of action can also provide analgesic effects in both the acute phase and for prevention. Tizanidine can be combined with NSAIDs because of its gastroprotective effect and good safety.
- Antiepileptic drugs and antidepressants can be used in patients with neuropathic pain. Common drugs for this purpose include gabapentin, pregabalin, amitriptyline, venlafaxine, and duloxetine.
Injection to the atlantoaxial and C2-C3 zygapophyseal joints and nerve block
Individualized injection therapy can be selected according to the pain’s location and characteristics. These procedures are associated with risks of structural damage from needle placement but can also result in the injection of local anesthetic into the vertebral artery, high-level epidural anesthesia, total spinal cord anesthesia, or injury of the spinal cord and nerve roots. Nonparticulate, water-soluble steroid hormones are recommended to prevent the embolism of steroid hormone particles.
Joint injection
- Atlantoaxial Joint Injection. This can benefit patients with suboccipital or occipital pain aggravated by cervical rotation 53 or pain due to inflammatory stimuli 54. Intraarticular injection can use a lateral or posterior approach and should be slow, with the volume not exceeding 1 ml. One study has shown that injection to the atlantoaxial joint was effective in 81.2% of cases. After 3 months’ follow-up, 20% of patients had pain relief exceeding 50% 55.
- C2-C3 Zygapophyseal Joint Injection. This injection can be considered for patients with upper neck pain spreading to the occipital region or pain that increases when the neck is rotated or back is stretched. During the procedure, the head can be rotated for a better field of vision. Again, the injection should be slow and should not exceed a total volume of 1 ml. However, the therapeutic efficacy of C2-C3 intra-articular injection remains controversial 56.
Nerve block
- Cervical Spinal Nerve Root Block. Selective nerve root injection could be used in patients with cervical spondylotic radiculopathy although the depth of the needle should be monitored to prevent complications. The effectiveness of this method is 70%, with 50% still reporting relief after 12 months 57.
- Third Occipital Nerve Block. This block can be used to diagnose cervicogenic headache and predict the efficacy of radiofrequency treatment.
- Occipital Nerve Block. This block can be used to diagnose and treat occipital pain 51. Clinically, occipital nerve injection can be repeatedly and intermittently used for symptomatic treatment. Dose for diagnostic injection should be limited to 2 ml; however, when it reaches 3–5 ml, the greater and small occipital nerves are completely blocked.
Minimally invasive interventional management
Radiofrequency therapy, including radiofrequency thermocoagulation and pulse radiofrequency, is minimally invasive interventional techniques. Nerve properties can be distinguished by monitoring the stimulation frequency and impedance. Interventional radiofrequency therapy can be considered if a diagnostic nerve block is effective 58.
Radiofrequency intervention is recommended for patients with intractable cervical headache from the C2-C3 zygapophyseal joint for which conservative treatment has failed and complete relief has been obtained from a diagnostic nerve block 59. The efficacy for cervicogenic headache of other origins needs to be confirmed. Pulse radiofrequency is a type of neuromodulation therapy that has shown satisfactory short-term efficacy, albeit with recurrence during long-term follow-up that requires repeated treatments [32]. The reason for poor performance of C2 ganglion pulse radiofrequency treatment in some patients may be occipital pain from the C1 and C3 spinal nerve branches through the superior cervical plexus. Percutaneous laser disc decompression is another effective minimally invasive procedure for patients with cervical disc herniation, protrusion, or disc degeneration who have neck and shoulder pain with nerve root symptoms. Also, plasma radiofrequency can be considered when other methods fail to achieve satisfactory results by reducing the volume of the nucleus pulposus, potentially improving symptoms.
Finally, ozone has strong anti-inflammatory and analgesic effects that can benefit patients in whom glucocorticoid use is contraindicated. Its efficacy can be further improved through combination with a nerve block. Clinical effectiveness of percutaneous radiofrequency ablation combined with ozone is superior to that of percutaneous radiofrequency ablation alone in the treatment of cervical disc herniation, providing better medium- and long-term outcomes. Percutaneous laser disc decompression, ozone therapy, and other techniques have shown some clinical efficacy.
Surgical procedures
Surgery is not usually recommended for cervicogenic headache, except when cervicogenic headache is refractory and does not respond to noninvasive treatment, and there is convincing evidence that cervicogenic headache is caused by pathological changes amenable to surgical treatment.
Surgery may be beneficial for three specific causes of cervicogenic headache as follows 60:
- C2 spinal nerve compression by vascular/ligamentous structures,
- Osteoarthritis of the lateral atlantoaxial joint, and
- Upper cervical intervertebral disc pathology.
Cervicogenic headache physical therapy
Physiotherapy is almost universally available and risk-free and has enormous benefits 61, such as reducing the frequency of cervicogenic headache and improving headaches in the long-term. In view of the noninvasive nature of physiotherapy, it is recommended that it be the first choice for patients with cervicogenic headache. Options include manipulation therapy (e.g., pulling, relaxation, and chiropractic), specific training therapy (e.g., static and dynamic stretching and training), and low-load endurance muscle exercise focusing on the neck and shoulder joints or the upper limbs (moderately strong evidence) 62. In the initial stages, the muscles are gently stretched and artificial neck traction is performed to make physical therapy easier for the patient. Next, strength training and aerobic exercise are gradually introduced according to the patient’s tolerance. High-velocity manipulation is not recommended because of the risk of interregional arterial dissection and stroke.
In spite of a growing body of evidence supporting cervical manipulation, further studies on this topic are needed to accurately assess the effectiveness of this technique for treating patients with cervicogenic headache 22. The findings of most of the included studies indicate manipulation or mobilization as promising interventions. However, the high heterogeneity in treatments, possibly due to the small number of studies included, suggests that the results should be interpreted cautiously. There is a lack of standardization in spinal manipulative therapy interventions and outcome measures in the literature. Further research is required to establish a strong evidence-based foundation for use of these interventions in cervicogenic headache patients 22.
References- Al Khalili Y, Jain S, Murphy PB. Cervicogenic Headache. [Updated 2019 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507862
- Page P. Cervicogenic headaches: an evidence-led approach to clinical management. Int J Sports Phys Ther. 2011;6(3):254–266. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3201065
- Drottning M, Staff PH, Sjaastad O. Cervicogenic headache (CEH) after whiplash injury. Cephalalgia (2002) 22(3):165–71. doi:10.1046/j.1468-2982.2002.00315.x
- Cooper G, Bailey B, Bogduk N. Cervical zygapophysial joint pain maps. Pain Med (2007) 8(4):344–53. doi:10.1111/j.1526-4637.2006.00201.x
- Zhou L, Hud-Shakoor Z, Hennessey C, Ashkenazi A. Upper cervical facet joint and spinal rami blocks for the treatment of cervicogenic headache. Headache (2010) 50(4):657–63. doi:10.1111/j.1526-4610.2010.01623.x
- Bogduk N. Cervicogenic headache: anatomic basis and pathophysiologic mechanisms. Curr Pain Headache Rep (2001) 5(4):382–6. doi:10.1007/s11916-001-0029-7
- Biondi DM. Cervicogenic headache: mechanisms, evaluation, and treatment strategies. J Am Osteopath Assoc (2000) 100(9 Suppl):S7–14.
- Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther (2006) 11(2):118–29. doi:10.1016/j.math.2005.04.007
- Sjaastad O, Bakketeig LS. Prevalence of cervicogenic headache: Vågå study of headache epidemiology. Acta Neurol Scand (2008) 117(3):173–80. doi:10.1111/j.1600-0404.2007.00962.x
- Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Pareja JA. Spinal manipulative therapy in the management of cervicogenic headache. Headache (2005) 45(9):1260–70. doi:10.1111/j.1526-4610.2005.00253_1.x
- Nilsson N. A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic headache. J Manip Physiol Ther (1995) 18(7):435–40.
- Racicki S, Gerwin S, DiClaudio S, Reinmann S, Donaldson M. Conservative physical therapy management for the treatment of cervicogenic headache: a systematic review. J Man Manip Ther (2013) 21(2):113–24. doi:10.1179/2042618612Y.0000000025
- Mayer C, Huber B, Peskind E. Traumatic brain injury, neuroinflammation, and post-traumatic headaches. Headache (2013) 53(9):1523–30. doi:10.1111/head.12173
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia (2013) 33(9):629–808. doi:10.1177/0333102413485658
- Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbaek E. “Cervicogenic” headache. An hypothesis. Cephalalgia (1983) 3(4):249–56. doi:10.1046/j.1468-2982.1983.0304249.x
- International Headache Society Classification Committee. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia (1988) 8(Suppl 7):1–96.
- Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia (2004) 24(Suppl1):9–160.
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache (1998) 38(6):442–5. doi:10.1046/j.1526-4610.1998.3806442.x
- Wu B, Yue L, Sun F, Gao S, Liang B, Tao T. The Feasibility and Efficacy of Ultrasound-Guided C2 Nerve Root Coblation for Cervicogenic Headache. Pain Med. 2019 Jun 01;20(6):1219-1226.
- Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (2002) 27(17):1835–43. doi:10.1097/01.BRS.0000025471.27251.BA
- Hall T, Briffa K, Hopper D. Clinical evaluation of cervicogenic headache: a clinical perspective. J Man Manip Ther (2008) 16(2):73–80. doi:10.1179/106698108790818422
- Mobilization and Manipulation of the Cervical Spine in Patients with Cervicogenic Headache: Any Scientific Evidence? Front. Neurol., 21 March 2016 https://doi.org/10.3389/fneur.2016.00040
- Dunning JR, Butts R, Mourad F, Young I, Fernandez-de-Las Peñas C, Hagins M, et al. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC Musculoskelet Disord (2016) 17(1):64. doi:10.1186/s12891-016-0912-3
- Youssef EF, Shanb A-SA. Mobilization versus massage therapy in the treatment of cervicogenic headache: a clinical study. J Back Musculoskelet Rehabil (2013) 26(1):17. doi:10.3233/BMR-2012-0344
- Haas M, Groupp E, Aickin M, Fairweather A, Ganger B, Attwood M, et al. Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manip Physiol Ther (2004) 27(9):547–53. doi:10.1016/j.jmpt.2004.10.007
- Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulativetherapy for cervicogenic headache. Spine 2002:27:1835–45.
- Biondi DM. Cervicogenic headache: a review of diagnostic and treatment strategies. J Am Osteopath Assoc (2005) 105(4 Suppl 2):16S–22S.
- Borusiak P, Biedermann H, Boßerhoff S, Opp J. Lack of efficacy of manual therapy in children and adolescents with suspected cervicogenic headache: results of a prospective, randomized, placebo-controlled, and blinded trial. Headache (2010) 50(2):224–30. doi:10.1111/j.1526-4610.2009.01550.x
- Johnson R. Anatomy of the cervical spine and its related structures. Torg JS, ed. Athletic Injuries to the Head, Neck, and Face. 2nd ed. St Louis, Mo: Mosby-Year Book; 1991. 371-83.
- Parke WW, Sherk HH. Normal adult anatomy. Sherk HH, Dunn EJ, Eismon FJ, et al, eds. The Cervical Spine. 2nd ed. Philadelphia, Pa: JB Lippincott Co; 1989. 11-32.
- McLain RF. Mechanoreceptor endings in human cervical facet joints. Spine. 1994 Mar 1. 19(5):495-501.
- Bogduk N, Twomey L. Clinical Anatomy of the Lumbar Spine. 2nd ed. New York, NY: Churchill Livingstone; 1991.
- Dreyfus P. The cervical spine: Non-surgical care Presented at: The Tom Landry Sports Medicine and Research Center; April 8, 1993; Dallas, Texas.
- Mendel T, Wink CS, Zimny ML. Neural elements in human cervical intervertebral discs. Spine. 1992 Feb. 17(2):132-5.
- Panjabi MM, Oxland TR, Parks EH. Quantitative anatomy of cervical spine ligaments. Part I. Upper cervical spine. J Spinal Disord. 1991 Sep. 4(3):270-6.
- Fielding JW, Cochran GB, Lawsing JF 3rd, Hohl M. Tears of the transverse ligament of the atlas. A clinical and biomechanical study. J Bone Joint Surg Am. 1974 Dec. 56(8):1683-91.
- Panjabi MM, Vasavada A, White A III. Cervical spine biomechanics. Semin Spine Surg. 1993. 5:10-6.
- Odonkor C. A., Tang T., Taftian D., Chhatre A. Bilateral intra-articular radiofrequency ablation for cervicogenic headache. Case Reports in Anesthesiology. 2017;2017:6. doi: 10.1155/2017/1483279.1483279
- Wang E., Wang D. Treatment of cervicogenic headache with cervical epidural steroid injection. Current Pain and Headache Reports. 2014;18(9):p. 442. doi: 10.1007/s11916-014-0442-3
- Dwyer A., Aprill C., Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine. 1990;15(6):453–457. doi: 10.1097/00007632-199006000-00004
- Bogduk N., Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. The Lancet Neurology. 2009;8(10):959–968. doi: 10.1016/s1474-4422(09)70209-1
- Xiao H, Peng B, Ma K, et al. The Chinese Association for the Study of Pain (CASP): Expert Consensus on the Cervicogenic Headache. Pain Res Manag. 2019;2019:9617280. Published 2019 Apr 1. doi:10.1155/2019/9617280 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6466854
- Sjaastad O., Fredriksen T. A., Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache: The Journal of Head and Face Pain. 1998;38(6):442–445. doi: 10.1046/j.1526-4610.1998.3806442.x
- Rubio-Ochoa J., Benítez-Martínez J., Lluch E., Santacruz-Zaragozá S., Gómez-Contreras P., Cook C. E. Physical examination tests for screening and diagnosis of cervicogenic headache: a systematic review. Manual Therapy. 2016;21:35–40. doi: 10.1016/j.math.2015.09.008
- Hall T., Briffa K., Hopper D., Robinson K. Reliability of manual examination and frequency of symptomatic cervical motion segment dysfunction in cervicogenic headache. Manual Therapy. 2010;15(6):542–546. doi: 10.1016/j.math.2010.06.002
- Frese A., Evers S. Biological markers of cervicogenic headache. Cephalalgia. 2008;28(1):21–23. doi: 10.1111/j.1468-2982.2008.01613.x
- Ko HC, Son BC. Chronic Unilateral Temporo-Occipital Headache Attributed to Unilateral C3 Radiculopathy. Asian J Neurosurg. 2018 Oct-Dec;13(4):1229-1232.
- Cervicogenic headache. https://ichd-3.org/11-headache-or-facial-pain-attributed-to-disorder-of-the-cranium-neck-eyes-ears-nose-sinuses-teeth-mouth-or-other-facial-or-cervical-structure/11-2-headache-attributed-to-disorder-of-the-neck/11-2-1-cervicogenic-headache
- Aguila M.-E. R., Rebbeck T., Mendoza K. G., De La Peña M.-G. L., Leaver A. M. Definitions and participant characteristics of frequent recurrent headache types in clinical trials: a systematic review. Cephalalgia. 2018;38(4):786–793. doi: 10.1177/0333102417706974
- Grimholt TK, Skogstad L, Hafstad GS, Vallersnes OM, Ekeberg Ø. [July 22, 2011 – psychological reactions in patients at the accident and emergency department in Oslo]. Tidsskr. Nor. Laegeforen. 2018 Jun 26;138(11).
- Biondi D. M. Cervicogenic headache: a review of diagnostic and treatment strategies. Journal of the American Osteopathic Association. 2005;105(2):16S–22S.
- Fernández-de-las-Peñas C., Cuadrado M. L. Therapeutic options for cervicogenic headache. Expert Review of Neurotherapeutics. 2014;14(1):39–49. doi: 10.1586/14737175.2014.863710
- Ehni G., Benner B. Occipital neuralgia and the C1-2 arthrosis syndrome. Journal of Neurosurgery. 1984;61(5):961–965. doi: 10.3171/jns.1984.61.5.0961
- Glémarec J., Guillot P., Laborie Y., Berthelot J. M., Prost A., Maugars Y. Intraarticular glucocorticosteroid injection into the lateral atlantoaxial joint under fluoroscopic control. A retrospective comparative study in patients with mechanical and inflammatory disorders. Joint Bone Spine. 2000;67(1):54–61.
- Narouze S. N., Casanova J., Mekhail N. The longitudinal effectiveness of lateral atlantoaxial intra-articular steroid injection in the treatment of cervicogenic headache. Pain Medicine. 2007;8(2):184–188. doi: 10.1111/j.1526-4637.2006.00247.x
- Zhou L., Hud-Shakoor Z., Hennessey C., Ashkenazi A. Upper cervical facet joint and spinal rami blocks for the treatment of cervicogenic headache. Headache: The Journal of Head and Face Pain. 2010;50(4):657–663. doi: 10.1111/j.1526-4610.2010.01623.x
- Persson L. C. G., Carlsson J. Y., Anderberg L. Headache in patients with cervical radiculopathy: a prospective study with selective nerve root blocks in 275 patients. European Spine Journal. 2007;16(7):953–959. doi: 10.1007/s00586-006-0268-8
- Hamer J. F., Purath T. A. Response of cervicogenic headaches and occipital neuralgia to radiofrequency ablation of the C2 dorsal root ganglion and/or third occipital nerve. Headache: The Journal of Head and Face Pain. 2014;54(3):500–510. doi: 10.1111/head.12295
- Nagar V. R., Birthi P., Grider J. S., Asopa A. Systematic review of radiofrequency ablation and pulsed radiofrequency for management of cervicogenic headache. Pain Physician. 2015;18(2):109–130.
- Schrot R. J., Mathew J. S., Li Y., Beckett L., Bae H. W., Kim K. D. Headache relief after anterior cervical discectomy: post hoc analysis of a randomized investigational device exemption trial. Journal of Neurosurgery: Spine. 2014;21(2):217–222. doi: 10.3171/2014.4.spine13669
- Hall T., Chan H. T., Christensen L., Odenthal B., Wells C., Robinson K. Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. Journal of Orthopaedic & Sports Physical Therapy. 2007;37(3):100–107. doi: 10.2519/jospt.2007.2379
- Sahrmann S., Azevedo D. C., Dillen L. V. Diagnosis and treatment of movement system impairment syndromes. Brazilian Journal of Physical Therapy. 2017;21(6):391–399. doi: 10.1016/j.bjpt.2017.08.001