What is choledochal cyst
Choledochal cyst also known as congenital cystic dilatation of the common bile duct 1, is a rare congenital anomaly usually caused by an abnormal union of the bile duct and the pancreatic duct (long common channel). Choledochal cysts are characterized by a dilation of the bile ducts that transport bile and can occur anywhere between the liver, where bile is produced, and the first part of the intestine (duodenum), where it empties. Choledochal cysts can occur in the bile ducts either inside or outside the liver. Most choledochal cysts (approximately two thirds) are diagnosed before your child reaches 10 years of age.
The liver produces bile to help digest food. When a child has a choledochal cyst, a swelling of that duct, bile may back up in the liver. This can cause liver problems or inflammation of the pancreas (pancreatitis) because it blocks the main duct from the pancreas gland to the intestine. Children with choledochal cysts have a higher rate of cancer of the bile duct in adulthood. Early treatment can reduce these risks.
Choledochal cysts are rare, with an incidence of 1 in 100,000–150,000 live births in Western countries and choledochal cysts occur more often in females than males (F:M ratio of 4:1). Choledochal cyst is more common in East Asian countries, especially Japan, though researchers do not know why.
Choledochal cysts are typically treated surgically, either by an open procedure or laparoscopic surgery.
If left untreated, complications of choledochal cysts may include:
- Infection
- Jaundice
- Pancreatitis
- Gallstones and sludge in the bile duct and gallbladder
- Gastrointestinal (GI) obstruction
- Cirrhosis
- Malignancy, or the development of bile duct cancer (cholangiocarcinoma)
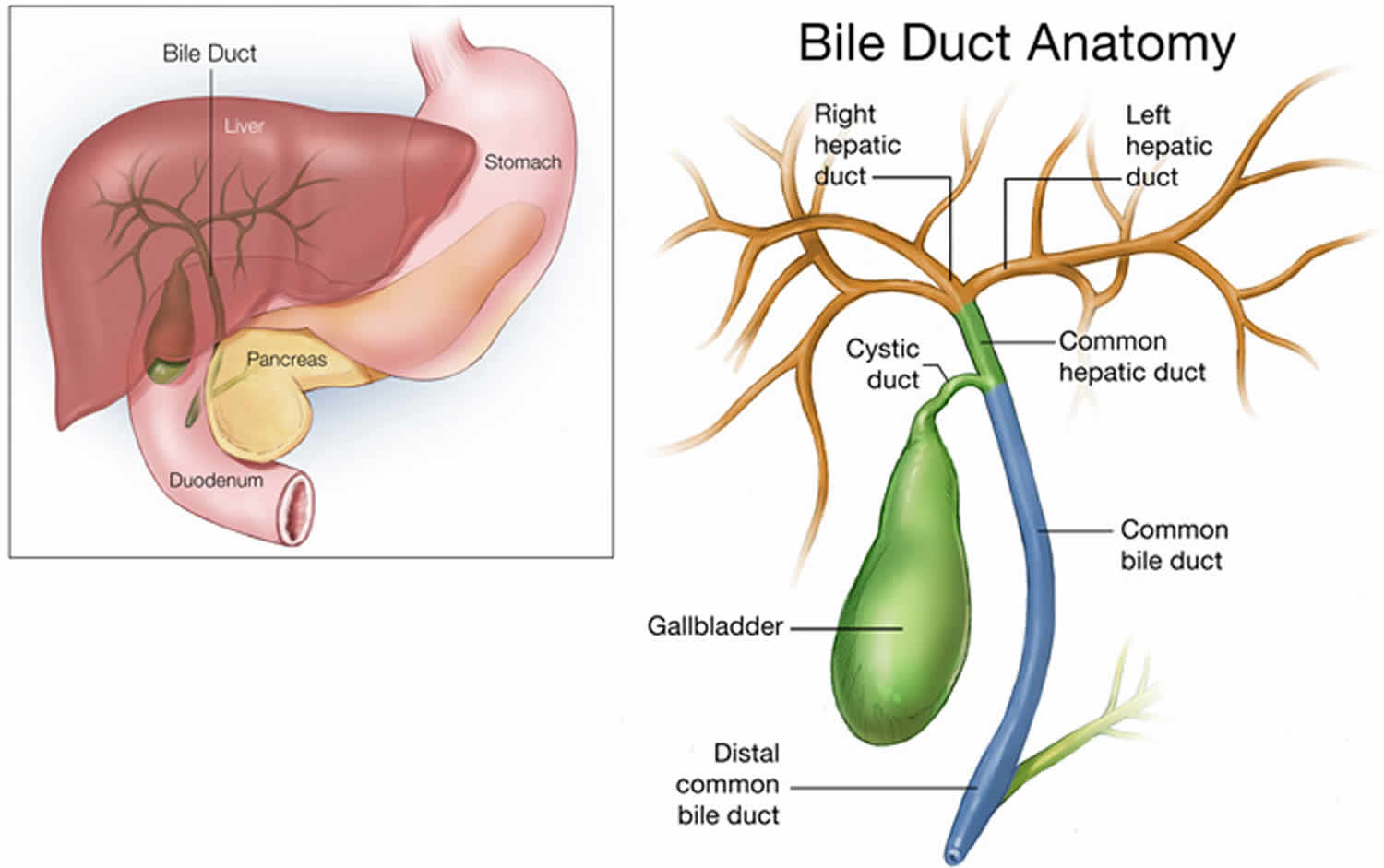
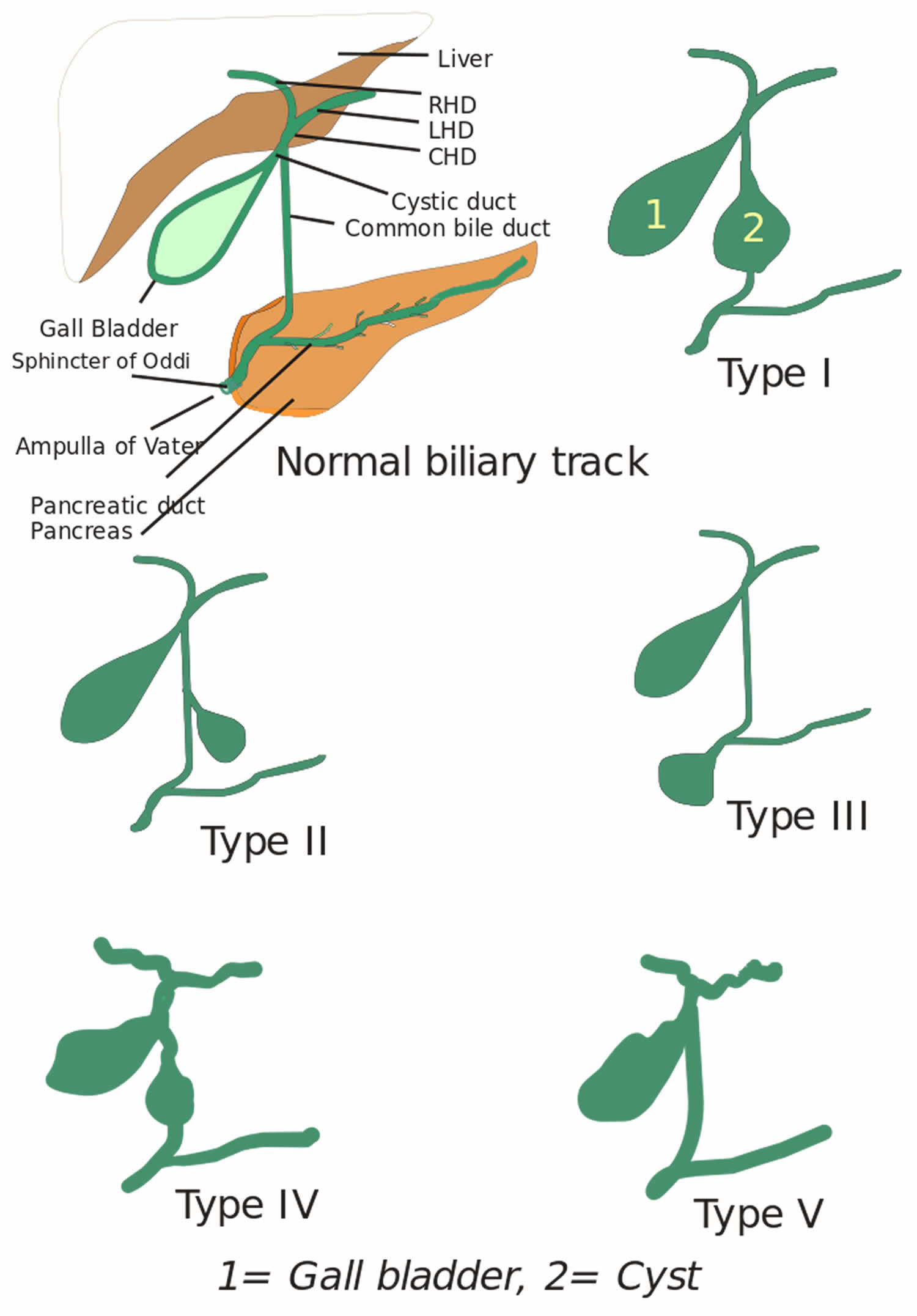
Figure 1. Bile duct anatomy
Choledochal cyst cancer risk
Choledochal cyst cancer risk lifetime incidence 10-15% 2.
Choledochal cyst types
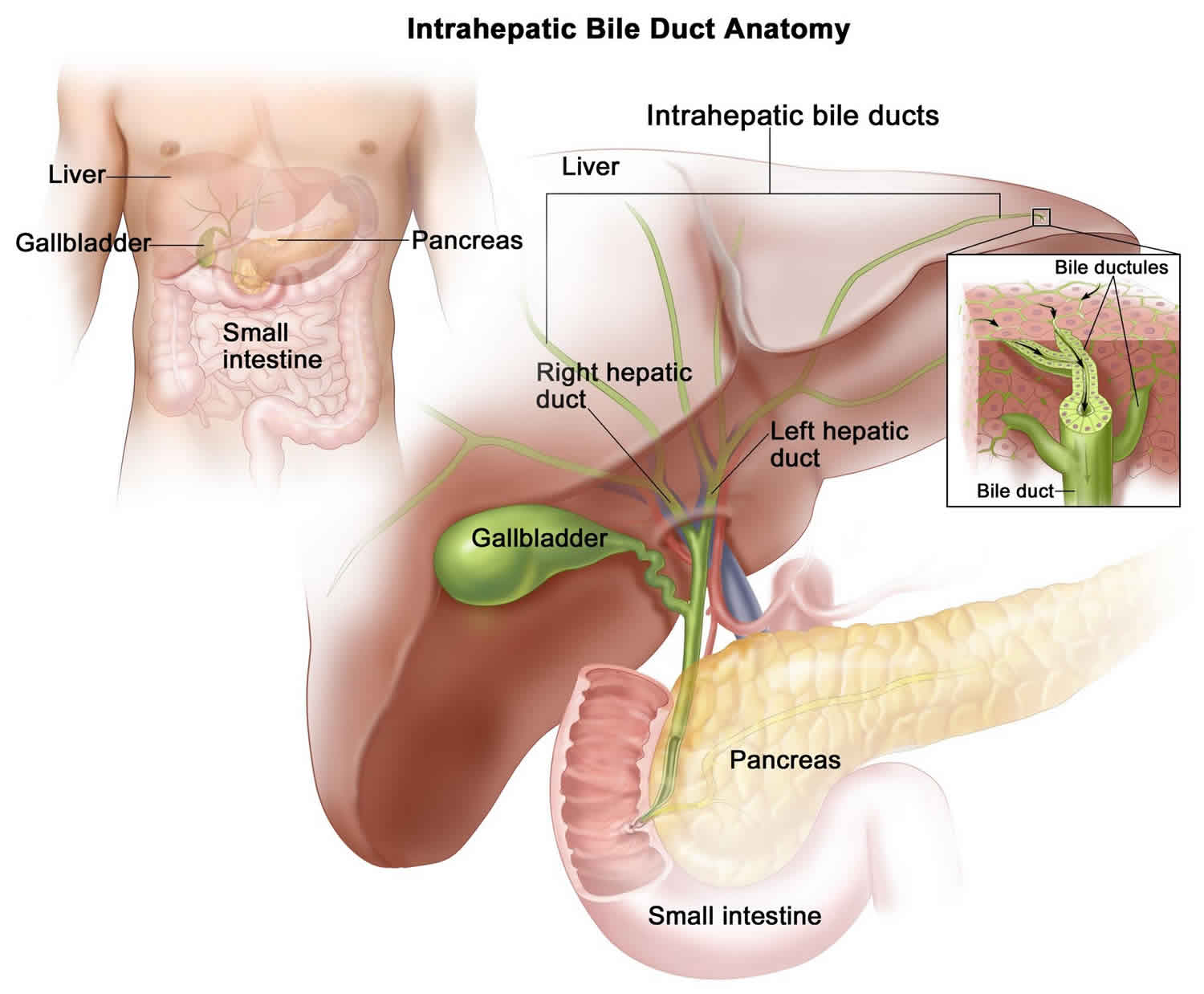
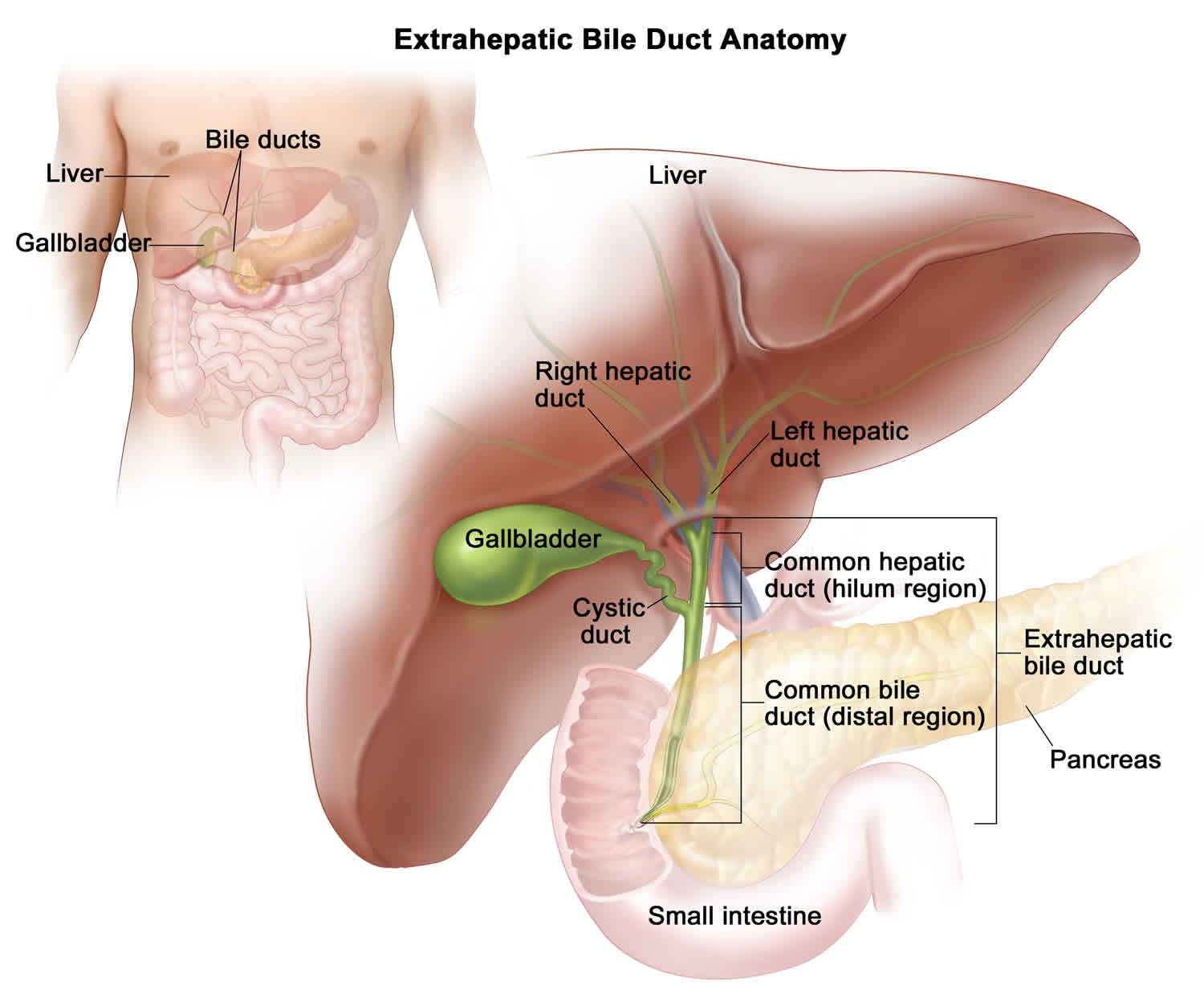
Choledochal cysts can form in the part of the bile duct inside of the liver (intrahepatic) or outside the liver (extrahepatic).
The Todani classification of bile duct cysts divides choledochal cysts into five groups. The Todani classification (1977) arose out of the earlier Alonso-Lej classification (1959). The Todani classification added type 5 (Caroli disease) to the earlier classification.
The Todani classification scheme has been called into question in the surgical literature, with claims that it may inaccurately link multiple distinct processes into a spuriously coherent grading scheme 3. Specifically, it is questioned whether types 2, 3, and 5 are pathophysiologically related to 1 and 4. Some also think the difference between 1 and 4 may be artificial.
Choledochal cysts are typically classified as one of several types based on where they appear:
- Type 1 choledochal cyst: Cyst of the extrahepatic (outside the liver) biliary duct. Most common type, accounting for 80-90% of all choledochal cysts (this type can present in utero) 4
- 1a: dilatation of extrahepatic bile duct (entire)
- 1b: dilatation of extrahepatic bile duct (focal segment)
- 1c: dilatation of the common bile duct portion of extrahepatic bile duct
- Type 2 choledochal cyst: Pouching or sac on the common bile duct (true diverticulum from extrahepatic bile duct).
- Type 3 choledochal cyst: Cyst within the wall of the duodenum or pancreas (choledochocoele).
- Type 4 choledochal cyst: A type 1 cyst with extension of the dilation into the intrahepatic (inside the liver) biliary ducts.
- 4a: cysts involving both intra and extrahepatic ducts
- 4b: multiple dilatations/cysts of extrahepatic ducts only
- Type 5 choledochal cyst: Multiple intrahepatic cystic dilations of the biliary ducts, also known as Caroli’s Disease.
Figure 2. Choledochal cyst types
 Type 1 choledochal cyst
Type 1 choledochal cyst
Type 1 choledochal cysts appear as a fusiform or cystic dilatation of the extrahepatic biliary system (common bile duct +/- common hepatic duct).
The designation “Type 1” arises from the Todani classification. Some believe that the division between type 1 and type 4 cysts is arbitrary 5.
Type 1 choledochal cyst
- account for 80-90% of all bile duct cysts
- characterized by fusiform dilation of the extrahepatic bile duct
- a subclassification has been proposed
- 1a: dilatation of extrahepatic bile duct (entire)
- 1b: dilatation of extrahepatic bile duct (focal segment)
- 1c: dilatation of the common bile duct portion of extrahepatic bile duct
Theorized to form as the result of reflux of pancreatic secretions into the bile duct via an anomalous pancreaticobiliary junction. Some believe them to arise from ductal plate anomalies.
Type 2 choledochal cyst
Also known as a bile duct diverticulum. Account for 3% of all bile duct cysts. Saccular outpouchings, representing a true diverticulum, arising from the supraduodenal extrahepatic bile duct or the intrahepatic bile ducts.
Type 3 choledochal cyst
Also known as a choledochocele:
- account for 5% of all bile duct cysts
- represent protrusion of a focally dilated, intramural segment of the distal common bile duct into the duodenum
Choledochoceles may be successfully managed with endoscopic sphincterotomy, surgical excision, or both, in symptomatic patients.
Type 4 choledochal cyst
Multiple communicating intra- and extrahepatic duct cysts:
- second most common type of bile duct cysts (10%)
- subdivided into subtypes:
- type 4a: fusiform dilation of the entire extrahepatic bile duct with extension of dilation of the intrahepatic bile ducts
- type 4b: multiple cystic dilations involving only the extrahepatic bile duct
Type 5 choledochal cyst
Also known as Caroli disease, which is a rare form of congenital biliary cystic disease manifested by cystic dilations of intrahepatic bile ducts. Association with benign renal tubular ectasia and other forms of renal cystic disease.
Choledochal cyst causes
The cause of choledochal cyst is uncertain, but a close association with the anomalous formation of the pancreaticobiliary ductal junction (an abnormality at the intersection between the bile duct and pancreatic duct) is reported in some subtypes 1. Due to this anomaly, there is a large common channel draining pancreatic and bile duct. This abnormal connection forces pancreatic juice to flow backward into the bile duct and cause cholangitis and bile duct wall destruction, which together with distal stenosis due to scarring result in the formation of a choledochal cyst.
Choledochal cyst symptoms
Although children are born with choledochal cysts, symptoms may appear in infancy or not for several years. The following symptoms may occur in infants or older children:
- Pain in the right upper belly
- Fever
- Jaundice
- Nausea and vomiting
- Abdominal mass
- Pancreatitis
The clinical signs and symptoms in older children and adults are variable. Children diagnosed with choledochal cysts after infancy typically present with intermittent biliary obstruction or recurrent bouts of pancreatitis with the following features:
- Biliary obstructive pattern: Palpable right upper quadrant mass and jaundice
- Primary manifestation of pancreatitis: May pose diagnostic difficulty; patients frequently have only intermittent attacks of colicky abdominal pain (elevated amylase and lipase concentrations lead to the proper diagnostic workup)
The classic triad in adults with choledochal cysts is abdominal pain, jaundice, and palpable right upper quadrant abdominal mass. However, this triad is found in only 10-20% of patients.
Adults may present with the following:
- Abdominal pain: Most common symptom; there may be vague epigastric or right upper quadrant pain
- Jaundice or cholangitis
- One or more severe complications (eg, hepatic abscesses, cirrhosis, portal hypertension, recurrent pancreatitis, cholelithiasis)
Choledochal cyst complications
The two most frequent complications of choledochal cysts are stone formation and malignancy. Complications include:
- stone formation: most common
- malignancy
- cholangiocarcinoma
- lifetime incidence 10-15% 2
- the cyst may rupture leading to bile peritonitis, most frequently seen in neonates 4
- pancreatitis
Choledochal cyst diagnosis
Choledochal cysts are most commonly diagnosed by ultrasound. In rare cases the cysts may be diagnosed before birth on a prenatal ultrasound. Other imaging tests that may be used in the diagnosis of a choledochal cyst include CT scans (computerized tomography scan), magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP).
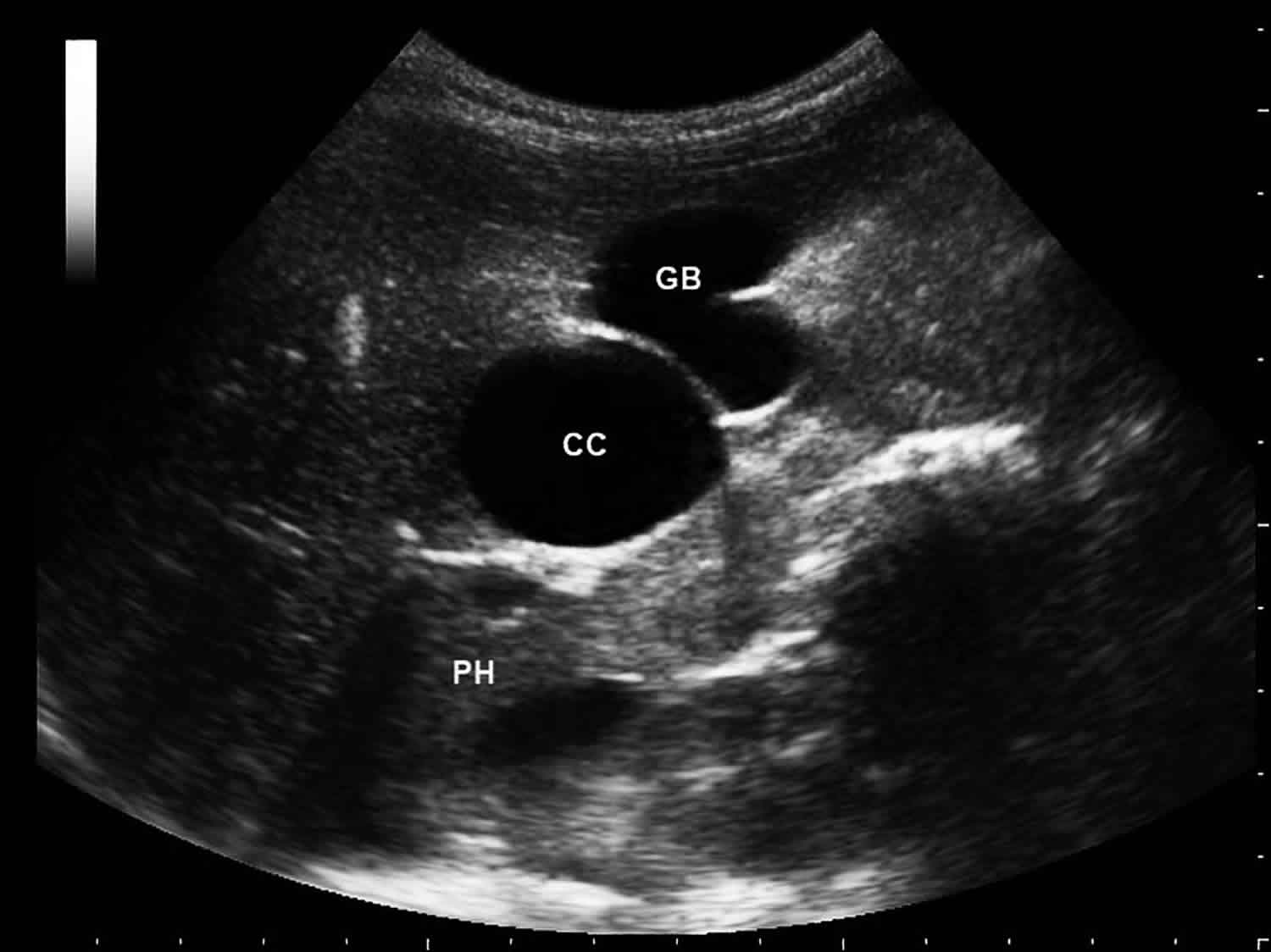
Figure 3. Choledochal cyst ultrasound
Footnote: Ultrasound study shows a cystic mass (CC) between pancreatic head (PH) and the gallbladder (GB). Smooth wall and homogeneous anechoic content was detected. The ultrasound study is compatible with dilatation of extrahepatic bile duct, that’s also known as a choledochal cyst. This is the type 1 of Todani classification of bile duct cysts.
Choledochal cyst treatment
Due to reported risk of malignancy in type 1 choledochal cysts ranging from 2.5-28%. Children with choledochal cysts are typically treated surgically to remove them, either by an open procedure or laparoscopically. Both procedures are performed in the operating room under general anesthesia. In both types of surgery for choledochal cysts, the cyst is removed and a reconstruction of the biliary system is frequently required using a section of intestine.
Treatment involves removing a lobe of the liver if the choledochal cysts are intrahepatic, or part of the duct outside of the liver if the cysts are located there and biliary reconstruction using a piece of intestine, usually requiring a hepaticojejunostomy. Rarely, reconstruction above the confluence of the left and right hepatic ducts is necessary.
Without surgery, children with choledochal cysts have an ongoing risk of other problems:
- biliary obstruction
- infection of the ducts
- jaundice
- cirrhosis
In adulthood, choledochal cysts can become cancerous if left untreated.
Choledochal cyst surgery
Laparoscopic excision of choledochal cyst
Laparoscopy, a minimally invasive surgical technique, may be used to remove your child’s choledochal cyst. The laparoscopic excision of a choledochal cyst begins with the surgeon making several small incisions in your child’s abdomen. In one incision, a small scope (or camera) is placed to allow the surgeon to see all of the abdominal organs. Small surgical tools are placed in 2 to 3 other incisions. The abdomen is filled with gas during the procedure to allow the surgeon to see easily.
The surgeon uses these tools to remove the cyst through a small incision inside your child’s belly button. The biliary system is then reconstructed using a section of the intestine called the duodenum (this procedure is called a hepaticoduodenostomy) or by a section of the intestine called the jejunum (called a Roux-en-Y hepaticojejunostomy). DERMABOND (skin glue) will cover the incisions.
In many cases children, can go home one to two days and return to their normal activities more quickly than children who have open surgery.
Other benefits of minimally invasive surgery include:
- very small scars, which are difficult to see after several months
- less pain after surgery
- usually a shorter hospital stay
Open excision of choledochal cyst
The surgeon will make an incision in your child’s right upper abdomen. The surgeon then removes the cyst and reconstructs the biliary system using either the duodenum (hepaticoduodenostomy) or a section of the intestine called the jejunum (Roux-en-Y hepaticojejunostomy). Your child’s incision will be closed with dissolvable stitches under the skin edges. A strip of tape or DERMABOND (skin glue) will cover the incision.
Follow-up care
After the operation, your child will go to the recovery room until he is awake and comfortable. He will then go to a hospital room. Your child will receive IV fluids until he is able to drink clear liquids without nausea or vomiting, and will slowly advance to a regular diet. We may give your child antibiotics through an IV to prevent infection. Pain medication will also go through the IV at first. When your child is eating, he can take pain medication by mouth.
Soon after surgery your child will need to get out of bed and begin to walk and move around. This helps to relieve gas pain that is common after surgery. It also helps your child heal faster. If the procedure was done laparoscopically, your child will go home in approximately 3 to 5 days. If your child had an open excision of a choledochal cyst, he will remain hospitalized a few days longer to ensure full recovery.
Your child’s surgeon and care team will discuss his recovery process with your family, including potential risks and complications to watch for:
- Bile leak
- Cholangitis
- Bleeding
- Strictures (narrowing of the bile duct)
- Wound infection
- Intrahepatic biliary stone formation
While choledochal cyst removal will reduce the risk of bile duct cancer (cholangiocarcinoma), your child will still be at higher risk of developing cancer in the remaining bile ducts inside the liver compared to the general population. There is also risk of narrowing in the reconstructed bile duct. Continued yearly follow up with a gastroenterologist or your pediatric surgeon is recommended to monitor for these complications. Your child may require ongoing blood work and imaging at regular intervals.
Choledochal cyst prognosis
The prognosis after excision of a choledochal cyst is usually excellent, but it is influenced by several factors, including patient age, cyst type, histologic features, and site 6. Moreover, patients need lifelong follow-up because of the increased risk of cholangiocarcinoma and gallbladder carcinoma, even after complete excision of the cyst. In adults, there appears to be a 6-30% risk of malignancy associated with choledochal cyst 6.
Morbidity/mortality
The morbidities associated with choledochal cysts depend on the age of the patient at the time of presentation. Infants and children may develop pancreatitis, cholangitis, and histologic evidence of hepatocellular damage. Adults in whom subclinical ductal inflammation and biliary stasis may have been present for years may present with one or more severe complications, such as hepatic abscesses, cirrhosis, portal hypertension, recurrent pancreatitis, cholangitis, and cholelithiasis.
Cholangiocarcinoma is the most feared complication of choledochal cysts, with a reported incidence of 9-28%. Wu and colleagues 7 exposed cells from a cholangiocarcinoma cell line to bile from patients with choledochal cysts and from controls with structurally normal biliary systems. The bile from the patients with choledochal cysts produced significantly more mitogenic activity in the cancer cell line than the bile from the controls.
References- Fan F, Xu DP, Xiong ZX, et al. Clinical significance of intrapancreatic choledochal cyst excision in surgical management of type I choledochal cyst. J Int Med Res. 2018;46(3):1221–1229. doi:10.1177/0300060517728598 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5972235
- Chung YE, Kim MJ, Park YN et-al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics. 29 (3): 683-700. doi:10.1148/rg.293085729
- Martin RF. Biliary cysts: a review and simplified classification scheme. Surg. Clin. North Am. 2014;94 (2): 219-32. doi:10.1016/j.suc.2014.01.011
- Imaging of the choledochal cyst. O H Kim, H J Chung, and B G Choi. RadioGraphics 1995 15:1, 69-88 https://pubs.rsna.org/doi/pdf/10.1148/radiographics.15.1.7899614
- 7. Visser BC, Suh I, Way LW et-al. Congenital choledochal cysts in adults. Arch Surg. 2004;139 (8): 855-60. doi:10.1001/archsurg.139.8.855
- Madadi-Sanjani O, Wirth TC, Kuebler JF, Petersen C, Ure BM. Choledochal cyst and malignancy: a plea for lifelong follow-up. Eur J Pediatr Surg. 2019 Apr. 29(2):143-149.
- Wu GS, Zou SQ, Luo XW, Wu JH, Liu ZR. Proliferative activity of bile from congenital choledochal cyst patients. World J Gastroenterol. 2003 Jan. 9(1):184-7.