Chronic cough
Chronic cough is a cough that lasts eight weeks or longer in adults, or four weeks in children 1. A chronic cough is more than just an annoyance. A chronic cough can interrupt your sleep and leave you feeling exhausted. Severe cases of chronic cough can cause vomiting, lightheadedness and even rib fractures.
While it can sometimes be difficult to pinpoint the problem that’s triggering a chronic cough, the most common causes are tobacco use (smoking), upper airway cough syndrome (postnasal drip syndrome), asthma, nonasthmatic eosinophilic bronchitis and gastroesophageal reflux disease/laryngopharyngeal reflux disease 2. Other potential causes of chronic cough include angiotensin-converting enzyme inhibitor (ACE inhibitor) use, environmental triggers, chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea. Fortunately, chronic cough typically disappears once the underlying problem is treated. See your doctor if you have a cough that lingers for weeks, especially one that brings up sputum or blood, disturbs your sleep, or affects school or work.
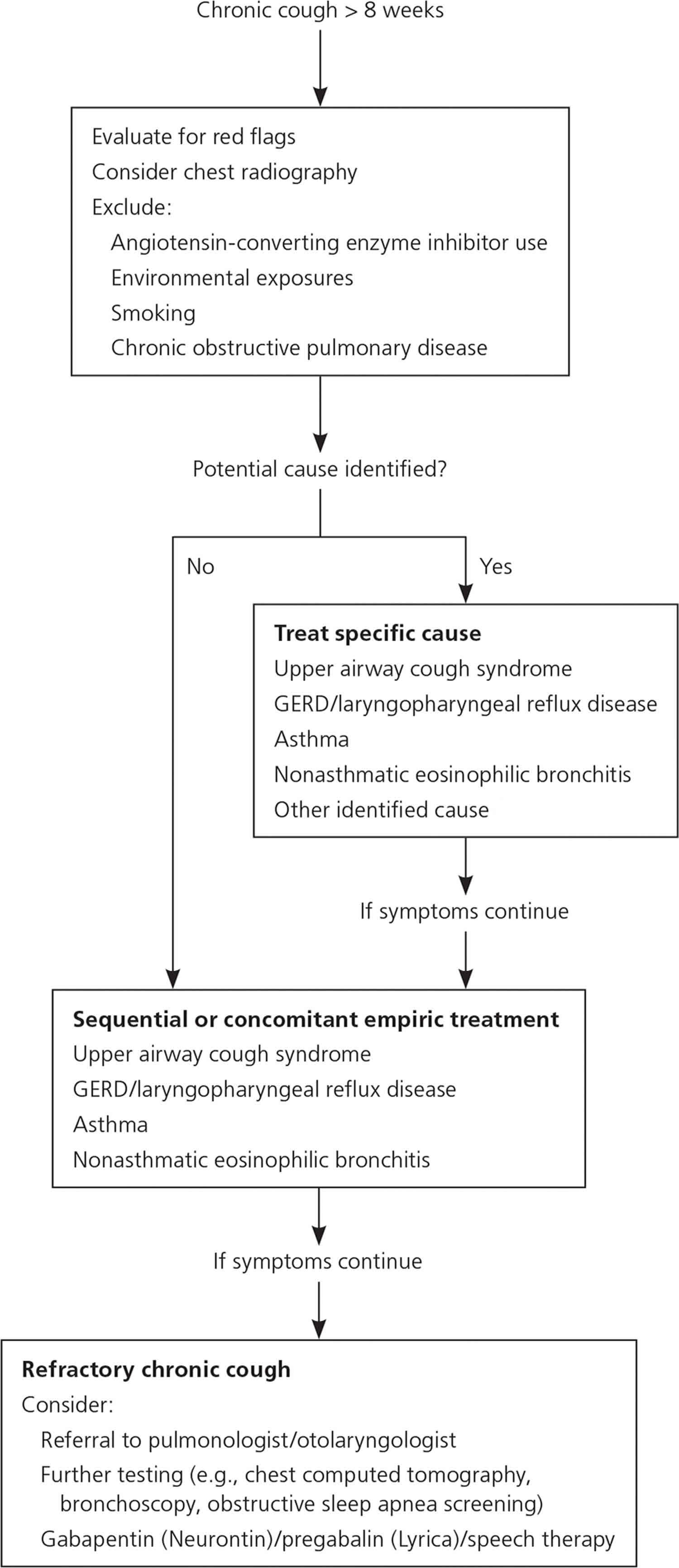
Patients should be evaluated clinically (with spirometry, if indicated), and empiric treatment should be initiated. Chest radiography can rule out concerning infectious, inflammatory, and malignant thoracic conditions. Patients with refractory chronic cough may warrant referral to a pulmonologist or otolaryngologist in addition to a trial of gabapentin, pregabalin, and/or speech therapy. In children six to 14 years of age, chronic cough is most commonly caused by asthma, protracted bacterial bronchitis, and postnasal drip (upper airway cough syndrome). Evaluation should focus initially on these causes, with targeted treatment and monitoring for resolution.
Cough caused by the common cold typically lasts one to three weeks and is self-limited. However, persistent chronic cough can be the first sign of a more serious disease process. According to the Centers for Disease Control and Prevention (CDC), cough of undifferentiated duration is the most common presenting symptom in patients of all ages in the primary care ambulatory setting 3. In adults, chronic cough is defined as symptoms lasting longer than eight weeks, whereas acute cough lasts less than three weeks and subacute cough from three to eight weeks 4. When persistent and excessive, cough can seriously impair quality of life and lead to vomiting, muscle pain, rib fractures, urinary incontinence, tiredness, syncope, and depression. Chronic cough also has psychosocial effects, such as embarrassment and negative impact on social interactions 5.
Chronic cough causes
An occasional cough is normal —coughing is how your body clears foreign objects and mucus from your lungs and breathing tubes. A cough that lasts a long time can be a sign of a health problem. In many cases, more than one cause is involved. A chronic cough is a cough that lasts longer than eight weeks or longer in adults, or four weeks in children.
The following causes, alone or in combination, are responsible for the majority of cases of chronic cough:
- Postnasal drip syndrome also called upper airway cough syndrome. The term upper airway cough syndrome previously referred to as postnasal drip syndrome, was coined in the 2006 American College of Chest Physicians guideline 6 in recognition of the fact that multiple causes, including chronic rhinosinusitis, allergic rhinitis, and nonallergic rhinitis, were difficult to differentiate solely by clinical presentation. Upper airway cough syndrome is the most common cause of chronic cough 7. When your nose or sinuses produce extra mucus, it can drip down the back of your throat and trigger your cough reflex. Rhinorrhea, nasal stuffiness, sneezing, itching, and postnasal drainage suggest the diagnosis, but their absence does not rule out upper airway cough syndrome 8. Physical findings may include swollen turbinates and direct visualization of postnasal drainage and cobblestoning of the posterior pharynx. If a specific cause is identified, therapy should be started; otherwise, initial treatment includes a decongestant combined with a first-generation antihistamine. Intranasal corticosteroids, saline nasal rinses, nasal anticholinergics, and antihistamines are also reasonable options 7. Clinical improvement should occur within days to weeks, and up to two months. If chronic rhinosinusitis is suspected, sinus computed tomography or flexible nasolaryngoscopy should be performed. Sinus radiography is not recommended because of limited sensitivity 9.
- Asthma. An asthma-related cough may come and go with the seasons, appear after an upper respiratory tract infection, or become worse when you’re exposed to cold air or certain chemicals or fragrances. In one type of asthma (cough-variant asthma), a cough is the main symptom. The prevalence of asthma in patients with chronic cough ranges from 24% to 29% 10. Asthma should be suspected in patients with shortness of breath, wheezing, and chest tightness, but cough can be the only manifestation in cough variant asthma. If the physical examination and spirometry findings are nondiagnostic, bronchial challenge testing (methacholine inhalation test) should be considered 11. Resolution of the cough after asthma treatment is also diagnostic. After counseling the patient about potential triggers, treatment usually includes an inhaled bronchodilator and high-dose inhaled corticosteroid. A leukotriene receptor antagonist (e.g., montelukast [Singulair]) can also be useful. Symptoms should resolve within one to two weeks after starting treatment 12. For severe or refractory cough, a five- to 10-day course of prednisone, 40 to 60 mg, or equivalent oral corticosteroid can be considered if asthma is strongly suspected 6.
- Gastroesophageal reflux disease (GERD). In this common condition, stomach acid flows back into the tube that connects your stomach and throat (esophagus). The constant irritation can lead to chronic coughing. The coughing, in turn, worsens GERD — a vicious cycle.
Infections. A cough can linger long after other symptoms of pneumonia, flu, a cold or other infection of the upper respiratory tract have gone away. A common but under-recognized cause of a chronic cough in adults is pertussis, also known as whooping cough. Chronic cough can also occur with fungal infections of the lung, tuberculosis (TB) infection or lung infection with nontuberculous mycobacterial organisms. - Chronic obstructive pulmonary disease (COPD). COPD, a chronic inflammatory lung disease that causes obstructed airflow from the lungs, includes chronic bronchitis and emphysema. Chronic bronchitis can cause a cough that brings up colored sputum. Emphysema causes shortness of breath and damages the air sacs in the lungs (alveoli). Most people with COPD are current or former smokers. COPD commonly causes chronic cough, but most patients presenting with chronic cough do not have undiagnosed COPD. Signs and symptoms suggestive of asthma also occur in persons with COPD. Spirometry is diagnostic, and purulent sputum production may also be present. Treatment includes an inhaled bronchodilator, inhaled anticholinergic, inhaled corticosteroid, and a one- to two-week course of oral corticosteroids (with or without antibiotics) 13.
- Blood pressure drugs. Angiotensin-converting enzyme (ACE) inhibitors, which are commonly prescribed for high blood pressure and heart failure, are known to cause chronic cough in some people.
- ACE inhibitor–related cough has been reported in 5% to 35% of patients and is more common in women 14. It may start within hours to months of the first dose. When the medication is discontinued, resolution of the cough should occur within one week to three months; this is the only way to determine if the ACE inhibitor is causing the cough. Angiotensin receptor blockers (ARBs) are a good alternative to ACE inhibitors. However, if the patient has a strong indication, restarting the ACE inhibitor may be attempted; in some patients, the cough will not recur 14. When considering ACE inhibitors as the cause of chronic cough, other common causes should also be investigated.
Less commonly, chronic cough may be caused by:
- Aspiration (food in adults; foreign bodies in children)
- Bronchiectasis (damaged, dilated airways)
- Bronchiolitis (inflammation of the very small airways of the lung)
- Cystic fibrosis
- Gastroesophageal reflux disease (GERD) / laryngopharyngeal reflux disease (stomach acid flows up into the throat)
- The prevalence of GERD and laryngopharyngeal reflux disease as causative factors in chronic cough varies from 0% to 73% 15. Studies have shown an association between GERD and chronic cough, but the pathophysiology is complex and treatment is controversial 16. Associated manifestations such as heartburn, regurgitation, sour taste, hoarseness, and globus sensation are clinical clues. Although several uncontrolled studies have shown improvement of chronic cough with antacid treatment, more recent randomized controlled trials have shown no differences between proton pump inhibitors and placebo 17. Although there is poor evidence that proton pump inhibitors are universally beneficial for GERD-induced chronic cough 18, consensus guidelines recommend empiric therapy for at least eight weeks in conjunction with lifestyle changes such as dietary changes and weight loss 19. The addition of a histamine H2 receptor antagonist and/or baclofen (Lioresal, 20 mg per day) may be helpful 20. Surgery can be considered in patients with GERD-associated chronic cough who have abnormal esophageal acid exposure (as proven by pH testing) if normal peristalsis is confirmed on manometry 19.
- Lung cancer
- Nonasthmatic eosinophilic bronchitis (airway inflammation not caused by asthma)
- Nonasthmatic eosinophilic bronchitis is characterized by chronic cough in patients with no symptoms or objective evidence of variable airflow obstruction, normal airway responsiveness on a methacholine inhalation test, and sputum eosinophilia 21. Sputum evaluation is not typically performed in the primary care setting, but it can be induced by saline nebulization or obtained by bron-choalveolar lavage in a subspecialist’s office. The prevalence is unclear, but studies assessing airway inflammation in patients with chronic cough showed that this condition accounts for 10% to 30% of cases referred for subspecialist investigation 22. It does not respond to inhaled bronchodilators, but should respond to inhaled corticosteroids. Avoidance strategies should be recommended when the inflammation is due to occupational exposure or inhaled allergens. Oral corticosteroids are rarely needed but can be considered if high-dose inhaled corticosteroids are ineffective 11.
- Sarcoidosis (collections of inflammatory cells in different parts of your body, most commonly the lungs)
- Idiopathic pulmonary fibrosis (chronic scarring of the lungs due to an unknown cause)
- Cough hypersensitivity syndrome
- Cough hypersensitivity syndrome is defined as “troublesome coughing triggered by a low level of thermal, mechanical or chemical exposure” 23. Cough hypersensitivity syndrome is characterized by enhancement of the cough reflex through sensitization of afferent neuronal pathways of a cough, both at the peripheral and central levels. Patients with cough hypersensitivity syndrome develop a cough in an exaggerated response to stimuli that would not otherwise elicit cough. It is thought that this nerve hypersensitivity is a result of various recurrent triggers, such as upper respiratory tract infection (URTI) or allergic rhinitis. A chronic cough is seen with upper airway cough syndrome, asthma, and reflux may be induced by the development of cough hypersensitivity. Pharyngeal and/or laryngeal sensations (irritation, tickle, tightness, throat clearing), which are frequently associated with upper airway cough syndrome and reflux-induced cough, may represent a sensory neuronal dysfunction of vagal afferents in the upper airways and a phenotype of cough hypersensitivity syndrome. Symptoms such as dysphonia, dysphagia, dyspnea, and abnormalities of vocal fold motion on laryngoscopy may also be present along with a cough as part of the pharyngeal/laryngeal nerve dysfunction seen with cough hypersensitivity syndrome.
Chronic cough causes in Adults
Adults
Most common 24
- Angiotensin-converting enzyme inhibitor (ACE inhibitor) use
- Asthma
- Environmental triggers
- Gastroesophageal/laryngopharyngeal reflux disease
- Nonasthmatic eosinophilic bronchitis
- Tobacco use
- Upper airway cough syndrome (postnasal drip syndrome)
Less common
- Bronchiectasis
- Chronic obstructive pulmonary disease (COPD)
- Obstructive sleep apnea
- A link between obstructive sleep apnea and chronic cough has been investigated. Treatment with continuous positive airway pressure may improve chronic cough by decreasing gastroesophageal reflux disease (GERD); therefore, evaluation for obstructive sleep apnea should be considered 25.
- Pertussis
- Postinfectious bronchospasm
Least common
- Arteriovenous malformation
- Bronchiolitis
- Bronchogenic carcinoma
- Chronic aspiration
- Chronic interstitial lung disease
- Irritation of external auditory canal
- Persistent pneumonia
- Psychogenic cough
- Sarcoidosis
- Tuberculosis
Chronic cough causes in Children
Children
Most common 24:
- Asthma
- Protracted bacterial bronchitis
- Upper airway cough syndrome (in children older than six years)
Less common
- Environmental triggers
- Foreign body (in younger children)
- Gastroesophageal reflux disease (GERD)
- Pertussis
- Postinfectious bronchospasm
Least common
- Chronic aspiration
- Congenital abnormality
- Cystic fibrosis
- Immunodeficiency
- Primary ciliary dyskinesia
- Psychogenic cough
- Tourette syndrome/tic
Risk factors for chronic cough
Being a current or former smoker is one of the leading risk factors for chronic cough. Frequent exposure to secondhand smoke also can lead to coughing and lung damage.
Chronic cough symptoms
A chronic cough can occur with other signs and symptoms, which may include:
- A runny or stuffy nose
- A feeling of liquid running down the back of your throat (postnasal drip)
- Frequent throat clearing and sore throat
- Hoarseness
- Wheezing and shortness of breath
- Heartburn or a sour taste in your mouth
- In rare cases, coughing up blood
Table 1. Abnormalities that suggest specific cause of cough
| Abnormality | Suggested cause |
|---|---|
Auscultatory findings | Wheeze: intrathoracic airway lesions (e.g., asthma, tracheomalacia) |
Crepitations: airway lesions (from secretions) or parenchymal disease (e.g., interstitial disease) | |
Cardiac abnormalities | Associated airway abnormalities, cardiac failure |
Chest pain | Arrhythmia, asthma |
Chest wall deformity | Pulmonary airway or parenchymal disease |
Daily moist or productive cough | Suppurative lung disease |
Digital clubbing | Suppurative lung disease |
Dyspnea or tachypnea | Pulmonary airway or parenchymal disease |
Exertional dyspnea | Pulmonary airway or parenchymal disease |
Failure to thrive | Serious systemic illness (including pulmonary illness, such as cystic fibrosis) |
Feeding difficulties | Aspiration, serious systemic illness (including pulmonary illness) |
Hemoptysis | Suppurative lung disease, vascular abnormalities |
Hypoxia/cyanosis | Pulmonary airway or parenchymal disease, cardiac disease |
Immunodeficiency | Atypical infection, suppurative lung disease |
Neurodevelopmental abnormality | Aspiration lung disease |
Recurrent pneumonia | Atypical infection, congenital lung abnormality, immunodeficiency, suppurative lung disease, tracheoesophageal fistula |
Chronic cough complications
Having a continuous cough can be exhausting. Coughing can cause a variety of problems, including:
- Sleep disruption
- Headache
- Dizziness
- Vomiting
- Excessive sweating
- Loss of bladder control (urinary incontinence)
- Fractured ribs
- Passing out (syncope)
Chronic cough diagnosis
Your doctor will ask about your medical history and perform a physical exam. A thorough medical history and physical exam can provide important clues about a chronic cough. Your doctor may also order tests to look for the cause of your chronic cough.
However, many doctors opt to start treatment for one of the common causes of chronic cough rather than ordering expensive tests. If the treatment doesn’t work, however, you may undergo testing for less common causes.
Figure 1. Chronic cough diagnostic algorithm for adults
Abbreviation: GERD = gastroesophageal reflux disease.
[Source 27 ]Imaging tests
- X-rays. Although a routine chest X-ray won’t reveal the most common reasons for a cough — postnasal drip, acid reflux or asthma — it may be used to check for lung cancer, pneumonia and other lung diseases. An X-ray of your sinuses may reveal evidence of a sinus infection.
- Computerized tomography (CT) scans. CT scans also may be used to check your lungs for conditions that may produce chronic cough or your sinus cavities for pockets of infection.
Lung function tests
These simple, noninvasive tests, such as spirometry, are used to diagnose asthma and COPD. They measure how much air your lungs can hold and how fast you can exhale.
Your doctor may request an asthma challenge test, which checks how well you can breathe before and after inhaling the drug methacholine (Provocholine).
Lab tests
If the mucus that you cough up is colored, your doctor may want to test a sample of it for bacteria.
Scope tests
If your doctor isn’t able to find an explanation for your cough, special scope tests may be considered to look for possible causes. These tests may include:
- Bronchoscopy. Using a thin, flexible tube equipped with a light and camera (bronchoscope), your doctor can look at your lungs and air passages. A biopsy can also be taken from the inside lining of your airway (mucosa) to look for abnormalities.
- Rhinoscopy. Using a fiberoptic scope (rhinoscope), your doctor can view your nasal passageways, sinuses and upper airway.
Children
A chest X-ray and spirometry, at a minimum, are typically ordered to find the cause of a chronic cough in children.
Chronic cough treatment
Determining the cause of chronic cough is crucial to effective treatment. In many cases, more than one underlying condition may be causing your chronic cough.
If you are currently smoking, your doctor will discuss with you your readiness to quit and provide assistance to achieve this goal.
If you’re taking an ACE inhibitor medication, your doctor may switch you to another medicine that doesn’t have cough as a side effect.
Patients with unexplained chronic cough after evaluation and treatment of common causes should be referred to a pulmonologist or otolaryngologist 28. Neuromodulators have shown some benefit in randomized trials based on the hypothesis that refractory chronic cough may be due to hypersensitivity of the cough reflex caused by peripheral (afferent limb of the cough reflex) and central mechanisms (central sensitization) 29. Therapies included gabapentin (Neurontin, 1,800 mg per day), which improved symptoms within four weeks; pregabalin (Lyrica, 300 mg per day) in conjunction with speech therapy, which showed greater improvement vs. placebo with speech therapy; and speech and language therapy alone 30.
Medications used to treat chronic cough may include:
- Antihistamines, corticosteroids and decongestants. These drugs are standard treatment for allergies and postnasal drip.
- Inhaled asthma drugs. The most effective treatments for asthma-related cough are corticosteroids and bronchodilators, which reduce inflammation and open up your airways.
- Antibiotics. If a bacterial, fungal or mycobacterial infection is causing your chronic cough, your doctor may prescribe medications to address the infection.
- Acid blockers. When lifestyle changes don’t take care of acid reflux, you may be treated with medications that block acid production. Some people need surgery to resolve the problem.
Cough suppressants
During the time your doctor is determining the reason for your cough and beginning treatment, your doctor may also prescribe a cough suppressant to try to speed your symptom relief.
Over-the-counter cough and cold medicines are intended to treat the symptoms of coughs and colds, not the underlying disease. Research suggests that these medicines haven’t been proved to work any better than inactive medicine (placebo). More important, these medications have potentially serious side effects, including fatal overdoses in children younger than 2 years old.
Don’t use over-the-counter medicines, except for fever reducers and pain relievers, to treat coughs and colds in children younger than 6 years old. Also, consider avoiding use of these medicines for children younger than 12 years old.
Home remedies
Follow the plan your doctor gives you for treating the cause of your cough. In the meantime, you can also try these tips to ease your cough:
- Drink fluids. Liquid helps thin the mucus in your throat. Warm liquids, such as broth, tea or juice, can soothe your throat.
- Suck on cough drops or hard candies. They may ease a dry cough and soothe an irritated throat.
- Consider taking honey. A teaspoon of honey may help loosen a cough. Don’t give honey to children younger than 1 year old because honey can contain bacteria harmful to infants.
- Moisturize the air. Use a cool-mist humidifier or take a steamy shower.
- Avoid tobacco smoke. Smoking or breathing secondhand smoke irritates your lungs and can worsen coughs caused by other factors. If you smoke, talk with your doctor about programs and products that can help you quit.
Chronic cough in children treatment
Chronic cough in children younger than 15 years is defined as cough lasting more than four weeks 31. Chest radiography and spirometry should be considered initially in age-appropriate patients 31. A watch-wait-review approach consisting of parental reassurance and observation for one to two weeks may be used in patients with a nonspecific cough 32.
The most common causes of chronic cough in children six to 14 years of age are asthma, protracted bacterial bronchitis, and upper airway cough syndrome (postnasal drip syndrome) 33. Protracted bacterial bronchitis is characterized by isolated chronic cough, wet/moist cough, resolution of cough with antibiotic treatment, and absence of findings suggestive of an alternative cause. Treatment consists of a two-week course of an appropriate antibiotic, such as amoxicillin/clavulanate (Augmentin) 34.
Upper airway cough syndrome (postnasal drip syndrome) is rare in children younger than six years, and antihistamines and decongestants are not recommended 35. GERD does not seem to be as common in children, and empiric proton pump inhibitors are not recommended in the absence of a specific diagnosis 31. Exposure to tobacco smoke, pets, and environmental irritants should be minimized. Pertussis can be considered but is usually associated with other symptoms, such as a “whoop” sound, apnea, low-grade fever, or vomiting. Less common causes, such as foreign body aspiration, congenital conditions, cystic fibrosis, and immune disorders, should also be considered.
References- Chronic cough. https://www.mayoclinic.org/diseases-conditions/chronic-cough/symptoms-causes/syc-20351575
- Chronic Cough: Evaluation and Management. Am Fam Physician. 2017 Nov 1;96(9):575-580. https://www.aafp.org/afp/2017/1101/p575.html
- Centers for Disease Control and Prevention. National ambulatory medical care survey: 2013 state and national summary tables. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2013_namcs_web_tables.pdf
- Irwin RS, Madison JM. The diagnosis and treatment of cough. N Engl J Med. 2000;343(23):1715–1721.
- French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med. 1998;158(15):1657–1661.
- Irwin RS, Baumann MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):1S–23S.
- Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):63S–71S.
- Mello CJ, Irwin RS, Curley FJ. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. Arch Intern Med. 1996;156(9):997–1003.
- Meltzer EO, Hamilos DL, Hadley JA, et al.; American Academy of Allergy, Asthma and Immunology (AAAAI); American Academy of Otolaryngic Allergy (AAOA); American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS); American College of Allergy, Asthma and Immunology (ACAAI); American Rhinologic Society (ARS). Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114(6 suppl):155–212.
- Dicpinigaitis PV. Chronic cough due to asthma: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):75S–79S.
- Brightling CE. Cough due to asthma and nonasthmatic eosinophilic bronchitis. Lung. 2010;188(suppl 1):S13–S17.
- Johnstone KJ, Chang AB, Fong KM, Bowman RV, Yang IA. Inhaled corticosteroids for subacute and chronic cough in adults. Cochrane Database Syst Rev. 2013;(3):CD009305
- Qureshi H, Sharafkhaneh A, Hanania NA. Chronic obstructive pulmonary disease exacerbations: latest evidence and clinical implications. Ther Adv Chronic Dis. 2014;5(5):212–227.
- Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):169S–173S.
- Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371(9621):1364–1374.
- Kahrilas PJ, Smith JA, Dicpinigaitis PV. A causal relationship between cough and gastroesophageal reflux disease (GERD) has been established: a pro/con debate. Lung. 2014;192(1):39–46.
- Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology. 2011;16(7):1150–1156.
- Chang AB, Lasserson TJ, Gaffney J, Connor FL, Garske LA. Gastrooesophageal reflux treatment for prolonged non-specific cough in children and adults. Cochrane Database Syst Rev. 2011;(1):CD004823.
- Kahrilas PJ, Altman KW, Chang AB, et al.; CHEST Expert Cough Panel. Chronic cough due to gastroesophageal reflux in adults: CHEST guideline and expert panel report. Chest. 2016;150(6):1341–1360.
- Xu X, Lv H, Yu L, Chen Q, Liang S, Qiu Z. A stepwise protocol for the treatment of refractory gastroesophageal reflux-induced chronic cough. J Thorac Dis. 2016;8(1):178–185.
- Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999;160(2):406–410.
- Dąbrowska M, Grabczak EM, Arcimowicz M, et al. Causes of chronic cough in non-smoking patients. Adv Exp Med Biol. 2015;873:25–33.
- Alhajjaj MS, Bajaj P. Chronic Cough. [Updated 2019 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430791
- Benich JJ III, Carek PJ. Evaluation of the patient with chronic cough. Am Fam Physician. 2011;84(8):888.
- Sundar KM, Daly SE. Chronic cough and OSA: an underappreciated relationship. Lung. 2014;192(1):21–25.
- Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):262S.
- Iyer VN, Lim KG. Chronic cough: an update. Mayo Clin Proc. 2013;88(10):1118.
- Irwin RS, French CT, Lewis SZ, Diekemper RL, Gold PM; CHEST Expert Cough Panel. Overview of the management of cough: CHEST guideline and expert panel report. Chest. 2014;146(4):885–889.
- Driessen AK, McGovern AE, Narula M, et al. Central mechanisms of airway sensation and cough hypersensitivity. Pulm Pharmacol Ther. 2017:S1094–S5539(17)30016-0
- Chamberlain Mitchell SA, Garrod R, Clark L, et al. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough: a multicentre randomised control trial. Thorax. 2017;72(2):129–136.
- Chang AB, Glomb WB. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):260S–283S.
- Asilsoy S, Bayram E, Agin H, et al. Evaluation of chronic cough in children. Chest. 2008;134(6):1122–1128.
- Gibson PG, Chang AB, Glasgow NJ, et al. CICADA: cough in children and adults: diagnosis and assessment. Australian cough guidelines summary statement. Med J Aust. 2010;192(5):265–271.
- Chang AB, Upham JW, Masters IB, et al. Protracted bacterial bronchitis: the last decade and the road ahead. Pediatr Pulmonol. 2016;51(3):225–242.
- Marchant J, Masters IB, Champion A, Petsky H, Chang AB. Randomised controlled trial of amoxycillin clavulanate in children with chronic wet cough. Thorax. 2012;67(8):689–693.