Contusion
Contusion is a medical term for a bruise or hematoma, which is a mark on your skin caused by blood trapped under the surface. Contusion happens when an injury crushes small blood vessels or capillaries but does not break the skin. Those small blood vessels break open and leak blood under the skin.
Contusions are often painful and swollen. You can get skin, muscle and bone contusion. Bone contusions are the more severe and painful.
There are three types of bruises:
- Subcutaneous — beneath the skin
- Intramuscular — within the belly of the underlying muscle
- Periosteal — bone bruise
Contusions are often caused by falls, sports injuries, car accidents, or blows received from other people or objects.
If you take a blood thinner, such as aspirin, warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), or clopidogrel (Plavix), you are likely to bruise more easily.
It can take months for a bruise to fade, but most last about two weeks. Contusion starts off a reddish color, and then turn bluish-purple and greenish-yellow before returning to normal. To reduce bruising, ice the injured area and elevate it above your heart.
Apply a cold compress to the bruise to help slow down the blood that’s flowing to the area, which decreases the amount of blood that ends up leaking into the tissues. It also helps keep the inflammation and swelling down. All you have to do is apply cold to the bruise for 15 to 20 minutes every hour for a day or two after the bruise appears.
You don’t need to buy a special cold pack, although they’re great to keep on hand in the freezer. Just get some ice, put it in a plastic bag, and wrap the bag in a cloth or a towel and place it on the bruise (don’t apply the ice directly to the skin).
Another trick is to use a bag of frozen vegetables. It doesn’t matter what kind — carrots, peas, lima beans, whatever — as long as they’re frozen. A bag of frozen vegetables is easy to apply to the bruise because it can form to the shape of the injured area. Also, like a cold pack, it can be used and refrozen again and again (just pick your least-favorite vegetables and label the bag — you don’t want to keep thawing and freezing veggies that you plan to eat!).
To reduce swelling and bruising, elevate the bruised area above the level of your heart. In other words, if the bruise is on your shin, lie down on a couch or bed and prop up your leg. This will help prevent blood from pooling in the area because more of the blood will flow back toward your heart. If you keep standing, more blood will flow to your bruised shin and the bruise will be larger.
Take acetaminophen for pain, if needed.
DO NOT
- Do not try to drain the bruise with a needle.
- Do not continue running, playing, or otherwise using the painful, bruised part of your body.
- Do not ignore the pain or swelling.
In the rare case of compartment syndrome, surgery is often done to relieve the extreme buildup of pressure. Compartment syndrome results from increased pressure on the soft tissues and structures beneath the skin. It can decrease the supply of blood and oxygen to the tissues.
See your health care provider if you seem to bruise for no reason, or if the bruise appears to be infected. Signs of infection around the bruised area including streaks of redness, pus or other drainage, or fever.
Also see your doctor for a bruise if:
- A bruise isn’t improving after 2 weeks.
- You bruise often and bruises seem to develop for no known reasons.
- Your bruise is swelling and very painful.
- You can’t move a joint or you think you may have a broken bone.
- The bruise is near your eye and you have difficulty moving your eyes or seeing
How long does contusion last?
Bruises usually fade away in about 2 weeks. Over that time, the bruise changes color as the body breaks down and reabsorbs the blood. The color of the bruise can give you an idea how old it is:
- When you first get a bruise, it’s kind of reddish as the blood appears under the skin.
- Within 1 or 2 days, the hemoglobin (an iron-containing substance that carries oxygen) in the blood changes and your bruise turns bluish-purple or even blackish.
- After 5 to 10 days, the bruise turns greenish or yellowish.
- Then, after 10 or 14 days, it turns yellowish-brown or light brown.
Finally, after about 2 weeks, your bruise fades away.
Bone contusion
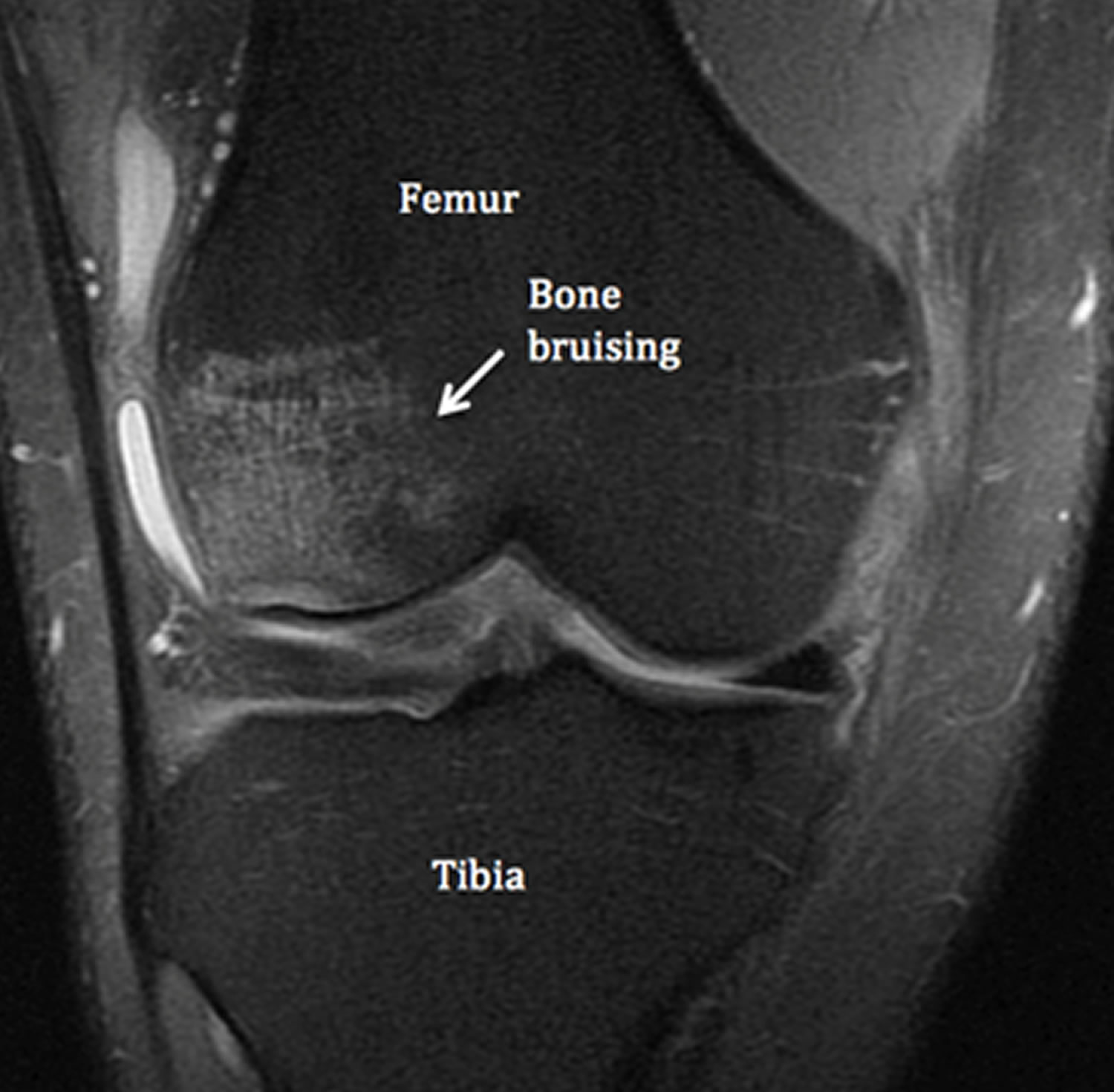
Bone contusion also called bone bruise, subchondral edema, bone marrow edema or trabecular microfractures not visible on plain x-ray images 1, results from traumatic compressive forces incurred during an injury. The damaged area occurs in the medullary portion of the bone and can be accompanied by bleeding and swelling. Bone contusions are acute traumatic noncystic areas of bone marrow edema, and they can be distinguished from cystic lesions and atraumatic presentations 2. The pathophysiology of bone marrow edema is currently nonspecific, and differentiation of the different causes can be difficult. In particular, distinguishing among osteochondritis dissecans, spontaneous osteonecrosis of the knee, and idiopathic transient bone marrow lesion syndrome is difficult because ischemic and microtraumatic factors both contribute to their presentation 3.
Bone contusions are often caused by falls, sports injuries, car accidents, or blows from other people or objects. Bone contusion can lasts from days to months, with the bone bruise being the most severe and painful.
Several classification systems have been proposed for bone contusion. Most authors agree on the differentiation between reticular and geographic/demarcated pattern. Others stress the importance of the location – subchondral vs at distance of joint space.
Costa-Paz et al 4 proposes the following classification:
- Type 1: Diffuse often reticular alterations of the medullary component, distant from the subjacent articular surface.
- Type 2 a and b: Localised geographic signal (mostly convex margins towards normal marrow) with contiguity to articular surface. In a type 2 lesion compared to type 1, the impact is more focally concentrated.
- Type 3: Slight disruption or depression of the normal contour of the cortical surface/subchondral lamella, often associated with type 2 lesion (small osteochondral fractures).
Another classification for the 3 different kinds of bone bruises 5, 6:
- Sub-periosteal hematoma: This is a concentrated collection of blood underneath the periosteal of the bone. It will appear mostly after a direct high-force trauma on the bone. This type is most common in the lower extremities.
- Inter-osseous bruising: This is a damage of the bone marrow. The blood supply within the bone is damaged, and this causes internal bleedings. The trigger to this type of bone bruise is a repetitive high compressive force on the bone (extreme pressure on regular base). The areas most affected are the knee and the ankle from professional athletes, such as foot-, basketball players and runners.
- Sub-chondral lesion: This type will occur beneath the cartilage layer of a joint. The main trigger is an extreme compressive force that literally crushes the cells, that results in a separation of the cartilage (or ligament) and the underlying bone, plus bleeding when the energy of the impact extends into the bone.
The other trigger is a shearing force, it sustains from a rotational mechanism such as twisting and translational forces. These will also cause that the cartilage tissue will be stripped away and exposing the underlying bone. It results in the same injury as a compressive force injury but this is another source of the injury. This type is seen more frequently in foot- and basketball players.
Figure 1. Bone bruise knee MRI
Bone contusion signs and symptoms
It is very difficult to identify clinical signs and symptoms directly attributable to the underlying bone bruise, because there are usually associated soft tissue changes.
In a prospective study of 95 patients with inversion injuries of the ankle and no plain fracture on plain radiographs, Alanen et al found an incidence of bone bruises of 27 percent. Most of the bone bruises were located in the talus, typically in the medial part. The authors further found no statistical difference in the time to return to work, limitation to walking or physical activity and clinical outcome at 3 months in the two groups with and without bone bruise. This findings were in line with previous study by Zanetti et al.
In another study involving the knee joint and bone bruise, bone bruise did not have any effect on the function, symptoms and activity at 6 months, despite patients initially presenting with bone bruise at the time of MRI had a significant higher level of symptoms, functional deficit and decrease in activity.
Bone contusion diagnosis
Difficulty arises in identifying clinical signs and symptoms directly attributable to the bone bruising, because of the spectra of associated injuries. However, patients with bone contusions appear to have a more protracted clinical recovery, with greater effusions and pain scores at matched time intervals and a slower return of motion 7.
Arthroscopic evidence of damage to the joint surface overlying bone bruises is not universally supported in the literature. Several authors found no arthroscopic evidence of osteochondral lesions corresponding anatomically with bone bruises in the acute phase 8, 9. Coen described normal joint appearance but “dimpling” of the cartilage over geographic femoral bruises when probed 10. Several authors describe articular lesions later at the time of anterior cruciate ligament reconstruction 11, 12. Speer found a small incidence of fissuring (6%) overlying lateral femoral condyle and posterolateral tibial plateau contusions 13. Although Spindler found 46% of patients had articular lesions, many did not correlate with bone bruise. The only significant relationship was in the lateral femoral condyle where 40% of bone bruises had an overlying lesion 12. In contrast, Johnson consistently found evidence of articular cartilage injury over femoral condyle bone bruises, varying from subtle indentation when probed, to severe fibrillation, fissuring or overt chondral fracture 14.
Some interesting histological information has arisen from biopsy at varying time periods 15. In acute lesions, Rangger found microfractures of the trabecular bone, oedema and bleeding in the fatty marrow 16. In Johnson’s series, all patients had articular cartilage and subchondral bone changes at ACL reconstruction. Chondrocytes in the superficial zone of the articular cartilage showed different stages of degeneration, and loss of matrix proteogylcan and variable osteocyte necrosis in the underlying subchondral bone was noted 14. Fang supported the evidence for proteoglycan loss and also found a 10-fold increase in matrix protein degradation products in the synovial fluid from injured compared with uninjured knees 15. This clinical data supports previous animal studies suggesting blunt trauma to articular cartilage produces profound changes in its histologic, biochemical and ultrastructural characteristics in the absence of surface disruption 17 and lends scientific evidence to the notion that bone bruising may be a precursor of posttraumatic arthritis.
Bone contusion treatment
Bone contusion treatment may consist of the following methods: ice therapy, elevation, medication and/or rest.
- Ice Therapy – An effective way to treat a bone bruise is to apply a pack of frozen vegetables or an ice pack to the injured bone. Ice therapy can ease the pain and reduce the inflammation in the affected area. Apply ice to the injured bone for 15 to 20 minute intervals, several times a day. Make sure to place a towel or washcloth over the affected area before you place the ice on it. Placing ice directly on the skin can cause frostbite.
- Elevation – Another beneficial bone bruise treatment is elevation. The first step when treating a bone bruise is to raise the affected area above the heart. This step prevents and/or limits fluid accumulation in the affected area, therefore reducing the risk of a bone bruise. Once the fluid has been restricted or reduced, the body is more efficiently able to repair the injured bone. It is important to elevate the affected area (injured bone) for 15 to 20 minutes, several times a day.
- Rest – One of the easiest and most effective ways to help a bone bruise heal is to rest it. Staying off the injured bone can help it heal. Walking and/or moving the damaged bone not only causes extra stress and pressure in the affected area, it also delays the healing process. In fact, excess stress and pressure can cause the blood vessels in the affected area to break, leading to blood accumulation, pain and/or bone damage. A physician may suggest the use of an assistive walking device such as: a walker, cane or crutches until the bone properly heals. Physical activity should also be limited or restricted while the bruised bone is trying to heal.
- Medication – Bone bruises can be treated with medications when natural remedies do not work. Medications like topical pain-relieving creams and gels and over-the-counter pain- relieving medications like Tylenol, Bayer and Excedrin have the ability to ease pain, reduce inflammation and aid in the healing process. Many medications, especially non-steroidal anti-inflammatory drugs, can change the way the brain interprets and responds to inflammation and pain, therefore accelerating the healing process.
Myocardial contusion
Myocardial contusion also called cardiac contusion, is a bruise of the heart muscle. Cardiac contusion is usually caused by blunt chest trauma and therefore is frequently suspected in patients involved in car or motorcycle accidents 18. The diagnosis of a myocardial contusion is difficult because of non-specific symptoms and the lack of an ideal test to detect myocardial damage. Cardiac contusion can cause life threatening arrhythmias and cardiac failure 19. If patients receive adequate treatment for such complications, death due to cardiac causes is rare. In one study, one patient (1.5%) died of persistent cardiogenic shock and in another study three severely injured patients died before treatment had been started 20.
In mildly injured patients a cardiac contusion is generally well tolerated. The majority of such patients never suffer any symptoms and proceed to an uncomplicated recovery with an excellent prognosis. However, life threatening ventricular arrhythmias and cardiac failure can also occur in these symptomless patients. It is therefore important to screen all patients with blunt chest trauma to identify those at risk for complications.
Cardiac contusion causes
The most common causes of myocardial contusion are:
- Car crashes
- Getting hit by a car
- Cardiopulmonary resuscitation (CPR)
- Falling from a height, most often greater than 20 feet (6 meters)
Cardiac contusion prevention
The following safety tips may help prevent a myocardial contusion:
- Wear a seat belt when driving.
- Choose a car with air bags.
- Take steps to ensure safety when working at heights.
Cardiac contusion symptoms
A severe myocardial contusion may lead to signs and symptoms of a heart attack.
Myocardial contusion symptoms can include:
- Pain in the front of the ribs or breastbone
- Feeling that your heart is racing
- Lightheadedness
- Nausea or vomiting
- Shortness of breath
- Weakness
Cardiac contusion complications
Early and late complications of cardiac contusion
- Early complications
- Ventricular and supraventricular arrhythmias
- Myocardial wall rupture with haemopericardium and tamponade
- Ventricular septum rupture
- Valvar insufficiencies caused by valvar lesions and papillary muscle ruptures
- Intracardiac thrombus resulting in thromboembolic events
- Coronary artery lesions with acute myocardial infarction
- Late complications
- Ventricular aneurysm
- Chronic dilated cardiac dysfunction
- Cardiac dysfunction caused by structural cardiac lesions
- Constrictive pericarditis
- Ventricular arrhythmias originating from myocardial scar tissue or aneurysm
Cardiac contusion diagnosis
Your health care provider will perform a physical exam. This may show:
- Bruise or scrapes on the chest wall
- Crunching sensation when touching the skin if there are rib fractures and puncture of the lung
- Fast heartbeat
- Irregular heartbeat
- Low blood pressure
- Rapid or shallow breathing
- Tenderness to the touch
- Abnormal chest wall movement from rib fractures
Tests may include:
- Blood tests (cardiac enzymes, such as Troponin-I or T or creatine kinase-MB)
- Chest x-ray
- CT scan of the chest
- Electrocardiogram (ECG or EKG)
- Echocardiogram
These tests may show:
- Problems with the heart wall and the ability for the heart to contract
- Fluid or blood in the thin sac surrounding the heart (pericardium)
- Rib fractures, lung or blood vessel injury
- Problem with the heart’s electrical signaling (such as a bundle branch block or other heart block)
- Fast heartbeat starting at the sinus node of the heart (sinus tachycardia)
- Abnormal heartbeat starting in the ventricles or lower chambers of the heart (ventricular dysrhythmia)
Electrocardiographic findings in cardiac contusion 18
- Non-specific abnormalities
- Pericarditis-like ST segment elevation or PTa depression
- Prolonged QT interval
- Myocardial injury
- New Q wave
- ST-T segment elevation or depression
- Conduction disorders
- Right bundle branch block
- Fascicular block
- AV nodal conduction disorders (1, 2, and 3 degree AV block)
- Arrhythmias
- Sinus tachycardia
- Atrial and ventricular extrasystoles
- Atrial fibrillation
- Ventricular tachycardia
- Ventricular fibrillation
- Sinus bradycardia
- Atrial tachycardia
Echocardiographic findings in acute cardiac contusion 18
- Transthoracic echocardiography
- Regional wall motion abnormalities
- Pericardial effusion
- Valvar lesions
- Right and left ventricular enlargement
- Ventricular septum rupture
- Intracardiac thrombus
- Transoesophageal echocardiography
- Aortic endothelial laceration or aortic dissection
- Aortic rupture
Cardiac contusion treatment
In most cases, you will be closely monitored for at least 24–48 hours after the trauma 21. An electrocardiogram (ECG) will be done continually to check your heart function. 81–95% life threatening ventricular arrhythmias and acute cardiac failures occur within 24–48 hours after the trauma 19
Emergency room treatment may include:
- Catheter placement through a vein (IV)
- Medicines to relieve pain, heart rate disturbances, or low blood pressure
- Pacemaker (temporary, may be permanent later)
- Oxygen
Other therapies may be used to treat a heart injury, include:
- Chest tube placement
- Draining blood from around the heart
- Surgery to repair blood vessels in the chest
Cardiac contusion prognosis
People with a mild myocardial contusion will recover completely most of the time. Serious heart injuries can increase your risk for heart failure or heart rhythm problems.
Severe cardiac injury with myocardial necrosis heals by scar formation, similar to that in ischemic myocardial infarction. This may lead to ventricular aneurysm formation and in some cases to chronic heart failure 22. A previous cardiac contusion must be taken into consideration in case of unexplained dilated cardiac dysfunction (especially if the right ventricle is affected), aneurysms of the ventricles or coronary arteries, unexplained constrictive pericarditis, or valvar lesions 23.
Pulmonary contusion
Pulmonary contusion is a medical term for lung contusion, which is injury to the alveolar capillaries, so blood and other fluids accumulate in the lung tissue, but it does not involve a cut or a tear of the lung tissue 24. Pulmonary contusion occurs in 25–35% of all blunt chest traumas, explosion injuries or a shock wave associated with penetrating trauma. This results in accumulation of blood and other fluids within the lung tissue. The excess fluid interferes with gas exchange leading to hypoxia. Pulmonary contusion is an independent risk factor for development of Acute Respiratory Distress Syndrome (ARDS) 25, pneumonia 26, long-term respiratory dysfunction, and is associated with 10 to 25% mortality rate 27. The pathophysiology of lung contusion includes ventilation/perfusion mismatching, increased intrapulmonary shunting, increased lung water, segmental lung damage, and a loss of compliance 28. Clinically, patient’s presents with hypoxiemia, hypercarbia and increase in laboured breathing of varying severity and duration 29. Patients are treated with supplemental oxygen and mechanical ventilation whenever indicated. Treatment is primarily supportive. Computed tomography (CT) is very sensitive for diagnosing pulmonary contusion.
Pulmonary contusion causes
Pulmonary contusion occurs by rapid deceleration when the moving chest strikes a fixed object 30. Pulmonary contusion occurs in 25-35% of all blunt chest traumas 31. Lung tissue is crushed when the chest wall bends inward on impact 32. Other causes are falls, assaults and sports injuries.
The pathophysiology of pulmonary contusion and blunt chest trauma includes inflammation, increased alveolo-capillary permeability and pulmonary edema, ventilation/perfusion mismatching increased intrapulmonary shunting, and a loss of compliance 33. Clinically, patients with pulmonary contusion manifest in hypoxemia, hypercarbia, and intensified labored breathing 34. Pulmonary contusion results in bleeding 35 and fluid leakage into lung tissue, which becomes rigid and loses its normal elasticity. The water content of the lung increases over the first 72 hours after injury, and may lead to frank pulmonary edema in more serious cases 34. The membrane between alveoli and capillaries is torn, and damage to small blood vessels causes both blood and fluid to leak into the alveoli and the interstitial space of the lung 36. Pulmonary contusion is characterized by micro-hemorrhages that occur when the alveoli are traumatically separated from airway structures and blood vessels 37. The contused lung is commonly surrounded by an area of edema 37. Fluid accumulation in alveoli interferes with gas exchange 38 and causes alveoli to be filled with proteins and collapse 37.
Pulmonary contusion prevention
Airbags in combination with seat belts distribute impact in the motor crashes more evenly across the body 39. Child restraints such as car seats protect children from pulmonary contusion in vehicle collisions 40. Special body armor for military personnel at high risk of sustaining blast injuries, prevent shock wave propagation across the chest wall to the lung, and thus protect wearers from blast lung injuries 41. These garments contain materials with alternate layers of high and low acoustic impedance in order to “decouple” the blast wave, thereby preventing its propagation in the tissues 41.
Pulmonary contusion symptoms
Impaired gas exchange at alveolar level, leads to decreasing blood oxygen saturation, reduced concentration of oxygen in arterial blood, cyanosis and dyspnea 39. There is decreased exercise tolerance 42. Patient may become tachypnoic and may have tachycardia 43 with more severe contusions. On auscultation, patient may have rales and decreased breath sounds in severe contusion 39. There may be wheezing, coughing, bronchorrhea and blood streaked sputum in up to half of cases 30. There may be hypotension and reduced cardiac output 36. Respiratory distress due to hypoxia and hypercarbia peaks at around 72 hours 44.
Pulmonary contusion complications
Pulmonary contusion usually resolves spontaneously in 3 to 5 days, provided no secondary insult occurs. The main complications of pulmonary contusion are Acute Respiratory Distress Syndrome (ARDS) and pneumonia. Acute Respiratory Distress Syndrome (ARDS) develops in 17% of patients with isolated pulmonary contusion, while 78% of those with additional injuries develop ARDS 39. Lung trauma, alveolar hypoxia and blood in the alveolar spaces all activate the inflammatory pathways that result in acute lung injury. Blood in the alveolar spaces provide an excellent medium for bacteria. Clearance of secretions from contused area is decreased which is augmented by any chest wall injury and mechanical ventilation. Good tracheal toilet and pulmonary care is essential to minimize the incidence of pneumonia in this susceptible group. Pneumonia, another potential complication, develops in 20% of people with pulmonary contusion 45.
Pulmonary contusion diagnosis
The following aspects are considered for the diagnosis of pulmonary contusion: mode of injury, physical examination, radiography 46, arterial blood gasses showing insufficient oxygen and excessive carbon dioxide even on receiving supplemental oxygen 47.
a) Chest X-ray: Chest X-ray (CXR) is the most common method used for diagnosis 48. Contusion is not restricted by the anatomical boundaries of the lobes or segments of the lung 49. The presence of hemothorax or pneumothorax may obscure the contusion on a radiograph 50. Signs of contusion that progress after 48 hours of injury are due to aspiration, pneumonia, or Acute Respiratory Distress Syndrome (ARDS) 51. It takes an average of six hours for the characteristic white region to show up on a chest X-ray, and sometimes contusion may not become apparent for 48 hours 49.
b) Computed tomography (CT): Findings on chest radiography vary from irregular, patchy areas of consolidation to diffuse and extensive homogeneous consolidation. Radiographic changes of contusion are evident within 6 hours after trauma to the chest, and resolve rapidly, typically within 3 to 10 days. CT findings of contusion consist of non-segmental areas of consolidation and ground-glass opacification that predominantly involve the lung and directed deeply into the area of trauma, often sparing 1 to 2 mm of sub-pleural lung parenchyma adjacent to the injured chest wall 52. CT is highly sensitive in detecting pulmonary contusions and the volume of lung involvement on CT scanning correlates with clinical outcomes 53. Unlike X-ray, CT scanning can detect the contusion almost immediately after the injury 49.
c) Ultrasound: Portable bedside ultrasound can be equated to visual stethoscope of the 21st century. A lung contusion is diagnosed by the presence of:
- (a) an irregularly delineated tissue image, which could be a moderately hypo-echoic blurred lesion with no change during respiration or hyper-echoic punctiform images corresponding to air bronchogram;
- (b) multiple B-lines.
The overall sensitivity of 94.6% for ultrasound and 27% for initial chest X-ray 54 to diagnose lung contusion proves sufficient evidence for ultrasonography to diagnose lung contusion in emergency settings. Thoracic ultrasonography as a bedside diagnostic modality is a better diagnostic test than CT and chest X-ray (CXR). In comparison with CT scanning, it is a better bedside diagnostic modality when evaluating supine chest trauma patients in the emergency situations, particularly for diagnosing pneumothorax and lung contusions 55; c) Sub-pleural, echo-poor, irregular bordered lesions without air-inlets and lacking a large focal effusion 56; d) alveolo- interstitial syndrome defined by increased number of comet tail artifacts/B-lines 57; e) moderate hypo-echoic blurred lesions with indistinct margins of constant dimension even during breathing 56.
d) Histopathological changes: Histopathological evaluation of the lung tissue at 8 min, 4 hour, and 12 hour post-contusion revealed diffuse intra-alveolar hemorrhage with alveolar disruption, along with interstitial hemorrhagic injury that frequently involve peri-hilar areas and extended to the visceral surface of the pleura. At 24 hour post-contusion, atelectasis is pronounced, and there is neutrophilic predominance within the alveoli and interstitium. At 48 hour, neutrophilic infiltration still predominates, while alveolar lining tissue is thickened with an increase in alveolar macrophage and cellular debris 58. Post-contusion fibrosis around bronchioles predominates after 7 days 58.
Pulmonary contusion treatment
Most lung contusions will require no specific therapy as such. The modality of care in lung contusion is to prevent additional injury, provide supportive care while waiting for the contusion to heal 59. Treatment helps prevent respiratory failure and to ensure adequate blood oxygenation 60. But large pulmonary contusions may affect gas exchange and result in hypoxemia. As the physiological impact of the contusion tends to develop over 24-48 hours, close monitoring is required along with administering supplemental oxygen. Tracheal intubation and mechanical ventilation may be necessary if there is difficulty in oxygenation or ventilation. Usually ventilatory support can be discontinued once the pulmonary contusion has resolved, irrespective of the chest wall injury. When the contusion does not respond to other treatments, extracorporeal membrane oxygenation may be used 61. Lung volume and compliance decrease marginally at 24 hour post-contusion injury 58.
Ventilation
Noninvasive positive pressure ventilation including continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) may be used to improve oxygenation and treat atelectasis 59. However it may cause gastric distension by forcing air into the stomach or cause aspiration of stomach contents, especially when level of consciousness is decreased 35. People with signs of inadequate respiration or oxygenation may need to be intubated 42 and mechanically ventilated 30. Ventilation can re-open collapsed alveoli, but their repeated opening will be harmful, and positive pressure ventilation can also damage the lung by overinflation 62. ARDS as a complication of traumatic lung contusion may cause lungs to lose compliance, so higher pressures may be needed to give normal amounts of air 35. When the compliance of the injured lung differs significantly from that of the uninjured one, the lungs can be ventilated independently with two ventilators in order to deliver air at different pressures; this provides adequate ventilation and prevents the injury of uninvolved lung from overinflation 63.
A recruitment maneuver is a sustained increase in airway pressure typically performed by increasing the positive end expiratory pressure (PEEP) setting on the ventilator to 30 to 40 cms H2O for 30 to 40 minutes, followed by applying a sufficient amount of positive end expiratory pressure (PEEP) to keep the lungs open. This strategy is being presumed to be helpful in traumatic lung contusion. Quasistatic pulmonary inflation volumes were severely reduced at 8 min post-contusion, and abnormalities in inflation mechanics persisted at 12 to 24 hours 58. The presence of very early decreases in lung inflation volumes with a lower point of inflection in the inflation P-V curve suggests that recruitment of alveoli with optimal PEEP might play an important therapeutic role in lung contusion 58. Early positive pressure ventilation with PEEP has been shown to be beneficial in some patients with lung contusion 64. Peak abnormalities in deflation P-V mechanics occurred at 24 h post-contusion 58.
Fluid therapy
The administration of fluid therapy in individuals with pulmonary contusion is controversial [55]. Measuring pulmonary artery pressure allows the clinician to give enough fluids to prevent shock without exacerbating edema 65.
Diuretics
Diuretics decrease fluid overload in the body system 66 and may be used in the treatment of pulmonary contusion to relax the smooth muscle of the pulmonary veins, thereby lowering pulmonary venous resistance and reducing pressure in the pulmonary capillaries 67.
Supportive care
Pulmonary toilet, use of suction, deep breathing, coughing, and other methods to remove mucus and blood from the airways 42, chest physiotherapy using methods such as breathing exercises, stimulation of coughing, suctioning, percussion, movement, vibration, and drainage to rid the lungs of secretions, increase oxygenation, and expanding collapsed parts of the lungs 64.
Pulmonary contusion prognosis
The mortality rate of pulmonary contusion is estimated to range from 14–40%, depending on the severity of the contusion and associated injuries 36. Another study reported, 11% mortality with isolated pulmonary contusion, whereas the number rose to 22% in those with additional injuries 39. Clearance of an uncomplicated contusion begins at 24 to 48 hours with complete resolution after 3 to 14 days 42.
Brain contusion
Brain contusion is a bruise of the brain, in which swollen brain tissue mixes with blood released from broken blood vessels. Brain contusion can occur from the brain shaking back and forth against the skull, such as from a car collision or sports accident or in shaken baby syndrome. Brain contusion is commonly identified in patients with traumatic brain injury and represent regions of primary neuronal and vascular injury 68. Brain contusions are formed in 2 ways: direct trauma and acceleration/deceleration injury 69.
Traumatic brain injury is a common presentation in emergency departments, which accounts for more than one million visits annually. It is a common cause of death and disability among children and adults 70.
Based on the Glasgow Coma Scale (GCS) score, it is classified as 71:
- Mild = GCS 14 to 15, also called concussion
- Moderate = GCS 9 to 13
- Severe = GCS 3 to 8
Brain contusion causes
The leading causes of head trauma are (1) motor vehicle-related injuries, (2) falls, and (3) assaults 72.
Based on the mechanism, head trauma is classified as (1) blunt (most common mechanism), (2) penetrating (most fatal injuries), (3) blast.
Most severe traumatic brain injuries result from motor vehicle collisions and falls.
Another cause of traumatic brain injury is shaken baby syndrome. Shaken baby syndrome can occur when an infant is shaken violently or hit. Nearly all victims of shaken baby syndrome suffer serious health consequences, and many babies who are violently shaken die.
Traumatic brain injury can be classified as primary injury and secondary injury:
Primary Injury
Primary injury includes injury upon initial impact that causes displacement of the brain due to direct impact, rapid acceleration-deceleration, or penetration. These injuries may cause contusions, hematomas, or axonal injuries.
- Contusion (bruise on the brain parenchyma)
- Hematoma (subdural, epidural, intraparenchymal, intraventricular, and subarachnoid)
- Diffuse axonal injury (stress or damage to axons)
Secondary Injury or Secondary Neurotoxic Cascade
Secondary injury consists of the changes that occur after the initial insult. It can be due to:
- Systemic hypotension
- Hypoxia
- Increase in intracranial pressure (ICP)
After a primary brain injury, a cascade of cellular and biochemical events occurs which include the release of glutamate into the presynaptic space resulting in activation of N-methyl-D-aspartate, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid, and other receptors. This ionic shift may activate cytoplasmic and nuclear enzymes, resulting in mitochondrial damage, and cell death and necrosis.
Brain contusion prevention
Some causes of traumatic brain injury are avoidable. The list below offers some ways to help prevent traumatic brain injury.
- Always wear a seat belt when riding in a motor vehicle.
- Make sure a child in a car is protected with a child safety seat and/or seat belt.
- Never drive while under the influence of alcohol or drugs.
- Wear a helmet and make sure children wear the appropriate helmets for such activities as bike-riding, skateboarding, and playing certain sports.
- Make living areas safer for older people with measures such as removing rugs and other tripping hazards and improving lighting throughout the home.
- Install window guards to keep young children from falling out of windows, and use safety gates at the top and bottom of stairs when young children are around 73.
Another preventable cause of traumatic brain injury is shaken baby syndrome. Preventing shaken baby syndrome involves helping people understand the dangers of shaking a baby, the risk factors and the triggers for shaken baby syndrome, and how to support overstressed parents and caregivers 74.
Brain contusion symptoms
Traumatic brain injury symptoms vary depending on the extent of the injury and the area of the brain affected. Some symptoms appear immediately; others may appear several days or even weeks later. A person with traumatic brain injury may or may not lose consciousness—loss of consciousness is not always a sign of severe traumatic brain injury.
Symptoms of mild traumatic brain injury
A person with a mild traumatic brain injury may experience:
- Headache
- Confusion
- Lightheadedness
- Dizziness
- Blurred vision
- Ringing in the ears
- Tiredness or sleepiness
- A bad taste in the mouth
- A change in sleep habits
- Behavior or mood changes
- Trouble with memory, concentration, attention, or thinking
- Loss of consciousness lasting a few seconds to minutes 75
- Sensitivity to light or sound
- Nausea or vomiting 76
Symptoms of moderate or severe traumatic brain injury
A person with moderate or severe traumatic brain injury may have some of the symptoms listed above. In addition, the person may experience any of the following:
- Headache that gets worse or won’t go away
- Repeated vomiting or nausea
- Slurred speech
- Convulsions or seizures
- An inability to wake up from sleep
- Enlargement of the pupil (dark center) of one or both eyes
- Numbness or tingling of arms or legs
- Loss of coordination
- Increased confusion, restlessness, or agitation
- Loss of consciousness lasting a few minutes to hours 77
A person who suffers a blow to the head or another trauma that may have caused a traumatic brain injury should seek medical attention.4
Brain contusion diagnosis
To diagnose traumatic brain injury, health care providers may use one or more tests that assess a person’s physical injuries, brain and nerve functioning, and level of consciousness.
The Glasgow Coma Scale (GCS) measures a person’s functioning in three areas:
- Ability to speak, such as whether the person speaks normally, speaks in a way that doesn’t make sense, or doesn’t speak at all
- Ability to open eyes, including whether the person opens his or her eyes only when asked
- Ability to move, ranging from moving one’s arms easily to not moving even in response to painful stimulation
A health care provider rates a person’s responses in these categories and calculates a total score. A Glasgow Coma Scale (GCS) score of 13 and higher indicates a mild traumatic brain injury, 9 through 12 indicates a moderate traumatic brain injury, and 8 or below indicates severe traumatic brain injury 77. However, there may be no correlation between initial GCS score and the person’s short- or long-term recovery or abilities 78.
A traumatic brain injury is considered mild if:
- The person was not unconscious or was unconscious for less than 30 minutes.
- Memory loss lasted less than 24 hours.
- The GCS was 13 to 15.
Research has found, however, that diagnosis of mild traumatic brain injury (concussion), in practice, uses inconsistent criteria and relies heavily on patients’ self-reported symptoms 79.
A traumatic brain injury is considered moderate if:
- The person was unconscious for more than 30 minutes and up to 24 hours.
- Memory loss lasted anywhere from 24 hours to 7 days.
- The GCS was 9 to 12.
A traumatic brain injury is considered severe if:
- The person was unconscious for more than 24 hours.
- Memory loss lasted more than 7 days.
- The GCS was 8 or lower 80
CT scan is required in patients with head trauma
- Moderate (GCS score 9 to 12)
- Severe (GCS score < 8)
For patients who are at low risk for intracranial injuries, there are two externally validated rules for when to obtain a head CT scan after traumatic brain injury 81.
Computed tomography (CT) is the most common imaging technology used to assess people with suspected moderate to severe traumatic brain injury. CT scans create a series of cross-sectional x-ray images of the skull and brain and can show fractures, hemorrhage, hematomas, hydrocephalus, contusions, and brain tissue swelling. CT scans are often used to assess the damage of a traumatic brain injury in emergency room settings.
Magnetic resonance imaging (MRI) may be used after the initial assessment and treatment as it is a more sensitive test and picks up subtle changes in the brain that the CT scan might have missed.
Unlike moderate or severe traumatic brain injury, milder traumatic brain injury may not involve obvious signs of damage (hematomas, skull fracture, or contusion) that can be identified with current neuroimaging. Instead, much of what is believed to occur to the brain following mild traumatic brain injury happens at the cellular level. Significant advances have been made in the last decade to image milder traumatic brain injury damage. For example, diffusion tensor imaging (DTI) can image white matter tracts, more sensitive tests like fluid-attenuated inversion recovery (FLAIR) can detect small areas of damage, and susceptibility-weighted imaging very sensitively identifies bleeding. Despite these improvements, currently available imaging technologies, blood tests, and other measures remain inadequate for detecting these changes in a way that is helpful for diagnosing the mild concussive injuries.
Neuropsychological tests to gauge brain functioning are often used in conjunction with imaging in people who have suffered mild traumatic brain injury. Such tests involve performing specific cognitive tasks that help assess memory, concentration, information processing, executive functioning, reaction time, and problem solving.
Cognition and Neuropsychological Tests
- Cognition describes the processes of thinking, reasoning, problem solving, information processing, and memory.
- Most patients with severe traumatic brain injury suffer from cognitive disabilities, including the loss of many higher level mental skills.
- Neuropsychological assessments are often used to obtain information about cognitive capabilities.
- These tests are specialized task-oriented evaluations of human brain-behavior relationships, evaluating higher cognitive functioning as well as basic sensory-motor processes 82.
- Testing by a neuropsychologist can assess the individual’s cognitive, language, behavioral, motor, and executive functions and provide information regarding the need for rehabilitative services 77.
- For this assessment, a neuropsychologist reviews the case history and hospital records of the patient, and interviews the patient and his/her family.
- The neuropsychologist acquires information about the “person” the individual was before the injury, based on aspects like school performance, habits, and lifestyle, in order to detail which abilities remain unchanged as well as areas of the brain that are adversely affected by the injury and how the injury is expected to impact the individual’s life 82.
Intracranial pressure (ICP) monitoring. Sometimes, swelling of the brain from a traumatic brain injury can increase pressure inside the skull. The pressure can cause additional damage to the brain. A health care provider may insert a probe through the skull to monitor this swelling.2 In some cases, a shunt or drain is placed into the skull to relieve ICP.
Brain contusion treatment
The types and extent of treatments depend on the severity of the injury and its specific location in the brain.
Treatment for Mild traumatic brain injury
Mild traumatic brain injury, sometimes called concussion, may not require specific treatment other than rest. However, it is very important to follow a health care provider’s instructions for complete rest and gradual return to normal activities after a mild traumatic brain injury. If a person resumes normal activities and starts experiencing traumatic brain injury symptoms, the healing and recovery process may take much longer than if he or she had followed the health provider’s instructions. Certain activities, like working on a computer and concentrating hard, can tire the brain even though they are not physically demanding. The person with the concussion might need to reduce these kinds of activities or might need to rest between periods of such activities to let the brain rest. In addition, alcohol and other drugs can slow recovery and increase the chances of re-injury 83.
Children and teens who may have sustained a concussion during sports should stop playing immediately. They should not return to play until a health care provider who is experienced in evaluating concussion confirms they are ready. Re-injury during recovery can slow healing and increase the chances of long-term problems. On rare occasions in which a person gets another concussion before healing from the first one, permanent brain damage and even death may result 84.
Emergency Treatment for traumatic brain injury
In most cases, emergency care focuses on stabilizing the patient and promoting survival. This care may include ensuring adequate oxygen flow to the brain, controlling blood pressure, and preventing further injury to the head or neck 77. Once the patient is stable, other types of care for traumatic brain injury and its effects can begin.
Surgery may be needed as part of emergency care to reduce additional damage to the brain tissues. Surgery may include:
- Removing clotted blood. Bleeding in the brain or between the brain and skull can lead to large areas of clotted blood, sometimes called hematomas, that put pressure on the brain and damage brain tissues 77.
- Repairing skull fractures. Setting severe skull fractures or removing pieces of skull or other debris from the brain can help start the healing process of the skull and surrounding tissues 85.
- Relieving pressure in the skull. Making a hole in the skull or adding a shunt or drain can relieve pressure inside the skull and allow excess fluid to drain 86.
Medications
Medications may be used to treat symptoms of traumatic brain injury and to lower some of the risks associated with it. These medications may include, but are not limited to:
- Anti-anxiety medication to lessen feelings of nervousness and fear
- Anticoagulants to prevent blood clots
- Anticonvulsants to prevent seizures
- Antidepressants to treat symptoms of depression and mood instability
- Muscle relaxants to reduce muscle spasms
- Stimulants to increase alertness and attention6
Researchers continue to explore medications that may aid recovery from traumatic brain injury. A study 87 investigated the effectiveness of citicoline, a drug meant to help protect neurological functioning. The study found, however, that patients with traumatic brain injury who took citicoline did not have any greater improvement in function than those who took a placebo.
Rehabilitation therapies
Therapies can help someone with traumatic brain injury relearn skills such as walking or cooking, or develop strategies for self-care, such as making lists of the steps involved in getting dressed. Rehabilitation can include several different kinds of therapy for physical, emotional, and cognitive difficulties. Depending on the injury, these treatments may be needed only briefly after the injury, occasionally throughout a person’s life, or on an ongoing basis.
Types of therapies for traumatic brain injury
Most people with a moderate to severe brain injury will need some type of rehabilitation therapy to address physical, emotional, and cognitive issues from the traumatic brain injury. Therapies will likely include relearning old skills or learning new ways to make up for lost skills. A treatment program should be designed to meet each person’s specific needs and to strengthen his or her ability to function at home and in the community 88.
Therapy usually begins in the hospital and can continue in a number of possible settings, including in a skilled nursing facility, at home, in a school, and in an outpatient program at a clinic. Therapy can be brief or long-term, depending on the type of injury, and it may need to change over time. Rehabilitation generally involves a number of health care specialists, the person’s family, and a person who manages the team.8 When devising a long-term treatment plan, patients, their families, and their providers should be aware that moderate and severe traumatic brain injury impairs patients’ ability to make sound medical decisions even a month after injury 89.
Types of rehabilitation therapy may include:
- Physical therapy. This treatment works to build physical strength, coordination, and flexibility.
- Occupational therapy. An occupational therapist helps a person learn or relearn how to perform daily tasks, such as getting dressed, cooking, and bathing.
- Speech therapy. This therapy works on the ability to form words and other communication skills as well as how to use special communication devices if necessary. Speech therapy can also include evaluation and treatment of swallowing disorders (dysphagia).
- Psychological counseling. A counselor can help a person learn coping skills, work on relationships, and improve general emotional well-being.
- Vocational counseling. This type of rehabilitation focuses on a person’s ability to return to work, find appropriate opportunities, and deal with workplace challenges.
- Cognitive therapy. This includes activities designed to improve memory, attention, perception, learning, planning, and judgment. For many people with traumatic brain injury, cognitive therapy is among the most common types of rehabilitation.
Brain contusion prognosis
The effects of traumatic brain injury range in duration and seriousness, depending on the extent of the injury and its location 77. According to the Centers for Disease Control and Prevention, almost one-half of those hospitalized after a traumatic brain injury have a related disability one year after the injury 90.
Immediate problems
Sometimes, a person will have medical complications as a result of traumatic brain injury, and the risk of these problems increases with the severity of the injury. Some complications of traumatic brain injury include seizures, nerve damage, blood clots, contraction of a blood vessel, stroke, coma, and infections in the brain.1 The risks of many of these problems decrease as more time passes from the initial traumatic brain injury and as the person’s condition stabilizes.
Longer-term Effects of traumatic brain injury
Traumatic brain injury may cause problems with various brain functions. The types and extent of these problems depend on where the brain was injured.
Possible problems from traumatic brain injury include:
- Cognition, such as difficulty learning, remembering, making decisions, and reasoning
- Senses, such as double vision, a consistent bitter taste in the mouth or a loss of the sense of taste, ringing in the ears, and tingling or pain
- Communication, such as trouble talking, reading, writing, and explaining feelings or thoughts
- Behavior, including difficulty with social situations, relationships, and self-control, or aggression
- Emotions, including depression, anxiety, mood swings, and irritability 77.
Degenerative effects of traumatic brain injury
Research suggests that having one or more traumatic brain injurys may increase the risk of diseases that cause the degeneration, or break down, of brain cells. Some evidence indicates that traumatic brain injury is associated with:
- Alzheimer’s disease, which impairs memory, emotions, and thinking skills
- Parkinson’s disease, which causes the loss of motor skills and control over motor skills
- Chronic traumatic encephalopathy, which often affects athletes involved in sports with head impacts, including boxing, football, and hockey, and causes problems with memory, thinking, and motor skills 77.
Hip contusion
Hip contusion also called hip pointer is a contusion to the iliac crest, the surrounding soft-tissue structures and/or the greater trochanter of the femur following a direct impact or collision that causes a contusion or subperiosteal hematoma 91. Typically, the injury is caused by a direct blow or fall 92. Hip contusion occurs most commonly in contact sports (eg, football, hockey) 93, but they can also occur in noncontact sports (eg, volleyball) as a result of a fall onto the hip or side. Pain and tenderness in this region can limit an athlete’s participation in sports.
A hip pointer is usually caused by a direct blow or from a fall striking the iliac crest or greater trochanter. The typical hip contusion injury is characterized by localized pain and severe palpable tenderness along a variable distance of the iliac crest 94. Athletes can often return to the field of play, and in professional sports their pain can be controlled with local anesthetic injection. These athletes usually recover in 1 to 3 weeks 94.
The assessment of routine hip pointers usually does not involve radiological investigation, and most of these injuries are managed clinically 93. The athlete’s symptoms and clinical signs are well localized to the iliac crest. It is common practice in professional athletes to treat pain with a guided or unguided local anesthetic injection to enable them to return to play on the same day or subsequent days to weeks. Although uncommon, iliac crest fractures can occur in collision sports, and an inability to return to play after a local anesthetic injection would warrant radiography to rule out a fracture.
The management of hip contusion or hip pointer injuries requires coordinated care between athletic trainers, clinical providers, and primary care and sports medicine specialists. The majority of hip pointer injuries improve with standard, first-line nonoperative management modalities.
Injuries to the hip and pelvis in sports are much less common compared to injuries about the knee and/or ankle 95. Hip injuries comprise 5 to 10% of athletic injuries, and hip pointers comprise an even smaller relative subset percentage of these hip injuries. A review of injuries in the National Football League from 1997 to 2006 reported an incidence of 0.3%, with an average of 5.6 days of training lost due to injury 96.
Figure 2. Hip pointer injury (bruising on the left anterolateral abdominal wall on day 3 post injury)

Hip contusion causes
The anterior iliac crest region and greater trochanter of the femur have, in most patients, minimal overlying fatty tissue and thus these areas are more susceptible to injury from direct trauma 97.
The primary cause of hip pointer is a direct blow to the iliac crest or greater trochanter during contact sports. American football and hockey are the most common sports that result in these injuries 97. The former implicates tackling and incidental collisions that regularly occur during competition. The same underlying mechanism can be said for rugby as well. In ice hockey, hip pointers can result from being checked into the boards or by contact with another player or player’s equipment 98. Other non-contact sports or high- versus low-energy traumatic mechanisms can also cause iliac crest contusions. In this scenario, a direct fall or a direct traumatic blow (i.e., secondary to a motor vehicle collision) is often the precipitating factor 99.
Following direct impact to the iliac crest, an ensuing hematoma develops around the area and often includes varying degrees of bleeding into the hip abductor musculature. The iliac crest is the origin of several muscles which can be affected depending on the degree and extent of the zone of injury 100:
- Sartorius
- Gluteus medius
- Tensor fascia lata
- Abdominal musculature – Transverse or oblique muscles
Hip contusion symptoms
Most commonly, patients present with varying degrees of bruising (ecchymoses) or contusion around the area of impact. The patient will be tender directly over these areas, and often range of motion (ROM) about the hip is limited secondary to pain. The hip abductors are typically weak, while the motor strength of the hip flexor and extensors should be intact. Hip abductors and external rotators may exhibit limited strength secondary to pain.
Hip contusion complications
- Chronic pain/dysfunction
- Inability to return to prior athletic performance
- Missed diagnosis leading to persistent pain/disability
Hip contusion diagnosis
A useful clinical test, not only to initially diagnose the hip pointer injury but also to track recovery, is the “resisted oblique sit-up test”; this maneuver entails stressing the involved anterolateral abdominal and assessing pain and strength, while palpating for a palpable defect or tenderness (Figure 3).
Figure 3. Resisted oblique sit-up test

Radiographs are needed if a fracture or myositis ossificans is suspected. Hip pointer injuries are an important consideration for high school and college athletes because the ischial tuberosity and anterior superior iliac spine may fuse as late as the 3rd decade of life. Pediatric and adolescent athletes should be evaluated to rule out potential pelvic avulsion injuries including 98:
- Iliac crest avulsion injuries secondary to abdominal musculature avulsions
- Anterior superior iliac spine (ASIS) avulsion injuries sartorius and/or tensor fascia lata avulsion(s)
- Anterior inferior iliac spine (AIIS) avulsion injuries rectus femoris avulsion injury
- Ischial tuberosity proximal hamstring avulsion injuries
Otherwise, radiographs obtained in the setting of a true, isolated, iliac crest contusion (hip pointer injury), radiographs are unremarkable.
Consider CT scans if the patient has continued pain or the pain exceeds that expected from examination findings. A bone scan can exclude stress fractures if initial symptoms do not resolve. An MRI obtained in the setting of an isolated iliac crest contusion would likely reveal a large hematoma but is otherwise unremarkable.
A hip pointer must be distinguished from chronic exertional compartment syndrome, a femoral neck fracture, avascular necrosis, hip fracture or dislocation, tendonitis, iliotibial band syndrome, osteitis pubis, sacroiliac joint injury, snapping hip syndrome, and slipped capital femoral epiphysis.
Hip contusion treatment
The initial therapy of a hip pointer injury includes ice, anti-inflammatory pain medication, compression, rest, and avoidance of weight bearing as guided by the patient’s reported symptoms 97. As the pain decreases, the initiation of range of motion and active resistance exercises should begin. If a hematoma is present, aspiration can provide some pain relief and may potentially mitigate the risks of developing myositis ossificans. A local anesthetic such as 1% to 2% lidocaine or 0.5% bupivacaine (5mL to 9 mL), may provide short-term pain relief. It is considered safe, but little data support this practice. Even though there are no studies supporting corticosteroids, it is an accepted practice in the sports medicine community. If compartment syndrome is suspected, measure compartment pressures and consult an orthopedic surgeon or sports medicine specialist. An orthopedic surgeon should also be consulted if there is an avulsion fracture or for pain lasting longer than two weeks.
Physical therapy is often prescribed. Graded strengthening program for lumbopelvic region, initially focusing on isometric co-contractions and progressing to more challenging exercises involving planking and side planking to strengthen and remodel the damaged anterolateral abdominal wall 94. In the later stages of the rehabilitation, perform dynamic strengthening of the thoracolumbar region, using gym equipment (free weights, pulleys, and clinical Pilates) 94.
Hip contusion recovery time
Most patients can gradually return to normal levels of activity within two to three weeks 97.
Padding at the injury site may decrease the incidence of re-injury, limit pain, and allow a return to activity sooner. Patients with a hip pointer may return to activity once the pain and swelling resolve, and normal function returns. Patients with a hip pointer are at risk for recurrent injury and should be advised to avoid activities that may induce a repeat injury.
References- Teli M, de Roeck N, Horowitz MD, Saifuddin A, Green R, Noordeen H. Radiographic outcome of vertebral bone bruise associated with fracture of the thoracic and lumbar spine in adults. European Spine Journal. 2005;14(6):541-545. doi:10.1007/s00586-004-0786-1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3489230/
- MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K, Guermazi A. Osteoarthritis Cartilage. 2009 Sep; 17(9):1115-31.
- Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. Yamamoto T, Bullough PG. J Bone Joint Surg Am. 2000 Jun; 82(6):858-66.
- Costa-Paz M, Musculo DL, Ayerza M et al (2001) ‘Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures’ Arthroscopy17: 445-449.
- V. Mandalia, J.H.L. Henson. Traumatic bone bruising – A review article, European Journal of Radiology 2008; 67; 54–61
- V. Mandalia, A.J.B. Fogg, R. Chari, J. Murray, A. Beale, J.H.L. Henson. Bone bruising of the knee. Clinical Radiology 2005; 60, 627–636.
- Johnson DL, Bealle DP, Brand JC et al. The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med. 2000 Mar;28(2):152-5.
- Graf BK, Cook DA, De Smet AA et al. “Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med 1993; 21(2):220-3.
- Vellet AD, Marks PH, Fowler PJ et al. Occult post-traumatic osteochondral lesions: Prevalence, classification and short-term sequelae evaluated with MR imaging. Radiology 1991; 178:271-6.
- Coen MJ, Caborn DN, Johnson DL. The Dimpling phenomenon: articular cartilage injury overlying an occult osteochondral lesion at the time of anterior cruciate ligament reconstruction. Arthroscopy 1996 Aug;12(4):502-5.
- Speer KP, Warren RF, Wickiewicz TL et al. Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med 1995; 23(1):77-81.
- Spindler KP, Schils JP, Bergfeld JA et al. Prospective study of osseous, articular and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med 1993; 21(4):551-6.
- Speer KP, Warren RF, Wickiewicz TL et al. Observations on the injury mechanism of anterior cruciate ligament (ACL) tears in skiers. Am J Sports Med 1995; 23(1):77-81.
- Johnson D, Urban WP, Caborn DNM et al. Articular cartilage changes seen with magnetic resonance imaging detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med 1998; 26(3):409-14.
- Fang C, Johnson D, Leslie MP et al. Tissue distribution and measurement of cartilage oligomeric matrix protein in patients with magnetic resonance imaging-detected bone bruises after acute anterior cruciate ligament tears. J Orthop Res. 2001 Jul;19(4):634-41.
- Rangger C, Kathrein A, Freund MC et al. Bone bruise of the knee: histology and cryosections in 5 cases. Acta Orthop Scand. 1998 Jun;69(3):291-4.
- Thompson RC Jr, Oegema TR Jr, Lewis JL et al. Osteoarthritic changes after acute transarticular load. J Bone Joint Surg 1991; 73A:990-1001.
- Sybrandy KC, Cramer MJ, Burgersdijk C. Diagnosing cardiac contusion: old wisdom and new insights. Heart. 2003;89(5):485–489. doi:10.1136/heart.89.5.485 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767619
- Determining which patients require evaluation for blunt cardiac injury following blunt chest trauma. Nagy KK, Krosner SM, Roberts RR, Joseph KT, Smith RF, Barrett J. World J Surg. 2001 Jan; 25(1):108-11.
- The usefulness of serum troponin levels in evaluating cardiac injury. Collins JN, Cole FJ, Weireter LJ, Riblet JL, Britt LD. Am Surg. 2001 Sep; 67(9):821-5; discussion 825-6.
- Clinically significant blunt cardiac trauma: role of serum troponin levels combined with electrocardiographic findings. Salim A, Velmahos GC, Jindal A, Chan L, Vassiliu P, Belzberg H, Asensio J, Demetriades D. J Trauma. 2001 Feb; 50(2):237-43.
- Ventricular aneurysm due to blunt chest injury. Grieco JG, Montoya A, Sullivan HJ, Bakhos M, Foy BK, Blakeman B, Pifarré R. Ann Thorac Surg. 1989 Feb; 47(2):322-9.
- [Unexplained right ventricle dilatation clarified by a cardiac contusion many years ago]. Sybrandy KC, Oosterom L, Burgersdijk C, van der Zant F. Ned Tijdschr Geneeskd. 2001 Dec 15; 145(50):2443-6.
- Ganie FA, Lone H, Lone GN, et al. Lung Contusion: A Clinico-Pathological Entity with Unpredictable Clinical Course. Bull Emerg Trauma. 2013;1(1):7–16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771236
- Early and late acute respiratory distress syndrome: two distinct clinical entities. Croce MA, Fabian TC, Davis KA, Gavin TJ. J Trauma. 1999 Mar; 46(3):361-6; discussion 366-8.
- Risk factors for early onset pneumonia in trauma patients. Antonelli M, Moro ML, Capelli O, De Blasi RA, D’Errico RR, Conti G, Bufi M, Gasparetto A. Chest. 1994 Jan; 105(1):224-8.
- Outcome of isolated pulmonary contusion in blunt trauma patients. Hoff SJ, Shotts SD, Eddy VA, Morris JA Jr. Am Surg. 1994 Feb; 60(2):138-42.
- Pathophysiology of pulmonary contusion in dogs. Oppenheimer L, Craven KD, Forkert L, Wood LD. J Appl Physiol Respir Environ Exerc Physiol. 1979 Oct; 47(4):718-28.
- Physiopathology of crushed chest injuries. Garzon AA, Seltzer B, Karlson KE. Ann Surg. 1968 Jul; 168(1):128-36.
- Yamamoto L, Schroeder C, Morley D, Beliveau C. Thoracic trauma: The deadly dozen. Crit Care Nurs Q. 2005;28(1):22–40.
- Moloney JT, Fowler SJ, Chang W. Anesthetic management of thoracic trauma. Curr Opin Anaesthesiol. 2008;21(1):41–6.
- Hwang JCF, Hanowell LH, Grande CM. 7 Peri-operative concerns in thoracic trauma. Baillière’s Clinical Anaesthesiology. 1996;10(1):123–53.
- Cohn SM, Zieg PM. Experimental pulmonary contusion: review of the literature and description of a new porcine model. J Trauma. 1996;41(3):565–71.
- Cohn SM. Pulmonary contusion: Review of the clinical entity. J Trauma. 1997;42(5):973–79.
- Livingston DH, Hauser CJ, Moore EE, Feliciano DV, Mattox KL. Trauma. McGraw-Hill Professional; 2003. Trauma to the chest wall; pp. 525–528.
- Gavelli G, Canini R, Bertaccini P, Battista G, Bnà C, Fattori R. Traumatic injuries: Imaging of thoracic injuries. Eur Radiol. 2002;12(6):1273–94.
- Sattler S, Maier RV, Karmy-Jones R, Nathens A, Stern EJ. Thoracic Trauma and Critical Care. Berlin: Springer; 2002. Pulmonary contusion; pp. 159–160.
- Bailey BJ, Johnson JT, Newlands SD. Head and Neck Surgery–Otolaryngology. Hagerstown, MD: Lippincott Williams & Wilkins; 2006. p. 929.
- Miller DL, Mansour KA. Blunt traumatic lung injuries. Thorac Surg Clin. 2007;17(1):57–61.
- Cullen ML. Pulmonary and respiratory complications of pediatric trauma. Respir Care Clin N Am. 2001;7(1):59–77.
- Cooper GJ. Protection of the lung from blast overpressure by thoracic stress wave decouplers. J Trauma. 1996;40(3 Suppl):S105–10.
- Wanek S, Mayberry JC. Blunt thoracic trauma: Flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20(1):71–81.
- Mick NW, Peters JR, Egan D, Nadel ES. Blueprints Emergency Medicine. 2nd edition. Philadelphia: Lippincott Williams & Wilkins; 2006. Chest trauma; p. 76.
- Cohn SM, Dubose JJ. Pulmonary contusion: an update on recent advances in clinical management. World J Surg. 2010;34(8):1959–70.
- Tovar JA. The lung and pediatric trauma. Semin Pediatr Surg. 2008;17(1):53–9.
- Ullman EA, Donley LP, Brady WJ. Pulmonary trauma emergency department evaluation and management. Emerg Med Clin North Am. 2003;21(2):291–313.
- Keough V, Pudelek B. Blunt chest trauma: Review of selected pulmonary injuries focusing on pulmonary contusion. AACN Clin Issues. 2001;12(2):270–81.
- Klein Y, Cohn SM, Proctor KG. Lung contusion: Pathophysiology and management. Current Opinion in Anaesthesiology. 2002;15(1):65–68.
- Johnson SB. Tracheobronchial injury. Semin Thorac Cardiovasc Surg. 2008;20(1):52–7.
- Stern EJ, White C. Chest Radiology Companion. Hagerstown: Lippincott Williams & Wilkins; 1999. p.
- Boyd AD, Hood RM, Boyd AD, Culliford AT. Thoracic Trauma. Philadelphia: Saunders; 1989. Lung injuries; pp. 153–155.
- Wiot JF. The radiologic manifestations of blunt chest trauma. JAMA. 1975;231(5):500–3.
- Deunk J, Poels TC, Brink M, Dekker HM, Kool DR, Blickman JG, et al. The clinical outcome of occult pulmonary contusion on multidetector-row computed tomography in blunt trauma patients. J Trauma. 2010;68(2):387–94.
- Soldati G, Testa A, Silva FR, Carbone L, Portale G, Silveri NG. Chest ultrasonography in lung contusion. Chest. 2006;130(2):533–8.
- Hyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, et al. Diagnostic accuracy of ultrasonography in the acute assessement of common thoracic lesions after trauma. Chest. 2012;141(5):1177–83.
- Rocco M, Carbone I, Morelli A, Bertoletti L, Rossi S, Vitale M, et al. Diagnostic accuracy of bedside ultrasonography in the ICU: feasibility of detecting pulmonary effusion and lung contusion in patients on respiratory support after severe blunt thoracict rauma. Acta Anaesthesiol Scand. 2008;52(6):776–84.
- Soldati G, Copetti R, Sher S. Sonographic interstitial syndrome: the sound of lung water. J Ultrasound Med. 2009;28(2):163–74.
- Raghavendran K, Davidson BA, Woytash JA, Helinski JD, Marschke CJ, Manderscheid PA, et al. The evolution of isolated, bilateral lung contusion from blunt chest trauma in rats: cellular and cytokine responses. Shock. 2005;24(2):132–8.
- Sutyak JP, Wohltmann CD, Larson J. Pulmonary contusions and critical care management in thoracic trauma. Thorac Surg Clin. 2007;17(1):11–23.
- Lucid WA, Taylor TB, Strange GR. Pediatric Emergency Medicine: A Comprehensive Study Guide. New York: McGraw-Hill; 2002. Thoracic trauma; pp. 92–100.
- Pettiford BL, Luketich JD, Landreneau RJ. The management of flail chest. Thorac Surg Clin. 2007;17(1):25–33.
- Dueck R. Alveolar recruitment versus hyperinflation: A balancing act. Curr Opin Anaesthesiol. 2006;19(6):650–4.
- Anantham D, Jagadesan R, Tiew PE. Clinical review: Independent lung ventilation in critical care. Crit Care. 2005;9(6):594–600.
- Ciesla ND. Chest physical therapy for patients in the intensive care unit. Phys Ther. 1996;76(6):609–25.
- Yalçinkaya I, Sayir F, Kurnaz M, Cobanoğlu U. Chest Trauma: Analysis of 126 Cases. Ulus Travma Derg. 2000;6(4):288–91.
- Smith M, Ball V. Thoracic trauma. Cardiovascular/Respiratory Physiotherapy. St. Louis: Mosby; 221.
- Trinkle JK, Furman RW, Hinshaw MA, Bryant LR, Griffen WO. Pulmonary contusion. Pathogenesis and effect of various resuscitative measures. Ann Thorac Surg. 1973;16(6):568–73.
- Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2004.
- Mutch CA, Talbott JF, Gean A. Imaging Evaluation of Acute Traumatic Brain Injury. Neurosurg Clin N Am. 2016 Oct. 27 (4):409-39.
- Brommeland T, Helseth E, Aarhus M, Moen KG, Dyrskog S, Bergholt B, Olivecrona Z, Jeppesen E. Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med. 2018 Oct 29;26(1):90.
- Shaikh F, Waseem M. Head Trauma. [Updated 2018 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430854
- Portaro S, Naro A, Cimino V, Maresca G, Corallo F, Morabito R, Calabrò RS. Risk factors of transient global amnesia: Three case reports. Medicine (Baltimore). 2018 Oct;97(41):e12723.
- Traumatic Brain Injury & Concussion Prevention. https://www.cdc.gov/traumaticbraininjury/prevention.html
- Preventing Abusive Head Trauma in Children. https://www.cdc.gov/violenceprevention/childabuseandneglect/Abusive-Head-Trauma.html
- Traumatic Brain Injury Information Page. https://www.ninds.nih.gov/disorders/all-disorders/traumatic-brain-injury-information-page
- Symptoms of Traumatic Brain Injury (TBI). https://www.cdc.gov/traumaticbraininjury/symptoms.html
- Traumatic Brain Injury: Hope Through Research. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Traumatic-Brain-Injury-Hope-Through
- About Brain Injury. https://www.biausa.org/brain-injury/about-brain-injury
- Duhaime, A. C., Beckwith, J. G., Maerlender, A. C., McAllister, T. W., Crisco, J. J., Duma, S. M., Brolinson, P. G., Rowson, S., Flashman, L. A., Chu, J. J., & Greenwald, R. M. (2012). Spectrum of acute clinical characteristics of diagnosed concussions in college athletes wearing instrumented helmets: clinical article. Journal of Neurosurgery, 117, 1092–1099.
- Centers for Disease Control and Prevention. Glasgow Coma Scale. Atlanta, GA: U.S. Department of Health and Human Services. https://www.cdc.gov/masstrauma/resources/gcs.pdf
- Pavlović T, Milošević M, Trtica S, Budinčević H. Value of Head CT Scan in the Emergency Department in Patients with Vertigo without Focal Neurological Abnormalities. Open Access Maced J Med Sci. 2018 Sep 25;6(9):1664-1667.
- Brain Injury Diagnosis. https://www.biausa.org/brain-injury/about-brain-injury/diagnosis
- Recovery from Concussion. https://www.cdc.gov/headsup/basics/concussion_recovery.html
- Responding to a Concussion and Action Plan for Coaches. https://www.cdc.gov/headsup/basics/concussion_respondingto.html
- Traumatic Brain Injury. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Traumatic-Brain-Injury
- Subdural hematoma. https://medlineplus.gov/ency/article/000713.htm
- Zafonte, R. D., Bagiella, E., Ansel, B. M., Novack, T. A., Friedewald, W. T., Hesdorffer, D. C., Timmons, S. D., Jallo, J., Eisenberg, H., Hart, T., Ricker, J. H., Diaz-Arrastia, R., Merchant, R. E., Temkin, N. R., Melton, S., & Dikmen, S. S. (2012). Effect of citicoline on functional and cognitive status among patients with traumatic brain injury: Citicoline Brain Injury Treatment Trial (COBRIT). Journal of the American Medical Association, 308, 1993–2000.
- NIH Consensus Development Conference on Rehabilitation of Persons with Traumatic Brain Injury. https://www.nichd.nih.gov/publications/pubs/TBI_1999/NIH_Consensus_Statement
- Triebel, K. L., Martin, R. C., Novack, T. A., Dreer, L., Turner, C., Pritchard, P. R., Raman, R., & Marson, D. C. (2012). Treatment consent capacity in patients with traumatic brain injury across a range of injury severity. Neurology, 2012 DOI: 10.1212/WNL.0b013e3182553c38
- Severe TBI. https://www.cdc.gov/traumaticbraininjury/severe.html
- Blazina ME. The “hip-pointer,” a term to describe a specific kind of athletic injury. Calif Med. 1967;106(6):450
- Hall M, Anderson J. Hip pointers. Clin Sports Med. 2013 Apr. 32(2):325-30.
- Hall M, Anderson J. Hip pointers. Clin Sports Med. 2013;32(2):325–330.
- Gultekin S, Cross T. The Franklin-Naismith Lesion: A Severe Variant of Hip Pointer. Orthop J Sports Med. 2019;7(1):2325967118820507. Published 2019 Jan 9. doi:10.1177/2325967118820507 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6329028/
- Bordoni B, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Dec 15, 2018. Anatomy, Bony Pelvis and Lower Limb, Thigh Quadriceps Muscle.
- Feeley BT, Powell JW, Muller MS, Barnes RP, Warren RF, Kelly BT. Hip injuries and labral tears in the national football league. Am J Sports Med. 2008 Nov;36(11):2187-95.
- Varacallo M, Bordoni B. Hip Pointer Injuries (Iliac Crest Contusions) [Updated 2019 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538258
- Bordoni B, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Dec 15, 2018. Anatomy, Bony Pelvis and Lower Limb, Thigh Quadriceps Muscle
- Smith JM, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 19, 2019. Osgood Schlatter’s Disease [Tibial Tubercle Apophysitis]
- Walters BB, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 14, 2018. Anatomy, Bony Pelvis and Lower Limb, Thigh Sartorius Muscle.





