Perilymph fistula
Perilymph fistula also known as perilymphatic fistula or labyrinthine fistula, is an abnormal communication (a tear or defect) between the fluid-filled perilymphatic space of the inner ear and the air-filled space of the middle ear, most commonly occurring at either the round window or oval window 1. This small opening (fistula) allows perilymph (fluid) to leak into the middle ear. Perilymph fistula symptoms are sudden or progressive fluctuating sensorineural hearing loss and vertigo. Other symptoms that may be present include tinnitus, disequilibrium, and aural fullness 2.
Changes in air pressure that occur in the middle ear (for example, when your ears “pop” in an airplane) normally do not affect your inner ear. However, when a fistula is present, changes in middle ear pressure will directly affect the inner ear, stimulating the balance and/or hearing structures within and causing perilymph fistula symptoms.
The perilymphatic space of the inner ear is connected to the cerebrospinal fluid (CSF) that surrounds the brain. Perilymphatic fluid, which is high in sodium (Na+), is similar in composition to CSF. When an abnormal connection between the membranes between the middle and inner ear exists, perilymph in the inner ear escapes, driven by the hydrostatic pressure of the CSF (cerebrospinal fluid), and is replaced by CSF. This can also result in lower than normal levels of CSF fluid around the brain and spinal cord, which may result in symptoms such as mild headache.
Patients with perilymph fistula often feel frustrated and depressed because, while they don’t feel well, they look fine to others. perilymph fistula patients specifically and vestibular patients in general often have a challenging time explaining to friends and family what they are going through. Sometimes it is enough to ask your support network for patience and understanding while you explore diagnosis and treatment options and learn to cope with the symptoms brought on by persistent dizziness.
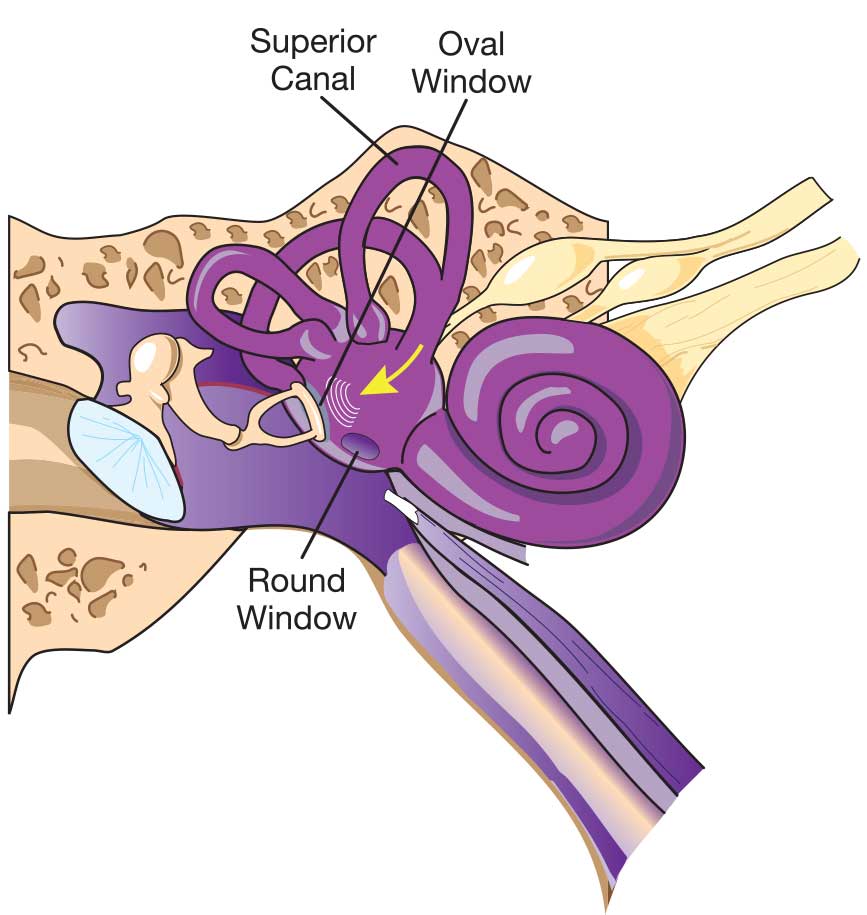
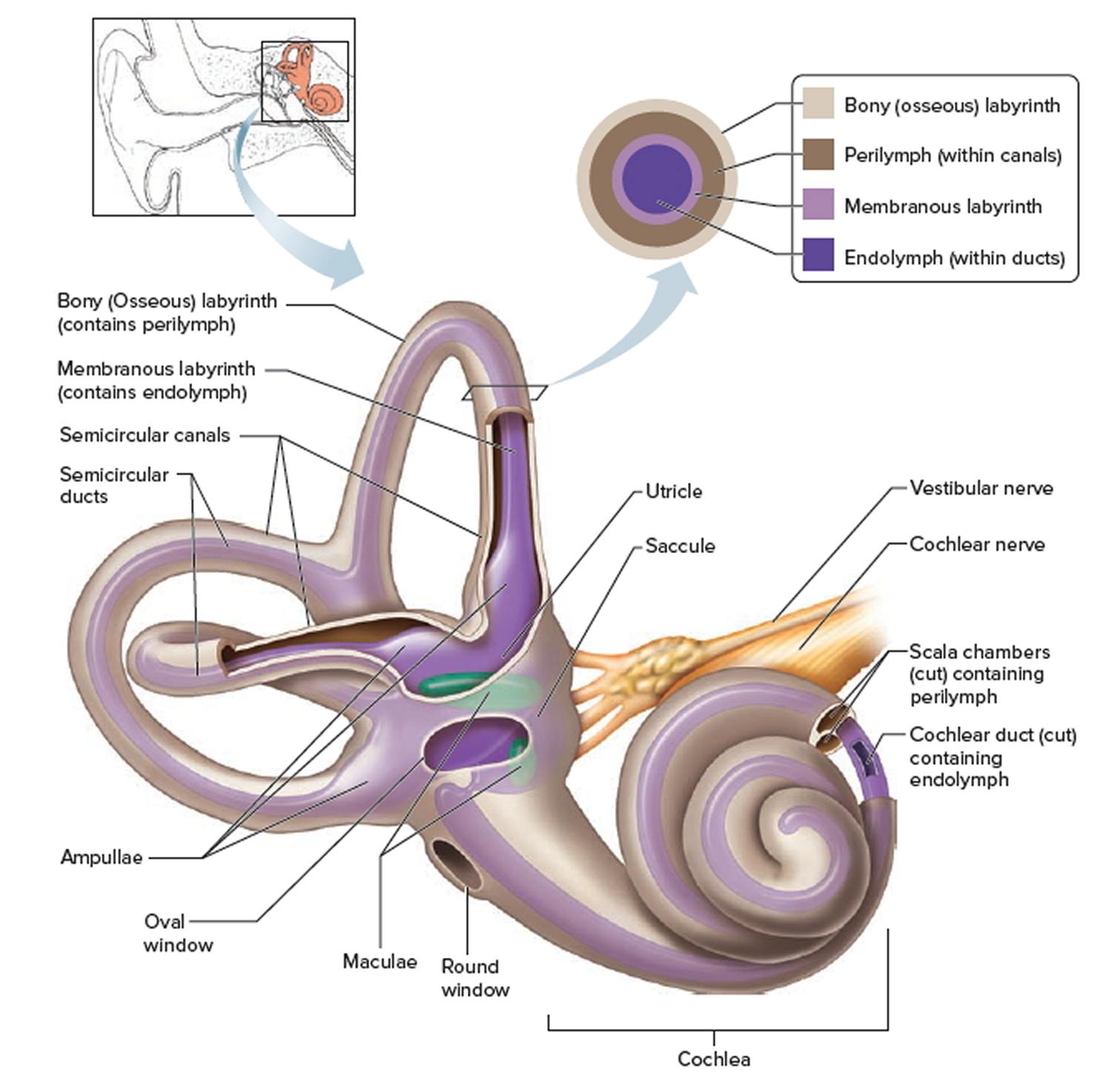
Figure 1. Inner ear anatomy
Figure 2. Inner ear bones
Perilymph fistula causes
Head trauma is the most common cause of perilymph fistulas, usually involving a direct blow to the head or in some cases a “whiplash” injury. Other common causes include ear trauma, objects perforating the eardrum, or “ear block” on descent of an airplane or scuba diving. Perilymph fistulas may also develop after rapid increases in intracranial pressure, such as may occur with weightlifting or childbirth.
Perilymph fistulas are infrequently present from birth. A long-running controversy has surrounded the idea of a “spontaneous perilymph fistula.” Instead, what may occur is that a patient has a causative event but does not see an ear specialist right away. The passage of time blurs the memory of such an event so that the perilymph fistula might seem to have been spontaneous. Rarely, perilymph fistula’s occur in both ears, and only after a severe head injury.
Perilymph fistula symptoms
The symptoms of a perilymph fistula most commonly include ear fullness, fluctuating or “sensitive” hearing, dizziness without true vertigo (spinning), and motion intolerance. Vertigo or sudden hearing loss can occur from a perilymph fistula. Most people with fistulas find that their symptoms get worse with changes in altitude (fast elevators, airplanes, and travel over mountain passes) or increased CSF pressure resulting from heavy lifting, bending over, and coughing or sneezing.
Perilymph fistula diagnosis
There is no positive way to diagnosis a perilymph fistula. For many years it was thought that it could be confirmed by performing a tympanotomy (surgical exploration of the middle ear) and directly viewing the area of the suspected fistula to detect a fluid leak. However, since the leak would be only a few microliters of clear fluid, visual detection has been found to be virtually impossible. Larger amounts of fluid leakage may indicate a CSF leak due to a congenital defect in the inner ear.
A physician can arrive at a presumptive diagnosis through a thorough probing for events close in time to the onset of symptoms, along with a variety of tests. These tests can include hearing tests (audiogram, ECOG), balance tests (VNG, VEMP) and some form of a “fistula test.”
Historically, a platform pressure test developed by Dr. F. Owen Black was seen to be the most reliable test to determine if a perilymph fistula was present. However, this equipment is no longer in production, and only a small number still exist today.
In the end, a physician has to present the possibility of a perilymph fistula to the patient based on history, test results, and the lack of spontaneous resolution of symptoms. Together the physician and patient (or guardian) must decide whether to undertake an operation to patch the oval and round window areas. Immediately following surgery there is a period of bed rest, followed by a period of restricted activity. Four to six weeks later a reassessment of the patient‘s symptoms is done to determine if the patching successfully corrected the perilymph fistula.
Perilymph fistula test
There is no diagnostic test can be considered a criterion standard for perilymph fistula, and none are immediately useful.
The current criterion standard for confirmation of perilymph fistula is direct visualization either by operative middle ear exploration or by in-office endoscopy. The subjectivity of this diagnostic maneuver has been questioned because no universally accepted criteria exist for diagnosis during surgery. More objective tests are being developed, particularly those that identify compounds specific to perilymph upon the examination of the fluid contents.
Otolaryngologists may use the following tests to diagnose perilymph fistulas:
- Audiograms to detect hearing loss
- Electrocochleography
- Fistula tests (Hennebert sign): The subjective fistula test is performed by applying positive and negative pressure to the intact eardrum using a pneumatic otoscope. Positive results include the elicitation of nystagmus or onset of dysequilibrium with the sensation of motion or nausea. Some otologists administer the test with electronystagmography or by using platform posturography.
Perilymph labeling methods
- Initial studies used intrathecal or intravenous fluorescein, but these have been abandoned for perilymph-specific protein testing, such as beta-2 transferrin, apo D, and apo J.
- Beta-2 transferrin, a protein found in perilymph and CSF but not in serum, has been the most actively studied. Initial enthusiasm for a Western blot assay for this protein has wavered due to low sensitivity. The presence of beta-2 transferrin in perilymph has been unreliable, possibly due to current collection methods or small sample volumes, and false-positive results may be secondary to CSF contamination during collection.
- Focus has recently switched to the efficacy of apolipoprotein D (apo D) as a marker for perilymph with encouraging results.
- Results of a study by Ikezono et al 3 strongly suggest that cochlin-tomoprotein may be a specific marker of perilymph leakage. Additionally, cochlin-tomoprotein could be a potential marker, allowing definitive diagnosis of perilymph fistula related hearing loss and vestibular disorders.
Perilymph fistula treatment
When a traumatic event results in sudden onset of hearing loss or dizziness, the patient is advised to severely restrict physical activity for 7-14 days. If the symptoms do not improve or they plateau, testing is ordered. If the tests are compatible with the diagnosis of perilymph fistula, a surgical intervention may be considered. Persons with diagnosed fistulas who are awaiting surgery should avoid lifting, straining and bending over as these activities can cause a worsening of the symptoms.
Vertigo suppressants, such as diazepam and meclizine, may be used, although their benefit remains unproven in this setting. Medical therapy is rarely reported. Some reports exist of spontaneous healing with bedrest, head elevation to 30°, and avoidance of lifting or middle-ear pressure–increasing activities.
Home remedies:
- Strict bedrest for 5-7 days or until reevaluation
- Bedrest with the head of the bed elevated to 30°
- Elevation of the patient’s head above the heart level
- Avoidance of straining
- Avoidance of nose blowing or Valsalva maneuver
- No lifting (>10 lb)
- Stool softeners
Perilymph fistula surgery
A perilymph fistula repair involves an operation, often under general anesthesia, working through the ear canal. The eardrum is lifted up and minute soft tissue grafts are placed around the base of the stapes (stirrup) and in the round window niche. The operation usually takes about 45-60 minutes to complete. There is very little, if any, pain. Some patients are kept overnight to restrict activity. Once discharged the patient is advised to spend three days at home with limited activity. After three days the patient may return to sedentary work activities. The patient is advised to avoid lifting more than 10 lbs. for one month and avoid sporting activities. After one month there are additional restrictions suggested on activities such as contact sports, diving, weight lifting, and roller coasters. All of these activities have resulted in recurrent perilymph fistula’s after an initial successful repair.
Complications
Both the patient and the physician should be prepared for no response to treatment, especially with regard to hearing improvement. Recurrence of postoperative signs and symptoms may occur in 21-47% of patients.
Perilymph fistula may be associated with recurrent meningitis in children.
Perilymph fistula prognosis
Because of the difficulty in making the diagnosis of perilymph fistula, the natural history of this disorder is unknown.
Significant improvement in symptoms that are presumed to be from perilymph fistula may occur with conservative treatment.
Surgery is more successful in relieving vertiginous symptoms than in improving hearing.
References- Al Felasi M, Pierre G, Mondain M, Uziel A, Venail F. Perilymphatic fistula of the round window. Eur Ann Otorhinolaryngol Head Neck Dis. 2011 Jun. 128(3):139-41.
- Perilymph fistula. https://emedicine.medscape.com/article/764117-overview
- Ikezono T, Shindo S, Sekine K, Shiiba K, Matsuda H, Kusama K, et al. Cochlin-tomoprotein (CTP) detection test identifies traumatic perilymphatic fistula due to penetrating middle ear injury. Acta Otolaryngol. 2011 Sep. 131(9):937-44.