Decidua
Decidua is the term for the modified mucosal lining of the uterus (modified endometrium) during a pregnancy, which forms the maternal part of the placenta. Decidua is formed in a process called decidualization under the influence of progesterone. Decidualization is a process that occurs in early pregnancy. It is an adaption of the uterus to enable implantation of the embryo. Decidualization begins in the stromal cells around the implanted blastocyst, but soon spreads to involve the rest of the pregnancy endometrium. In humans, blastocyst formation begins about 5 days after fertilization when a fluid-filled cavity opens up in the morula, a ball of cells. Endometrial cells become decidual cells. As the stromal cells enlarge, they dominate the endometrium and the glandular component becomes insignificant. Decidual cells are large with ample cytoplasm, distinct cell borders and small, rounded nuclei. As the maternal interface to the embryo the decidua participates in the exchanges of nutrition, gas, and waste with the gestation. It also protects the pregnancy from the maternal immune system. Furthermore, the decidua has to allow a very controlled invasion of the trophoblast. In invasive placental disorders like placenta accreta decidualization have been consistently found to be deficient. The decidua is shed during the birthing process.
The decidua secretes hormones, growth factors, and cytokines. It has receptors for estrogen, progesterone, growth hormone, and others. Among its products are hormones commonly associated with other organs such as cortisol, CRF, GnRH, prolactin, and relaxin. Decidual prolactin is not under dopaminergic control. Pregnancy protein 14 (PP-14), also called placental protein 12, and Insulin-like growth factor-binding protein 1(IGFBP1) appear to be specific products of the secretory and decidual lining. Other factors released include interleukin-15 and vascular endothelial growth factor (VEGF). A reasonable understanding of the role and interplay of these hormones and factors has not been evolved.
After ovulation, in mammals, the endometrial lining becomes transformed into a secretory lining in preparation of accepting the embryo. Without implantation, the secretory lining will be absorbed (estrous cycle) or shed (menstrual cycle). With implantation the lining now termed decidua evolves further during the pregnancy.
The thickened superficial endometrial layers become the decidua, as follows:
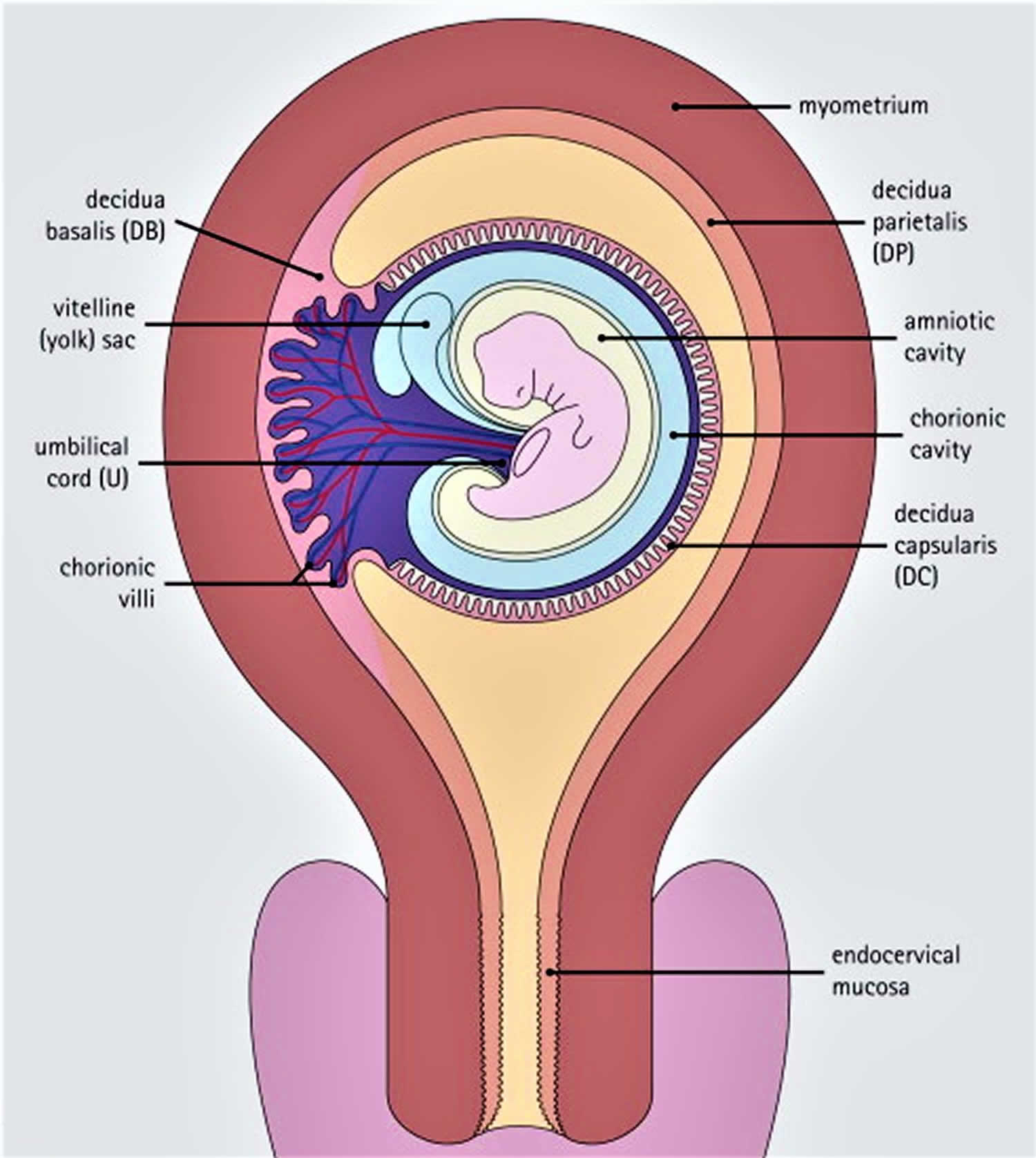
- The endometrium immediately beneath the implantation site, into which the major trophoblast growth occurs, becomes the decidua basalis
- The thin rim of endometrial stroma overlying the blastocyst becomes the decidua capsularis
- The endometrium lining the rest of the uterine cavity is called the decidua parietalis.
Of the decidua, the decidua basalis is the most important, as the vessels in this part of the modified endometrium supply maternal arterial blood to the lacunae between the fetal chorionic villi and receive venous blood from the lacunae. The villous trophoblast (from the fetus) and the decidua basalis (from the mother), and the intervillous spaces between them, comprise the placenta.
Decidual stromal cells have prominent, pale-staining, round or ovoid nuclei, often with finely granular chromatin and one or two nucleoli; their cytoplasm is bulky, and usually eosinophilic, and granular or slightly foamy, although some cells may have a basophilic tinge.
Ultrastructurally, the decidualized stromal cells contain prominent, often long mitochondria, together with variable amounts of rough endoplasmic reticulum
The eosinophilia or basophilia of the cytoplasm in individual cells depends on the relative proportions of mitochondria (eosinophilic) and rough endoplasmic reticulum (basophilic).
Figure 1. Uterine decidua
Footnote: The decidua and their relationships with the developing fetus and placenta.
Layers of decidua
Different layers of the deciduas have been described:
- a compact outer layer (stratum compactum)
- an intermediate layer (stratum spongiosum)
- a boundary layer adjacent to the myometrium.
That part of the decidua that interacts with the trophoblast is the decidua vera (“true decidua”). The remainder of the decidua is termed the decidua parietalis.
The decidua has a histologically-distinct appearance, displaying large polygonal decidual cells in the stroma. These are enlarged endometrial stromal cells, which resemble epithelium (and are referred to as “epithelioid”).
Formation of a specialized decidua is called decidualization, which is a special property of endometrium seen only in hemochorial placentation.
Decidualization includes the process of differentiation of the spindle-shape stromal fibroblasts into the plump secretory decidual cells, which create a pericellular extracellular matrix rich in fibronectin and laminin (similar to epithelial cells).
Vascularity, as well as vascular permeability, is enhanced in the decidualizing endometrium.
Its leukocyte population is distinct, with the presence of large endometrial granular leukocytes being predominant, while polynuclear leukocytes and B-cells are scant.
The large granular lymphocytes (CD56 bright) are called “uterine NK cells” or “uNK cells” in mice, and “decidual NK cells” or “dNK cells” in humans.
The border to the trophoblast is called Nitabuch’s layer.
Decidua function
The purpose of the decidua is to impede the invasion of trophoblasts, a feat it accomplishes not only by forming the physical barrier but also by generating cytokines promoting attachment of the trophoblast.