Diastolic dysfunction
Diastolic dysfunction also called diastolic heart failure, is heart failure with preserved ejection fraction where the left ventricle loses its ability to relax normally and fill with blood during diastole (abnormalities in heart relaxation and filling), because the left ventricle heart muscle has become stiff. The heart can’t properly fill with blood during the resting period between each beat. Diastolic dysfunction is mainly the result of either impaired myocardial relaxation or increased cardiac muscle stiffness. As a result, the pressure in the left ventricle increases at the end of diastole and causes a build up of pressure in the left atrium and consequently in the pulmonary circulation. The result is pulmonary edema and dyspnea. Diastolic dysfunction often occurs in people with certain types of cardiomyopathy or diseases of the heart muscle. Cardiomyopathy damages the muscle tone of the heart and reduces its ability to pump blood to the rest of the body.
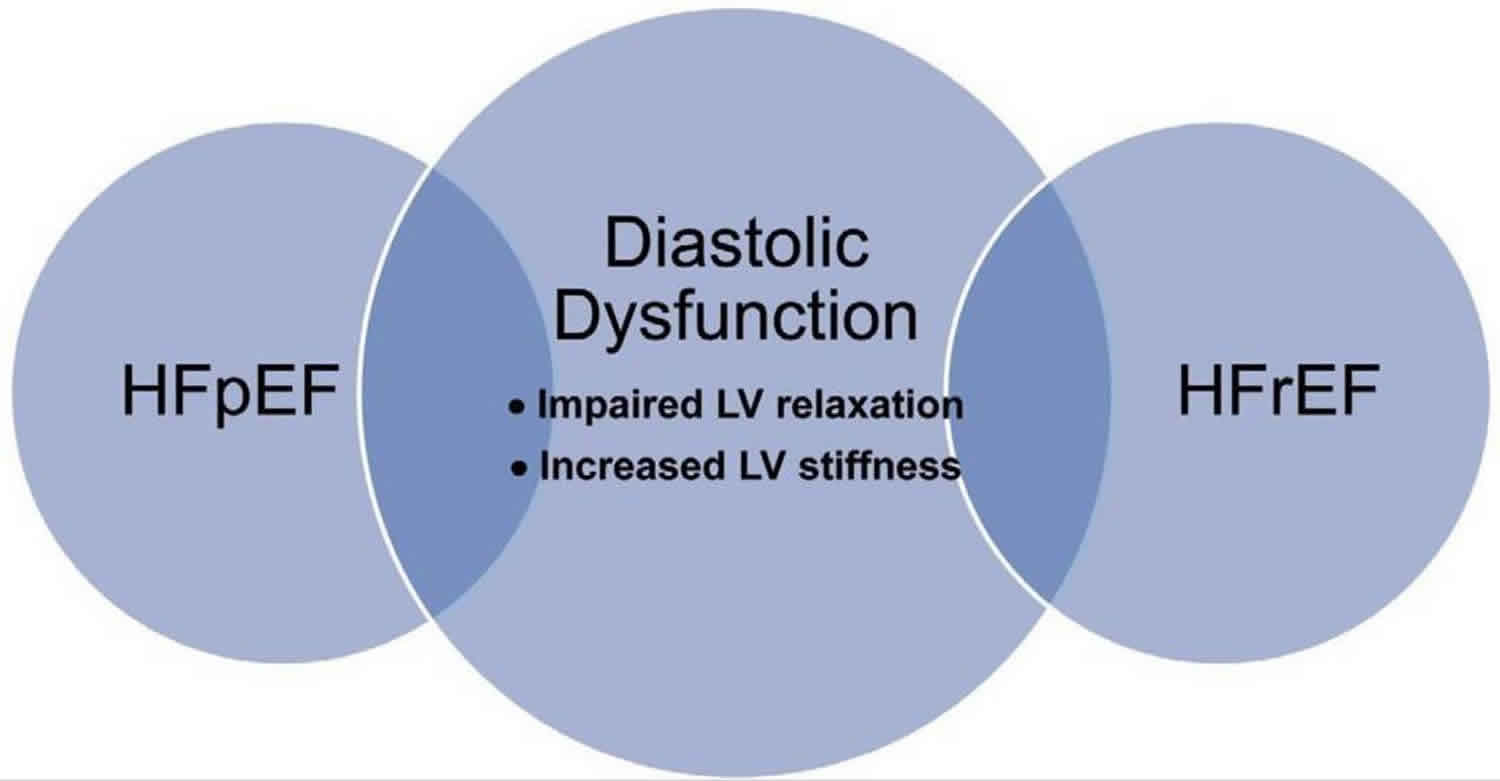
Since the first report of the syndrome of heart failure with a preserved ejection fraction nearly 30 years ago 1, the diagnosis, pathophysiology, and most effective therapies for diastolic dysfunction and heart failure with preserved ejection fraction caused by diastolic dysfunction (ie, diastolic heart failure) have remained controversial 2. Some of the confusion exists because diastolic dysfunction can be present in asymptomatic patients, patients with preserved ejection fraction, and patients with reduced ejection fraction (Figure 1) 3. Moreover, not all cases of heart failure with preserved ejection fraction or heart failure with reduced ejection fraction are associated with diastolic dysfunction 4. Therefore, the relationship of diastolic dysfunction to the clinical syndrome of heart failure is somewhat ill-defined.
Normally, with reference to the left side of the heart, blood flows from the lungs, into the pulmonary veins, into the left atrium, through the mitral valve and finally into the left ventricle. Diastolic dysfunction is the inability of the heart to properly relax and fill with blood during diastole.
A heartbeat is a two-part pumping action that takes about a second. As blood collects in the upper chambers (the right and left atria), the heart’s natural pacemaker (the sinoatrial or SA node) sends out an electrical signal that causes the atria to contract. This contraction pushes blood through the tricuspid and mitral valves into the resting lower chambers (the right and left ventricles). This part of the two-part pumping phase (the longer of the two) is called diastole.
The second part of the pumping phase begins when the ventricles are full of blood. The electrical signals cause the ventricles to contract and push blood through the pulmonary and aortic valves. This is called systole.
If the diastole part of the two-part pumping phase is abnormal, this is called diastolic dysfunction.
In some people with heart failure, the ventricles do not relax properly during diastole. If the ventricles are not relaxed, the pressure inside of them will increase as blood from the next heartbeat tries to enter. This can lead to extra pressure and fluid in the blood vessels of your lungs (called pulmonary congestion) or in the blood vessels leading back to your heart (called systemic congestion).
Heart failure is a major and growing public health problem in the USA, affecting approximately 5.1 million patients, and over 23 million patients worldwide 5. More than 650,000 new patients are diagnosed with heart failure in the USA each year, and approximately half of them show diastolic dysfunction 6. Aging is an independent factor in heart failure incidence. The absolute mortality rate is high, and the prevalence of asymptomatic left ventricular (LV) dysfunction is increasing annually 7. Major risk factors for diastolic dysfunction include age, hypertension, diabetes mellitus, and left ventricular hypertrophy 8. Diastolic dysfunction is common in diabetic patients and is associated with increased left ventricular mass, wall thickness, and arterial stiffness 6. Of note, 34% of patients with diabetes have diastolic dysfunction 9.
Although these risk factors are similar to those for heart failure with reduced ejection fraction, growing evidence indicates that the mechanism of diastolic dysfunction is quite different from that in systolic dysfunction. Many effective treatments for heart failure with reduced ejection fraction have shown disappointing results when applied to heart failure with preserved ejection fraction patients 10. There are also clear clinical differences between heart failure with preserved ejection fraction and heart failure with reduced ejection fraction. Patients with heart failure with preserved ejection fraction are older and more likely to be female 9. In heart failure with preserved ejection fraction, the left ventricular end-diastolic volume is not increased relative to the stroke volume, and there is concentric remodeling. In contrast, heart failure with reduced ejection fraction has eccentric remodeling with left ventricular dilation 11. The major risk factors for diastolic dysfunction are shared between heart failure with preserved ejection fraction and heart failure with reduced ejection fraction 9.
Differentiation between normal and abnormal diastolic function is complicated by overlap between Doppler indices values in healthy individuals and those with diastolic dysfunction 12. Furthermore, normal aging is associated with a number of changes in the heart and vascular system, especially slowing of left ventricle relaxation which may lead to diastolic dysfunction. Therefore, filling patterns in the elderly resemble those observed in mild diastolic dysfunction in younger patients (40–60 years) and age should be taken into account when evaluating diastolic function variables 13. The accuracy of clinicians to diagnose diastolic dysfunction has been questioned 14.
Figure 1. Diastolic dysfunction
Footnote: The relationship of diastolic dysfunction to heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF). Diastolic heart failure is a subset of heart failure with preserved ejection fraction, diastolic dysfunction can exist in heart failure with reduced ejection fraction, and many patients with diastolic dysfunction are asymptomatic.
Abbreviations: HFrEF = heart failure with reduced ejection fraction; HFpEF = heart failure with preserved ejection fraction
[Source 2 ]Diastolic dysfunction grade
There are four basic echocardiographic patterns of diastolic heart failure, which are graded 1 to 4. Grade 1 is called an “abnormal relaxation pattern”, grade 2 is called “pseudonormal filling dynamics”, grade 3 is called “restrictive filling dynamics”, and grade 4 is called “reversible restrictive diastolic dysfunction”.
Table 1. Grades of Diastolic Dysfunction as Categorized by Echocardiography
| Normal | Grade I Abnormal relaxation | Grade II Pseudonormal | Grade III Restrictive (reversible) | Grade IV Restrictive (fixed) | |
|---|---|---|---|---|---|
| NYHA | I–II | II–III | III–IV | IV | |
| Mitral inflow (PW) | 0.75<E/A<1.5 150<DT<240 ms IVRT 70–90 ms | E/A≤0.75 DT >240 ms IVRT >90 ms | 0.75<E/A<1.5 150<DT<200 ms IVRT <90 ms | E/A >1.5 DT <150 ms IVRT <70 ms | E/A >1.5 DT <15 ms IVRT <70 ms |
| Mitral inflow on valsalva | ΔE/A >0.5 | ΔE/A ≤0.5 | ΔE/A ≥0.5 | ΔE/A ≥0.5 | ΔE/A <0.5 |
| Mitral anular motion (TDI) | E/e’ <10 e’ >8 | E/e’ <10 e’ <8 | E/e’ ≥10 e’ <8 | E/e’ ≥10 e’ <8 | E/e’ ≥10 e’ <8 |
| Vp (Color M-mode) | Vp >55 | Vp >45 | Vp <45 | Vp <45 | Vp <45 |
| Pulmonary venous flow (PW-Doppler) | S≥D ARdur-Adur <0 ms | S>D ARdur-Adur <0 ms | S<D or ARdur-Adur ≥30 ms | S<D or ARdur-Adur ≥30 ms | S<D or ARdur-Adur ≥30 ms |
| LV relaxation (tau) | Normal | Impaired | Impaired | Impaired | Impaired |
| LV compliance | Normal | Normal to ↓ | ↓↓ | ↓↓↓ | ↓↓↓↓ |
| LA pressure | Normal | Normal | ↑↑ | ↑↑↑ | ↑↑↑↑ |
| LV blood filling | Normal | ↓ | ↓↓ | ↓↓↓ | ↓↓↓ |
| LV volume index | <34 ml/m2 | <34 ml/m2 | >34 ml/m2 | >34 ml/m2 | >34 ml/m² |
Abbreviations: A = late diastolic mitral velocity; Adur = duration of A wave; ARdur = peak pulmonary venous atrial reversal flow velocity duration; D = a diastolic wave in pulmonary vein flow; E = early diastolic mitral velocity; e’ = peak early diastolic mitral annulus velocity; IVRT = isovolumic relaxation time; PW-Doppler = pulse-wave Doppler; S = a larger systolic wave in pulmonary vein flow; TDI = tissue Doppler imaging; Vp = color M-mode Doppler blood velocity.
[Source 2 ]Grade 1 diastolic dysfunction
The mildest form is called an “abnormal relaxation pattern” or grade 1 diastolic dysfunction. On the mitral inflow Doppler echocardiogram, there is reversal of the normal E/A ratio. This pattern may develop normally with age in some patients, and many grade 1 patients will not have any clinical signs or symptoms of heart failure.
The E/A ratio is the ratio of the early (E) to late (A) ventricular filling velocities. In a healthy heart, the E velocity is greater than the A velocity. In certain conditions, especially ventricular hypertrophy, and with aging, the left ventricular wall can become stiff, increasing the back pressure as it fills, which slows the early (E) filling velocity, thus lowering the E/A ratio.
Grade 2 diastolic dysfunction
Grade 2 diastolic dysfunction is called “pseudonormal filling dynamics”. This is considered moderate diastolic dysfunction and is associated with elevated left atrial filling pressures. These patients more commonly have symptoms of heart failure, and many have left atrial enlargement due to the elevated pressures in the left heart.
Grade 3 diastolic dysfunction
Grade 3 diastolic dysfunction is associated with “restrictive filling dynamics”. This is a severe forms of diastolic dysfunction, and patients tend to have advanced heart failure symptoms. Grade 3 diastolic dysfunction patients will demonstrate reversal of their diastolic abnormalities on echocardiogram when they perform the Valsalva maneuver. This is referred to as “reversible restrictive diastolic dysfunction”.
Grade 4 diastolic dysfunction
Grade 4 diastolic dysfunction patients will not demonstrate reversibility of their echocardiogram abnormalities, and are therefore said to suffer from “fixed restrictive diastolic dysfunction”.
Causes of diastolic heart failure
Diastolic dysfunction is the mechanical abnormality of the heart to properly relax and fill with blood during diastole. Several medical conditions may cause this to occur; namely cardiovascular conditions, genetic conditions, pulmonary conditions, rheumatologic conditions, and diabetes.
Causes of abnormal diastolic function:
- Amyloidosis
- Aortic stenosis
- Constrictive pericarditis
- Diabetes
- Effusive-constrictive pericarditis
- Glycogen storage disease
- Hemochromatosis
- Hypereosinophilic syndrome
- Hypertrophic heart diseases(for example, as seen in hypertension)
- Hypertrophic obstructive cardiomyopathy (HOCM)
- Infiltrative diseases ( for example, amyloidosis)
- Ischemia
- Mitral stenosis
- Myocardial infarction and scar
- Pericardial effusion
- Restrictive cardiomyopathy
- Sarcoidosis
- Systolic dysfunction
Diastolic dysfunction associations with other diseases
In these studies, it is not clear whether these association are unique to diastolic heart failure or whether they may also be associated with systolic heart failure. It is not clear how well the observational studies control for the degree of hypertension as the studies only measured the presence of absence of a history of hypertension.
Relationship of diastolic dysfunction to diastolic heart failure
Epidemiological evidence suggests there is a latent phase in which diastolic dysfunction is present and progresses in severity before the symptoms of heart failure arise 4. Asymptomatic mild left ventricular diastolic dysfunction is found in 21%, and moderate or severe diastolic dysfunction is present in 7% of the population 4. Both moderate and severe diastolic dysfunction is associated with an increased risk of symptomatic heart failure and mortality 4. This asymptomatic phase represents a potential time to intervene to prevent symptomatic heart failure. Suggesting the success of possible interventions, a mortality benefit has been observed in those whose diastolic dysfunction improved compared with those whose diastolic dysfunction remained the same or worsened 17. In early diastolic dysfunction, elevated left ventricular stiffness is associated with diastolic filling abnormalities and normal exercise tolerance. Asymptomatic diastolic dysfunction may be present for significant periods before it develops into a symptomatic clinical event. When the disease progresses, pulmonary pressures increase abnormally during exercise, producing reduced exercise tolerance. When filling pressures increase further, clinical signs of heart failure appear 8. In a significant number of cases of diastolic heart failure, patients have atrial fibrillation at the time of diagnosis, suggesting an association and a possible common pathogenesis 18. With atrial fibrillation, diastolic dysfunction may rapidly lead to overt diastolic heart failure (Figure 2) 19.
Figure 2. Major risk factors for diastolic dysfunction, which can lead to asymptomatic or symptomatic diastolic dysfunction.
Abbreviations: HTN = hypertension; LVH = left ventricular hypertrophy.
[Source 2 ]Diastolic dysfunction symptoms
The most common complaints of diastolic dysfunction at presentation are exertional dyspnea and fatigue. The diagnosis of diastolic dysfunction or diastolic heart failure is not clinical and requires a work up that goes beyond the history, physical exam, echocardiography and chest X-rays. Several studies have evaluated the diagnostic criteria to follow in differentiating systolic dysfunction from diastolic dysfunction.
Currently, three criteria must be met to establish the diagnosis:
- Clinical symptoms consistent with heart failure
- Preserved left ventricular ejection fraction (LVEF at least 50 percent)
- Evidence of cardiac dysfunction
Diastolic dysfunction diagnosis
The presence and severity of diastolic dysfunction is commonly evaluated by echocardiography using color Doppler and tissue Doppler imaging. Alternative modalities include strain analysis from cardiac magnetic resonance imaging (CMR) and speckle tracking echocardiography (STE). The diagnosis of diastolic heart failure, a subset of heart failure with preserved ejection fraction, requires 3 conditions to be simultaneously satisfied
- The presence of signs and symptoms of heart failure
- The presence of normal or only slightly reduced left ventricular ejection fraction (LVEF >50%) and
- The presence of increased diastolic pressure or impaired filling as indicated by delayed isovolumic relaxation or elevated stiffness.
Two-dimensional echocardiography with Doppler flow measurements is commonly used to assess diastolic dysfunction 20. Exercise may be required to clearly demonstrate diastolic functional changes 21. During diastole, blood flows through the mitral valve when the left ventricular relaxes, causing an early diastolic mitral velocity (E), and then additional blood is pumped through the valve when the left atrium contracts during late diastole (A). The E/A ratio can be altered in diastolic dysfunction. Tissue Doppler imaging is an echocardiographic technique that measures the velocity of the mitral annulus. This velocity has been shown to be a sensitive marker of early myocardial dysfunction. With abnormal active relaxation, mitral annulus velocity during early diastole (e’) is decreased while mitral annulus velocity during late diastole (a’) is increased, resulting in a lowered e’/a’ ratio. In animal models, tissue Doppler imaging has been validated as a reliable tool for the evaluation of diastolic dysfunction 22. Left ventricular inflow propagation velocity (VP) by color M-mode Doppler is another relatively preload-insensitive index of left ventricular relaxation 23. It has been shown to correlate well with the time constant of isovolumic relaxation (τ), both in animals and humans 20.
Recently, speckle tracking echocardiography has emerged as a promising technique for the evaluation of myocardial wall motion by strain analysis. By tracking the displacement of speckles during the cardiac cycle, speckle tracking echocardiography allows semiautomated delineation of myocardial deformation.
Cardiac magnetic resonance imaging is a newer technique for measuring diastolic dysfunction 24. Myocardial tagging allows the labeling of specific myocardial regions. Following these regions during diastole enables them to be analyzed in a manner similar to speckle tracking echocardiography. In addition, the rapid diastolic untwisting motion followed by cardiac magnetic resonance tagging is directly related to isovolumic relaxation and can be used as an index of the rate and completeness of relaxation 24.
Biomarkers may contribute to the diagnosis. B-type natriuretic peptide (BNP) and TnI have been used as heart failure biomarkers and exhibit strong association with hospitalization 25. Nevertheless, they are nonspecifi and not well correlated with diastolic dysfunction. Recently, it has been reported that cMyBP-C could be a new biomarker releases from damaged myofilaments 26. Additionally, elevated S-glutathionylated cMyBP-C level can be detected in the blood of patients with diastolic dysfunction 27. Hypertension and diabetes lead to cardiac oxidation and S-glutathionylation of cMyBP-C, a cardiac contractile protein, which leads to impaired relaxation, and modified cMyBP-C in the blood may represent a circulating biomarker for diastolic dysfunction 28.
Diastolic dysfunction diagnostic criteria
The diagnostic criteria published by the Working Study Group for the European Society of Cardiology in 1998 29 included three obligatory conditions for the diagnosis of diastolic heart failure:
- Signs or symptoms of heart failure: Heart failure often presents with a history of dyspnea and orthopnea, and pulmonary rales on examination.
- Normal or mildly abnormal systolic left ventricular (LV) function:
- Left ventricular ejection fraction (LVEF) > 50% and an left ventricular end-diastolic volume index (LVEDVI) <97 mL/m²
- Evidence of diastolic left ventricular dysfunction:
- Isovolumic relaxation time (IVRT): <30 years > 92 ms; 30–50 years > 100 ms; >50 years > 105 msc
- E/A <1 + deceleration time (DT) >220 ms + S/D <1.5 <50 years
- E/A<0.5 + DT >280 msec + S/D >2.5 >50 years
Abbreviations: DT = deceleration time of E velocity, E/A = ratio of early diastolic velocity to atrial velocity, EF = ejection fraction, HF = heart failure, IVRT = isovolumic relaxation time, LV = left ventricular, LVIDDi = left ventricular internal diastolic diameter index, S/D = ratio of systolic to diastolic velocity of venous pulmonary veins.
Other authors have suggested that signs and symptoms of heart failure with a normal ejection fraction is adequate in chronic heart failure 30 and acute heart failure 31.
Determining diastolic dysfunction severity
Echocardiography may grade the severity of diastolic dysfunction, parameters include 32:
Mild diastolic dysfunction:
- E/A ratio <0.8
- E/e′ ratio < 8
Moderate diastolic dysfunction (grade 2; “impaired myocardial relaxation with mild to moderate elevation of LV filling pressures”):
- E/A ratio 0.8 to 1.5 (pseudonormal)
- E/e′ (average) ratio is 9 to 12
Severe diastolic dysfunction (grade 3; “restrictive LV filling occurs”):
- E/A ratio ≥ 2
- E/e′ (average) ratio > 13
The E/A ratio is the ratio of the early (E) to late (A) ventricular filling velocities. In a healthy heart, the E velocity is greater than the A velocity. In certain conditions, especially ventricular hypertrophy, and with aging, the left ventricular wall can become stiff, increasing the back pressure as it fills, which slows the early (E) filling velocity, thus lowering the E/A ratio.
The reversal of the E/A ratio (‘A’ velocity becomes greater than ‘E’ velocity) is often accepted as a clinical marker of diastolic dysfunction, in which the left ventricular wall becomes so stiff as to impair proper filling, which can lead to diastolic heart failure. This can occur, for instance, with longstanding untreated hypertension.
Diastolic dysfunction treatment
To date, there are no specific treatments for diastolic dysfunction to selectively enhance myocardial relaxation. Moreover, no drug has been developed to improve long-term outcomes for diastolic heart failure 33. Nevertheless, recent trials and new hypotheses about the mechanism of diastolic dysfunction suggest possible directions for specific therapies.
The chronic treatment of diastolic dysfunction involves aggressive management of the underlying disorder that is causing the diastolic dysfunction such as diabetes or hypertension. Mild diastolic dysfunction that is well tolerated requires no specific treatment. Rate control is an important part of the acute therapy of the patient with diastolic heart failure. It takes a longer period of time for a stiff left ventricle to fill, and therefore rate control is a critical part of the acute therapy of diastolic dysfunction.
Acute treatment of diastolic heart failure
Rate control
It takes a longer period of time for a stiff left ventricle to fill, and therefore rate control is a critical part of the acute therapy diastolic dysfunction. Furthermore, in atrial fibrillation there is a failure of atrial kick to augment the filling of the left ventricle.
Diuresis
Diuresis may reduce acute volume overload.
Relief of ischemia
Acute myocardial ischemia leads to diastolic dysfunction which increases left atrial pressure and causes pulmonary edema.
Chronic treatment of diastolic heart failure
Afterload reduction
There is some evidence that calcium channel blocker drugs may be of benefit in reducing ventricular stiffness in some cases. Likewise, treatment with angiotensin converting enzyme inhibitors such as enalapril, ramipril, and other ACE inhibitors may be of benefit due to their effect on ventricular remodeling.
Treatment for heart failure with preserved ejection fraction
Recent clinical trials using drugs of advantage in systolic dysfunction have failed to demonstrate improvement in long-term outcome for diastolic heart failure, further emphasizing differences in the underlying pathophysiology of diastolic dysfunction. Several trials of these drugs for heart failure with preserved ejection fraction are summarized in Table 2. Despite abundant evidence of the efficacy of reninangiotensin system inhibition in systolic dysfunction, the PEP-congestive heart failure trial using perindopril showed no overall difference in mortality and or need for heart failure hospitalization 34. In the Hong Kong Diastolic Heart Failure study, only diuretics in combination with irbesartan or ramipril marginally improved diastolic function and lowered NT-proBNP over 1 year 35. Angiotensin II receptor blockers show a similar lack of efficacy. The CHARM-preserved trial, which randomized 3,023 patients between candesartan and placebo, showed no beneficial effect in cardiovascular death at 3-year follow-up 36. In the I-PRESERVE trial, which randomized 4,128 patients, irbesartan showed no reduction in all-cause mortality or hospitalization for a cardiovascular cause at 49.5-month follow-up 37. In OPTIMIZE-heart failure, carvedilol, a beta-blocker, did not affect primary or long-term outcomes for heart failure with preserved ejection fraction 38. In the SENIORS trial, nebivolol showed limited beneficial effect in the elderly heart failure with preserved ejection fraction group (age >70) 39. The CORONA trial used a statin and showed only LV remodeling improvement without changes in the primary outcomes 40. Aldosterone antagonists are known to prevent the development of cardiac hypertrophy and fibrosis 41. Aldo-diastolic heart failure, using spironolactone, revealed little improvement in left ventricular relaxation and no change in the primary outcome in heart failure with preserved ejection fraction patients 42. In the TOPCAT trial, there was no reduction in mortality, aborted cardiac arrest or hospitalization for heart failure with preserved ejection fraction patients using spironolactone 43. Furthermore, the inotropic agent digoxin showed no significant advantage in heart failure with preserved ejection fraction 44.
There is accumulating evidence indicating diastolic dysfunction is associated with oxidative stress and the nitric oxide (NO) pathway. Oxidative stress is often associated with reduced nitric oxide (NO) and cGMP levels, leading to vasoconstriction and cardiac stiffness 45. Therefore, it might stand to reason that increasing NO-cGMP signaling by phosphodiesterase (PDE)-5 inhibition would improve diastolic function. Nevertheless, the RELAX trial, which used sildenafil to treat NYHA class II/III heart failure with preserved ejection fraction patients showed no significant difference in clinical outcomes 46. This suggests that diastolic dysfunction is independent of downstream cGMP-dependent signaling, but the result does not clearly rule out the oxidative stress hypothesis.
Ranolazine
Ranolazine, an anti-anginal drug with multiple putative mechanisms of action, has shown some promise as a treatment for diastolic dysfunction. In an animal model of hypertension-induced diastolic dysfunction, ranolazine worked directly on myofilaments to correct the defect in relaxation 47. Ranolazine is also known to decrease the late Na+ current, which may lower internal Na+ and Ca2+ levels in diastole 48. In the randomized clinical trial, RALI-diastolic heart failure, acute infusion of ranolazine in heart failure with preserved ejection fraction patients resulted in modest improvements in hemodynamics, but no improvement in LV relaxation 49. It is possible that ranolazine may have therapeutic efficacy in diastolic dysfunction, even if the mechanism is unclear.
Tetrahydrobiopterin (BH4)
NO synthase (NOS) usually produces nitric oxide (NO), which relaxes the heart 50. When the NOS cofactor, BH4, becomes oxidized and depleted, NOS begins to produce superoxide, an oxidant, rather than nitric oxide. This situation is called NOS uncoupling. In hypertension-induced diastolic dysfunction, cardiac NOS is uncoupled, BH4 is reduced, and nitric oxide is decreased. Cardiac oxidation generated diastolic dysfunction independent of changes in the vasculature. Supplementation with oral BH4 prevented or reversed the cardiac changes, including the diastolic dysfunction.
The cellular level of BH4 also regulates SERCA2A activity 51. HMG-CoA reductase inhibitors (statins) or resveratrol increase BH4 availability and improve LV relaxation in diabetes 52 and in a hyperlipidemia animal model 53. Therefore, increasing BH4 may be a promising therapeutic target for diastolic dysfunction. Currently, oral BH4 is used to treat atypical phenylketonuria and shows a favorable safety profile 54.
Mitochondria-Targeted Antioxidants
Oxidative stress has been implicated in the pathophysiology of cardiac remodeling and diastolic dysfunction 55. Mitochondria are a major source of cardiac oxidative stress, especially in diabetes, and diabetes is a risk factor for diastolic dysfunction. In preliminary data, Chung et al 56 have shown that diabetes is associated with cardiac mitochondrial oxidative stress and diastolic dysfunction. Injecting animals with a mitochondria-targeted antioxidant, mitoTEMPO, prevented diabetic-associated diastolic dysfunction 57. Other mitochondria-targeted antioxidants that have shown beneficial effects in muscle include MitoQ10 58 and the mitochondria-selective peptide, SS-31 59. Any of these may represent a novel therapeutic strategy for diastolic dysfunction.
Table 2. Randomized preclinical or clinical trials for heart failure with preserved ejection fraction
| Pre- or clinical trial | Drug type | Drug | n | Years* | Comments | Outcome** Mortality/ Hospitalization | Reference |
|---|---|---|---|---|---|---|---|
| PEP-CHF | ACEI | Perindopril | 850 | 1 | Improved HF symptom, exercise capacity | No/partial at 1 st year | Cleland et al 34 |
| Hong Kong DHF | ACEI+diuretics | Ramipril+ Irbesartan | 150 | 1 | Improved HF symptoms and LV function with diuretics combination, but no effect with irbesartan or ramipril alone | No/No | Yip et al 35 |
| CHARM- preserved | ARB | Candesartan | 3,023 | 1–3 | Moderate effect in preventing admissions for CHF among HFpEF patients | No/partial | Persson et al 36 |
| I-PRESERVE | Irbesartan | 4,128 | <1 | No improvement | No/No | Massie et al 37 | |
| OPTIMIZE-HF | β-blocker | Carvediol | 24,689 | 1 | No beneficial effect on mortality | No/No | Hernandez et al 38 |
| SENIOR | Nebivolol | 2,128 | <2 | Beneficial on primary outcome in seniors >70 years, HFpEF Well- tolerated, vasodilation | Yes/Yes | Flather et al 39 | |
| CORONA | HMG-CoA inhibitor | Rosuvastatin | 2,514 | 0.5 | Beneficial on LV remodeling, hyper- trophy & fibrosis | No/No | Kjekshus et al 40 |
| Aldo-DHF | Aldosterone antagonist | Spironolactone | 209 | 1 | Beneficial on LV stiffness, but no better exercise capacity | No/No | Edelmann et al 42 |
| TOPCAT | Spironolactone | 3,445 | 3.3 | No benefit in HFpEF | No/No | Pitt et al 43 | |
| DIG | Inotropic vasodilator | Digoxin | 3,397 | 2 | Beneficial to reduce LV blood over- load, pulmonary congestion | No/No | DIG 44 |
| RALI-DHF† | Late INa inhibitor | Ranolazine | 20 | Acute | 24 h infusion, 14-day oral treatment; improved hemodynamics No relaxation improvement, no NT-proBNP changes | No/No | Maier et al 49 |
| RELAX | PDE-5 inhibitor | Sidenafil | 206 | 6 | Increase NO production to improve relaxation, but no better exercise capacity, 24-week treatment | No/No | Redfield et al 46 |
Footnote:
*Study period (years);
**primary outcome of mortality and hospitalization;
†preclinical trial with acute treatment.
Abbreviations: ACEI = angiotensin-converting enzyme inhibitor; ARB = angiotensin II receptor blocker; BNP = brain natriuretic peptide; DHF = diastolic heart failure; DIG = Digitalis Investigation Group trial; HFpEF = heart failure with preserved ejection fraction; HMG-CoA = hydroxymethylglutaryl-coenzyme A; INa = sodium current; PDE = phosphodiesterase.
[Source 2 ] References- Congestive heart failure with normal systolic function. Dougherty AH, Naccarelli GV, Gray EL, Hicks CH, Goldstein RA. Am J Cardiol. 1984 Oct 1; 54(7):778-82.
- Jeong EM, Dudley SC Jr. Diastolic dysfunction. Circ J. 2015;79(3):470–477. doi:10.1253/circj.CJ-15-0064 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4861951
- Mechanisms of diastolic dysfunction in heart failure with a preserved ejection fraction: If it’s not one thing it’s another. LeWinter MM, Meyer M. Circ Heart Fail. 2013 Nov; 6(6):1112-5.
- Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. JAMA. 2003 Jan 8; 289(2):194-202.
- Heart disease and stroke statistics–2010 update: a report from the American Heart Association. WRITING GROUP MEMBERS., Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2010 Feb 23; 121(7):e46-e215.
- Prevention of heart failure: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Schocken DD, Benjamin EJ, Fonarow GC, Krumholz HM, Levy D, Mensah GA, Narula J, Shor ES, Young JB, Hong Y, American Heart Association Council on Epidemiology and Prevention., American Heart Association Council on Clinical Cardiology., American Heart Association Council on Cardiovascular Nursing., American Heart Association Council on High Blood Pressure Research., Quality of Care and Outcomes Research Interdisciplinary Working Group., Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation. 2008 May 13; 117(19):2544-65.
- 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation., American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 Oct 15; 62(16):e147-239.
- Diastolic heart failure. Mandinov L, Eberli FR, Seiler C, Hess OM. Cardiovasc Res. 2000 Mar; 45(4):813-25.
- Trends in prevalence and outcome of heart failure with preserved ejection fraction. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. N Engl J Med. 2006 Jul 20; 355(3):251-9.
- What mechanisms underlie diastolic dysfunction in heart failure? Kass DA, Bronzwaer JG, Paulus WJ. Circ Res. 2004 Jun 25; 94(12):1533-42.
- HFpEF: cardiovascular abnormalities not just comorbidities. Little WC, Zile MR. Circ Heart Fail. 2012 Nov; 5(6):669-71.
- Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277-314. https://orbi.uliege.be/bitstream/2268/220260/1/byrd.pdf
- Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D, et al. Echocardiographic reference ranges for normal cardiac Doppler data: results from theNORRE Study. Eur Heart J Cardiovasc Imaging 2015;16:1031-41.
- Diastolic heart failure: neglected or misdiagnosed? J Am Coll Cardiol. 2002 Jan 2;39(1):138-41. https://doi.org/10.1016/S0735-1097(01)01704-1
- Is it time to recognize a new phenotype? Heart failure with preserved ejection fraction with pulmonary vascular disease. Eur Heart J. 2017 Oct 7;38(38):2874-2878. doi: 10.1093/eurheartj/ehx184 https://www.ncbi.nlm.nih.gov/pubmed/28431020
- Unger ED, Dubin RF, Deo R, et al. Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2016;18(1):103–112. doi:10.1002/ejhf.445 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713321
- Mortality rate in patients with diastolic dysfunction and normal systolic function. Halley CM, Houghtaling PL, Khalil MK, Thomas JD, Jaber WA. Arch Intern Med. 2011 Jun 27; 171(12):1082-7.
- Diastolic dysfunction and risk of atrial fibrillation: a mechanistic appraisal. Rosenberg MA, Manning WJ. Circulation. 2012 Nov 6; 126(19):2353-62.
- Diastolic dysfunction and heart failure with a preserved ejection fraction: Relevance in critical illness and anaesthesia. Maharaj R. J Saudi Heart Assoc. 2012 Apr; 24(2):99-121.
- Oh JK, Park SJ, Nagueh SF. Established and novel clinical applications of diastolic function assessment by echocardiography. Circ Cardiovasc Imaging. 2011;4:444–455.
- Asrar ul Haq M, Mutha V, Lin T, Profitis K, Tuer Z, Lim K, et al. Left ventricular torsional dynamics post exercise for LV diastolic function assessment. Cardiovasc Ultrasound. 2014;12:8.
- Maharaj R. Diastolic dysfunction and heart failure with a preserved ejection fraction: Relevance in critical illness and anaesthesia. J Saudi Heart Assoc. 2012;24:99–121.
- Garcia MJ, Palac RT, Malenka DJ, Terrell P, Plehn JF. Color M-mode Doppler flow propagation velocity is a relatively preload-independent index of left ventricular filling. J Am Soc Echocardiogr. 1999;12:129–137.
- Dusch MN, Thadani SR, Dhillon GS, Hope MD. Diastolic function assessed by cardiac MRI using longitudinal left ventricular fractional shortening. Clin Imaging. 2014;38:666–668.
- Vorovich E, French B, Ky B, Goldberg L, Fang JC, Sweitzer NK, et al. Biomarker predictors of cardiac hospitalization in chronic heart failure: A recurrent event analysis. J Card Fail. 2014;20:569–576.
- Govindan S, McElligott A, Muthusamy S, Nair N, Barefield D, Martin JL, et al. Cardiac myosin binding protein-C is a potential diagnostic biomarker for myocardial infarction. J Mol Cell Cardiol. 2012;52:154–164.
- Jeong EM, Brahmanandam V, Raicu M, Lee SY, Chung JH, Rutledge C, et al. Plasma myosin binding protein-C fragments and S-glutathionylation in diastolic heart failure (abstract) Circulation. 2012;126:A11366.
- Jeong EM, Dudley SC., Jr New diagnostic and therapeutic possibilities for diastolic heart failure. RI Med J. 2014;97:35–37.
- European study Group on Diastolic Heart Failure. How to diagnose diastolic heart failure. Eur Heart J 1998;19:990-1003.
- Heart failure with a normal ejection fraction: is measurement of diastolic function necessary to make the diagnosis of diastolic heart failure? Circulation. 2001 Aug 14;104(7):779-82. https://www.ahajournals.org/doi/pdf/10.1161/hc3201.094226
- The Pathogenesis of Acute Pulmonary Edema Associated with Hypertension. N Engl J Med. 2001 Jan 4;344(1):17-22. DOI: 10.1056/NEJM200101043440103
- Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009 Feb;22(2):107-33. doi: 10.1016/j.echo.2008.11.023. https://www.onlinejase.com/article/S0894-7317(08)00739-6/fulltext
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–e239.
- Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–2345.
- Yip GW, Wang M, Wang T, Chan S, Fung JW, Yeung L, et al. The Hong Kong diastolic heart failure study: A randomised controlled trial of diuretics, irbesartan and ramipril on quality of life, exercise capacity, left ventricular global and regional function in heart failure with a normal ejection fraction. Heart. 2008;94:573–580.
- Persson H, Lonn E, Edner M, Baruch L, Lang CC, Morton JJ, et al. Diastolic dysfunction in heart failure with preserved systolic function: Need for objective evidence: Results from the CHARM Echocardiographic Substudy-CHARMES. J Am Coll Cardiol. 2007;49:687–694.
- Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–2467.
- Hernandez AF, Hammill BG, O’Connor CM, Schulman KA, Curtis LH, Fonarow GC. Clinical effectiveness of beta-blockers in heart failure: Findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry. J Am Coll Cardiol. 2009;53:184–192.
- Flather MD, Shibata MC, Coats AJ, van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS) Eur Heart J. 2005;26:215–225.
- Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JG, Cornel JH, et al. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357:2248–2261.
- Tsutamoto T, Wada A, Maeda K, Mabuchi N, Hayashi M, Tsutsui T, et al. Effect of spironolactone on plasma brain natriuretic peptide and left ventricular remodeling in patients with congestive heart failure. J Am Coll Cardiol. 2001;37:1228–1233.
- Edelmann F, Wachter R, Schmidt AG, Kraigher-Krainer E, Colantonio C, Kamke W, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: The Aldo-DHF randomized controlled trial. JAMA. 2013;309:781–791.
- Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–1392.
- Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–533.
- Silberman GA, Fan TH, Liu H, Jiao Z, Xiao HD, Lovelock JD, et al. Uncoupled cardiac nitric oxide synthase mediates diastolic dysfunction. Circulation. 2010;121:519–528.
- Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: A randomized clinical trial. JAMA. 2013;309:1268–1277.
- Lovelock JD, Monasky MM, Jeong EM, Lardin HA, Liu H, Patel BG, et al. Ranolazine improves cardiac diastolic dysfunction through modulation of myofilament calcium sensitivity. Circ Res. 2012;110:841–850.
- Zhang XQ, Yamada S, Barry WH. Ranolazine inhibits an oxidative stress-induced increase in myocyte sodium and calcium loading during simulated-demand ischemia. J Cardiovasc Pharmacol. 2008;51:443–449.
- Maier LS, Layug B, Karwatowska-Prokopczuk E, Belardinelli L, Lee S, Sander J, et al. RAnoLazIne for the treatment of diastolic heart failure in patients with preserved ejection fraction: The RALI-DHF proof-of-concept study. JACC Heart Fail. 2013;1:115–122.
- Smith TW, Balligand JL, Kaye DM, Wiviott SD, Simmons WW, Han X, et al. The role of the NO pathway in the control of cardiac function. J Card Fail. 1996;2:S141–S147.
- Carnicer R, Hale AB, Suffredini S, Liu X, Reilly S, Zhang MH, et al. Cardiomyocyte GTP cyclohydrolase 1 and tetrahydrobiopterin increase NOS1 activity and accelerate myocardial relaxation. Circ Res. 2012;111:718–727.
- Zhang H, Morgan B, Potter BJ, Ma L, Dellsperger KC, Ungvari Z, et al. Resveratrol improves left ventricular diastolic relaxation in type 2 diabetes by inhibiting oxidative/nitrative stress: In vivo demonstration with magnetic resonance imaging. Am J Physiol Heart Circ Physiol. 2010;299:H985–H994.
- Xia N, Daiber A, Habermeier A, Closs EI, Thum T, Spanier G, et al. Resveratrol reverses endothelial nitric-oxide synthase uncoupling in apolipoprotein E knockout mice. J Pharmacol Exp Ther. 2010;335:149–154.
- Jeong EM, Monasky MM, Gu L, Taglieri DM, Patel BG, Liu H, et al. Tetrahydrobiopterin improves diastolic dysfunction by reversing changes in myofilament properties. J Mol Cell Cardiol. 2013;56:44–54.
- Maack C, Bohm M. Targeting mitochondrial oxidative stress in heart failure: Throttling the afterburner. J Am Coll Cardiol. 2011;58:83–86.
- Chung J, Jeong EM, Go Y, Gladstein S, Farzaneh-Far A, Lewandowski ED, et al. Mitochondria-targeted antioxidant ameliorates diet-induced diabetes and diastolic dysfunction (abstract) J Am Coll Cardiol. 2015;61:E597.
- Luo M, Guan X, Luczak ED, Lang D, Kutschke W, Gao Z, et al. Diabetes increases mortality after myocardial infarction by oxidizing CaMKII. J Clin Invest. 2013;123:1262–1274.
- He Q, Harris N, Ren J, Han X. Mitochondria-targeted antioxidant prevents cardiac dysfunction induced by tafazzin gene knockdown in cardiac myocytes. Oxid Med Cell Longev. 2014;2014:654198.
- Dai DF, Chiao YA, Marcinek DJ, Szeto HH, Rabinovitch PS. Mitochondrial oxidative stress in aging and healthspan. Longev Healthspan. 2014;3:6.