Disability rating scale
Disability Rating Scale was developed as a method of rating the effects of traumatic brain injury (TBI) to determine how long recovery might take 1. The Disability Rating Scale provides insight into the patient’s cognitive impairment by tracking progress over time. Key aspects of disability are assessed, including the impairment and handicap of an individual. Eye opening, communication ability, and motor response are among the capabilities measured. Data that reflects these aspects of function can predict the patient’s length of stay in rehabilitation and the ability to return to employment. A primary advantage of the Disability Rating Scale is its ability to track patient progress. Its ease in assessing a patients progress makes the scale a valuable clinical tool. Scaling a person’s general behavioral disability is another benefit of the Disability Rating Scale.
Disability Rating Scale was developed and tested with older juvenile and adult individuals with moderate and severe traumatic brain injury (TBI) in an inpatient rehabilitation setting. One advantage of the disability rating scale is its ability to track an individual from coma to community. Measurement across a wide span of recovery is possible because various items in this scale address all three World Health Organization categories: impairment, disability and handicap. The first three items of the disability rating scale (“Eye Opening,” “Communication Ability” and “Motor Response”) are a slight modification of the Glasgow Coma Scale 2, and reflect impairment ratings. Cognitive ability for “Feeding,” “Toileting” and “Grooming” reflect level of disability. The “Level of Functioning” item is the modification of a measure used by Scranton et al. 3, and reflects handicap, as does the last item, “Employability.”
The maximum score a patient can obtain on the disability rating scale is 29 (extreme vegetative state). A person without disability would score zero. The disability rating scale rating must be reliable, i.e., obtained while the individual is not under the influence of anesthesia, other mind-altering drugs, recent seizure, or recovering from surgical anesthesia.
The disability rating scale is intended to measure accurately general functional changes over the course of recovery. Rappaport et al. 4 obtained disability rating scale scores on 63 traumatic brain injury individuals at rehabilitation admission, discharge, and up to ten years post injury (median = nine years). Results showed a proportional change in disability rating scale scores based on time elapsed between injury and admission to rehabilitation. A significantly greater improvement was seen in the early admission group. Others have also demonstrated the utility of the disability rating scale to make comparisons across time 5. The relative sensitivity of the disability rating scale was addressed by Hall et al. 6. In a comparison with the Glasgow Outcome Scale 7, 71% of traumatic brain injury individuals showed improvement on disability rating scale vs. 33% on Glasgow Outcome Scale.
The disability rating scale has been proven reliable and valid, as addressed in more detail in following sections. It can be self-administered or scored through interview with the client or the family member. The ease of scoring and the brevity of the scale are compelling reasons for its popularity. Scoring time can range from 30 seconds (if one is very familiar with the scale and the client) to 15 minutes, assuming the rater must interview the client/family and seek additional information from available staff.
An additional advantage is the ease and brevity with which information can be obtained by phone interview. Although not optimum, disability rating scale ratings can even be obtained by medical record review retrospectively in certain cases. Another advantage of the disability rating scale is that expertise in the field is not needed to complete it accurately.
A limitation of the disability rating scale is its relative insensitivity at the low end of the scale (mild traumatic brain injury) and its inability to reflect more subtle but sometimes significant changes in an individual within a specific, limited window of recovery.
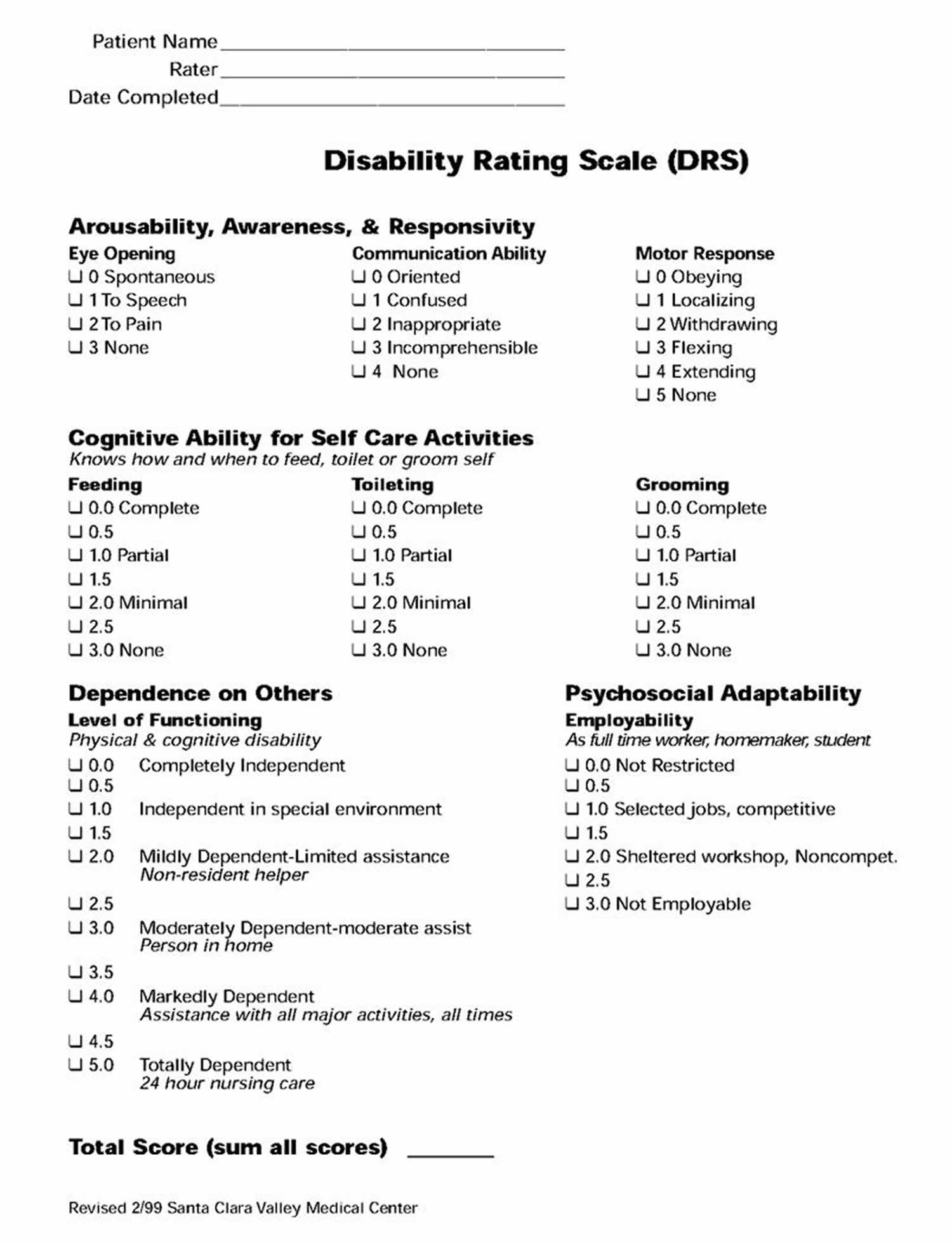
Table 1. Disability Rating Scale
Category | Item | Instructions | Score |
| Arousability, Awareness and Responsivity | Eye Opening | 0 = spontaneous 1 = to speech 2 = to pain 3 = none | |
| Communication Ability | 0 = oriented 1 = confused 2 = inappropriate 3 = incomprehensible | ||
| Motor Response | 0 = obeying 1 = localizing 2 = withdrawing 3 = flexing 4 = extending 5 = none | ||
| Cognitive Ability for Self Care Activities | Feeding | 0 = complete 1 = partial 2 = minimal 3 = none | |
| Toileting | 0 = complete 1 = partial 2 = minimal 3 = none | ||
| Grooming | 0 = complete 1 = partial 2 = minimal 3 = none | ||
| Dependence on Others | Level of Functioning | 0 = completely independent 1 = independent in special environment 2 = mildly dependent 3 = moderately dependent 4 = markedly dependent 5 = totally dependent | |
| Psychosocial Adaptability | Employability | 0 = not restricted 1 = selected jobs 2 = sheltered workshop (non-competitive) 3 = not employable | |
| Total Disability Rating Score | |||
Disability Categories
- Total disability rating score 0 = No disability
- Total disability rating score 1 = Mild disability
- Total disability rating score 2-3 = Partial disability
- Total disability rating score 4-6 = Moderate disability
- Total disability rating score 7-11 = Moderately severe disability
- Total disability rating score 12-16 = Severe disability
- Total disability rating score 17-21 = Extremely severe disability
- Total disability rating score 22-24 = Vegetative state
- Total disability rating score 25-29 = Extreme vegetative state
- Rappaport et al., (1982). Disability rating scale for severe head trauma patients: coma to community. Archives of Physical Medicine and Rehabilitation, 63: 118-123
- Teasdale G, Jennett B: Assessment of coma and impaired consciousness: A practical scale. Lancet 1974;2:81-84.
- Scranton J, Fogel ML, Erdman WJ II: Evaluation of functional levels of patients during and following rehabilitation. Arch Phys Med Rehabil 1970;51: 1-21.
- Rappaport M, Herrero-Backe C, Rappaport ML, Winterfield K: Head injury outcome up to ten years later. Archives of Physical Medicine and Rehabilitation 1989; 70: 885-892.
- Novack TA, Bergquist TF, Bennett G, Gouvier WD: Primary caregiver distress following severe head injury. J Head Trauma Rehabil 1992;6(4):69-77
- Hall K, Cope N, Rappaport M: Glasgow Outcome Scale and Disability Rating Scale: Comparative usefulness in following recovery in traumatic head injury. Arch Phys Med Rehab 1985; 66:35-37.
- Jennett B, Snoek J, Bond MR: Disability after severe injury: observations on use of the Glasgow outcome scale. J Neurol Neurosurg Psychiatry 1981; 44:285-293.