Duke treadmill score
Duke Treadmill Score is a composite index which is used in the evaluation of symptomatic patients to predict the presence of coronary artery disease and their prognosis. The Duke Treadmill score was developed to provide accurate diagnostic and prognostic information for the evaluation of patients with suspected coronary artery disease (coronary heart disease) who has undergone an exercise stress test. The Duke Treadmill score uses three exercise parameters: exercise time, ST segment deviation (depression or elevation) and exertional angina to determine if patients are at a low, intermediate or high risk for ischemic heart disease 1. The typical range is from +15 to -25 1. If patient’s Duke Treadmill Score greater than or equal to 5, they are considered low risk while those who score less than or equal to -11 are considered high risk 1. Duke Treadmill scoring system predicts 5-year mortality, where low-risk scores have a 5-year survival of 97%, intermediate risk scores have a 5-year survival of 90%, and high-risk scores indicate a 5-year survival of about 65%. Patients with an intermediate risk assessment should generally be referred for additional risk stratification with imaging modality 2.
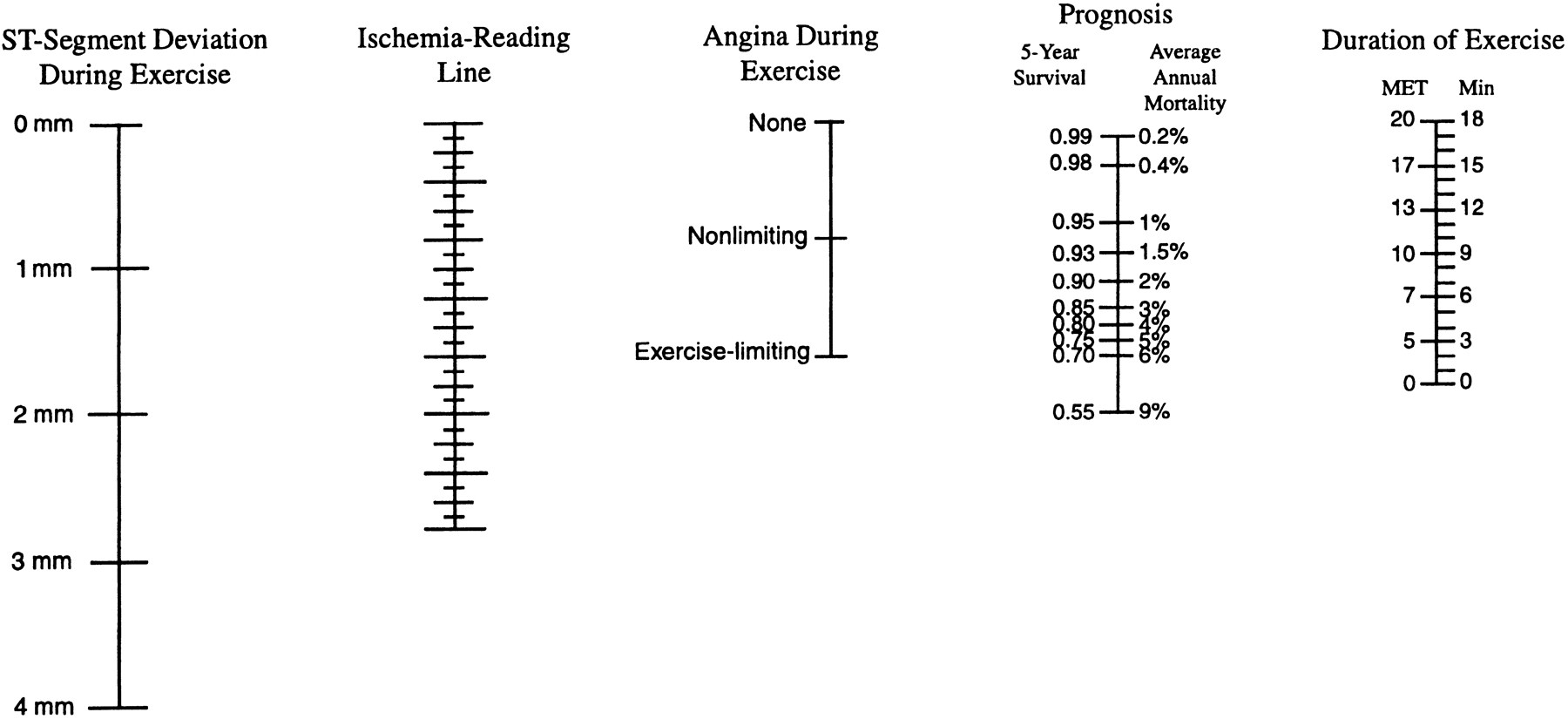
The Duke Treadmill Score incorporates both groups of prognostic markers (exercise capacity and exercise-induced ischemia) 3. Duke Treadmill Score was originally developed using data from 2842 consecutive inpatients referred to Duke University Medical Center between 1969 and 1980 with known or suspected coronary artery disease who underwent exercise testing according to the Bruce protocol 4 before diagnostic angiography who had both cardiac catheterization and treadmill exercise testing 5. None of the patients had prior revascularization or recent myocardial infarction. The Duke Treadmill score has subsequently been validated in 613 outpatients at Duke University Medical Center as well as in populations at other centers. The Duke Treadmill Score works equally well in males and females but has not been extensively evaluated in elderly patients. A nomogram for practical application of this score is shown in Figure 1 below.
All the study patients had a standard Bruce-protocol treadmill test 4. A 12-lead electrocardiogram was recorded before exercise, at the end of each exercise stage, at peak exercise, and at two-minute intervals during recovery. During exercise, three standard electrocardiographic leads were continuously monitored. Exercise was continued until the development of limiting symptoms (angina, dyspnea, or fatigue), abnormalities of rhythm (ventricular tachycardia or frequent couplets) or blood pressure, or marked and progressive ST-segment deviation (≥0.20 mV in the presence of typical angina or in the first stage of exercise).
Exercise stress testing is performed in a designated lab, supervised by a trained healthcare personnel. Electrodes are placed on the chest, which is attached to an ECG machine that is recording the electrical activity of the heart. Your resting ECG, heart rate, and blood pressure are obtained prior to starting the exercise regimen.
The baseline ECG should be evaluated closely prior to starting the exercise portion of the test. There are several baseline ECG changes that can obscure the test results and make it difficult to interpret for ischemia. Such baseline changes include ST-segment changes that are greater than or equal to 1 mm, left bundle branch block, ventricular paced rhythm, left ventricular or right ventricular hypertrophy, ventricular pre-excitation (i.e., Wolff-Parkinson-White syndrome), T wave inversions due to strain pattern or previous injury, conduction abnormalities and medication-induced ST-T wave changes. If any of these ECG abnormalities are noted, the test should be performed with the addition of an imaging modality. The resting ECG is usually obtained both supine and standing, since patient position can influence the QRS and T wave axes.
Once it is determined that there are no limiting factors based on baseline ECG, the patient is placed on a treadmill with a designed protocol that increases in intervals as you exercise. Blood pressure and heart rate are monitored throughout exercise, and the patient is monitored for any developing symptoms such as chest pain, shortness of breath, dizziness or extreme fatigue. The most common protocol used during treadmill exercise stress testing is the Bruce protocol. This protocol is divided into successive 3-minute stages, each of which requires the patient to walk faster and at a steeper grade. The testing protocol could be adjusted to a patient’s tolerance, aiming for 6 to 12 minutes of exercise duration. There is a modified Bruce protocol for those who cannot exercise vigorously, which adds two lower workload stages to the beginning of the standard Bruce protocol, both of which require less effort than Stage 1. There are a number of other protocols for patients who have a limited exercise tolerance; however, other methods that do not include exercise are also available for such patients.
During the exercise test, data about heart rate, blood pressure and ECG changes should be obtained at the end of each stage and at any time an abnormality is detected with cardiac monitoring. In general, heart rate and systolic blood pressure should rise with each stage of exercise until a peak is achieved. Patients should be questioned about any symptoms they experience during exercise. All patients should be monitored closely during the recovery period until heart rate, and ECG are back to baseline, as arrhythmias and ECG changes can still develop.
It is not necessary to stop exercise at the onset of mild symptoms if there are no abnormalities noted on ECG and patient is hemodynamically stable. Indications for terminating the test include if the patient request to stop due to severe symptoms (i.e., chest pain, shortness of breath or fatigue), severe exercise-induced hypotension or hypertension, horizontal or downsloping ST depression of greater than or equal to 1 mm or ST-segment elevation, new bundle branch block, AV block, ventricular arrhythmia, if patients achieve their maximal heart rate or all stages have been completed.
At the conclusion of testing, a report should be included. This report should outline the baseline ECG interpretation, baseline heart rate, and blood pressure, ECG changes during exercise including the presence of arrhythmia/ectopy and the onset of such changes, maximal heart rate, and blood pressure during exercise, estimated exercise capacity in metabolic equivalents of task (METS) test, exercise duration and Stage completed, symptoms experienced during exercise and the reason for terminating the test.
A normal test is when patient’s blood pressure and heart rate increase appropriately to graded exercise. There should be no ECG changes suggestive of ischemia and no arrhythmias during testing. Failure of the blood pressure to increase or a decrease with signs of ischemia has a significant prognostic indication. Angina or significant ST depression (greater than 2 mm) before completing Stage 2 of the Bruce protocol and/or ST depressions that persist for more than 5 minutes into recovery suggest severe ischemia and high risk for coronary events. Exercise testing will either be positive, negative, equivocal or uninterpretable if there is a limiting factor such as heart rate.
Duke Treadmill score formula
The Duke Treadmill score is calculated as follows 6:
- Duke Treadmill Score = maximum exercise time in minutes — (5 × ST segment deviation in millimeters during or after exercise) — (4 × the treadmill angina index [where 0 = no angina, 1 = non-limiting angina, 2 = exercise limiting angina]).
The angina index has a value of 0 if the patient had no angina during exercise, 1 if the patient had nonlimiting angina, and 2 if angina was the reason the patient stopped exercising. In the original inpatient population, the Duke Treadmill score had a range from —25 (indicating the highest risk) to + 15 (indicating the lowest risk). For illustrative purposes, the sample was divided into three groups: high risk (score <— 10), moderate risk (—10 to +4), and low risk (≥ + 5). A Duke Treadmill score ⩾5 indicates low risk for cardiovascular events (predicted 4 year survival was 99%). This population does not need further investigation with coronary angiography 6. A Duke Treadmill score <–10 indicates high risk for cardiovascular events (predicted 4 year survival was 79%). These patients require further investigation with coronary angiography. A Duke Treadmill score between 4 and –10 indicates intermediate risk. Such patients may require further investigation with myocardial perfusion scanning or coronary angiography, or both, depending on the pretest probability.
The patients in the high-risk group had an average five-year survival rate <75 percent, whereas those in the low-risk group had an average five-year survival rate ≥95 percent 5. To generate a more direct method of determining prognosis on the basis of data from treadmill exercise testing, the relations described by the treadmill score have been plotted as a nomogram (Figure 1) that provides an estimate of five-year survival or average annual mortality.
Figure 1. Duke Treadmill score nomogram
Footnote: Nomogram of the prognostic relations embodied in the treadmill score. Prognosis is determined in five steps: (1) The observed amount of exercise-induced ST-segment deviation (the largest elevation or depression after resting changes have been subtracted) is marked on the line for ST-segment deviation during exercise. (2) The observed degree of angina during exercise is marked on the line for angina. (3) The marks for ST-segment deviation and degree of angina are connected with a straight edge. The point where this line intersects the ischemia-reading line is noted. (4) The total number of minutes of exercise in treadmill testing according to the Bruce protocol (or the equivalent in multiples of resting oxygen consumption [METs] from an alternative protocol) is marked on the exercise-duration line. (5) The mark for ischemia is connected with that for exercise duration. The point at which this line intersects the line for prognosis indicates the 5-year cardiovascular survival rate and average annual cardiovascular mortality for patients with these characteristics. Patients with <1 mm of exercise-induced ST-segment depression should be counted as having 0 mm. Angina during exercise refers to typical effort angina or an equivalent exercise-induced symptom that represents the patient’s presenting complaint. This nomogram applies to patients with known or suspected coronary artery disease, without prior revascularization or recent myocardial infarction, who undergo exercise testing before coronary angiography 7.
[Source 5 ] References- Vilcant V, Zeltser R. Treadmill Stress Testing. [Updated 2019 Mar 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499903
- Pargaonkar VS, Kobayashi Y, Kimura T, Schnittger I, Chow EKH, Froelicher VF, Rogers IS, Lee DP, Fearon WF, Yeung AC, Stefanick ML, Tremmel JA. Accuracy of non-invasive stress testing in women and men with angina in the absence of obstructive coronary artery disease. Int. J. Cardiol. 2019 May 01;282:7-15.
- ACC/AHA guidelines for exercise testing: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997 Jul 1;96(1):345-54. https://doi.org/10.1161/01.CIR.96.1.345
- Bruce RA, Hossack KF, DeRouen TA, Hofer V. . Enhanced risk assessment for primary coronary heart disease events by maximal exercise testing: 10 years’ experience of Seattle Heart Watch . J Am Coll Cardiol 1983; 2:565–73
- Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med. 1991 Sep 19;325(12):849-53. DOI: 10.1056/NEJM199109193251204
- Lairikyengbam SK, Davies AG. Interpreting exercise treadmill tests needs scoring system. BMJ. 2002;325(7361):443. doi:10.1136/bmj.325.7361.443 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1123951
- Mark DB, Shaw L, Harrell FE Jr, et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med. 1991; 325(12):849-853